Abstract
Even though citalopram is commonly used in psychiatry, there are several reports on its toxic effects. So, the current study was designed to elucidate the mechanisms of cytotoxic effects of in vitro and in vivo citalopram treatment on liver and the following cytolethal events. For in vitro experiments, freshly isolated rat hepatocytes were exposed to citalopram along with/without various agents. To do in vivo studies liver function enzyme assays and histological examination were performed. In the in vitro experiments, citalopram (500 µM) exposure demonstrated cell death, a marked elevation in ROS formation, mitochondrial potential collapse, lysosomal membrane leakiness, glutathione (GSH) depletion and lipid peroxidation. In vivo biochemistry panel assays for liver enzymes function (AST, ALT and GGTP) and histological examination confirmed citalopram (20 mg/kg)-induced damage. citalopram-induced oxidative stress cytotoxicity markers were significantly prevented by antioxidants, ROS scavengers, MPT pore sealing agents, endocytosis inhibitors, ATP generators and CYP inhibitors. Either enzyme induction or GSH depletion were concomitant with augmented citalopram-induced damage both in vivo and in vitro which were considerably ameliorated with antioxidants and CYP inhibitors. In conclusion, it is suggested that citalopram hepatotoxicity might be a result of oxidative hazard leading to mitochondrial/lysosomal toxic connection and disorders in biochemical markers which were supported by histomorphological studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depression is a common dilapidating disorder in the world requiring long term treatment. Citalopram (1-[3-(Dimethylamino) propyl]-1-(4-fluorophenyl)-1,3-dihydroisobenzofuran-5-carbonitrile) as a selective serotonin reuptake inhibitor (SSRI) is one of the most prominent classes of antidepressants widely prescribed worldwide to counteract major depressive disorders and anxiety problems (Wagner et al. 2014). Despite the favorable safety profile, hepatotoxicity is documented as an adverse effect during citalopram clinical use which is concomitant with marked elevation of liver function enzymes as well as hepatocellular and cholestatic liver injury (Milkiewicz et al. 2003; López-Torres et al. 2004; Solomons et al. 2005). It was shown that citalopram induced dose dependently fatty infiltration in the liver of experimental animals (Overø and Svendsen 1978). Although citalopram is recommended for the treatment of depression during pregnancy and lactation, it causes detrimental effect in rat fetus liver (Mohammadi et al. 2013). Moreover, citalopram represents cytotoxic effects in various cell lines in vitro and activates apoptotic machinery (Xia et al. 1999a). There is evidence of oxidative tissue damages in rat liver, kidney and heart after citalopram intake (Abdelmajeed 2009). Besides, citalopram at the recommended human doses is genotoxic after long-term treatment in germ cells with the involvement of oxidative pathway (Attia and Bakheet 2013). Upon absorption, citalopram undergoes hepatic metabolism via the cytochrome P450 enzymes mainly CYP2C19, 3A4 and 2D6, which in turn increases drug toxicity suggesting the possible role of metabolites in citalopram -associated hepatotoxicity (Overø and Svendsen 1978).
Elevated reactive oxygen species (ROS) formation, which is accompanied by the augmented risk of tissue damage and organ dysfunction, has a leading role in environmental agents, chemicals and/or drugs- induced cytotoxicity (Jaeschke et al. 2012). Furthermore, ROS generation is a primary event which activates various downstream signaling pathways contributed to cellular proteins and DNA damages as well as subcellular organelles such as endoplasmic reticulum, mitochondria and lysosomes (Bayir and Kagan 2008; Ahmadian et al. 2015). Mitochondria, as the cellular powerhouse play a decisive role in producing energy supplies, initiating apoptosis and interfering with intracellular signaling pathways. Besides, mitochondria are amongst the possible targets for drug/xenobiotic-induced damages with different mechanistic hypotheses, one of which is the increased generation of free radicals (Eftekhari et al. 2015). As a result, mitochondrial function disturbance or abnormality might terminate in cell dysfunction or death. Antidepressants-induced mitochondrial dysfunction has been addressed in a number of studies (Xia et al. 1999b; Abdel-Razaq et al. 2011). Lysosomes due to their natural function of degrading and recycling an extensive range of macromolecules encompass hydrolytic enzymes including nucleases, proteases and lipases which on liberation can also digest cellular contents and exhibit deleterious effects (Luzio et al. 2007). Oxidative stress has a fundamental role in increasing lysosomal membrane permeability (LMP) leading to cellular necrosis or apoptosis ultimately (Boya and Kroemer 2008). Medications have also emerged as the executioners of cell death through damaging lysosomal membrane via producing reactive species (Pourahmad et al. 2012a). Antioxidants have gained clinical prominence in mitigation of cellular damages induced by various kinds of drugs and/or xenobiotics (Lim et al. 2013; Yun et al. 2015).
However, the potential cytotoxic impact of citalopram on hepatocytes and the underlying mechanisms of toxicity have not been fully investigated so far. Hence, the present study attempted to evaluate potential cytotoxicity of citalopram in isolated rat hepatocytes using accelerated cytotoxic mechanism screening (ACMS) technique and to outline the consequences of molecular mechanisms involved in the citalopram-induced hepatotoxicity, particularly the role of oxidative stress, the involvement of subcellular organelles and possible role of citalopram reactive metabolites in freshly isolated rat hepatocytes and also in and in vivo rat model. Also, the protective role of antioxidants, ROS scavengers, MPT pore sealing agents, endocytosis inhibitors, ATP generators and CYP inhibitors against citalopram-induced liver damage were examined in order to suggest strategies for prevention and treatment of adverse effects caused by citalopram in different organs.
Methods and materials
Chemicals
Cimetidine was purchased from Medisca Pharmaceutique Inc (Montreal, Canada). Thiobarbituric acid (TBA) was purchased from Serva (Heidelberg, Germany). Albumin bovine serum was purchased from the Roche diagnostic corporation (IN). 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) and oxidized glutathione (GSSG) were obtained from Acros (New Jersey, USA). N-acetyl cysteine, taurine, quercetin, citalopram and all other reagents were obtained from Sigma-Aldrich Chemical Co. (St. Louis, USA). The kit for alanine aminotransferase (ALT), aspartate aminotransferase (AST) and Gamma glutamyl transferase (GGT) analysis were obtained from Pars Azmun Company (Tehran, Iran).
Animal Treatment and Hepatocyte Preparation
Sprague–Dawley rats with the average weight of 200–250 g were housed in standard cages with normal chew food and tap water available ad libitum in a laboratory with adjusted ambient temperature (21–23 °C) and under a 12 h light–dark cycle obtained from the animal research center of Tabriz University of Medical Science, Tabriz, Iran.
The study protocol was designed and approved by the Ethics Committee for the Use of Animals in Research at Tabriz University of Medical Sciences (No: 91/2-2/5/4 Dec 2012).
