Abstract
In order to characterize the in situ intestinal permeability and in vivo oral bioavailability of celecoxib (CXB), a poorly water-soluble cyclooxygenase (COX)-2 inhibitor, various formulations including the self-emulsifying drug delivery system (SEDDS) and supersaturating SEDDS (S-SEDDS) were compared. The S-SEDDS formulation was obtained by adding Soluplus as a precipitation inhibitor to SEDDS, composed of Capryol 90 as oil, Tween 20 as surfactant, and Tetraglycol as cosurfactant (1:4.5:4.5 in volume ratio). An in situ single pass intestinal perfusion study in rats was performed with CXB-dissolved solutions at a concentration of 40 μg/mL. The effective permeability (Peff) of CXB in the control solution (2.5 v/v% Tween 20-containing PBS) was 6.39 × 10−5 cm/s. The Peff value was significantly increased (P < 0.05) by the lipid-based formulation, yielding 1.5- and 2.9-fold increases for the SEDDS and S-SEDDS solutions, respectively, compared to the control solution. After oral administration of various formulations to rats at the equivalent dose of 100 mg/kg of CXB, the plasma drug level was measured by LC–MS/MS. The relative bioavailabilities of SEDDS and S-SEDDS were 263 and 355 %, respectively, compared to the CXB suspension as a reference. In particular, S-SEDDS revealed the highest Cmax and the smallest Tmax, indicating rapid and enhanced absorption with this formulation. This study illustrates the potential use of the S-SEDDS formulation in the oral delivery of poorly water-soluble compounds.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Celecoxib (CXB) is a selective cyclooxygenase (COX)-2 inhibitor used to treat osteoarthritis, rheumatoid arthritis and acute pain (Clemett and Goa 2000). CXB is hydrophobic (log P value of 3.5) and is categorized as a Class II drug as it is a highly permeable and poorly soluble compound according to the biopharmaceutical classification system (BCS) (Amidon et al. 1995; Paulson et al. 2001). Its limited solubility affects the extent and variability of absorption after oral administration.
The self-emulsifying drug delivery system (SEDDS) has been employed to enhance the solubilization capacity and the oral bioavailability of poorly soluble drugs. However the drug may precipitate out of solution when SEDDS disperses in the gastrointestinal (GI) tract. Inhibition of drug precipitation may be controlled by the addition of hydrophilic polymers or surfactants to the emulsion pre-concentrate (Guzman et al. 2007; Vasconcelos et al. 2007). The supersaturating SEDDS (S-SEDDS) formulation has the characteristics to stabilize a drug in its supersaturated state by inhibiting precipitation and by maintaining a metastable state of the drug in the GI tract for a sufficient length of time to allow its absorption (Brouwers et al. 2009). In our earlier study, S-SEDDS composed of Capryol 90 as oil, Tween 20 as surfactant, Tetraglycol as cosurfactant, and Soluplus as a precipitation inhibitor was proposed for the enhanced dissolution of CXB and improved oral delivery (Song et al. 2013). Even though the SEDDS formulation revealed improved dissolution of CXB of up to about 20 % for the initial period of 5 min, the dissolution decreased to half levels at 2 h. In contrast, by the addition of 40 mg/mL Soluplus, the greatest dissolution, of approximately 90 %, was obtained, and delayed drug crystallization was achieved. And CXB dissolution by S-SEDDS was pH-independent, indicating its potential for absorption throughout the whole GI tract. Therefore, it is necessary to demonstrate whether these enhanced performances in vitro correlate well with the absorption behavior in vivo.
Investigation of drug absorption across intestinal membranes is important when developing a strategy for improving the oral bioavailability (BA) of drugs, and this requires increased understanding of the basic mechanisms involved in the membrane translocation of drugs across the intestinal epithelium (Zakeri-Milani et al. 2005). Moreover, it is very important to choose the most suitable model for assessment of lipid-based formulations. A rat model would be the first choice for in situ permeability and in vivo pharmacokinetic studies because it is a reliable and versatile model suitable for initial screening and identification of the optimum prototype of lipid-based formulation (O’driscoll and Griffin 2008). Lennernas et al. (1992) evaluated the potential of the new perfusion technique as a tool for investigation of drug absorption mechanisms in the human intestine. Although a human in vivo study would be the most desirable, it is not easy to carry out. So far, various animal models have been evolved to estimate the GI absorption behavior of drugs and to establish the relationship between the animal and the human (Karlsson and Artursson 1991; Hillgren et al. 1995; Rubas et al. 1993; Salphati et al. 2001; Chiou and Barve 1998). The in situ single pass intestinal perfusion (SPIP) approach is one of the most common techniques used to investigate the intestinal absorption behavior of drugs. The SPIP technique provides the following advantages: (1) a preserved microclimate above the intestinal membrane which makes it less sensitive to pH variation; (2) easy experimental control of drug concentration and intestinal perfusion rate; (3) ability to study regional difference; (4) presence of an intact blood supply in the experimental animals; and (5) high correlation between human and rat intestinal permeability coefficient (Fagerholm et al. 1996; Kang et al. 2012). The rat jejunal permeability coefficient (Peff) obtained by the SPIP technique is highly correlated with human intestinal permeability and the fraction absorbed of the compounds for both low permeable and high permeable drugs (Zakeri-Milani et al. 2007). Therefore, a SPIP technique using rat jejunum can be a useful approach to investigate the effect of the S-SEDDS vehicle on CXB absorption.
