Abstract
Purpose of Review
This review summarizes the fungal literature currently available for adult tinea capitis (ATC), as well as providing data for clinical practice.
Recent Findings
Available studies in ATC are scarce; however, they provide essential information for treating ATC.
Summary
Treatment of TC is effective; however, it needs a minimum of 1 month to watch clinical efficacy. Systemic treatment is often needed to favor drug penetration to the deepest part of the hair follicle. The newest oral antifungal has higher efficacy rates than conventional therapy, as well as much shorter duration of treatment but at higher costs. We review the literature concerning ATC, including treatment schemes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Superficial mycoses caused by dermatophytes comprise four principal genera: Trichophyton, Microsporum, Nannizzia, and Epidermophyton. None of these is part of the microbiota of the skin and may provoke hair diseases, nail thickening or plaques with erythema, and scaling with active borders. The first involves tinea capitis (TC), an infection or parasitization of the hair, scalp, eyebrows, and eyelashes. It is commonly observed in scalp hair related to dermatophytic fungi (Trichophyton, Microsporum, and Nannizzia) and more often in children, although there is a growing number of reports in adults (Table 1) [12••, 13•].
The global epidemiology of TC is varied; Trichophyton tonsurans is the most common agent in America, Europe, and Africa, followed by Microsporum canis, mostly in Mediterranean countries. The most important carriers of dermatophytes are cats, dogs, and rabbits [14].
Epidemiology
Tineas are cosmopolitan mycoses that predominate in tropical environments; these are considered the most frequent fungal diseases, appearing in subjects of any age, race, or sex, as well as any socioeconomic level or occupation [15]
In epidemics caused by T. tonsurans affecting the head, infections are usually subclinical and related to fomites; epidemics due to M. canis are related to contact with dogs or cats. Some factors are commonly associated with TC, including socioeconomic status (rural and suburban regions), poor hygiene, and overcrowding, usually schools, where the infection spreads rapidly [1•, 16,17,18,19].
Shaving hair is one of the most commonly related habits. Immunosuppression is also an increased risk factor for TC, mainly among adults [10, 11].
Although TC is rarely reported in adults, as shown in several studies [1•, 2, 3,4,5, 12••, 13•, 20], it is far from being exceptional. In a study carried out in the Afro-American population in the USA, the incidence of TC in adults was 11.4% [21]. In a study, Park et al. reported a rate of up to 44% of TC in adults [1•]. However, most studies report an incidence ranging from 2 to 5.8% [2,3,4,5].
In Mexico, TC predominates in rural or suburban areas, and it is more frequent in rural workers and people of low socioeconomic status. It is almost exclusive among children (98%); it often affects women after puberty and around the menopause or the elderly in a frequency ranging from 2 to 2.5% of cases [13•].
It can also occur in immunosuppressed people (HIV/AIDS infection, posttransplant, immunosuppressant, etc.). The asymptomatic carrier status, usually in adults of the same family of the patients, is related to flares in children [12••]. Previous studies have documented a higher incidence of adult TC among menopausal women [6•], explained by the involution of sebaceous glands following a decreased blood estrogen level during menopause [22, 23].
Etiopathogenesis
The most often associated agents in adult TC include T. tonsurans, T. violaceum, T. verrucosum, M. canis, and N. gypsea [5].
Dermatophytes reproduces in the stratum corneum, penetrating at the follicular infundibulum, and invades the hair sheath; it extends to the depth without exceeding the keratogenic zone (Adamson’s stripe) (the growth of hyphae and arthroconidia occurs in the opposite direction of hair growth) [13•]. Simultaneously, it extends towards the distal part of the hair developing a thick, fragile, and easily breaking hair [12••, 13•].
Typically, the growth of the fungus takes place inside the hair bulb, generating spores without affecting the cuticle (endothrix) or affecting it (ectotrix). These infections develop in parallel with hair growth [12••, 13•]. The keratinocyte fungal adhesion favors the infection from one host to another, which eventually progresses into an active infection [24].
Fungal proteolytic enzymes favor invasion even in hostile media (acid or alkaline) [24]. Protease genes are variably expressed with different enzyme patterns in human infection or in vitro cultures [25].