Rat hepatocytes isolation was carried out with collagenase-perfusion method as described previously (Heidari et al. 2014a). The isolated hepatocytes in a density of 106/ml were then suspended in the Krebs-Henseleit buffer (pH = 7.4) in continuously rotating round bottom flasks supplemented with 12.5 mM HEPES, in a 37 °C water bath under an atmosphere of carbogen gas (95 % O2 and 5 % CO2) (Eghbal et al. 2004). Chemical addition was done 30 min after the adaptation period of hepatocytes to the incubation medium. The optimum effective dose to provide appropriate protection was evaluated to be 500 µM for quercetine and 200 µM for N-acetyl cysteine (NAC) and taurine. The doses of ROS scavengers (α-tocopherol succinate and butylated hydroxytoluen (BHT)), ATP generators (fructose and l-glutamine), MPT pore sealing agents (carnitine and trifluoperazine), endocytosis inhibitors (chloroquine and methylamine), autophagy inhibitor (3-methyladenine) and CYP450 inhibitors (4-methylpyrazole and cimetidine) were selected from parallel investigations that were conducted on freshly isolated rat hepatocytes (Heidari et al. 2013; Eftekhari et al. 2015). Also, we examined these concentrations in our laboratory conditions and obtained that they have maximal inhibitory effects on the cytotoxicity markers (data not shown). Glutathione (GSH)-depleted hepatocytes were prepared by preincubation of hepatocytes with 200 µM 1-bromoheptane for 30 min as described by (Khan and O’Brien 1991).
CYP450-inhibited hepatocytes were prepared by adding cimetidine and/or 4-methylpyrazole 30 min before citalopram to flasks (Jamshidzadeh et al. 2007) and CYP450 s were induced by intraperitoneal injection of β-naphtoflavone (80 mg/kg) and/or phenobarbital (10 mg/kg) for 3 days before hepatocyte isolation (Heidari et al. 2014a).
Cell viability
Hepatocyte viability was determined using a hemocytometer with trypan blue (0.1 %w/v) exclusion test microscopically (Eghbal et al. 2004). Sampling was performed every 60 min during a 3 h of incubation period.
Reactive oxygen species (ROS) formation assay
To assess the amount of hepatocyte ROS generation during citalopram metabolism, 1.6 μM of 2.7-dichlorofluorescein diacetate (DCFH-DA) was added to hepatocytes as it infiltrates hepatocytes and is hydrolyzed to non-fluorescent dichlorofluorescein (DCF) by an intracellular esterase. The latter in the presence of ROS commences a reaction and turns into a highly fluorescent, dichlorofluorescin. In 15, 30, and 60 min time points over isolation, 1 mL (106 cell) of hepatocytes suspension was picked up and centrifuged at 3000g for 1 min. Fluorescence intensity per 106 cells as a result of ROS production was measured using a Jasco R_FP-750 spectrofluorometer (Jasco Corporation, Tokyo, Japan) with excitation and emission wavelengths of 500 and 520 nm, respectively (Heidari et al. 2013).
Measurement of lipid peroxidation (LPO)
Disintegration of lipids with hydroperoxidase was evaluated through measuring thiobarbituric acid reactive substances (TBARS). Briefly, 1 mL of hepatocytes suspension was treated with 250 μL trichloroacetic acid (TCA 70 % w/v) and centrifuged at 3000g for 15 min; then 1 mL of thiobarbituric acid (TBA 0.8 % w/v) was added to supernatant and boiled for 20 min. The absorbance was determined at 532 nm in an Ultrospec® 2000 UV spectrophotometer (Eghbal et al. 2014).
Mitochondrial membrane potential assay
The accumulation of the cationic dye, rhodamine 123 in intact mitochondria was used to estimate mitochondrial membrane potential (MMP). When MMP is altered by any xenobiotic, the facilitated diffusion of dye is diminished leading to the accretion of the amount of rhodamine 123 in media. At the given times, aliquots of 1 mL samples of the cell suspension were taken and centrifuged at 1000g for 1 min. Then the cell pellet was resuspended in 2 mL of fresh incubation medium containing 1.5 μM of rhodamine 123 and incubated at 37 °C in a water bath with a gentle shaking. Hepatocytes were separated by centrifugation at 3000g for 1 min and the amount of rhodamine 123 remaining in the incubation medium was calculated using a Jasco FP-750 fluorescence spectrophotometer set at 490 nm excitation and 520 nm emission wavelengths (Taziki et al. 2013a).
Determination of intracellular GSH and GSSG
Glutathione (GSH) and glutathione disulfide (GSSG) content in isolated hepatocytes were determined in deproteinized samples (5 % metaphosphoric acid) after derivatization with iodoacetic acid and 1-fluoro-2,4-dinitrobenzene (FNDB), according to the HPLC method (Reed et al. 1980), using a µBondapak NH2 column (Water Associates, Milford, MA). In brief, 0.8 mL of the cell suspension was spun at 50 g for 40 s, and the cell pellet was resuspended in 0.8 mL of fresh Krebs-Hensleit medium. The cell suspension was deproteinized with 0.2 mL volume of 25 % metaphosphoric acid and then was centrifuged at 100 g for 5 min. The mixture of 0.5 mL of supernatant and 0.05 mL of iodoacetic acid in the presence of excess sodium bicarbonate was sealed and left in the dark and room temperature for 1 h. Ultimately, 0.5 mL of FDNB solution (1.5 %, v/v in ethanol) was added to the sample, left in the dark for 24 h at room temperature and then was analyzed by HPLC (Eghbal et al. 2004).
Lysosomal membrane integrity assay
The redistribution of fluorescent dye, acridine orange was used to evaluate the hepatocyte lysosomal membrane stability (Eftekhari et al. 2015). To do the experiment, 0.5 mL of the cell suspension which was previously stained with acridine orange (5 µM) was separated from the incubation medium by 1 min centrifugation at 800 g. Afterwards, the cell pellet was resuspended in 2 mL of fresh incubation buffer. The washing process was performed twice to remove the fluorescent dye from the media. The distribution of dye in the cell suspension was then determined fluorimetrically using a Jasco FP-750 fluorescence spectrophotometer set at 495 nm excitation and 530 nm emission wavelengths.
Microscopic assessment of lysosomal membrane integrity
After attaching hepatocytes to glass cover slips 5 mg/ml acridine orange was used to stain hepatocytes for 2 min at 37 °C. In the next step, hepatocytes were rinsed with buffer and 500 µM citalopram was added. The acridine orange induced granular green (lysosomal) fluorescence from 50 cells in each experimental group was then measured at 10 min intervals on fluorescence microscope (Olympus BX50) using excitation light (800× magnification) under the microscope (Pourahmad et al. 2012a).
