Abstract
We previously demonstrated the alleviation of ovalbumin (OVA)-induced airway inflammation by Inulae flos. In the present study, the effects of britanin, a sesquiterpene compound isolated from Inulae flos, were evaluated in an in vivo animal model for anti-asthma activity through observation of airway hyperresponsiveness (AHR), eosinophil recruitment, Th2 cytokine and IgE levels, and lung histopathology. Britanin administration effectively reduced AHR induced by aerosolized methacholine, airway eosinophilia, Th2 cytokines in bronchoalveolar lavage fluids and the supernatant of cultured splenocytes compared with OVA-induced mice. Histological studies showed that increased inflammatory cell infiltration and mucus secretion were reduced by britanin administration. Thus, britanin may have therapeutic potential for treating allergic asthma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma is a chronic inflammatory disease of the lung characterized by inflammatory cell infiltration, airway hyperresponsiveness (AHR), and mucus overproduction. The prevalence of asthma is increasing around the world, with higher asthma rates in more developed and westernized countries (Kim et al. 2013). Current standard medications for asthma are limited to symptomatic control of disease mediators including inhaled corticosteroids, β2-agonists, leukotriene modifiers, and others (Szefler 2011; Baker et al. 2014).
Both eosinophils and T helper 2 (Th2) lymphocytes play pathogenic roles in asthma (Kudo et al. 2013). Eosinophils are commonly associated with allergic inflammation and act as effector cells in the pathogenesis of this disease by releasing cytotoxic granule proteins. Th2 cytokines including IL-4, IL-5, and IL-13 typically increase in allergic disease and have important IgE production and mucus secretion effects in addition to releasing a variety of inflammatory mediators.
Terpenes are known to have anti-allergic activities. Parthenolide, a sesquiterpene lactone isolated from Tanacetum parthenium exhibits anti-inflammatory and anti-allergic properties in vitro and in vivo (Miyata et al. 2008). Sesquiterpene lactones such as dehydroleucodine and xanthatin, isolated, respectively, from Artemisia douglasiana Besser and Xanthium cavanillesii Schouw as well as magnolialide from Laurus nobilis L. show anti-allergic activities in vitro (Penissi et al. 2009; Lee et al. 2013).
We previously reported that sesquiterpene lactons such as britanin and tomentosin isolated from Inulae flos have anti-inflammatory and anti-allergic effects (Park et al. 2013, 2014a, 2014b). However, the anti-asthma activity of britanin has not been investigated to our knowledge. In the present study, we investigated the effects of britanin on airway inflammation, and our findings suggest that britanin has a therapeutic potential for treating this inflammation.
Materials and methods
Chemicals
Britanin (Fig. 1) was isolated from Inulae flos as described (Park et al. 2013). In brief, Inulae flos was extracted with methanol followed by partition of different solvents, producing n-hexane, ethyl acetate, n-butanol, and water extracts. The ethyl acetate extract was repeatedly subjected to treatment with both silica gel and reverse-phase gel to afford the compound. The structure was elucidated as known compounds by comparison of their NMR spectra with the public values. The purity of britanin was 99.8 % based on HPLC analysis.
Animals and experimental protocol
Female BALB/c mice (6 weeks old, Koatech Co., Korea) were used with the approval of the animal care committee of the National Development Institute of Korean Medicine (Approval No. KOTMIN-2013-5). The induction of asthma in the model was described previously (Choi et al. 2010). Mice were sensitized on days 0 and 14 by intraperitoneal (i.p) administration of 20 μg/ml of ovalbumin (OVA, Sigma Chemicals, St. Louis, MO, USA) in PBS mixed with equal volumes of alum (1 mg) as an adjuvant in a total volume of 200 μl. On days 22–24, the mice were challenged by ultrasonic nebulization (Nebulizer, NE-U17, OMRON, Tokyo, Japan) using 1 % OVA in PBS or only PBS for 30 min. Britanin (5 or 10 mg/kg, brt5 and brt10) was administered orally once a day from days 22 to 24. Normal (PBS group) and OVA-induced positive control mice (OVA group) were treated orally with carboxymethyl cellulose. Reference groups were administered montelukast (Mont, 20 mg/kg, Cayman Chemicals, Ann Arbor, MI, USA) and dexamethasone (Dexa; 1 mg/kg, Sigma Chemicals).