In some patients, an intense inflammatory reaction occurs; in others, it is minimal, and there may be asymptomatic commensalism between fungus and host [1•]. The degree of response relies on two aspects: (1) the causal species; strains of granular morphology have high production of enzymes; it is also probable that some strains produce substances that expel near bacteria; arthroconidia production is related to the parasitic form (the zoophilic and geophilic strains generate intense inflammation), and (2) the degree of host hypersensitivity [12••, 13•].
Increased cellular immunity and a delayed hypersensitivity reaction contribute to clinical and mycological cure; while defects of cellular immunity and the hypersensitivity reaction as occurring among adults, may predispose to chronic and recurrent dermatophytosis [6•, 13•].
The relative resistance to TC after puberty is probably due to the presence of long-chain fatty acids; however, in adults, mainly in postmenopausal women, there are quantitative and qualitative variations of cutaneous sebum, in particular of medium-chain fatty acids [26].
Clinical Manifestations
TC is commonly seen in children, and rarely seen among adults. M. canis and T. tonsurans are the causal agents identified in Mexico and many Latin American counties. TC can be dry or inflammatory, although the state of asymptomatic carrier and a clinical presentation with diffuse flake pityriasis capitis-type are present when the causative agent is T. tonsurans [13•].
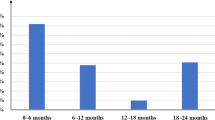
The clinical appearance of TC is determined by the ability of the fungus to invade the hair, and the host immune status. The clinical expressions vary from an asymptomatic carrier to severe inflammatory presentations that develop scarring alopecia. Most affected patients are children from 6 months to 12 years [27, 28]. The typical clinical pattern includes broken hairs with scaling; however, this image has changed due to the geographical distribution of the infectious species [29].
Adult TC (ATC) has a different presentation than in children. In a study by Park et al [1•], .they found that the most common clinical type of ATC was pustular and similar to seborrheic dermatitis (26.8% and 25.5%, respectively), initially diagnosed in about 65.9% of cases such as folliculitis or dermatitis seborrheic, which contributed to the delay in diagnosis in up to 7–8 months; usually in children’s TC the duration in confirmation of the diagnosis is less than 1 month. The authors observed that more than half of patients with ATC (62.2%) had no obvious alopecia. The low frequency of the disease as well as the atypical presentation can contribute to delayed diagnosis, so ATC requires a high index of suspicion, and a mycological study should be performed on adult patients, mainly the elderly with inflammatory changes in the scalp (Fig. 1a) even without an alopecia patch.
a A 78 year-old female with an 8-month history of scaling, patchy hair loss, and mild perifollicular erythema. b Dermoscopy of the scalp showing comma hairs (white arrow) and corkscrew hairs (black arrow). c Spore ectothrix fungus typical of M. canis surrounds and fills the hair shafts (Grocott, 60×)
The carrier status is considered in non-clinically asymptomatic infections. This status is usually evident in children or parents, becoming potential reservoirs of fungi and thus spreading the infection [11, 13•].
Diagnosis
Direct Examination
Direct examination shows long, tabicated, and artrosporated hyphae. In the trichoscopic study, when viewing with the dermatoscopy, the pseudo-alopecia patch of the microsporic TC, short hair, “coma” hairs, corkscrew, and peripilar chainstays is found (Fig. 1b). The hair can present five types of parasitism, two endothrix, and three ecto-endothrix. The trichophytic parasitism (T. tonsurans) with many spores clustered densely inside the hair, and a phallic form with few spores and hyphae as well as with air vesicles inside the hair (T. schoenleinii) is evident in the endothrix type [13•].
The parasitoid ectoendothrix (classic ectothrix) has a microscopic modality (M. canis) with small spores that form a cuff around the hair, a microid form with spores with loose disposition around the hair (T. mentagrophytes), and a megasporated presentation (T. verrucosum) with large spores around the hair (Fig. 1c) [13•].
Culture
Macroscopic and microscopic characteristics of the colonies are useful for diagnosis; Trichophyton colonies have smooth walls, in Microsporum and Nannizzia equinulated and Epidermophyton colonies are also smooth, the latter without microconidia [13•].