Animals experiment
Rats were randomly divided into seventeen groups of five animals. The treatments were as follows: Group 1 (control): vehicle (0.9 % saline solution) only. Group2: 20 mg/kg citalopram (PO dissolved in 0.9 % saline), Group 3: 20 mg/kg citalopram + BSO (1 g/kg, i.p), Group 4: 20 mg/kg citalopram + BSO (1 g/kg) + NAC (400 mg/kg, PO), Group 5: 20 mg/kg citalopram + BSO (1 g/kg) + taurine (400 mg/kg, PO), Group 6: 20 mg/kg citalopram + BSO (1 g/kg) + quercetine (400 mg/kg, PO). Group 7: β-naphtoflavone-induced animals (80 mg/kg, i.p) + 20 mg/kg citalopram, Group 8: β-naphtoflavone-induced animals + 20 mg/kg citalopram + NAC (400 mg/kg), Group 9: β-naphtoflavone-induced animals + 20 mg/kg citalopram + taurine (400 mg/kg), Group 10: β-naphtoflavone-induced animals + 20 mg/kg citalopram + quercetine (500 mg/kg). Group 11: Phenobarbital-induced animals (10 mg/kg) + 20 mg/kg citalopram. Group 12: Phenobarbital-induced animals + 20 mg/kg citalopram + NAC 300 mg/kg, Group 13: Phenobarbital-induced animals + 20 mg/kg citalopram + taurine (400 mg/kg), Group 14: Phenobarbital-induced animals + 20 mg/kg citalopram + quercetine (500 mg/kg). There was no significant differences between groups; 15 (BSO-treated animals), 16 (β-naphtoflavone-induced animals), and group 17 (Phenobarbital-induced animals), and the control (vehicle-treated) animals in the parameters evaluated in the experiment. Buthionine sulfoximine (BSO) (1 g/kg) administration is cited as a model for hepatic glutathione depletion (Heidari et al. 2014b). One hour later after BSO-treatment, animals were given citalopram (20 mg/kg). The amount of liver GSH level was measured 5 h after citalopram intake to verify the impact of BSO on GSH depletion. Food was removed at 15 h before dosing with BSO and supplied again at 2 h after citalopram administration. Antioxidant administration was performed 0.5 h before citalopram gavage.
Serum alanine transaminase (ALT) aspartate aminotransferase (AST) and Gamma Glutamyl Transferase (GGT) activities were measured with a commercial kit (Pars Azmun Company, Tehran, Iran). To assess the histopathological changes, paraffin-embedded liver sections were stained with heamotoxyline and eosine (H&E) before light microscopy. An HPLC method was used to evaluate the amount of GSH in rat liver as previously reported (Yoshida 1996). Briefly, liver tissue samples (100 mg) were homogenized in the presence of 3 mL 10 mM EDTA and 50 mM NaClO4 0.1 % H3PO4 buffer. Separation of GSH from excised livers was performed using a Spherisorb ODS2 column (4.6 × 250 mm, 5 µm, waters, Ireland) and 50 mM NaClO4 0.1 % H3PO4 as the mobile phase with the flow rate of 1 ml min−1, detected GSH at the wavelength of 215 nm (Yilmaz et al. 2009). LPO pace was measured to evaluate the extent of lipid membrane damage induced by citalopram in various experimental groups as reported previously (Uchiyama and Mihara 1978).
Statistical analysis
The results are presented as the Mean ± SEM for at three independent experiments. Statistical analysis for the control and experimental groups was done by a one-way analysis of variance (ANOVA) followed by Tukey’s post hoc test to evaluate significance. Results with values of p < 0.05 were considered statistically significant.
Results
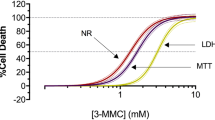
Cytotoxicity caused by citalopram
Control cell groups of isolated rat hepatocytes were at least 80–90 % viable during the incubation period. To avoid either nontoxic or very toxic amounts in this investigation, we used LC50concentrations for citalopram. According to the ACMS technique, the LC50 of a chemical in hepatocytes is identified as the concentration at which cell viability plunges in number to the 50 % following the 2 h of incubation. In order to determine this value for citalopram, dose–response curves were plotted and the LC50 was established based on a regression plot of three different concentrations (data not shown). This amount for citalopram was evaluated to be 500 µM in isolated rat hepatocytes which was applied for the assessment of other biochemical markers of toxicity in hepatocytes. Hepatotoxicity due to membrane intactness was considered through trypan blue exclusion assay. As demonstrated in Table 1, citalopram (500 µM) obviously increased cell death compared to control hepatocytes. Co-treatment of hepatocytes with antioxidants NAC, quercetin and/or taurine was concurrent with significant reduction of citalopram-induced membrane lysis (Table 1). Furthermore, citalopram-induced cytotoxicity was considerably inhibited by ROS scavengers (α-tocopherol succinate and/or BHT), ATP generators (fructose and/or l-glutamine), MPT pore sealing agents (carnitine and/or trifluoperazine), endocytosis inhibitors (chloroquine and/or methylamine), autophagy inhibitor (3-methyladenine) as well as CYP450 inhibitors (4-methylpyrazole and cimetidine) (Table 1). Depletion of hepatocytes GSH reservoirs with 1-bromoheptane beforehand, increased citalopram-induced cell death (Table 1). citalopram-induced cytotoxicity rocketed in hepatocytes whose CYP450 s were induced with either β-naphtoflavone or phenobarbital (CYP450 enzyme inducers) (Figs. 1, 2), in which CYP450 inhibitors (4-methylpyrazole and/or cimetidine) and/or antioxidants (NAC, quercetin and/or taurine) markedly diminished the effect of enzyme induction on augmentation of citalopram-associated cell death (Figs. 1, 2).
The effect of cimetidine, 4-methylpyrazole (a) and N-acetylcysteine, quercetine, taurine (b) on β-naphtoflavone (βNF) and citalopram (CIT)-induced cytotoxicity toward isolated rat hepatocytes. Isolated rat hepatocytes (106 cells/mL) were incubated at 37 °C in rotating round bottom flasks in Krebs-Henseleit buffer (pH 7.4). Data are shown as Mean ± SEM for at least three separate experiments. aSignificantly higher than control group (p < 0.05). bSignificantly higher than CIT-treated animals (p < 0.05). cSignificantly lower than βNF-induced animals which were treated with CIT (p < 0.05)
The effect of cimetidine, 4-methylpyrazole (a) and N-acetyl cysteine, quercetine, taurine (b) on phenobarbital (PB) and citalopram (CIT)-induced cytotoxicity toward isolated rat hepatocytes. Isolated rat hepatocytes (106 cells/mL) were incubated at 37 °C in rotating round bottom flasks in Krebs-Henseleit buffer (pH 7.4). Data are shown as Mean ± SEM for at least three separate experiments. aSignificantly higher than control group (p < 0.05). bSignificantly higher than CIT-treated animals (p < 0.05). cSignificantly lower than βNF-induced animals which were treated with CIT (p < 0.05)
All of the aforementioned antioxidants, radical scavengers, endocytosis inhibitors, autophagy inhibitor, CYP450 inhibitors and/or 1-bromoheptan (GSH depletory agent) did not have any significant impact on hepatocyte membrane intactness and other toxicity evaluation assays at concentrations utilized during solitary incubation in rat hepatocytes (data not shown).