The present study aimed to compare the formulation effect of SEDDS and S-SEDDS on CXB solubilization and oral absorption in rats. Both an in situ permeability study using rat’s SPIP model and an in vivo pharmacokinetic study after oral administration were performed to characterize the intestinal absorption behavior and to evaluate the potential use of these formulations in the oral delivery of CXB. The correlation between in situ permeability and the in vivo BA of CXB was investigated.
Materials and methods
Materials
CXB was purchased from Cadila Pharmaceuticals Ltd. (Gujarat, India). CXB-d4 was purchased from Toronto Research Chemicals (Toronto, Canada). Tween 20 (polyoxyethylene 20 sorbitan monolaurate), Tetraglycol, sodium carboxymethyl cellulose and phenol red were purchased from Sigma-Aldrich (St. Louis, MO, USA). Capryol 90 (propylene glycol monocaprylate) was supplied by Gattefosse (Saint Priest, France). Soluplus (polyvinyl caprolactam-polyvinyl acetate-polyethylene glycol graft copolymer) was supplied by BASF (Ludwigshafen, Germany). Acetonitrile and methanol of HPLC grade were purchased from J. T. Baker (Phillipsburg, NJ, USA). All other chemicals used were of analytical grade.
Animals
All animal experiments were performed in accordance with the National Institute of Health (NIH) guidelines “Principles of laboratory animal care” (NIH publication No. 85-23, revised 1996) and were approved by the Institutional Animal Care and Use Committee of Chung-Ang University in Seoul, Korea. Sprague–Dawley rats (male; 200 ~ 250 g; 7–9 weeks) were purchased from Orient Bio (Kyungki-do, Korea). Rats were fasted for approximately 12–18 h with free access to water to clear the gut prior to the SPIP and pharmacokinetic studies.
Preparation of SEDDS and S-SEDDS formulations
The SEDDS and S-SEDDS formulations were prepared as reported earlier (Song et al. 2013). The CXB-containing SEDDS was prepared by dissolving the drug to the mixture of oil (10 % Capryol 90), surfactant (45 % Tween 20), and cosurfactant (45 % Tetraglycol). The mixture was vortexed to get a clear homogenous solution. The S-SEDDS formulation was obtained by addition of Soluplus as a precipitation inhibitor to the SEDDS prepared at the concentration of 40 mg/mL. CXB was solubilized at the level of 200 mg/mL in both formulations.
In situ permeability study
Preparation of perfusion solution
Phosphate buffered solution (PBS) was used in the SPIP and it comprised 33 mM of sodium phosphate monobasic, 33 mM of sodium phosphate dibasic and 80 mM of sodium chloride, and pH was adjusted to 7.4 with phosphoric acid. Phenol red as a non-absorbable marker was added to the perfusion solution to correct for any water absorption and secretion that may occur during the experiment. Four kinds of perfusion solution containing CXB at the concentration of 40 μg/mL were prepared as follows: (1) control solution, CXB was dissolved in 2.5 v/v% Tween 20-containing PBS; (2) S-Control solution, Soluplus was added (160 μg/mL) to control solution; (3) SEDDS solution, CXB-dissolved SEDDS was diluted 250 times with PBS; (4) S-SEDDS solution, CXB-dissolved S-SEDDS was diluted 250 times with PBS.
Single pass intestinal perfusion (SPIP) experiment
Preliminary studies are required before commencing SPIP study to ensure that the losses of drug during the perfusion resulted only from absorption or from other causes such as nonspecific binding to the tubing and/or degradation. In order to evaluate the effect of binding to the tubing, the perfusion solution of CXB was incubated 37 °C with tubing for 2 h. Samples were collected after 2 h and analyzed by HPLC. In order to evaluate stability, the perfusion solution containing CXB was incubated at 37 °C for 2 h. Aliquots were withdrawn and analyzed by HPLC.
The in situ SPIP technique was applied as previously reported (Zakeri-Milani et al. 2007; Berggren et al. 2004; Kang et al. 2012). Briefly, rats were anaesthetized using an intraperitoneal injection of urethane (0.75 g/kg), and a heating pad and lamp was used to maintain body temperature. The abdomen was opened with a midline incision, and the proximal rat jejunum of approximately 10 cm was isolated and cannulated with plastic tubing (1 mm in id and 2 mm in od). The intestinal segment was rinsed with PBS maintained at 37 °C for approximately 30 min until the outlet solution was visually clear. The remained PBS was completely removed by idling the peristaltic pump (BT100-2J, Baoding Longer Precision Pump, China). The perfusion fluids were infused at a rate of 0.2 mL/min into the jejunal segment for 120 min. The perfusate was collected every 20 min and centrifuged (Micro 17TR, Hanil Science) at 15,000 rpm for 10 min. The upper layer was filtered through a membrane filter (0.45 μm, PVDF, Smartpor®) and subjected for HPLC assay.
HPLC assay of CXB in perfusate
The concentrations of CXB and phenol red in perfusate solution were simultaneously determined by HPLC. The HPLC systems consisted of a pump (W2690/5, Waters, USA), UV detector (W2489, Waters, USA), and a data station (Empower3, Waters, USA). Chromatographic separation was performed using a Kromasil 100-5C18 column (150 × 4.6 mm, 5 μm, AkzoNobel, Sweden) at the flow rate of 1.0 mL/min. The isocratic mobile phase consisted of acetonitrile and pH 6.0 phosphoric acid with 0.5 v/v% triethylamine (55:45, v/v). 10 μL of each sample was injected onto the column and the UV detection was performed at 251 nm.