Molecular Studies and Dermatoscopy
Molecular tools with enough specificity using different techniques are available: standard polymerase chain reaction [30, 31], as well as the newest diagnostic methods, such as multiplex-dependent probe amplification and rolling circle amplification [32], allowing faster and more accurate results for identifying dermatophytes. Trichoscopy (dermoscopy) is a diagnostic technique widely used in dermatology [33, 34]. In infections by T. tonsurans, multiple “coma”, as well as corkscrew hairs, can be seen [35]; while in M. canis infection, we can observe dystrophic and elbow-shaped hairs, and different levels of broken hair height [36]. Campos et al. [37], in a prospective study, found that trichoscopy is also useful for recording the response to treatment; they observed that 8 weeks after starting treatment, all the dermatoscopic signs evaluated with TC decreased at the end of follow-up; there was no dystrophic hair. The authors inferred that disappearing dystrophic hair could be a marker of therapeutic success.
In a study by Arrazola-Guerrero et al. [38], which included 37 Latin American patients, mostly children, the following dermatoscopic patterns were confirmed: “coma hairs” (41%), corkscrew hairs (22%), short hairs (49%), and black dots (33%). They also observed the presence of scales (89%), peripilarial cylinders (46%), alopecia (65%), pustules (8%), and meliceric crusts (16%).
Histopathological Study
A biopsy is not usually necessary in superficial TC since there are no specific images; however, hyperkeratosis with parakeratosis and the presence of hyphae between the corneous cells may be seen. In TC, parasitized hair is detected, with rounded arthrospores into the follicles or the stratum corneum [39].
Wood’s Light
It is carried out in a dark room, and an ultraviolet light lamp of 320 to 400 nm is used and gives a green fluorescence in microscopic hairs, white-bluish in the favus, and does not generate any in trichophytic tinea [40]. Wood’s light shows fluorescence in microsporic and favic hairs; also, Wood’s light may be useful for therapy follow-up and carrier status [41].
Differential Diagnosis
TC in adults often present an atypical clinical pattern, which can easily lead to confusion with other dermatoses, resembling bacterial folliculitis, folliculitis decalvans, dissecting cellulitis, or the scarring related to lupus erythematosus. Thus, the correct diagnosis and treatment are delayed often, increasing the risk of a new infection. Other diagnoses include seborrhoeic dermatitis, alopecia areata, trichotillomania, psoriasis, discoid lupus erythematosus, impetigo, folliculitis, and erosive pustular dermatosis [1•, 12••, 13•].
Treatment
Treatment of ATC is similar to that of TC in children; however, it is necessary to take into account the age of the patient by association with different comorbidities and interactions with other treatments. The most suitable treatment for TC is griseofulvin, 10 to 20 mg/kg/day, and in resistant cases, up to 30 mg for 8 to 12 weeks. In older than 12 years old, 500 mg/day is usually prescribed (although some authors recommend higher doses for micronized griseofulvin) [42, 43•]. Fatty meals, milk, or ice cream increase the bioavailability of griseofulvin [13•].
It is possible to add a topical antifungal or 2.5% Selenium disulphur or azoles in shampoo to remove spores from the surface of the scalp; after a week, there is no possible transmission. It is advisable to lightly rub the affected areas during the bath to remove parasitized hairs or scales. The treatment lasts 2 to 3 months (it is advisable to prolong the treatment 1 month after the clinical cure). It is advisable to check for infected animals or relatives and use bleaches to disinfect fomites [12••, 13•].
In a recent meta-analysis about the efficacy of oral antifungals for TC [44], it was stated that terbinafine is “more efficacious than” griseofulvin for TC caused by Trichophyton sp., while griseofulvin is “more efficacious than” terbinafine for Microsporum sp. In a recent Cochrane summary review, Chen et al. [45••] included 25 randomized controlled trials (4449 study subjects). The authors found that terbinafine and griseofulvin had similar effects in children with both microscopic and trichophytic infections. Terbinafine showed a higher rate of complete cure compared with griseofulvin in T. tonsurans infections; however, griseofulvin was better for Microsporum sp. Itraconazole and fluconazole show similar efficacy against Trichophyton infections but are not optimal choices.
Terbinafine is active at a dose of 250 mg or 10 mg/kg, and a dose of 3 to 6 mg/kg/day, in case of trichophytic tinea for at least 1 week and in microsporic TC for 4 weeks. It is often required to prolong the treatment or double the dose. An additional alternative for microsporic TC is itraconazole 100 mg/day for 4 weeks [44].
Both terbinafine and itraconazole can also be given as intermittent therapy (“pulses”) of 1 week each month, for at least 3 months [46,47,48].