The effects of citalopram on ROS formation
Incubation of hepatocytes with citalopram at the LC50 for 2 h (500 µM), led to a significant rise in ROS generation compared to the control cells. Antioxidants (NAC, quercetine and/or taurine), ROS scavengers (α-tocopherol succinate and/or BHT), ATP generators (fructose and/or l-glutamine), MPT pore sealing agents (carnitine and/or trifluoperazine), endocytosis inhibitors (chloroquine and/or methylamine), autophagy inhibitor (3-methyladenine) and/or CYP450 inhibitors (4-methylpyrazole and/or cimetidine) markedly impeded citalopram-induced ROS formation. In GSH depleted rat hepatocytes an increase of the citalopram-induced ROS formation (Table 2) was observed.
The effects of citalopram on lipid peroxidation
To investigate the role of citalopram in inducing LPO in isolated rat hepatocytes, the amount of TBARS was estimated. We came up with the results that citalopram induces noticeable LPO in isolated rat hepatocytes while antioxidants (NAC, quercetine and/or taurine), ROS scavengers (α-tocopherol succinate and/or BHT), ATP generators (fructose and/or l-glutamine), MPT pore sealing agents (carnitine and/or trifluoperazine), endocytosis inhibitors (chloroquine and/or methylamine), autophagy inhibitor (3-methyladenine) and/or CYP450 inhibitors (4-methylpyrazole and/or cimetidine) plummeted the citalopram-induced TBARS formation significantly (Table 3). Also, GSH depletion resulted in an upward trend in citalopram-induced LPO (Table 3).
The effects of citalopram on mitochondrial membrane potential
As shown in Table 4, citalopram (500 µM) resulted in mitochondrial membrane potential collapse during 1 h of incubation period. Mitochondrial membrane potential collapse is a crucial parameter of mitochondrial toxicity in all mitochondrial destructing pathways. The latter toxicity was inhibited by antioxidants (NAC, quercetine and/or taurine), ROS scavengers (α-tocopherol succinate and BHT), ATP generators (fructose and l-glutamine), MPT pore sealing agents (carnitine andtrifluoperazine), endocytosis inhibitors (chloroquine and methylamine), autophagy inhibitor (3-methyladenine) and CYP450 inhibitors (4-methylpyrazole and cimetidine) substantially. GSH depletion led to more severe mitochondrial membrane collapse following citalopram (500 µM) treatment (Table 4).
The effects of citalopram on GSH/GSSG levels
As illustrated in Tables 5, 6, treatment of hepatocytes with citalopram (500 µM) promptly depleted hepatocyte GSH pools, which mostly was in association with GSSG production. In addition, incubation of hepatocytes with antioxidants (NAC, quercetine and/or taurine) ROS scavengers (α-tocopherol succinate and/or BHT), ATP generators (fructose and/or l-glutamine), MPT pore sealing agents (carnitine and/or trifluoperazine), endocytosis inhibitors (chloroquine and/or methylamine), autophagy inhibitor (3-methyladenine) and/or CYP450 inhibitors (4-methylpyrazole and/or cimetidine) significantly prohibited both the citalopram-induced GSH decrease and GSSG rise suggesting the occurrence of oxidative stress after citalopram administration (Tables 5, 6).
Citalopram: induced lysosomal membrane damage
The extent of lysosomal membrane damage was stated through the redistribution of the fluorescent dye acridine orange which has a great tendency to accumulate in the lysosomes, to the cytoplasmic space. Treatment of hepatocytes with citalopram significantly injured lysosomes in 60 min time period which was countered by antioxidants antioxidants (NAC, quercetine and/or taurine) ROS scavengers (α-tocopherol succinate and/or BHT), ATP generators (fructose and/r l-glutamine), MPT pore sealing agents (carnitine and/or trifluoperazine), endocytosis inhibitors (chloroquine and/r methylamine), autophagy inhibitor (3-methyladenine) and/or CYP450 inhibitors (4-methylpyrazole and/or cimetidine), while preceding GSH depletion elevated the liberation of acridine orange into the cytosol dramatically (Table 7). Additionally, fluorescence micrographs of acridine orange-loaded hepatocytes showed loss of granular green fluorescence and increment of nuclear and cytosolic fluorescence from the same hepatocytes at about 30 min upon the addition of 500 µM citalopram (Fig. 3).
a Fluorescence micrograph of acridine orange loaded hepatocytes before addition of 500 µM citalopram demonstrated clear granular green fluorescence representing accumulation of fluorescent dye inside the lysosomes (800× magnification). b Fluorescence micrograph of the same acridine orange loaded hepatocytes established loss of granular green fluorescence and increase of nuclear and cytosolic fluorescence at about 60 min following the addition of 500 µM citalopram
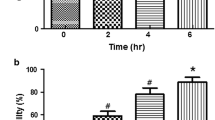
Animal experiments results
The present research interrogated the effect of citalopram treatment (20 mg/kg) (Abdelmajeed 2009) in addition to in vitro experiments in isolated rat hepatocytes. Liver function tests and histopathological evaluation were performed in order to follow up the extent of citalopram-induced liver damage. Serum ALT level as the prominent indicator of hepatotoxicity was measured at various time points subsequent to citalopram administration. As Fig. 4 represents, the highest level of ALT was observed after 5 h of citalopram treatment and then started to fall back again gradually within the next 24 h. So, we provided a framework to do all other experiments 5 h after citalopram administration to the animals.
Serum ALT levels after citalopram (20 mg/kg) administration to rat. The peak serum ALT level was observed at 5 h after citalopram administration. Uptight arrow: Control (vehicle-treated) animals. Filled circle: citalopram-treated animals. Data are expressed as Mean ± SEM for at least five animals. *Significantly higher than control levels (p < 0.05)
As Table 8 illustrates, citalopram (20 mg/kg) resulted in marked elevation of ALT compared to the control group, suggesting the possible damaging effect of citalopram in the liver. To determine if the generation of reactive metabolites has contributed to citalopram-induced hepatotoxicity, the effect of enzyme induction with β-naphtoflavone and phenobarbital was investigated using the serum ALT level as an indicator. Citalopram caused a significant increment in serum ALT in enzyme induced animals (Table 8). NAC, quercetine and/or taurine administration effectively attenuated ALT level in enzyme-induced rats which were treated with citalopram (Table 8).
Hepatic glutathione (GSH) content was depleted with BSO (Drew and Miners 1984), to investigate the impact of the glutathione reservoirs and their fundamental defense mechanism in xenobiotic/drug induced liver injuries. GSH-depleted group showed a dramatic increase in serum ALT level, while NAC, quercetine and/or taurine administration significantly decreased ALT surge both in BSO-treated and intact group receiving citalopram (Table 9). Furthermore, similar results were obtained at the level of serum AST and GGT as other markers of liver function in Tables 8, 9. To verify the results of Table 9 we measured the effect of BSO on hepatic GSH level 5 h after citalopram treatment. (Fig. 5).