Measurement of airway responsiveness
Airway responsiveness to aerosolized methacholine (MCh, Sigma Chemicals) was measured in conscious and unstrained mice 18 h after last OVA challenge by whole body plethysmography (Emka Technologies, Paris, France). Mice were stabilized in the chamber for 10 min and then exposed to aerosolized saline (1 min) as a control. Mice were then challenged every 20 min with aerosolized MCh. Increasing doses of aerosolized MCh were administered and enhanced pause (Penh) was measured over the subsequent 5 min as an index of airway obstruction.
Bronchoalveloar lavage fluid (BALF) analysis
1 day after Penh measurement, mice were anesthetized by i.p injection of rumpun and ketatol. A tracheal cannula was inserted in each mouse via a midcervical incision, and BALF obtained by washing the airway lamina two times with 0.5 ml of PBS. The cells were resuspended in 0.5 ml of PBS after removing the supernatant, BALF. The suspended cells were spun onto glass microscope slides (Shandon Cytospin 4, Thermo Scientific, Kalamazoo, MI, USA), each slide was air dried and then stained with a Diff-Quick staining (Sysmex, Kobe, Japan). The number of eosinophils was determined by counting at least 200 cells of leukocytes.
Quantification of serum IgE and cytokine
The levels of IL-4, IL-5, and IL-13 in BALF and cultured supernatants of splenocytes were quantified by enzyme immunoassays performed according to the manufacturer’s protocols (R&D Systems, Inc., Minneapolis, MN, USA) as described previously (Choi et al. 2010). Total serum IgE was measured using OptEIA™ mouse Ig ELISA Set (BD Biosciences, San Diego, CA, USA).
Lung tissue analysis
The lungs were removed and analyzed for histological analysis as previous described (Park et al. 2011). Briefly, lungs were fixed with 10 % (v/v) formaldehyde, sections of fixed paraffin lung tissues were cut to a thickness of 4 μm using a microtome, and then stained with hematoxylin and eosin (H&E) and periodic acid Schiff reagent (PAS). Peribronchial inflammation, eosinophil recruitment, and mucus secretion were assessed based on a five point scale by two independent examiners as previously described (Park et al. 2011).
Statistical analysis
Data were analyzed by one-way ANOVA followed by Dunnett’s multiple comparison tests. Results were represented as mean ± SEM and considered as statistical significance at p values < 0.05, 0.01, or 0.001.
Results
Inhibitory effects of britanin on AHR
To determine the effects of britanin on airway function in a murine asthma model, AHR to methacholine was examined. As shown in Fig. 2, OVA group showed a dose-dependent increase in airway hypersensitivity in response to methacholine compared with the PBS group, indicating the development of AHR in the OVA-induced mice, but the increase was significantly inhibited by britanin treatment. Treating mice with Mont also diminished the increased AHR and resulted in similar dose–response curves of airway hypersensitivity to that of the britanin with a slightly stronger effect than britanin’s. These results indicate that britanin administration effectively reduced the AHR in the murine asthma model.
Effect of britanin on airway hyperresponsiveness (AHR). AHR of in the PBS and OVA-induced mice was measured after exposure to increased concentrations of methacholine (Mch). The data are expressed as mean ± SEM. ##p < 0.01, ###p < 0.001 indicated statistically significant differences from the PBS group. **p < 0.01, ***p < 0.001 indicated statistically significant differences from the OVA group. PBS PBS-induced; OVA OVA-induced; Brt britanin; Mont montelukast
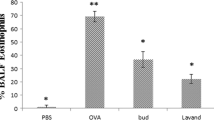
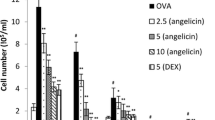
Inhibitory effects of britanin on OVA-induced increase in total cell and eosinophil numbers in BALF
Because one of the most important phenomena in asthma is leukocyte infiltration, especially eosinophils in the airway, leukocyte numbers and eosinophil percentages in BALF were measured. Figure 3a shows that the total number of leukocytes in the BALF of the OVA-induced lung tissues was significantly higher than that in the PBS group. This increased number of leukocytes was decreased by treating with britanin at the concentration of both 5 and 10 mg/kg. The eosinophil numbers in BALF were determined as a percentage of the total number of cells. Britanin treatment suppressed the percentage of eosinophils that were recruited into the airways of the OVA group (Fig. 3b). Treating the OVA group with Mont and Dexa also suppressed the total leukocyte filtration including eosinophils into their airway, indicating that britanin effectively inhibits cell infiltration into the OVA-induced mouse lung.
