Abstract
DWI, which is less affected by the state of the background mammary gland, has sufficient capability to diagnose invasive, noninvasive, and invasive lobular carcinoma. DWI is different from conventional methods based on blood flow data and has the potential to provide useful information for the evaluation of NAC, which is considered to be insufficient at present. Having the ability to provide steady, high-resolution tissue images, DWI is expected to play an important role in future breast cancer diagnosis. DWI, however, is not a complete method of diagnosis. Limits exist in spatial resolution and problems with ADC. In consideration of these shortcomings, we need to apply DWI to clinical practice while taking advantage of its high contrast resolution.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
DWI is an imaging method that uses in vivo thermal diffusion of water molecules. Diffusion-weighted images regularly used in clinical practice reflect the diffusion of water molecules in the extracellular fluid space and allow estimation of cellularity and tissue structure. This article outlines essentials of parameter setting of DWI for scanning mammary glands and the application of DWI to breast cancer diagnosis.
Characteristics and roles of DWI
DWI reveals cellularity and yields very high contrast resolution of tissues. Because DWI is low in spatial resolution, comparison with other types of imaging data is required to supplement anatomical data and signal interpretation. The main roles of DWI in its application to mammary gland imaging are diagnostic identification of potential lesions and reduction of oversight. More specifically, DWI identifies lesions by non-contrast imaging, identifies lesions when mastopathy exists in the background, and detects multiple ipsilateral breast cancers and contralateral breast cancers.
Areas of high signal intensity do not always represent malignant lesions. The common diagnostic procedure, therefore, involves identification of potential lesions by DWI and acquisition of supporting information from other imaging techniques. DWI data are then reinterpreted in conjunction with the supporting data.
Procedure of DWI
Table 1 shows an example of the DWI parameters used for investigating the mammary gland. The scanning conditions need to be optimized according to equipment capabilities as explained below.
Application of parallel imaging method
Presently, DWI of the body is based on data acquisition by single-shot echo-planar imaging (SS-EPI). The SS-EPI method, however, is easily affected by susceptibility artifacts. As another advance in MRI, parallel imaging techniques have been developed with the aim of reducing imaging time and improving spatial resolution, as exemplified by the sensitivity encoding (SENSE) technique [1]. Image distortion is determined by the phase-shift-per-line interval in k-space. By applying the parallel imaging technique to SS-EPI-DWI, the number of phase-encoding steps is reduced. As a result, the phase shift is reduced when the entire k-space is filled, thus leading to reduced image distortion.
Image distortion also can be reduced by reducing the field of view or increasing the pixel size, but these approaches may conflict with clinical needs. Accordingly, application of the parallel imaging technique to DWI may be warranted. Diffusion-weighted images with quality sufficient for daily clinical practice were finally achieved through the development and application of the parallel imaging technique. Comprehensive clinical application of DWI to the body has now begun.
Selection of fat suppression technique
Fat suppression is essential to breast DWI. The two main fat suppression techniques presently used for DWI are the short time inversion recovery (STIR) and chemical shift selective suppression (CHESS) methods. The STIR method used for diffusion-weighted whole-body imaging with background body signal suppression (DWIBS) provides steady fat suppression, but its signal-to-noise ratio is lower than that of CHESS. The CHESS method does not always provide uniform fat suppression, but its signal-to-noise ratio is higher.
The STIR and CHESS methods were applied to the same cases in this study to investigate the stability of the fat suppression effect, visibility in breast cancer imaging, and correlation between the two methods in terms of the apparent diffusion constant (ADC) (Figs. 1, 2) [2]. Whereas fat suppression was effective in all cases in which the STIR method was employed, uniform fat suppression was not achieved in 40% of the cases using the CHESS method. The signal intensity in breast cancer imaging was significantly higher in the CHESS method than the STIR method. Whereas the CHESS method could delineate lesions in all cases, the STIR method failed to delineate lesions in 3% of the cases. The correlation between the ADC values of the two methods was very high, and thus both methods appear to be adequate in terms of ADC. We selected the CHESS method to obtain a higher signal-to-noise ratio and performed an improvement of positioning of breast and shimming during imaging to control the nonuniform fat suppression effect.
Comparison of signal intensities obtained by different fat suppression techniques. Comparison of DWI signal intensities between the chemical shift selective (CHESS) and short tau inversion recovery (STIR) methods for the same cases. The CHESS method provides significantly higher signal intensity than the STIR method
Selection of b factor
Image contrast in DWI varies greatly with the b factor, which is a scan parameter that should be set carefully. The optimum b factor depends on target organs, lesions, and equipment. The optimum b factor should sufficiently suppress the background signal of the mammary gland and provide a cancer signal that is strong enough to allow image interpretation. Both the background and cancer signals decrease as the b factor is increased (Fig. 3). The two signals were separated considerably when the b factor was 750 s/mm2. As the b factor was increased to 1,000 s/mm2, the background signal decreased to near noise levels, whereas the cancer signal remained at a significant level. As the b factor was further increased to 1,500 s/mm2, the background signal decreased to noise levels in most cases; the cancer signal also was reduced, but was still sufficiently intense for interpretation. When the b factor was increased to 2,000 s/mm2, both the background signal and the cancer signal decreased to near noise levels, making image interpretation impossible. If only one b factor is to be selected, the present results suggest the use of 1,000 s/mm2.