The effect of BSO administration on citalopram (CIT)-induced glutathione (GSH) content reduction in rat and the effect of NAC, quercetine and taurine. BSO L-buthionine sulfoximine; NAC N-acetyl cysteine. Data are expressed as Mean ± SEM for at least five animals. aSignificantly lower than control (p < 0.05). bSignificantly lower than BSO-control (p < 0.05). cSignificantly higher than BSO-administrated animals which were treated with citalopram (p < 0.05)
Since it was founded from this experiment that GSH reservoir depletion led to higher magnitude of citalopram-related liver damage, hepatic GSH level was assessed with HPLC technique. Citalopram (20 mg/kg) administration reduced GSH contents compared to control vehicle receiving group. Also, in enzyme-induced animals treated with citalopram the GSH level was significantly lower than that in enzyme-induced controls (Fig. 6). These outcomes indicate that citalopram metabolites contribute to the citalopram-induced liver damage. The application of antioxidants NAC, quercetine and/or taurine bounced back the levels of GSH in β-naphtoflavone and phenobarbital induced rats significantly.
The effect of enzyme induction on citalopram (CIT)-induced glutathione (GSH) content reduction in rat. Data are expressed as Mean ± SEM for at least five animals. aSignificantly lower than β-naphtoflavone control (p < 0.05). bSignificantly lower than phenobarbital control (p < 0.05). cSignificantly higher than β-naphtoflavone-induced animals which were treated with citalopram (p < 0.05). dSignificantly higher than phenobarbital-induced animals which were treated with citalopram (p < 0.05)
Our results revealed that citalopram caused an increase in TBARS in rat liver, which indicates the occurrence of LPO. Enzyme induction with β-naphtoflavone and/or phenobarbital exacerbated peroxidation of hepatic lipids, whereas NAC, quercetine and/or taurine alleviated the production of TBARS in enzyme induced groups treated with citalopram (Fig. 7). Besides, the LPO was more severe in GSH-depleted animals. NAC, quercetine and/or taurine administration exerted protective role in intact or BSO-depleted rats (Fig. 8).
The effect of enzyme induction on citalopram (CIT)-induced lipid peroxidation in rat liver. Data are expressed as Mean ± SEM for five animals. aSignificantly higher than β-naphtoflavone control (p < 0.05). bSignificantly higher than phenobarbital control (p < 0.05). cSignificantly lower than β-naphtoflavone-induced animals which were treated with citalopram (p < 0.05). dSignificantly lower than phenobarbital-induced animals which were treated with citalopram (p < 0.05)
Citalopram (CIT)-induced lipid peroxidation: the role of glutathione reservoirs and the effect of NAC quercetine and taurine administration. BSO l-buthionine sulfoximine; NAC N-acetyl cysteine. Data are given as Mean ± SEM for five animals. aSignificantly higher than control animals (p < 0.05). bSignificantly higher than citalopram-treated animals (p < 0.05). cSignificantly lower than citalopram-treated animals (p < 0.05). dSignificantly lower than citalopram-treated animals which were depleted of glutathione (p < 0.05)
The study of the histopathological changes following citalopram administration revealed a mild inflammatory cell infiltration compared to control group which were mainly lymphocytes (Fig. 9b). The impact of enzyme-induction on rat liver histopathology was studied. From the histopathological point of view, in enzyme-induced animals treated with citalopram, hepatocellular single-cell necrosis and inflammatory cells infiltration was occurred (Fig. 9c, d). The protective effects of NAC, quercetine and/or taurine against citalopram-associated hepatotoxicity and their role in alleviating pathologic lesions were evident in this experiment (Fig. 9e–j).
Effect of enzyme-induction on rat liver histopathological changes, induced by citalopram (20 mg/kg). a normal control, b citalopram (20 mg/kg), c βNF-induced + citalopram (20 mg/kg), d phenobarbital-induced + citalopram (20 mg/kg), e βNF-induced + citalopram (20 mg/kg) + NAC (400 mg/kg), f phenobarbital-induced + citalopram (20 mg/kg) + NAC (400 mg/kg), g βNF-induced + citalopram (20 mg/kg) + quercetine (500 mg/kg), h Phenobarbital-induced + citalopram (20 mg/kg) + quercetine (500 mg/kg), i βNF-induced + citalopram (20 mg/kg) + taurine (400 mg/kg), j phenobarbital-induced + citalopram (20 mg/kg) + taurine(400 mg/kg). When enzyme-induced animals were treated with citalopram single cell necrosis of liver parenchymal cells and inflammatory cells (mainly lymphocytes) infiltration were occurred (c and d), alleviation of citalopram-induced alterations in enzyme-induced animals was observed by NAC, quercetine and taurine administration, which diminished necrosis and inflammatory cells infiltration (e–j). (Yellow arrows show single cell necrosis. Black arrows show infiltrated lymphocytes)
Discussion
Drug-induced liver injury has engendered fear and apprehension in medicine, being one of the most important reasons of drug withdrawal. Long term drug use in depression has been implicated with various kinds of adverse drug effects. Literature search has fetched with clinical manifestations of citalopram-induced hepatotoxicity (Guerra et al. 2014; Voican et al. 2014) but the exact cellular and molecular mechanism has not been exclusively cleared yet. Hence, in the present experiment we evaluated the potential hepatotoxic effect of citalopram in vitro in isolated rat hepatocytes and also in vivo. Regarding the in vitro assays, we used ACMS technique with freshly isolated rat hepatocytes to explore the mechanisms of citalopram-associated toxicity and plausible protective effects of antioxidants and the selected inhibitors. This technique is useful and important in determining the cytotoxic effects of a drug or xenobiotics in freshly isolated rat hepatocytes over two to 3 h. A major advantage of ACMS is that a high dose/short duration (2–3 h) exhibits the same hepatotoxicity in vitro as would do a low dose/long duration (24–48 h) in vivo (O’Brien and Siraki 2005). In other words, this method could be utilized to characterize and anticipate hepatotoxicity in vivo. The outcome of our study revealed that citalopram induces liver cell damage (cytotoxicity) and oxidative stress in isolated rat hepatocytes. Oxidative stress, imbalance between the generation and elimination of ROS, is not only implicated in the pathophysiology of depression, but also in detrimental impacts of the antidepressant agents (Taziki et al. 2013b). Targeting cellular key components including DNA, lipids and proteins damage cells in consequence of drug-induced oxidative stress. As ROS generation was markedly increased after hepatocytes treatment with citalopram, our study is the first to demonstrate a direct connection between citalopram-induced cytotoxicity and ROS overproduction in isolated rat hepatocytes with ACMS method. The protective role of various antioxidants against drug/xenobiotic-induced hepatotoxicity has been addressed in many studies such as NAC, taurine and quercetine (Heidari et al. 2014a). These protective functions of the aforementioned antioxidants are in accord with our study in citalopram-induced oxidative damage in rat hepatocytes.