Permeability calculation
The intestinal effective permeability was calculated from the steady-state concentration of the compound in the collected perfusate as described elsewhere (Komiya et al. 1980; Fagerholm et al. 1996; Kang et al. 2012). The ratio of outlet to inlet drug concentration (\({\text{C}}_{\text{out}}^{\prime}/{\text{C}}_{\text{in}}^{\prime}\)) was obtained to substitute the concentration of phenol red for correcting water flux: \( ( {\text{C}}_{\text{out}}^{\prime } /{\text{C}}_{\text{in}}^{\prime } ) = ({\text{C}}_{\text{out}} /{\text{C}}_{\text{in}} ) \times ({\text{C}}_{{{\text{in}}\,{\text{phenol}}\,{\text{red}}}} /{\text{C}}_{{{\text{out}}\,{\text{phenol}}\,{\text{red}}}} ) \), where Cout is the concentration of CXB in the outlet perfusate, Cin is the CXB concentration in entering perfusate, and Cin phenol red and Cout phenol red are the inlet and the outlet concentration of phenol red, respectively. The effective permeability coefficient (Peff, cm/s) was calculated according to a parallel tube model: \( {\text{P}}_{\text{eff}} = \left[ { - {\text{Q}}\;{ \ln }\left( {{\text{C}}_{\text{out}}^{\prime } /{\text{C}}_{\text{in}}^{\prime } } \right)} \right]/{\text{A}} \), in which Q is the flow rate (0.2 mL/min) of the entering perfusate and A is the surface area (cm2) of the intestinal segment assumed to be the area of a cylinder (2πrL) with the length (L) of 10 cm and radius (r) of 0.21 cm for the jejunum. The apparent first-order absorption rate constant (Ka, min−1) was calculated as follows: \( {\text{K}}_{\text{a}} = \left[ { 1 - \left( {{\text{C}}_{\text{out}}^{\prime } /{\text{C}}_{\text{in}}^{\prime } } \right)} \right]{\text{Q}}/\pi {\text{r}}^{ 2} {\text{L}} \).
In vivo oral absorption study
Oral administration and plasma sampling
After fasting the rats for approximately 12–18 h, test samples were administered via oral gavage at a dose of 100 mg/kg as CXB. Four kinds of test sample (CXB 40 mg/mL) were prepared and administered to four groups as follows: Group (1) CXB suspension, CXB crystalline powder was suspended in water containing 0.2 w/v% sodium carboxymethyl cellulose; Group (2) Celebrex suspension, granular content of Celebrex® capsule was suspended in water; Group (3) SEDDS, CXB-containing SEDDS formulation was five times diluted with water; Group (4) S-SEDDS, CXB-containing S-SEDDS formulation was five times diluted with water. Blood samples of about 0.3 mL were collected from the retro-orbital plexus at predetermined time points of 0.5, 1, 2, 3, 5, 8, and 12 h using heparinized tubes, and centrifuged at 13,000 rpm for 15 min. Plasma samples were stored at −80 °C until analysis by LC–MS/MS.
CXB determination in plasma samples by LC–MS/MS
The concentrations of CXB in rat plasma were determined by LC–MS/MS. A stock solution of CXB was prepared in mobile phase at 100 mg/mL. Using this stock solution, plasma calibration solution was prepared at concentrations of 0.1, 0.2, 0.5, 1, 5, and 10 μg/mL. Briefly, an aliquot of each plasma sample (250 μL) was pipetted into an Eppendorf tube, followed by the addition of 25 μL of CXB-d4 as an internal standard (IS) solution (20 μg/mL) and 1 mL of acetonitrile as extraction solvent. The mixture was vortexed and centrifuged at 10,000 rpm for 4 min. 100 μL of the upper layer was pipetted into an Eppendorf tube and 1 mL of the mobile phase was added. Samples were transferred to autosampling vials and 10 μL aliquots were injected into the LC–MS/MS system. An API 3200 Triple-quadrupole mass spectrometer (Applied biosystems/MDS SCIEX, USA) with electrospray ionization (ESI) in negative ion mode for ion production was used for CXB detection. Chromatography was performed on an X-Terra C18 column (50 × 2.1 mm, 5 μm, Waters, USA). The mobile phase was 10 mM ammonium acetate (pH 4.0)-acetonitrile (10:90, v/v) at a flow rate of 0.25 mL/min. The ion-spray voltage was set at -4.5 kV and the source temperature was 500 °C. Multiple reactions monitoring (MRM) was performed using nitrogen as the collision gas. The analytes were detected by monitoring the transitions m/z 380.0 → 316.0 and 384.0 → 320.0 with collision energy of −32 V for CXB and CXB-d4, respectively.
Pharmacokinetic assessment
Data analysis was performed using a BA Calc 2007 pharmacokinetic analysis program (Korea Food & Drug Administration, Korea). Area under the curve (AUC) from 0 to 12 h was calculated using the program’s linear trapezoidal rule. Maximum plasma concentration (Cmax) and time needed to reach the maximum plasma concentration (Tmax) were determined directly from concentration–time data. The relative bioavailability (BA) was calculated as the ratio of the AUCs of test samples to CXB suspension.
Statistical analysis
All data were expressed as the mean ± standard deviation (SD). Statistical significance was determined by Student’s t test with a threshold of P < 0.05.