Signal intensity of breast cancer and background mammary gland plotted against b-factor. The breast cancer and background mammary gland signals decrease as the b-factor increases. When the b-factor is raised to 1,000 s/mm2, the intensity of the normal mammary gland signal decreases to noise levels, but the breast cancer signal remains at a discernible level. The intensity of the mammary gland signal decreases to the bottom level when the b-factor reaches 1,500 s/mm2
Previous studies have indicated that the spread of cancers that develop mainly through breast ducts is not as restricted as that of invasive cancers [3, 4]. Therefore, if the b factor is set too high, cancers may be detected in a reduced form. In severe cases of mastopathy, the background mammary gland signal may not be suppressed sufficiently even when a b factor of 1,000 s/mm2 is used. If multiple b factor values could be selected, a combination of 750 and 1,500 s/mm2, or 1,000 and 1,500 s/mm2, may be useful.
Normal image
In diffusion-weighted images, ideally the normal mammary gland signal should be suppressed to noise levels. The signal of cysts depends on the diffusion of their content. When the content is serous, the signal intensity is low because of the low restriction on diffusion. When the content is mucinous, the signal intensity increases according to the extent of restriction on diffusion. The DWI signal of fibroadenoma depends on cellularity. When diagnosing tumors, morphologic and other data are required in addition to DWI data.
Breast cancer imaging capability
Typical diffusion-weighted images of mammary gland tumors are shown in Figs. 4 and 5. Both invasive and noninvasive cancers show high signal intensity, and the morphology of the cancers is well delineated despite low spatial resolution. The non-contrast MRI method combining DWI with STIR (DWI–STIR) has shown high performance in cancer diagnosis as discussed below [5].
a A case of invasive ductal carcinoma (solid-tubular). The morphology of the cancer observed in the DWI study, including fibrosis in the central area, agrees well with that observed in the early phase of the dynamic study. b A case of predominant intraductal component. Invasive cancer developing mainly through breast ducts. The morphology observed in the DWI study, including development through breast ducts, agrees with that observed in the early phase of the dynamic study. The DWI signal intensity is high
Images of fibroadenoma, invasive ductal carcinoma, and noninvasive cancer obtained with different b-factors in the same cases. In the fibroadenoma case, the signal intensity is suppressed when the b-factor is 750 s/mm2. In the noninvasive cancer case, the signal intensity is high when the b-factor is 750 s/mm2 and is partly suppressed when the b-factor is increased to 1,500 s/mm2. In the invasive ductal carcinoma case, the signal intensity is high even when the b-factor is 1,500 s/mm2
Invasive cancer
A total of 54 cases were studied: 22 cases of papillotubular carcinoma, 22 cases of solid-tubular carcinoma, and 10 cases of scirrhous carcinoma. The cancers could be detected by the DWI–STIR method in all 54 cases. No significant differences were observed in the percentages of correct diagnosis between different pT categories or different mammary gland densities.
Noninvasive cancer
A total of 30 cases were studied, and cancers could be detected as malignant lesions by the DWI–STIR method in 26 cases (87%). Seven cases were identified as mammography category 1 or 2, and five cases (71%) could be diagnosed as malignant lesions by the DWI–STIR method. When the background mammary gland was classified into two categories, fatty and fibroglandular breast (10 cases) and heterogeneous and dense breasts (20 cases), their percentages of correct diagnosis were 80 and 90%, respectively. The percentages were high, with no significant differences between different mammary gland densities.
Invasive lobular cancer
A total of 30 cases were studied, and cancers could be detected as malignant lesions by the DWI–STIR method in 28 cases (93%). Of the 30 cases, 6 were identified as mammography category 1 or 2, and 5 cases (83%) could be diagnosed as malignant lesions by the DWI-STIR method. Excluding the pT4 category (2 cases), the percentages of correct diagnosis for the pT1 category (12 cases) and the pT2 and pT3 categories (16 cases) were 92 and 94%, respectively. When the background mammary gland was classified into two categories, fatty and fibroglandular breast (6 cases) and heterogeneous and dense breasts (24 cases), their percentages of correct diagnosis were 100 and 92%, respectively. The percentages were high, with no significant differences between different pT categories or different mammary gland densities.
Evaluation of neoadjuvant chemotherapy
Neoadjuvant chemotherapy (NAC) has been found to be effective for breast cancer and is being applied to an increasing number of cases. NAC is found to correlate with prognosis only when the therapeutic effect is judged as a pathologically complete response (pCR). Although diagnosis of pCR is required in diagnostic imaging, the therapeutic effect is difficult to judge in many cases because of the additional effects of NAC.