Effect of britanin on leukocyte infiltration. The cells in the BALF that was obtained from the mouse lungs were counted (a). The eosinophils after Diff-Quick staining were counted and expressed as a percentage of the total leukocytes (b). The data are expressed as mean ± SEM. ##p < 0.01, ###p < 0.001 indicated statistically significant differences from the PBS group. **p < 0.01, ***p < 0.001 indicated statistically significant differences from the OVA group. PBS PBS-induced; OVA OVA- induced; Brt britanin; Mont montelukast; Dexa dexamethasone
Suppressive effects of britanin on cytokine and IgE production
Airway inflammation is generally accompanied by the increased production of Th2 cytokines (IL-4, -5, and -13) that drive serum IgE production. First, the levels of IL-4, IL-5, and IL-13 in the BALF and the cultured splenocyte supernatants were determined using ELISA. The Th2 cytokines were significantly upregulated in the OVA-induced mice compared with the PBS group except for IL-4 in the BALF, and britanin treatment decreased the Th2 cytokine levels in both the BALF (Fig. 4a) and the splenocyte supernatants (Fig. 4b). However, the level of IFN-γ in the cultured splenocyte supernatant from the britanin-treated mice was not significantly different from that of cultures from the OVA-induced mice. Serum IgE levels were dramatically increased in the OVA group, but britanin treatment resulted in a significant decrease in the serum levels of IgE (Fig. 4c).
The effect of britanin on production of cytokines and serum IgE. The levels of cytokines in the BALF (a), the splenocyte supernatant (b), and the serum IgE (c) were determined using ELISA. The data are expressed as mean ± SEM. #p < 0.05, ##p < 0.01, ###p < 0.001 indicated statistically significant differences from the PBS group. *p < 0.05, **p < 0.01, ***p < 0.001 indicated statistically significant differences from the OVA group. PBS PBS-induced; OVA OVA-induced; Brt britanin; Mont montelukast; Dexa dexamethasone
Alleviated inflammation and mucus secretion in lung tissue
To examine the inhibitory effects of britanin on leukocyte infiltration and mucus secretion in the lungs of the OVA-induced asthma model, we stained lung sections using H&E and PAS staining solutions. As shown in Fig. 5a, dense infiltration of total leukocytes into the peribronchiolar and perivascular lesions of the lungs was observed in the OVA group. Lung tissues treated by britanin exhibited less leukocyte infiltration at both the 5 and 10 mg/kg doses. Lung tissues from asthmatic mice were also stained with PAS and showed clear mucus secretion within the bronchi when compared with the normal tissue (Fig. 5b). However, the mucus staining of the lung tissues was reduced in the britanin treated asthmatic mice. Therefore, britanin’s suppressing the increased infiltration of leukocytes and the mucus secretion reveals that britanin has inhibitory effects on airway inflammation.
Histological analysis of lung tissue. Lung tissues were fixed, and sections of PBS group, OVA group, and asthmatic mice treated with Brt, Mont, or Dexa were stained with H&E (a magnification ×200) or PAS (b magnification ×200). The cell infiltration and mucus production in the tissues were examined and categorized with scores (c). The data are expressed as mean ± SEM. ##p < 0.01, ###p < 0.001 indicated statistically significant differences from the PBS group. *p < 0.05, **p < 0.01 indicated statistically significant differences from the OVA group. PBS PBS-induced; OVA OVA-induced; Brt britanin; Mont montelukast; Dexa dexamethasone
Discussion
In previous studies, we demonstrated anti-inflammatory and anti-allergic activities in vitro as well as an anti-asthma effect of Inulae flos in vivo (Choi et al. 2010; Park et al. 2011; Lu et al. 2012). Furthermore, compounds isolated from Inulae flos were studied for their activity. Among them, britanin, a sesquiterpene lacton, was investigated in detail. It inhibits the production of inflammatory mediators including nitric oxide, prostaglandin E2 (PGE2), and pro-inflammatory cytokines in LPS-induced RAW 264.7 cells by suppressing NF-kB activation and MAP kinase signaling pathways (Park et al. 2013). In addition, the suppressive effects of britanin on mast cell-mediated inflammatory response were demonstrated in HMC-1 and bone marrow-derived mast cells (BMMC) (Lu et al. 2014; Park et al. 2014b). However, the anti-asthmatic mechanism of britanin has not been investigated to date. In this study, we demonstrated for the first time that britanin alleviated OVA-induced airway inflammation, likely because of decreased leukocyte infiltration, AHR, Th2 cytokines, IgE production, and mucus secretion in a mouse model of asthma.