Citalopram is metabolized by the hepatic cytochrome P450 system mainly via CYP2C19, CYP3A4, and CYP2D6 (von Moltke et al. 1999).The role of metabolic pathways and reactive intermediates in citalopram-induced hepatotoxicity was determined by examining the impact of this agent in enzyme-induced rats. β-naphtoflavone induces various CYP enzymes, mainly CYP1A family (Chatuphonprasert et al. 2011). Besides, phenobarbital causes different types of CYP enzyme induction such as CYP1A, CYP2A, CYP2B, and CYP3A (Pelkonen et al. 1998). Involvement of a wide range of metabolic enzymes with these agents makes it challenging to differentiate between specific enzymes which are involved in citalopram metabolism. For this reason, more studies are required to elucidate the role of the precise CYP and/or other enzymes, which are in charge of converting citalopram to its reactive metabolites.
In this experiment, initiation of LPO was also observed in rat hepatocytes exposed to citalopram. The mentioned effects were prevented by antioxidants and/or free radical scavengers, which stringently propose the participation of ROS and oxidative stress in the cytotoxicity mechanism of citalopram in hepatocytes. In hepatocytes, ROS derives from CYP 2E1 while in Kupffer cells is the result of NADPH oxidase activation (Siegmund and Brenner 2005). CYP2E1 is a drastic enzyme for ROS generation and is one the most dominant inducers of oxidative stress in liver cells. In this study citalopram-induced ROS formation was protected by inhibitor of CYP2E1 (4-methylpyrazole) representing the role of cytochrome P450 as a source of citalopram-induced ROS production and its subsequent cytotoxic events. Attenuated cellular death, ROS formation and also LPO with CYP2E1 inhibitor (4-methylpyrazole), ATP generators (fructose and/or l-glutamine), MPT pore sealing agents (carnitine and/or trifluoperazine), endocytosis inhibitors (chloroquine and/or methylamine) and/or autophagy inhibitor (3-methyladenine) provides the evidence of mitochondrial and lysosomal involvement in citalopram-mediated oxidative damage and its subsequent cytotoxic events.
Another objective of this study was to assess the role of GSH in citalopram -associated oxidative stress in hepatocytes. Glutathione exists in the reduced (GSH) and disulfide oxidized (GSSG) forms which can convert to each other. Oxidative stress reduces the amount of GSH while elevated GSSG is an indicator of toxicity (Zitka et al. 2012). Citalopram-mediated ROS formation leads to the GSH depletion in isolated hepatocytes. Thus, it gives us a clue that oxidative stress is involved in the cytotoxicity mechanism of citalopram. Moreover, depletion of hepatocyte GSH content beforehand potentiated entire citalopram-induced cytotoxicity, ROS generation, mitochondrial membrane potential decline, lysosomal membrane leakiness pointing out the protective role of GSH in citalopram-induced liver damage.
Drugs/xenobiotic influence mitochondria in various ways such as interfering with the electron-transfer chain, energy (ATP) production, and/or mitochondrial membrane permeability (Santos et al. 2008). Antidepressants could cause mitochondrial dysfunction via other processes such as decreasing the amount of nitric oxide (Hwang et al. 2008) and effecting mitochondrial membrane permeability and respiration rate (Dykens et al. 2008; Taziki et al. 2013a). Mitochondrial respiratory chains transfer electrons from complex I to complexes III and IV. Citalopram has been shown to display inhibitory effects on respiratory chain complexes (Hroudova and Fisar 2010). This inhibitory action is believed to have a tight link with mitochondrial impairment which is considered a substantial source of ROS (Pourahmad et al. 2010). Mitochondrial ROS formation gives rise to some primary deleterious effects in situ (Haj-Mirzaian et al. 2015). Besides, targeting respiratory chain and mitochondrial membrane via the ROS, it should not be ruled out that the mitochondrion is also the major target of reactive species. In this study, we examined the impact of citalopram on mitochondrial membrane potential (∆Ψm) collapse as a marker of mitochondrial dysfunction through measuring mitochondrial ability to retain rhodamine 123 in isolated hepatocytes (Shaki et al. 2012). Rapid reduction of hepatocyte mitochondrial membrane potential following citalopram treatment was postponed by antioxidants suggesting the direct relationship between ROS formation and mitochondrial injury. Also, inhibition of citalopram-induced cell death and mitochondrial toxicity by ATP generators and MPT pore sealing agents point toward the possibility of the latter consequences due to MPT pore opening and ATP depletion. Any damage to mitochondrial energy generation results in intracellular acidosis and osmotic injury which in turn causes plasma membrane lysis (Pourahmad et al. 2010). On the other hand, mitochondrial membrane disruption eventually leads to uncoupling of the oxidative phosphorylation and the production of superoxide anion which could trigger the generated mitochondrial cytopathy (Addabbo and Goligorsky 2009).
Lysosomes, the acidic organelles, are the basic house cleaning compartments of the cell with a high iron pool which is provided by autophagy. Both the production of mitochondrial ROS mainly in the form of H2O2 and the insufficiency of detoxifying processes due to drug/xenobiotic-induced cell damage leads to the easy diffusion of lipophilic H2O2 and its penetration to lysosomal membrane. The interaction between H2O2 and lysosomal Fe3+ in a Fenton-type reaction results in the production of highly reactive hydroxyl radical which induces lysosomes integrity leakiness and the liberation of lysosomal enzyme content into the cytosol. The contribution of mitochondria and redox-active iron rich lysosomes increases the amount ROS in this destructive pathway. Lysosomal membrane stability (LMS) evaluation has revealed acute toxic effects of antidepressant agents through lysosomal membrane damage (Minguez et al. 2014). Our results also have shown that citalopram treatment attenuated membrane intactness, leading to the leakiness of the lysosomal membrane. Also, our data demonstrated that lysosomal fragility was prevented by antioxidants and other inhibitors. All these interesting events brings in mind that there is a tight link between initiation of oxidative stress and further mitochondrial and lysosomal involvement in citalopram-induced toxicity.
Regarding the in vivo studies, citalopram (20 mg/kg) caused hepatotoxicity in rats, which was accompanied by the elevation of liver enzymes levels, liver glutathione decline, LPO and changes in liver histopathology. Our results met with a more severe toxic effect in glutathione-depleted and/or enzyme-induced animals and NAC (400 mg/kg), quercetine (500 mg/kg) and/or taurine (400 mg/kg) administration significantly reduced citalopram-induced hepatotoxicity in all animal groups.
Cellular glutathione is a potent detoxification system, which can also bond to additional intracellular ROS sources. However, these processes lead to glutathione reservoir depletion (Kalgutkar et al. 2005). Evidences of oxidative tissue damage related to citalopram might be the possible cause of cellular GSH stores amelioration (Abdelmajeed 2009). Further, GSH depletion accelerates the hepatotoxic effect of several xenobiotic/drugs (Heidari et al. 2014a). Likewise, it was observed in our experiments in animals receiving BSO as a glutathione depleting agent. Moreover, citalopram drastically increased the amount of LPO. Both LPO and liver serum enzymes function were more severe in GSH-depleted rats indicating the role of GSH in preventing CIT-induced hepatotoxicity. Also, the findings of this study suggest the protective role of NAC, quercetine and/or taurine in citalopram-induced liver injury in rats.