For patients without a clinical cure, it is advisable to consider lack of adherence; suboptimal drug absorption; fungal resistance; biofilm formation [49]; as well as reinfection. When clinical improvement is observed, although mycological cure has not been achieved, treatment should be continued for an additional month. If there has been no clinical response and signs persist at the end of the treatment period, we can increase the dose or the treatment duration [45••].
The most commonly used oral antifungal is safe for long periods, or even at higher doses. In resistant cases, we recommend changing the treatment for another oral antifungal, for example, in cases of lack of response to griseofulvin, change to terbinafine or itraconazole [50,51,52].
The choice of the oral antifungal drug depends on the characteristics of the patient; griseofulvin has been widely used and, more recently, terbinafine [47]. Ketoconazole, itraconazole, and fluconazole are used to a lesser extent. In AIDS patients, some authors recommend terbinafine [53, 54]; however, it can be ineffective in cases of TC due to M. canis, and thus, griseofulvin is preferred [47]. Frequent and significant adverse reactions have been reported with griseofulvin and terbinafine, mainly in transplant patients due to its interaction with cyclosporine [55, 56]. Also, several studies have shown a faster efficacy of terbinafine when compared with griseofulvin (4 weeks vs. 8 weeks) in TC related to Trichophyton [57, 58].
Prevention
There is no effective preventive measure for TC; a vaccine that prevents infection in animals has been developed; however, it is not suitable for humans [59].
Conclusion
TC is a common disease throughout the world, with a wide variety of clinical presentations leading to many differential diagnoses. It is often seen in adults, mostly postmenopausal women, and immunosuppressed patients. The use of oral antifungal medications for clinical and mycological cures is commonly required in order to prevent epidemics and carrier status.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Park SK, Park SW, Yun SK, Kim HU, Park J. Tinea capitis in adults: a 18-year retrospective, single-centre study in Korea. Mycoses. 2019;62:609–16. https://doi.org/10.1111/myc.12916This paper shows the most common clinical manifestations of tinea capitis in adults.
Oh SH, Kim SH, Suh SB. Tinea capitis of adults in Taegu city for 11 years (1978~1988). Korean J Dermatol. 1989;27:666–79.
Aste N, Pau M, Biggio P. Tinea capitis in adults. Mycoses. 1996;39:299–301. https://doi.org/10.1111/j.1439-0507.1996.tb00142.x.
Mebazaa A, Oumari KE, Ghariani N, Mili AF, Belajouza C, Nouira R, et al. Tinea capitis in adults in Tunisia. Int J Dermatol. 2010;49:513–6. https://doi.org/10.1111/j.1365-4632.2010.04296.x.
El-Khalawany M, Shaaban D, Hassan H, et al. A multicenter clinicomycological study evaluating the spectrum of adult tinea capitis in Egypt. Acta Dermatovenerol Alp Pannonica Adriat. 2013;22:77–82. https://doi.org/10.2478/v10162-012-0040-1.
• Lova-Navarro M, Gómez-Moyano E, Martínez Pilar L, Fernandez-Ballesteros MD, Godoy-Díaz DJ, Vera-Casaño A, et al. Tinea capitis in adults in southern Spain. A 17-year epidemiological study. Rev Iberoam Micol. 2016;33:110–3. https://doi.org/10.1016/j.riam.2015.02.007This paper shows the most common clinical manifestations of tinea capitis in adults.
Devliotou-Panagliotidou D, Koussidou-Eremondi T, Chaidemenos GC, Theodoridou M, Minas A. Tinea capitis in adults during 1981-95 in northern Greece. Mycoses. 2001;44:398–400. https://doi.org/10.1046/j.1439-0507.2001.00675.x.
Cervetti O, Albini P, Arese V, Ibba F, Novarino M, Panzone M. Tinea capitis in adults. Adv Microbiol. 2014;4:12–4. https://doi.org/10.4236/aim.2014.41003.
Duarte B, Galhardas C, Cabete J. Adult tinea capitis and tinea barbae in a tertiary Portuguese hospital: a 11-year audit. Mycoses. 2019. https://doi.org/10.1111/myc.12991.
Diop A, Ly F, Diagne F, Ndiaye MT, Seck B, Ndiaye M, et al. Epidemiological, clinical and etiological profile of tinea capitis in adult patients in Dakar, Senegal. Ann Dermatol Venereol. 2019;146:100–5. https://doi.org/10.1016/j.annder.2018.11.007.