Results
Formulation characteristics
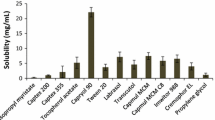
Previously, we developed the optimal S-SEDDS formulation for enhanced dissolution of CXB, a poorly water-soluble drug (Song et al. 2013). Since the SEDDS formulation used in this study contains an oil of less than 20 and 45 % surfactant (HLB > 12), it is classified as Type IIIb, based on the lipid formulation classification system (LFCS). This formulation can induce the formation of a microemulsion that is smaller and faster than other types of LFCS, by virtue of its increased hydrophilic property (Pouton 2006). This formulation had the characteristics of small droplet size and great solubility which were 208 nm and 556.7 mg/mL on average, respectively. The addition of Soluplus to SEDDS did not influence the dispersion characteristics, but significantly increased the dissolution level and delayed the criticial precipitation time, as reported earlier (Song et al. 2013). Reference solutions of CXB for the perfusion or absorption study were successfully prepared by either solubilizing CXB in PBS with 2.5 v/v% Tween 20 or suspending in water with 0.2 w/v% sodium carboxymethyl cellulose, respectively.
Analytical method establishment
The HPLC method proposed provided a simultaneous determination of CXB and phenol red in the perfusate. The retention times of a collected sample containing CXB and phenol red were 9.9 and 1.5 min, respectively. The separation of the representative chromatogram was sufficient enough for no interfering peak to be observed on chromatogram. The selectivity parameter calculated by the ratio of the respective capacity factor of two components (Zakeri-Milani et al. 2005) was found to be 19.8, indicating successful separation of phenol red and CXB. The calibration curves displayed excellent linearity (r2 > 0.999) over the concentration range from 10 to 80 μg/mL that was investigated. The inter-day precision and accuracy data are listed in Table 1. This concentration range was selected based on the drug concentration used in permeability studies. Meanwhile, the analytical method of LC–MS/MS showed good validity, revealing acceptable linearity (r2 > 0.999) over the concentration range of 0.1–10 μg/mL as shown in Table 1.
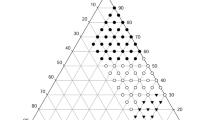
In situ permeability in SPIP study
The intestinal permeability of CXB in various types of solutions was studied with the rat’s jejunum segment using the SPIP technique, which examines diffusion of a drug molecule across the intestine at steady state. The steady state is confirmed by plotting the ratio of the outlet to inlet concentrations as corrected for water uptake against time. As shown in Fig. 1, the ratio reached a plateau within 20 min in all test solutions. Meanwhile, in the preliminary study on nonspecific binding of the drug to the tubing and/or drug, and stability in the perfusion solution, no adsorption of CXB was observed while the aqueous stability of the drug was maintained for the whole period of the experiment (data not shown).
Representative plots for the ratio of outlet to inlet drug concentration (\( {\text{C}}_{\text{out}}^{\prime } /{\text{C}}_{\text{in}}^{\prime } \)) versus time in the SPIP using different samples. Values represent mean ± SD (n = 3). Filled triangle Control solution, open triangle S-Control solution, filled circle SEDDS solution, open circle S-SEDDS solution
The Peff and Ka values of the different perfusion solutions were calculated using average (\( {\text{C}}_{\text{out}}^{\prime } /{\text{C}}_{\text{in}}^{\prime } \)) data gathered for all subsequent 20 min intervals over 2 h, and these values are listed in Table 2. In comparison to the control solution that contained solubilized CXB, all test solutions including Soluplus-added control solution (S-Control), SEDDS, and S-SEDDS showed significant difference at P < 0.05. The decreasing order in the permeability was observed as S-SEDDS > SEDDS > S-Control > Control. The permeability of CXB was affected by the formulation factor. Compared to the control solution, Soluplus addition or the SEDDS formulation increased intestinal permeability about 1.2 or 1.5 times, respectively. Moreover, by the combination of both the Soluplus addition and SEDDS formulation (S-SEDDS), the permeability of CXB was further increased; there was an approximately 2.9-fold increase versus the control solution; a 2.4-fold increase versus S-Control; a 1.9-fold increase versus the SEDDS solution. As a result, enhancement of the effect of Soluplus was dependent on the solubilized state of CXB, and this finding could be interpreted as stabilization of the emulsion droplet with the polymeric intercalation.
In vivo oral absorption through pharmacokinetic study
In order to find the formulation’s effect on oral absorption behavior, four different samples, CXB suspension (Goup 1), Celebrex suspension (Group 2), SEDDS (Group 3), and S-SEDDS (Group 4), were administered. The plasma level of CXB was measured and plotted as shown in Fig. 2. Both the CXB suspension and Celebrex suspension groups revealed a similar pattern of an increase of the plasma level over 5 h, even though the increment of the Celebrex suspension was much greater than that of the CXB suspension. In contrast, both the SEDDS and S-SEDDS formulations (Group 3 and 4) yielded a faster and greater increase than the other suspension systems (Group 1 and 2), possibly due to the solubilization capacity of self-emulsifying delivery systems. Furthermore, S-SEDDS brought a sharp increase in the earlier phase compared to SEDDS, which resulted in the highest CXB level throughout the whole period of observation.
The pharmacokinetic parameters including Tmax, Cmax, and AUC are listed in Table 3. As expected, S-SEDDS (Group 4) was superior to the other samples in all parameters; the parameters were significantly different at P < 0.05. The AUC and Cmax values of CXB suspension (Group 1) were much lower than those of the others. Insignificant differences between the Celebrex suspension and SEDDS were found in all parameters. The AUC value of S-SEDDS was 1.4-fold greater than that of Celebrex or SEDDS and 3.5-fold greater than that of CXB suspension. The Cmax value of S-SEDDS was about 1.3- to 3.9-fold higher than that of other samples. In the comparison of the Tmax values, S-SEDDS showed the fastest absorption with a 2.2 times smaller Tmax on average than the others. As a result, the oral BA of CXB was greatly improved by the S-SEDDS formulation.