The role of metabolic pathways and reactive metabolites in citalopram-induced liver damage was evaluated through enzyme-induced animals. Citalopram displayed severe hepatotoxic profile in β-naphtoflavone and/or phenobarbital-induced animals. These findings indicate that metabolic activation plays a key role in citalopram-induced hepatotoxicity.
Histopathological evaluation of rat liver revealed severe damage ensured by loss of liver normal architecture, shrinkage of hepatocytes with a mild inflammatory cell infiltration. Antioxidant administration effectively alleviated pathologic lesions in enzyme–induced citalopram-treated rats.
Based on our findings, the exposure of rat hepatocytes to citalopram (500 µM) caused a time-dependent cell death by the formation of ROS, LPO, depletion of cellular GSH level, and accumulation of GSSG. Also, excess ROS target mitochondrial and lysosomal membranes and cause oxidative stress damage in these sub-organelles which in turn this toxic crosstalk triggers ROS generation and accelerates citalopram-induced hepatotoxicity. In vivo studies stayed in line with the evidence of oxidative liver damage induced by citalopram. Furthermore, both GSH depletion and enzyme induction augmented the latter toxicity, suggesting the possible role of reactive metabolites in citalopram hepatotoxicity. The findings of this study also suggest the administration of NAC, quercetine and/or taurine for protection of patients against citalopram-induced liver injury which needs to be confirmed by clinical studies.
References
Abdelmajeed NA (2009) Oxidative tissue damage induced by citalopram in rat different organs. RES J Med Med Sci 4:580–586
Abdel-Razaq W, Kendall D, Bates T (2011) The effects of antidepressants on mitochondrial function in a model cell system and isolated mitochondria. Neurochem Res 36:327–338
Addabbo Montagnani M, Goligorsky MS (2009) Mitochondria and reactive oxygen species. Hypertension 53:885–892
Ahmadian E, Jafari S, Khosroushahi AY (2015) Role of angiotensin II in stem cell therapy of cardiac disease. J Renin Angiotensin Aldosterone Syst 16:702–711
Attia SM, Bakheet SA (2013) Citalopram at the recommended human doses after long-term treatment is genotoxic for male germ cell. Food Chem Toxicol 53:281–285
Bayir H, Kagan VE (2008) Bench-to-bedside review: mitochondrial injury, oxidative stress and apoptosis–there is nothing more practical than a good theory. Crit Care 12:206
Boya P, Kroemer G (2008) Lysosomal membrane permeabilization in cell death. Oncogene 27:6434–6451
Chatuphonprasert W, Sangkawat T, Nemoto N, Jarukamjorn K (2011) Suppression of beta-naphthoflavone induced CYP1A expression and lipid-peroxidation by berberine. Fitoterapia 82:889–895
Drew R, Miners JO (1984) The effects of buthionine sulphoximine (BSO) on glutathione depletion and xenobiotic biotransformation. Biochem Pharmacol 33:2989–2994
Dykens JA, Jamieson JD, Marroquin LD, Nadanaciva S, Xu JJ, Dunn MC, Smith AR, Will Y (2008) In vitro assessment of mitochondrial dysfunction and cytotoxicity of nefazodone, trazodone, and buspirone. Toxicol Sci 103:335–345
Eftekhari A, Azarmi Y, Parvizpur A, Eghbal MA (2015) Involvement of oxidative stress and mitochondrial/lysosomal cross-talk in olanzapine cytotoxicity in freshly isolated rat hepatocytes. Xenobiotica 46:369–378
Eghbal MA, Tafazoli S, Pennefather P, O’Brien PJ (2004) Peroxidase catalysed formation of cytotoxic prooxidant phenothiazine free radicals at physiological pH. Chem Biol Interact 151:43–51
Eghbal MA, Taziki S, Sattari MR (2014) Mechanisms of phenytoin-induced toxicity in freshly isolated rat hepatocytes and the protective effects of taurine and/or melatonin. J Biochem Mol Toxicol 28:111–118
Guerra LN, Escudero A, Sáinz M, Venegoni M, Montastruc JL, Carvajal A (2014) Hepatotoxicity related to agomelatine and other new antidepressants. J Clin Psychopharmacol 34:327–330
Haj-Mirzaian A, Rahimi-Balaei M, Naserzadeh P, Dehpour A, Mehr SE, Hosseini M-J (2015) Tropisetron attenuated the anxiogenic effects of social isolation by modulating nitrergic system and mitochondrial function. Biochim Biophys Acta 1850:2464–2475
Heidari R, Babaei H, Eghbal MA (2013) Cytoprotective effects of taurine against toxicity induced by isoniazid and hydrazine in isolated rat hepatocytes. Arh Hig Rada Toksikol 64:15–24
Heidari R, Babaei H, Eghbal M (2014a) Amodiaquine-induced toxicity in isolated rat hepatocytes and the cytoprotective effects of taurine and/or N-acetyl cysteine. Res Pharm Sci 9:97–105
Heidari R, Babaei H, Roshangar L, Eghbal MA (2014b) Effects of enzyme induction and/or glutathione depletion on methimazole-induced hepatotoxicity in mice and the protective role of N-acetylcysteine. Adv Pharm Bull 4:21–28
Hroudova J, Fisar Z (2010) Activities of respiratory chain complexes and citrate synthase influenced by pharmacologically different antidepressants and mood stabilizers. Neuroendocrinol Lett 31:336–342
Hwang J, Zheng LT, Ock J, Lee MG, Kim S-H, Lee H-W, Lee W-H, Park H-C, Suk K (2008) Inhibition of glial inflammatory activation and neurotoxicity by tricyclic antidepressants. Neuropharmacol 55:826–834
Jaeschke H, McGill MR, Ramachandran A (2012) Oxidant stress, mitochondria, and cell death mechanisms in drug-induced liver injury: lessons learned from acetaminophen hepatotoxicity. Drug Metab Rev 44:88–106
Jamshidzadeh A, Niknahad H, Kashafi H (2007) Cytotoxicity of chloroquine in isolated rat hepatocytes. J Appl Toxicol 27:322–326
Kalgutkar AS, Gardner I, Obach RS, Shaffer CL, Callegari E, Henne KR, Mutlib AE, Dalvie DK, Lee JS, Nakai Y (2005) A comprehensive listing of bioactivation pathways of organic functional groups. Curr Drug Metab 6:161–225
Khan S, O’Brien PJ (1991) 1-bromoalkanes as new potent nontoxic glutathione depletors in isolated rat hepatocytes. Biochem Biophys Res Commun 179:436–441
Lim S, Lee S-J, Nam K-W, Kim KH, Mar W (2013) Hepatoprotective effects of reynosin against thioacetamide-induced apoptosis in primary hepatocytes and mouse liver. Arch Pharm Res 36:485–494