Arachidonic acid metabolites including PGs and leukotrienes (LTs) play important roles in airway inflammatory disease. LTs, especially cysteinyl-LTs (cysLTs) have been demonstrated to cause infiltration of lung tissue with inflammatory cells and bronchoconstriction in asthma (Ismail et al. 2012; Liu and Yokomizo 2015). Zieuton that inhibits the synthesis of LTs has efficacy in asthma patients. Another asthma treatment is anti-LT receptor antagonist, Mont, which ameliorates airway bronchoconstriction and inflammation by reducing cysLTs generation (Nayak and Langdon 2007; Shimbori et al. 2011). We have already reported that britanin inhibited LTC4 generation by reducing cytosolic phospholipase A2α (cPLA2α) phosphorylation and the translocation of phospho-cPLA2α and 5-lipoxygenase to the nuclear membrane in BMMC (Lu et al. 2014). Since bronchial constriction correlates with the release of cysLTs (Dahlen et al. 1983), the reduced generation of LTC4 in vitro study could be one of explanations that britanin treatment significantly reduced AHR in a murine asthma model (Fig. 2), which suggests britanin’s possible role as a bronchodilator for asthma intervention.
It is generally accepted that Th2 cytokines play a vital role in asthmatic responses because IL-4 increases IgE production and IL-5 attributes eosinophil infiltration. Total leukocyte recruitment, including eosinophils, into the BALF of OVA-induced asthmatic mice was observed but inhibited by britanin treatment (Fig. 3), suggesting that britanin prevents inflammatory cell infiltration, especially eosinophils. Excessive Th2 cell activation results in allergic diseases such as asthma. In this study, we used the OVA-induced murine model of asthma to investigate the effect of britanin on Th2 cytokine secretion in BALF and in splenocyte supernatant. Britanin reduced IL-4, -5, and, -13 in BALF and cultured splenocytes (Fig. 4) compared with the OVA group. The reduced Th2 cytokine production in this experiment suggested low levels of serum IgE by regulating B cell class-switching (Fig. 4) as well as decreased leukocyte infiltration and mucus secretion into the lung tissue of asthmatic mice (Fig. 5). However, britanin did not affect the production of Th1 cytokines such as IFN- γ in splenocytes, indicating no effect of britanin on Th1 cells.
In the present study, we investigated the effect of britanin on OVA-induced airway inflammation. Britanin effectively reduced the productions of Th2 cytokines such as IL-4, IL-5, and IL-13 which are responsible for IgE production, eosinophil infiltration, and mucus hypersecretion in a murine asthma model. This inhibitory effect was observed in BALF and in cultured splenocytes at the protein levels, indicating that the reduced cytokine expression by britanin might have anti-asthmatic effects in vivo. Furthermore, the decreased leukocyte count and mucus secretion in lung tissue suggest that britanin might attenuate lung histopathological changes by decreasing Th2 cytokine levels in cultured splenocytes. It is worthy of notice that the effective concentration of britanin on anti-asthmatic activity in this study was low compared with the known LTRA, Mont. Although corticosteroids including Dexa are the most effective drug for allergic asthma, the medication is limited because of side effects. Thus, britanin could possibly be applied for anti-allergic diseases including asthma.