Regarding the 47 cases of breast cancer to which NAC was applied and the effect was judged as a complete response, the diagnostic performance of conventional Gd-dynamic MRI combined with DWI was investigated. Specificity remained the same, but sensitivity and negative predictive value were improved significantly when DWI was added to Gd-dynamic MRI (Table 2). This result possibly reflects that lesions contrasted only in the late phase of Gd-dynamic MRI could be distinguished to some extent as either remnant cancer or fibrotic change by using DWI. Complete diagnosis of small cancer foci, however, is impossible with the addition of DWI data. The use of other methods of examination (e.g., ultrasound), therefore, is essential in conjunction with DWI. Even biopsy may be required if the diagnosis greatly affects therapeutic decisions.
Application to cancer screening
The ultimate objective of cancer screening is to improve the vital prognosis of individual cancer patients and reduce the mortality of the population. Accurate and timely detection of cancer is crucial in situations where lives can be saved. The conditions for the use of DWI for cancer screening are that the target cancer can be detected in a timely manner and that a reasonable level of cost effectiveness can be achieved compared with other examination methods. Appropriate selection of patients to be examined also must be carefully considered; high-risk groups are likely to be given priority. At present, we do not have sufficient objective data to evaluate the effectiveness of using DWI for cancer screening, and future studies are warranted.
Pitfalls
Measurement of ADC
In the conventional MRI diagnosis of mammary gland tumors, benign and malignant tumors have been distinguished mainly on the basis of morphology and blood flow data. As DWI has become more widely employed, a new approach for distinguishing between benign and malignant tumors through ADC measurements is being pursued. Compared with normal mammary gland and benign tumors, cancers cause low ADC values because of significantly reduced diffusion. However, cancers cannot be distinguished completely from benign tumors because there is an overlap between their ADC ranges. Moreover, MRI equipment is not yet precise enough to be used as a measuring instrument in routine clinical practice, and problems exist in the measurement methods.
The following equation generally holds true for diffusion-weighted images.
D is the actual coefficient of diffusion. S is the signal intensity when the MPG (motion probing gradient) pulse is used. S(0) is the signal intensity when the MPG pulse is not used. b is the b-factor. ADC is approximated by:
f is the ratio of perfusing water molecules. Thus, the b-factor is given by
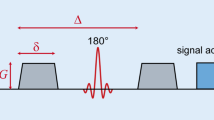
γ is the gyromagnetic ratio. G is the intensity of the MPG pulse. δ is the duration of the MPG pulse application. Δ is the time between the first MPG pulse application and the next MPG pulse application (Fig. 6). Here, Δ − δ/3 is considered the duration of diffusion observation.
Sequence design of SE-type single-shot EPI-DWI and equation for b-factor. The value of the b-factor is given by: b = γ 2 G 2 δ 2(Δ − δ/3) where G is the intensity of the MPG pulse, δ is the duration of the MPG pulse application, Δ is the time between the first MPG pulse application and the next MPG pulse application, and γ is the gyromagnetic ratio. The duration of diffusion observation is given by Δ − δ/3
When we measure diffusion-weighted images in clinical practice, the b-factor is determined by assigning appropriate values to G, δ, and Δ, which are specific to the equipment. These values affect ADC measurement in terms of the duration of observation. Also, the effects of perfusion, signal intensity during measurement, and the ratio between bound and free water cannot be neglected. Figure 7 shows how ADC depends on the b-factor. ADC decreases as b-factor increases. If the b-factor is further increased, measurement will become impossible because of reduced signal intensity.
To measure ADC, the region of interest needs to be set by the operator, which is arbitrary and adds to the above problems. It is prudent to use ADC only for reference purposes because of difficulty in achieving universality in ADC measurement.
Conclusion
Through the progress of recent MR technique, application to breast cancer of DWI has established. To interpret DWI, we can use molecular information for diagnosis of breast cancer and evaluation of neoadjuvant chemotherapy, as well as conventional morphologic and vascular information. In the future, a further study of the diffusion phenomenon in vivo and optimization of the scan parameter in the higher magnetic fields is expected.
References
Pruessmann KP, Weiger M, Scheidegger MB, et al. SENSE: sensitivity encoding for fast MRI. Magn Reson Med. 1999;42:952–62.
Kazama T, Nasu K, Kuroki Y, et al. A change of image quality of DWI of breast: influence of a difference of fat suppression methods. In: 31st Chiba MRI Conference 2005.
Kuroki Y, Nasu K, Kuroki S, et al. Diffusion-weghted imaging of breast cancer with the sensitivity encoding technique: analysis of apparent diffusion coefficient value. Magn Reson Med Sci. 2004;3:79–85.
Woodhams R, Matsunaga K, Iwabuchi K, et al. Diffusion-weighted imaging of malignant breast tumor: the usefulness of apparent diffusion coefficient (ADC) value and ADC map for the detection of malignant breast tumors and evaluation of cancer extension. J Comput Assist Tomogr. 2005;29:644–9.
Kuroki-Suzuki S, Kuroki Y, Nasu K, et al. Detecting breast cancer with non-contrast MR imaging: combining diffusion-weighted and STIR imaging. Magn Reson Med Sci. 2007;6(1):21–7.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kuroki, Y., Nasu, K. Advances in breast MRI: diffusion-weighted imaging of the breast. Breast Cancer 15, 212–217 (2008). https://doi.org/10.1007/s12282-008-0050-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-008-0050-3