Discussion
Lipid-based formulations provide positive influences on drug absorption through various mechanisms including; (1) enhanced solubilizing capacity, (2) inhibition of drug precipitation on intestinal dilution, (3) enhanced intestinal permeability, (4) inhibition of efflux transporters, (5) reduced cytochrome enzymes, and (6) enhanced lymphatic transport (O’driscoll and Griffin 2008). As CXB is categorized as a BCS Class II drug, the S-SEDDS formulation can contribute greatly to the increased dissolution of CXB in the GI tract, and it can also have an additive influence on intestinal permeability (Gursoy and Benita 2004; Gao et al. 2003). Meanwhile, the inhibition of efflux transporters is not a major concern in the CXB absorption study because CXB is not a substrate of P-glycoprotein, which is one of the representative efflux transporters (de Vries et al. 2007). Our previous study demonstrated that S-SEDDS formulations provided increased maximum dissolution as well as delayed drug precipitation compared with both the CXB capsule dosage formulation and conventional SEDDS formulation. In this study, in situ intestinal permeability and in vivo pharmacokinetics of various kinds of CXB-containing formulations including SEDDS and S-SEDDS were evaluated in order to demonstrate the influence of these ingredients on drug absorption and oral BA.
For a successful SPIP experiment, the drug molecule should be in solubilized form and there should be no adsorption to the tubing for accurate estimation of the intestinal permeability of the drug (Zakeri-Milani et al. 2007; Kang et al. 2012). In this study, all perfusion solutions were maintained in the solution state without drug crystallization or precipitation throughout the experiment, as CXB was solubilized by micelle formation or the SEDDS formulation. CXB is a poorly water-soluble drug since its solubility in water is 3–7 μg/mL (Subramanian et al. 2004). The use of a cosolvent like 30 v/v% methanol increased the solubility of CXB up to 10 μg/mL (Shakeel et al. 2007). In contrast, by the addition of 2.5 v/v% Tween 20 as a surfactant, its solubility was increased over 40 μg/mL due to micellar solubilization: the critical micelle concentration of Tween 20 in aqueous solution was reported as 60 mg/L (Ullah et al. 2011). Self-emulsification further contributed to solubilize the drug. Even though the total amount of surfactant added to the SEDDS or S-SEDDS solutions was considerably less than the amount of Tween 20 added to the control solution, the formation of emulsion droplets improved CXB solubility. This result is highly consistent with the dissolution behavior reported earlier (Song et al. 2013).
The selected SEDDS has the desirable properties of small droplet size upon dispersion and high solubilization capacity. The spontaneous formation of an emulsion in the GI tract maintains drug molecules in their dissolved state to a high degree and the small droplet size provides a large interfacial surface area for drug absorption (Charman et al. 1992; Shah et al. 1994). It was reported that surfactants used in the SMEDDS formulation not only improve solubilization of a drug but also increase drug permeability by causing reversible injury in biological cell membranes and reducing the thickness of the unstirred aqueous layer (Swenson and Curatolo 1992; Yao et al. 2008). Similarly, as listed in Table 2, the Peff value of CXB was significantly increased by the SEDDS formulation. Since CXB belongs to the BCS Class II, with drugs in this class having the property of low solubility and high permeability, solubilization is a crucial factor for enhancing CXB absorption. Nevertheless, permeation enhancement also could contribute to the increase in the oral BA of CXB. The Peff value of CXB (6.39 × 10−5 cm/s) is similar to that of other BCS Class II drugs such as ketoprofen (9.7 × 10−5 cm/s) and naproxen (11.7 × 10−5 cm/s), which were measured by an SPIP study as a surfactant-free solution state (Zakeri-Milani et al. 2005). Although CXB was micellar solubilized in this experiment, its Peff value still remained at a similar level with other anti-inflammatory drugs. Therefore, we assumed that the surfactant alone was less effective in enhancing the intestinal permeation of CXB. On the other hand, the permeability of CXB was significantly increased (P < 0.05) by the lipid-based formulation, yielding a 1.5- to 2.9-fold increase for the SEDDS or S-SEDDS formulations, respectively, compared to the control solution.
Stabilization of the micellar structure or emulsion droplet by the employment of amphiphilic polymers is well recognized to enhance not only the solubilization capacity but also the intestinal absorption of hydrophobic drug molecules (Brusewitz et al. 2007; Chen et al. 2013). Soluplus which is a recently introduced supersaturating agent for inhibiting drug crystallization acts like a surfactant, since it possesses both hydrophilic and hydrophobic groups in its structure. In this regards, a stabilizing mechanism of Soluplus at the interface of the dispersed droplets was proposed in our earlier report (Song et al., 2013). Tween 20 (surfactant) and Tetraglycol (cosurfactant) played the most important role in stable self-emulsification, and Soluplus further contributed to optimize the S-SEDDS formulation through the formation of mixed micellar structures. The polycaprolactam moiety of the Soluplus hydrophobic group intercalates to the hydrophobic tail packing, and the hydrophilic head group of polyethylene glycol is arranged on the surface of the emulsion droplets. In the aspect of CXB dissolution, with S-SEDDS, the maximum level of drug dissolution increased by a large factor (to approximately 90 %) compared with SEDDS (maximum dissolution was about 20 %). Chen et al. (2013) reported that Pluronic P105/F127 mixed micelles used for the delivery of docetaxel improved drug solubilization and increased the plasma concentration. Linn et al. (2012) reported that Soluplus improved intestinal absorption of BCS Class II drugs including danazol, fenofibrate and itraconazole for which both the in vivo absorption in beagle dogs and in vitro transport across Caco-2 cell monolayers were tested. It was reported that polymers may interact with surfactants and enhance their solubility properties (Saito 1967; Attwood and Florence 1983; Jones 1968; Arai et al. 1971). The synergic interaction of Soluplus and the SEDDS vehicle including Tween 20 might enhance the dissolution profile and intestinal permeability as well.