Khosravi AR, Shokri H, Vahedi G. Factors in etiology and predisposition of adult tinea capitis and review of published literature. Mycopathologia. 2016;181:371–8. https://doi.org/10.1007/s11046-016-0004-9.
•• Hay RJ. Tinea capitis: current status. Mycopathologia. 2017;182:87–93. https://doi.org/10.1007/s11046-016-0058-8This paper gives important strategies for treating tinea capitis.
• Rebollo N, López-Barcenas AP, Arenas R. Tinea apitis. Actas Dermosifiliogr. 2008;99:91–100. https://doi.org/10.1016/S0001-7310(08)74630-1This paper offers an excellent overview of the disease.
Bennassar A, Grimalt R. Management of tinea capitis in childhood. Clin Cosmet Investig Dermatol. 2010;3:89–98.
Beardsley J, Denning DW, Chau NV, Yen NT, Crump JA, Day JN. Estimating the burden of fungal disease in Vietnam. Mycoses. 2015;58:101–6. https://doi.org/10.1111/myc.12382.
Nenoff P, Krüger C, Ginter-Hanselmayer G, Tietz HJ. Mycology - an update. Part 1: dermatomycoses: causative agents, epidemiology, and pathogenesis. J Dtsch Dermatol Ges. 2014;12:188–209. https://doi.org/10.1111/ddg.12245.
Farag AGA, Hammam MA, Ibrahem RA, Mahfouz RZ, Elnaidany NF, Qutubuddin M, et al. Epidemiology of dermatophyte infections among school children in Menoufia Governorate, Egypt. Mycoses. 2018;61:321–5. https://doi.org/10.1111/myc.12743.
Aly R. Ecology, epidemiology and diagnosis of tinea capitis. Pediatr Infect Dis J. 1999;18:180–5. https://doi.org/10.1097/00006454-199902000-00025.
Cafarchia C, Romito D, Capelli G, Guillot J, Otranto D. Isolation of Microsporum canis from the hair coat of pet dogs and cats belonging to owners diagnosed with M. canis tinea corporis. Vet Dermatol. 2006;17:327–31. https://doi.org/10.1111/j.1365-3164.2006.00533.x.
Lee JY, Hsu ML. Tinea capitis in adults in Southern Taiwan. Int J Dermatol. 1991;30:572–5. https://doi.org/10.1111/j.1365-4362.1991.tb02643.x.
Silverberg NB, Weinberg JM, DeLeo VA. Tinea capitis: focus on African American women. J Am Acad Dermatol. 2002;46:S120–4. https://doi.org/10.1067/mjd.2002.120793.
Toksöz L, Güzel AB, Ilkit M, Akar T, Saraçlı MA. Scalp dermatophyte carriage in pregnant, pre-, and postmenopausal women: a comparative study using the hairbrush and cytobrush methods of sample collection. Mycopathologia. 2011;171:339–44. https://doi.org/10.1007/s11046-010-9377-3.
Chen W, Yang CC, Todorova A, Al Khuzaei S, Chiu HC, Worret WI, et al. Hair loss in elderly women. Eur J Dermatol. 2010;20:145–51. https://doi.org/10.1684/ejd.2010.0828.
Yamada N, Wakumoto K, Yamamoto O. Scanning electron microscopic observation on the parasitic form of the fungi in the horny layer in dermatophytosis. Med Mycol J. 2012;53:117–21. https://doi.org/10.3314/mmj.53.117.
Kaufman G, Horwitz BA, Duek L, Ullman Y, Berdicevsky I. Infection stages of the dermatophyte pathogen Trichophyton: microscopic characterization and proteolytic enzymes. Med Mycol. 2007;45:149–55. https://doi.org/10.1080/13693780601113618.
Terragni L, Lasagni A, Oriani A. Tinea capitis in adults. Mycoses. 1989;32:482–6.
Chen M, Xu Y, Hong N, Yang Y, Lei W, Du L, et al. Epidemiology of fungal infections in China. Front Med. 2018;12:58–75. https://doi.org/10.1007/s11684-017-0601-0.
Chokoeva AA, Zisova L, Sotiriou E, Miteva-Katrandzhieva T. Tinea capitis: a retrospective epidemiological comparative study. Wien Med Wochenschr. 2017;167:51–7. https://doi.org/10.1007/s10354-016-0493-7.