References
Baker KE, Bonvini SJ, Donovan C, Foong RE, Han B, Jha A, Shaifta Y, Smit M, Johnson JR, Moir LM (2014) Novel drug targets for asthma and COPD: lessons learned from in vitro and in vivo models. Pulm Pharmacol Ther 29:181–198
Choi JH, Park YN, Li Y, Jin MH, Lee J, Lee Y, Son JK, Chang HW, Lee E (2010) Flowers of Inula japonica attenuate inflammatory responses. Immune Netw 10:145–152
Dahlen SE, Hansson G, Hedqvist P, Bjorck T, Granstrom E, Dahlen B (1983) Allergen challenge of lung tissue from asthmatics elicits bronchial contraction that correlates with the release of leukotrienes C4, D4, and E4. Proc Natl Acad Sci USA 80:1712–1716
Ismail N, Jambari NN, Zareen S, Akhtar MN, Shaari K, Zamri-Saad M, Tham CL, Sulaiman MR, Lajis NH, Israf DA (2012) A geranyl acetophenone targeting cysteinyl leukotriene synthesis prevents allergic airway inflammation in ovalbumin-sensitized mice. Toxicol Appl Pharmacol 259:257–262
Kim YM, Kim YS, Jeon SG, Kim YK (2013) Immunopathogenesis of allergic asthma: more than the th2 hypothesis. Allergy Asthma Immunol Res 5:189–196
Kudo M, Ishigatsubo Y, Aoki I (2013) Pathology of asthma. Front Microbiol 4:263
Lee T, Lee S, Ho Kim K, Oh KB, Shin J, Mar W (2013) Effects of magnolialide isolated from the leaves of Laurus nobilis L. (Lauraceae) on immunoglobulin E-mediated type I hypersensitivity in vitro. J Ethnopharmacol 149:550–556
Liu M, Yokomizo T (2015) The role of leukotrienes in allergic diseases. Allergol Int 64:17–26
Lu Y, Li Y, Jin M, Yang JH, Li X, Chao GH, Park HH, Park YN, Son JK, Lee E, Chang HW (2012) Inula japonica extract inhibits mast cell-mediated allergic reaction and mast cell activation. J Ethnopharmacol 143:151–157
Lu Y, Li X, Park YN, Kwon O, Piao D, Chang YC, Kim CH, Lee E, Son JK, Chang HW (2014) Britanin suppresses IgE/Ag-induced mast cell activation by inhibiting the syk pathway. Biomol Ther 22:193–199
Miyata N, Gon Y, Nunomura S, Endo D, Yamashita K, Matsumoto K, Hashimoto S, Ra C (2008) Inhibitory effects of parthenolide on antigen-induced microtubule formation and degranulation in mast cells. Int Immunopharmacol 8:874–880
Nayak A, Langdon RB (2007) Montelukast in the treatment of allergic rhinitis: an evidence-based review. Drugs 67:887–901
Park YN, Lee YJ, Choi JH, Jin M, Yang JH, Li Y, Lee J, Li X, Kim KJ, Son JK, Chang HW, Kim JY, Lee E (2011) Alleviation of OVA-induced airway inflammation by flowers of Inula japonica in a murine model of asthma. Biosci Biotechnol Biochem 75:871–876
Park HH, Kim MJ, Li Y, Park YN, Lee J, Lee YJ, Kim SG, Park HJ, Son JK, Chang HW, Lee E (2013) Britanin suppresses LPS-induced nitric oxide, PGE2 and cytokine production via NF-kappaB and MAPK inactivation in RAW 264.7 cells. Int Immunopharmacol 15:296–302
Park HH, Kim SG, Kim MJ, Lee J, Choi BK, Jin MH, Lee E (2014a) Suppressive effect of tomentosin on the production of inflammatory mediators in RAW264.7 cells. Biol Pharm Bull 37:1177–1183
Park HH, Kim SG, Park YN, Lee J, Lee YJ, Park NY, Jeong KT, Lee E (2014b) Suppressive effects of britanin, a sesquiterpene compound isolated from Inulae flos, on mast cell-mediated inflammatory responses. Am J Chin Med 42:935–947
Penissi AB, Vera ME, Mariani ML, Rudolph MI, Cenal JP, de Rosas JC, Fogal TH, Tonn CE, Favier LS, Giordano OS, Piezzi RS (2009) Novel anti-ulcer alpha, beta-unsaturated lactones inhibit compound 48/80-induced mast cell degranulation. Eur J Pharmacol 612:122–130
Shimbori C, Shiota N, Okunishi H (2011) Effects of montelukast, a cysteinyl-leukotriene type 1 receptor antagonist, on the pathogenesis of bleomycin-induced pulmonary fibrosis in mice. Eur J Pharmacol 650:424–430
Szefler SJ (2011) Advancing asthma care: the glass is only half full! J Allergy Clin Immunol 128:485–494
Acknowledgments
This study was supported by a grant of the Traditional Korean Medicine R&D Project (HI13C0538), Ministry of Health & Welfare, Republic of Korea.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Sun-Gun Kim and Eujin Lee have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Kim, SG., Lee, E., Park, NY. et al. Britanin attenuates ovalbumin-induced airway inflammation in a murine asthma model. Arch. Pharm. Res. 39, 1006–1012 (2016). https://doi.org/10.1007/s12272-016-0783-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12272-016-0783-z