Four types of different samples such as CXB suspension, Celebrex suspension, SEDDS, and S-SEDDS were administered orally to rats and their pharmacokinetic parameters were compared. The relative BA of SEDDS was 263 % compared to CXB suspension, used as a reference. SEDDS also produced relatively higher plasma concentrations up until 3 h later than Celebrex suspension. This might be induced by the enhanced dissolution and permeability of CXB. However, the relative BA of SEDDS was similar to that of Celebrex suspension. In the SPIP experiment, a surfactant-free simulated intestinal fluid (pH 7.4) was used for the evaluation of supersaturation, but this medium can not reflect the physiology of the GI tract. Rats have no gall bladder and always secret bile salt regardless of food intake. Bile salt usually plays a crucial role in the solubilization of poorly water soluble drugs. It was reported that CXB can be absorbed throughout the whole GI tract (Paulson et al. 2001). Besides, it was reported that the Celebrex® capsule was designed to improve the oral absorption of CXB in the following ways: (1) particle size reduction of CXB by milling; (2) enhanced wettability of CXB by the addition of an adjuvant, sodium lauryl sulfate, as a surfactant; (3) enhanced dissolution by the help of a hydrophilic polymer and superdisintegrant (Gao et al. 2003). Therefore, the BA of the Celebrex suspension was significantly higher than that of CXB suspension but similar with that of SEDDS. Meanwhile, Soluplus improved not only the intestinal permeability but also the supersaturating state in the CXB-dissolved SEDDS formulation. The essential steps of supersaturating drug delivery systems comprise the enhancement of the dissolution level (spring) and the inhibition of drug precipitation (parachute). The S-SEDDS formulation showed fast Tmax and significantly improved oral absorption of CXB compared to CXB suspension, Celebrex suspension, and SEDDS. The increased plasma concentration in the upper GI tract resulting in the fast Tmax may be attributed to the spring effect. This result may indicate the fast onset of the pharmacological effect, especially useful in the treatment of acute pain.
There are numerous reports that BA enhancement generally correlates with increase in intestinal permeability of a drug. Kang et al. (2012) found strong correlation between in situ jejunal permeability and in vivo AUC of olmesartan medoxomil in rats. Zakeri-Milani et al. (2007) observed a high correlation of rat jejunum permeability with the fraction of the oral dose absorbed in humans for 13 different drugs covering all types of BCS classes. We observed that in situ jejunal Peff values were linearly correlated with in vivo AUC in rats (r2 = 0.853), as shown in Fig. 3a. On the other hand, correlations between BA increase and solubility enhancement should be taken into consideration. Especially for poorly soluble drugs like BCS Class II drugs, aqueous solubilization becomes more important since dissolution is the rate-limiting step for drug absorption in the gut. Biorelevant dissolution can be used to successfully predict the in vivo behavior of poorly soluble drugs such as danazol, ketoconazole, atovaquone and troglitazone (Dressman and Reppas 2000). Based on the dissolution data reported earlier (Song et al. 2013), the dissolution efficiency of CXB in various formulations were calculated according to the equation proposed by the literature (Khan and Rhodes 1975). As depicted in Fig. 3b, excellent correlations (r2 = 0.996) between in vivo oral BA expressed as AUC values and in vitro dissolution efficiency for 2 h were obtained. In particular, S-SEDDS revealed the highest value in all aspects covering in vivo oral BA, in situ intestinal permeability, and in vitro dissolution efficiency. Therefore, the self-emulsifying lipid-based DDS, particularly S-SEDDS, would be a selectable candidate for the formulation of poorly soluble compounds by virtue of its ability to produce significant improvements in both aqueous solubility and intestinal permeability. In future, this study would be possibly extended to the formulation of various kinds of poorly water-soluble drugs such as itraconazole, albendazole, paclitaxel, tacrolimus, dutasteride, and etc.
Correlations between in vivo oral BA and in situ permeability a or in vitro dissolution efficiency b for various formulations of CXB. Dissolution efficiency (D.E.) proposed by Khan and Rhodes in 1975 is defined as follows: \( {\text{D}}.{\text{E}}.\left( \% \right) = \left[ {\int\limits_{\text{t1}}^{{{\text{t}}2}} {{\text{y dt /y}}_{100} \cdot ({\text{t}}2 - {\text{t}}1)} } \right] \times 100 \), where y is the percentage of dissolved product. D.E. is then the area under the dissolution curve between time points t1 and t2 expressed as a percentage of the curve at maximum dissolution, y100, over the same time period
Conclusion
An in situ intestinal permeability study and an in vivo absorption study in rats were successfully performed with CXB-dissolved SEDDS and S-SEDDS formulations. The addition of Soluplus as a supersaturating agent to SEDDS, composed of Capryol 90, Tween 20 and Tetraglycol, resulted in a positive effect on the intestinal permeability as well as the dissolution of CXB, as shown by a significantly higher oral BA compared to other formulations including CXB suspension, Celebrex suspension, and SEDDS. This study illustrates the potential use of the S-SEDDS formulation in the oral delivery of poorly water-soluble compounds.