Vena GA, Chieco P, Posa F, Garofalo A, Bosco A, Cassano N. Epidemiology of dermatophytoses: retrospective analysis from 2005 to 2010 and comparison with previous data from 1975. New Microbiol. 2012;35:207–13.
Farokhipor S, Ghiasian SA, Nazeri H, Kord M, Didehdar M. Characterizing the clinical isolates of dermatophytes in Hamadan city, central west of Iran, using PCR-RLFP method. J Mycol Med. 2018;28:101–5. https://doi.org/10.1016/j.mycmed.2017.11.009.
Allahdadi M, Hajihossein R, Kord M, Rahmati E, Amanloo S, Didehdar M. Molecular characterization and antifungal susceptibility profile of dermatophytes isolated from scalp dermatophyte carriage in primary school children in Arak city, center of Iran. J Mycol Med. 2019;29:19–23. https://doi.org/10.1016/j.mycmed.2019.01.002.
Deng S, Zhou Z, de Hoog GS, Wang X, Abliz P, Sun J, et al. Evaluation of two molecular techniques for rapid detection of the main dermatophytic agents of tinea capitis. Br J Dermatol. 2015;173:1494–500. https://doi.org/10.1111/bjd.14156.
Bourezane Y, Bourezane Y. Analysis of trichoscopic signs observed in 24 patients presenting tinea capitis: hypotheses based on physiopathology and proposed new classification. Ann Dermatol Venereol. 2017;144:490–6. https://doi.org/10.1016/j.annder.2016.12.012.
Lacarrubba F, Micali G, Tosti A. Scalp dermoscopy or thichoscopy. Curr Probl Dermatol. 2015;47:21–32. https://doi.org/10.1159/000369402.
Daroach M, Hanumanthu V, Kumaran MS. Utility of trichoscopy in tinea capitis. Postgrad Med J. 2019;95:173. https://doi.org/10.1136/postgradmedj-2018-136106.
Lekkas D, Ioannides D, Apalla Z, Lallas A, Lazaridou E, Sotiriou E. Dermoscopy for discriminating between Trichophyton and Microsporum infections in tinea capitis. J Eur Acad Dermatol Venereol. 2018;32:e234–5. https://doi.org/10.1111/jdv.14755.
Campos S, Brasileiro A, Galhardas C, Apetato M, Cabete J, Serrão V, et al. Follow-up of tinea capitis with trichoscopy: a prospective clinical study. J Eur Acad Dermatol Venereol. 2017;31:e478–80. https://doi.org/10.1111/jdv.14322.
Arrazola-Guerrero J, Isa-Isa R, Torres-Guerrero E, Arenas R. Tinea capitis. Dermoscopic findings in 37 patients. Rev Iberoam Micol. 2015;32:242–6. https://doi.org/10.1016/j.riam.2014.09.002.
Auchus IC, Ward KM, Brodell RT, Brents MJ, Jackson JD. Tinea capitis in adults. Dermatol Online J. 2016;22.
Trovato MJ, Schwartz RA, Janniger CK. Tinea capitis: current concepts in clinical practice. Cutis. 2006;77:93–9.
Wigger-Alberti W, Elsner P. Fluorescence with Wood’s light. Current applications in dermatologic diagnosis, therapy follow-up and prevention. Hautarzt. 1997;48:523–7.
Bhanusali D, Coley M, Silverberg JI, Alexis A, Silverberg NB. Treatment outcomes for tinea capitis in skin of color population. J Drugs Dermatol. 2012;11:852–6.
• Bar J, Samuelov L, Sprecher E, Mashiah J. Griseofulvin vs terbinafine for paediatric tinea capitis: when and for how long. Mycoses. 2019. https://doi.org/10.1111/myc.12970An important review of the main therapeutic options for adult tinea capitis.
Tey HL, Tan AS, Chan YC. Meta-analysis of randomized, controlled trials comparing griseofulvin and terbinafine in the treatment of tinea capitis. J Am Acad Dermatol. 2011;64:663–70. https://doi.org/10.1016/j.jaad.2010.02.048.
•• Chen X, Jiang X, Yang M, Bennett C, González U, Lin X, et al. Systemic antifungal therapy for tinea capitis in children: an abridged Cochrane review. J Am Acad Dermatol. 2017;76:368–74. https://doi.org/10.1016/j.jaad.2016.08.061Important paper that summarizes the clinical trials available for tinea capitis.