López-Torres E, Lucena MI, Seoane J, Verge C, Andrade RJ (2004) Hepatotoxicity related to citalopram. Am J Psychiatry 161:923–924
Luzio JP, Pryor PR, Bright NA (2007) Lysosomes: fusion and function. Nat Rev Mol Cell Biol 8:622–632
Milkiewicz P, Chilton A, Hubscher S, Elias E (2003) Antidepressant induced cholestasis: hepatocellular redistribution of multidrug resistant protein (MRP2). Gut 52:300–303
Minguez L, Farcy E, Ballandonne C, Lepailleur A, Serpentini A, Lebel J-M, Bureau R, Halm-Lemeille M-P (2014) Acute toxicity of eight antidepressants: what are their modes of action? Chemosphere 108:314–319
Mohammadi Z, Azarnia M, Mirabolghasemi G, Shiravi A, Mohammadi Z (2013) Histological changes in the liver of fetuses of pregnant rats following citalopram administration. Indian J Pharmacol 45:517–521
O’Brien P, Siraki A (2005) Accelerated cytotoxicity mechanism screening using drug metabolising enzyme modulators. Curr Drug Metab 6:101–109
Overø KF, Svendsen O (1978) Toxicological aspects of food safety. In: Leonard BJ (ed) Hepatotoxicity of citalopram in rats and first-pass metabolism. Springer, Berlin Heidelberg, pp 177–180
Pelkonen O, Maenpaa J, Taavitsainen P, Rautio A, Raunio H (1998) Inhibition and induction of human cytochrome P450 (CYP) enzymes. Xenobiotica 28:1203–1253
Pourahmad J, Hosseini M-J, Eskandari MR, Shekarabi SM, Daraei B (2010) Mitochondrial/lysosomal toxic cross-talk plays a key role in cisplatin nephrotoxicity. Xenobiotica 40:763–771
Pourahmad J, Eskandari MR, Kaghazi A, Shaki F, Shahraki J, Fard JK (2012) A new approach on valproic acid induced hepatotoxicity: involvement of lysosomal membrane leakiness and cellular proteolysis. Toxicol In Vitro 26:545–551
Reed DJ, Babson JR, Beatty PW, Brodie AE, Ellis WW, Potter DW (1980) High-performance liquid chromatography analysis of nanomole levels of glutathione, glutathione disulfide, and related thiols and disulfides. Anal Biochem 106:55–62
Santos N, Medina W, Martins N, Mingatto FE, Curti C, Santos A (2008) Aromatic antiepileptic drugs and mitochondrial toxicity: effects on mitochondria isolated from rat liver. Toxicol In Vitro 22:1143–1152
Shaki F, Hosseini M-J, Ghazi-Khansari M, Pourahmad J (2012) Toxicity of depleted uranium on isolated rat kidney mitochondria. Biochim Biophys Acta 1820:1940–1950
Siegmund SV, Brenner DA (2005) Molecular pathogenesis of alcohol-induced hepatic fibrosis. Alcohol Clin Exp Res 29:102S–109S
Solomons K, Gooch S, Wong A (2005) Toxicity with selective serotonin reuptake inhibitors. Am J Psychiatry 162:1225
Taziki S, Sattari MR, Eghbal MA (2013) Mechanisms of trazodone-induced cytotoxicity and the protective effects of melatonin and/or taurine toward freshly isolated rat hepatocytes. J Biochem Mol Toxicol 27:457–462
Uchiyama M, Mihara M (1978) Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Anal Biochem 86:271–278
Voican CS, Corruble E, Naveau S, Perlemuter G (2014) Antidepressant-induced liver injury: a review for clinicians. Am J Psychiatry 171:404–415
von Moltke LL, Greenblatt DJ, Grassi JM, Granda BW, Venkatakrishnan K, Duan SX, Fogelman SM, Harmatz JS, Shader RI (1999) Citalopram and desmethylcitalopram in vitro: human cytochromes mediating transformation, and cytochrome inhibitory effects. Biol Psychiatry 46:839–849
Wagner KD, Robb AS, Findling RL, Jin J, Gutierrez MM, Heydorn WE (2014) A randomized, placebo-controlled trial of citalopram for the treatment of major depression in children and adolescents. Am J Psychiatry 161:1079–1083
Xia Z, Bergstrand A, DePierre JW, Nässberger L (1999a) The antidepressants imipramine, clomipramine, and citalopram induce apoptosis in human acute myeloid leukemia HL-60 cells via caspase-3 activation. J Biochem Mol Toxicol 13:338–347
Xia Z, Lundgren B, Bergstrand A, DePierre JW, Nässberger L (1999b) Changes in the generation of reactive oxygen species and in mitochondrial membrane potential during apoptosis induced by the antidepressants imipramine, clomipramine, and citalopram and the effects on these changes by Bcl-2 and Bcl-X L. Biochem Pharmacol 57:1199–1208
Yilmaz O, Keser S, Tuzcu M, Guvenc M, Cetintas B, Irtegun S, Tastan H, Sahin K (2009) A practical HPLC method to measure reduced (GSH) and oxidized (GSSG) glutathione concentrations in animal tissues. J Anim Vet Adv 8:343–347
Yoshida T (1996) Determination of reduced and oxidized glutathione in erythrocytes by high-performance liquid chromatography with ultraviolet absorbance detection. J Chromatogr B Biomed Sci Appl 678:157–164
Yun J, Lee Y, Yun K, Oh S (2015) Bergenin decreases the morphine-induced physical dependence via antioxidative activity in mice. Arch Pharmacal Res 38:1248–1254
Zitka O, Skalickova S, Gumulec J, Masarik M, Adam V, Hubalek J, Trnkova L, Kruseova J, Eckschlager T, Kizek R (2012) Redox status expressed as GSH: GSSG ratio as a marker for oxidative stress in paediatric tumour patients. Oncol Lett 4:1247–1253
Acknowledgments
The authors would like to thank Drug Applied Research Center of Tabriz University of Medical Sciences, Tabriz, Iran, for providing technical facilities. This is a report of a database from thesis entitled “Evaluation of the mechanisms of hepatic injuries induced by antidepressant drugs” registered and funded by a grant (Grant number: 77/93) from the Drug Applied Research Center of Tabriz University of Medical Sciences, Tabriz, Iran. The authors are also thankful to the University’s “Students’ Research Committee” for providing technical supports to the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest associated with this work.
Funding information
Drug applied research center (Grant number: 77/93).
Rights and permissions
About this article
Cite this article
Ahmadian, E., Eftekhari, A., Fard, J.K. et al. In vitro and in vivo evaluation of the mechanisms of citalopram-induced hepatotoxicity. Arch. Pharm. Res. 40, 1296–1313 (2017). https://doi.org/10.1007/s12272-016-0766-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12272-016-0766-0