References
Amidon, G.L., H. Lennernas, V.P. Shah, and J.R. Crison. 1995. A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharmaceutical Research 12: 413–420.
Arai, H., M. Murata, and J. Shinoda. 1971. The interaction between polymer and surfactant: the composition of the complex between polyvinylpyrrolidone and sodium alkyl sulfate as revealed by surface tension, dialysis, and solubilization. Journal of Colloid and Interface Science 37: 223–227.
Attwood, D., and A.T. Florence. 1983. Surfactant systems: their chemistry, pharmacy and biology. New York: Chapman and Hall.
Berggren, S., J. Hoogstraate, U. Fagerholm, and H. Lennernas. 2004. Characterization of jejunal absorption and apical efflux of ropivacaine, lidocaine and bupivacaine in the rat using in situ and in vitro absorption models. European Journal of Pharmaceutical Sciences 21: 553–560.
Brouwers, J., M.E. Brewster, and P. Augustijns. 2009. Supersaturating drug delivery systems: the answer to solubility-limited oral bioavailability? Journal of Pharmaceutical Sciences 98: 2549–2572.
Brusewitz, C., A. Schendler, A. Funke, T. Wagner, and R. Lipp. 2007. Novel poloxamer-based nanoemulsions to enhance the intestinal absorption of active compounds. International Journal of Pharmaceutics 329: 173–181.
Charman, S.A., W.N. Charman, M.C. Rogge, T.D. Wilson, F.J. Dutko, and C.W. Pouton. 1992. Self-emulsifying drug delivery systems: formulation and bio-pharmaceutical evaluation of an investigational lipophilic compound. Pharmaceutical Research 9: 87–93.
Chen, L., X. Sha, X. Jiang, Y. Chen, Q. Ren, and X. Fang. 2013. Pluronic P105/F127 mixed micelles for the delivery of docetaxel against Taxol resistant non-small cell lung cancer: optimization and in vitro, in vivo evaluation. International Journal of Nanomedicine 8: 73–84.
Chiou, W.L., and A. Barve. 1998. Linear correlation of the fraction of oral dose absorbed of 64 drugs between humans and rats. Pharmaceutical Research 15: 1792–1795.
Clemett, D., and K.L. Goa. 2000. Celecoxib: a review of its use in osteoarthritis, rheumatoid arthritis and acute pain. Drugs 59: 957–980.
de Vries, N.A., J. Zhao, E. Kroon, T. Buckle, J.H. Beijnen, and O. van Tellingen. 2007. P-glycoprotein and breast cancer resistance protein: two dominant transporters working together in limiting the brain penetration of topotecan. Clinical Cancer Research 13: 6440–6449.
Dressman, J.B., and C. Reppas. 2000. In vitro-in vivo correlations for lipophilic, poorly water-soluble drugs. European Journal of Pharmaceutical Sciences 11: S73–S80.
Fagerholm, U., M. Johansson, and H. Lennernas. 1996. Comparison between permeability coefficients in rat and human jejunum. Pharmaceutical Research 13: 1336–1342.
Gao, P., B.D. Rush, W.P. Pfund, T. Huang, J.M. Bauer, W. Morozowich, M.S. Kuo, and M.J. Hageman. 2003. Development of a supersaturable SEDDS(S-SEDDS) formulation of paclitaxel with improved oral bioavailability. Journal of Pharmaceutical Sciences 92: 2386–2398.
Gursoy, R.N., and S. Benita. 2004. Self-emulsifying drug delivery systems (SEDDS) for improved oral delivery of lipophilic drugs. Biomedicine & Pharmacotherapy 58: 173–182.
Guzman, H.R., M. Tawa, Z. Zhang, P. Ratanabanangkoon, P. Shaw, C.R. Gardner, H. Chen, J.P. Moreau, O. Almarsson, and J.F. Remenar. 2007. Combined use of crystalline salt forms and precipitation inhibitors to improve oral absorption of celecoxib from solid oral formulations. Journal of Pharmaceutical Sciences 96: 2686–2702.
Hillgren, K.M., A. Kato, and R.T. Borchardt. 1995. In vitro systems for studying intestinal drug absorption. Medicinal Research Reviews 15: 83–109.
Jones, M.N. 1968. Dye solubilization by a polymer-surfactant complex. Journal of Colloid and Interface Science 26: 532–533.
Kang, M.J., H.S. Kim, H.S. Jeon, J.H. Park, B.S. Lee, B.K. Ahn, K.Y. Moon, and Y.W. Choi. 2012. In situ intestinal permeability and in vivo absorption characteristics of olmesartan medoxomil in self-microemulsifying drug delivery system. Drug Development and Industrial Pharmacy 38: 587–596.
Khan, K.A., and C.T. Rhodes. 1975. The concept of dissolution efficiency. Journal of Pharmacy and Pharmacology 27: 48–49.
Karlsson, J., and P. Artursson. 1991. A method for the determination of cellular permeability coefficients and aqueous boundary layer thickness in monolayers of intestinal epithelial (Caco-2) cells grown in permeable filter chambers. International Journal of Pharmaceutics 71: 55–64.
Komiya, I., J.Y. Park, A. Kamani, N.F.H. Ho, and W.I. Higuchi. 1980. Quantitative mechanistic studies in simultaneous fluid flow and intestinal absorption using steroids as model solutes. International Journal of Pharmaceutics 4: 249–262.