Gupta AK, Adam P, Hofstader SL, Lynde CW, Taborda P, Taborda V, et al. Intermittent short duration therapy with fluconazole is effective for tinea capitis. Br J Dermatol. 1999;141:304–6. https://doi.org/10.1046/j.1365-2133.1999.02981.x.
Nyawalo JO, Bwire M. Single dose and intermittent griseofulvin regimens in the treatment of tinea capitis in Kenya. Mycoses. 1988;31:229–34. https://doi.org/10.1111/j.1439-0507.1988.tb03871.x.
McClellan KJ, Wiseman LR, Markham A. Terbinafine. An update of its use in superficial mycoses. Drugs. 1999;58:179–202. https://doi.org/10.2165/00003495-199958010-00018.
Danielli LJ, Lopes W, Vainstein MH, Fuentefria AM, Apel MA. Biofilm formation by Microsporum canis. Clin Microbiol Infect. 2017;23:941–2. https://doi.org/10.1016/j.cmi.2017.06.006.
Ginter-Hanselmayer G, Smolle J, Gupta A. Itraconazole in the treatment of tinea capitis caused by Microsporum canis: experience in a large cohort. Pediatr Dermatol. 2004;21:499–502. https://doi.org/10.1111/j.0736-8046.2004.21419.x.
Kovacs SO, Hruza LL. Superficial fungal infections. Getting rid of lesions that don’t want to go away. Postgrad Med. 1995;98:61–2 68–9, 73–5.
Degreef HJ, DeDoncker PR. Current therapy of dermatophytosis. J Am Acad Dermatol. 1994;31:S25–30. https://doi.org/10.1016/s0190-9622(08)81263-7.
Ferguson L, Fuller LC. Spectrum and burden of dermatophytes in children. J Inf Secur. 2017;74:S54–60. https://doi.org/10.1016/S0163-4453(17)30192-5.
Bournerias I, De Chauvin MF, Datry A, Chambrette I, Carriere J, Devidas A, et al. Unusual Microsporum canis infections in adult HIV patients. J Am Acad Dermatol. 1996;35:808–10. https://doi.org/10.1016/s0190-9622(96)90089-4.
Lo AC, Lui SL, Lo WK, Chan DT, Cheng IK. The interaction of terbinafine and cyclosporine a in renal transplant patients. Br J Clin Pharmacol. 1997;43:340–1.
Güleç AT, Demirbilek M, Seçkin D, Can F, Saray Y, Sarifakioglu E, et al. Superficial fungal infections in 102 renal transplant recipients: a case-control study. J Am Acad Dermatol. 2003;49:187–92. https://doi.org/10.1067/s0190-9622(03)00861-2.
Mikaeili A, Kavoussi H, Hashemian AH, Shabandoost Gheshtemi M, Kavoussi R. Clinico-mycological profile of tinea capitis and its comparative response to griseofulvin versus terbinafine. Curr Med Mycol. 2019;5:15–20. https://doi.org/10.18502/cmm.5.1.532.
Gupta AK, Mays RR, Versteeg SG, Piraccini BM, Shear NH, Piguet V, et al. Tinea capitis in children: a systematic review of management. J Eur Acad Dermatol Venereol. 2018;32:2264–74. https://doi.org/10.1111/jdv.15088.
Frymus T, Gruffydd-Jones T, Pennisi MG, Addie D, Belák S, Boucraut-Baralon C, et al. Dermatophytosis in cats: ABCD guidelines on prevention and management. J Feline Med Surg. 2013;15:598–604. https://doi.org/10.1177/1098612X13489222.
Kelati A, Meziane M, Soughi M, Mernissi F. Erythema nodosum due to tinea. Arch Pediatr. 2016;23:727–30. https://doi.org/10.1016/j.arcped.2016.04.014.
Romano C, Gaviria EM, Feci L, Fimiani M. Erythema nodosum complicating kerion of the scalp caused by Trichophyton mentagrophytes. J Eur Acad Dermatol Venereol. 2016;30:357–9. https://doi.org/10.1111/jdv.12775.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Fungal Infections of Skin and Subcutaneous Tissue
Rights and permissions
About this article
Cite this article
Tirado-Sánchez, A., Estrada-Caraveo, Y., Saldaña, M. et al. Adult Tinea Capitis: a Clinical Entity in Increasing Frequency. Curr Fungal Infect Rep 13, 196–202 (2019). https://doi.org/10.1007/s12281-019-00366-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-019-00366-2