Lennernas, H., O. Ahrenstedt, R. Hallgren, L. Knutson, M. Ryde, and L.K. Paalzow. 1992. Regional jejunal perfusion, a new in vivo approach to study oral drug absorption. Pharmaceutical Research 9: 1243–1251.
Linn, M., E.M. Collnot, D. Djuric, K. Hempel, E. Fabian, K. Kolter, and C.M. Lehr. 2012. Soluplus® as an effective absorption enhancer of poorly soluble drugs in vitro and in vivo. European Journal of Pharmaceutical Sciences 45: 336–343.
O’driscoll, C.M., and B.T. Griffin. 2008. Biopharmaceutical challenges associated with drugs with low aqueous solubility—the potential impact of lipid-based formulations. Advanced Drug Delivery Reviews 60: 617–624.
Paulson, S.K., M.B. Vaughn, S.M. Jessen, Y. Lawal, C.J. Gresk, B. Yan, T.J. Maziasz, C.S. Cook, and A. Karim. 2001. Pharmacokinetics of celecoxib after oral administration in dogs and humans: effect of food and site of absorption. Journal of Pharmacology and Experimental Therapeutics 297: 638–645.
Pouton, C.W. 2006. Formulation of poorly water-soluble drugs for oral administration: physicochemical and physiological issues and the lipid formulation classification system. European Journal of Pharmaceutical Sciences 29: 278–287.
Rubas, W., N. Jezyk, and G.M. Grass. 1993. Comparison of the permeability characteristics of a human colonic epithelial (Caco-2) cell line to colon of rabbit, monkey, and dog intestine and human drug absorption. Pharmaceutical Research 10: 113–118.
Saito, S. 1967. Solubilization properties of polymer-surfactant complexes. Journal of Colloid and Interface Science 24: 227–234.
Salphati, L., K. Childers, L. Pan, K. Tsutsui, and L. Takahashi. 2001. Evaluation of a single-pass intestinal-perfusion method in rat for the prediction of absorption in man. Journal of Pharmacy and Pharmacology 53: 1007–1013.
Shah, N.H., M.T. Carvajal, C.I. Patel, M.H. Infeld, and A.W. Malick. 1994. Self-emulsifying drug delivery systems with polyglycolyzed glycerides for improving in vitro dissolution and oral absorption of lipophilic drugs. International Journal of Pharmaceutics 106: 15–23.
Shakeel, F., S. Baboota, A. Ahuja, J. Ali, M. Aqil, and S. Shafiq. 2007. Nanoemulsions as vehicles for transdermal delivery of aceclofenac. AAPS PharmSciTech 8: 191–199.
Song, W.H., J.H. Park, D.W. Yeom, B.K. Ahn, K.M. Lee, S.G. Lee, H.S. Woo, and Y.W. Choi. 2013. Enhanced dissolution of celecoxib by supersaturating self-emulsifying drug delivery system (S-SEDDS) formulation. Archives of Pharmacal Research 36: 69–78.
Subramanian, N., S. Ray, S.K. Ghosal, R. Bhadra, and S.P. Moulik. 2004. Formulation design of self-microemulsifying drug delivery systems for improved oral bioavailability of celecoxib. Biological and Pharmaceutical Bulletin 27: 1993–1999.
Swenson, E.S., and W.J. Curatolo. 1992. Intestinal permeability enhancement for proteins, peptides and other polar drugs: mechanisms and potential toxicity. Advanced Drug Delivery Reviews 8: 39–92.
Ullah, I., M.K. Baloch, and G.F. Durrani. 2011. Solubility of nonsteroidal anti-inflammatory drugs (NSAIDs) in aqueous solution of non-ionic surfactants. Journal of Solution Chemistry 40: 1341–1348.
Vasconcelos, T., B. Sarmento, and P. Costa. 2007. Solid dispersions as strategy to improve oral bioavailability of poor water soluble drugs. Drug Discovery Today 12: 1068–1075.
Yao, J., Y. Lu, and J.P. Zhou. 2008. Preparation of nobiletin in self-microemulsifying systems and its intestinal permeability in rats. Journal of Pharmacy and Pharmaceutical Sciences 11: 22–29.
Zakeri-Milani, P., M. Barzegar-Jalali, H. Tajerzadeh, Y. Azarmi, and H. Valizadeh. 2005. Simultaneous determination of naproxen, ketoprofen and phenol red in samples from rat intestinal permeability studies: HPLC method development and validation. Journal of Pharmaceutical and Biomedical Analysis 39: 624–630.
Zakeri-Milani, P., H. Valizadeh, H. Tajerzadeh, Y. Azarmi, Z. Islambolchilar, S. Barzergar, and M. Barzegar-Jalali. 2007. Predicting human intestinal permeability using single-pass intestinal perfusion in rat. Journal of Pharmacy and Pharmaceutical Sciences 10: 368–379.
Acknowledgments
This research was supported by the Chung-Ang University Research Scholarship Grants in 2013.
Author information
Authors and Affiliations
Corresponding author
Additional information
W. H. Song and D. W. Yeom have contributed equally to this study.
Rights and permissions
About this article
Cite this article
Song, W.H., Yeom, D.W., Lee, D.H. et al. In situ intestinal permeability and in vivo oral bioavailability of celecoxib in supersaturating self-emulsifying drug delivery system. Arch. Pharm. Res. 37, 626–635 (2014). https://doi.org/10.1007/s12272-013-0202-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12272-013-0202-7