Abstract
A prospective, observational single-center study was carried out. Pediatric patients undergoing congenital heart defect surgery were evaluated before, during, and after surgery. At each time point, sublingual microcirculation and clinical parameters were assessed, along with analytical variables. Twenty-four patients were included. All microcirculatory parameters worsened during cardiopulmonary bypass and returned to baseline values after surgery (p ≤ 0.001). In the intraoperative evaluation, body temperature correlated with perfused small vessel density (p = 0.014), proportion of perfused small vessels (p < 0.001), small vessel microvascular flow index (p = 0.003), and small vessel heterogeneity index (p < 0.002). Patients with cyanotic disease exhibited higher small vessel density (p < 0.008) and higher density of perfused small vessels (p < 0.022) at baseline, and a lower microvascular flow index (p = 0.022) and higher heterogeneity (p = 0.026) in the intraoperative phase. Children with congenital heart disease exhibited decreased vascular density and microvascular blood flow and increased heterogeneity during cardiopulmonary bypass. All these parameters returned to baseline values after surgery.
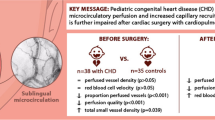
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The microcirculatory system is composed of small arterioles, capillaries, and venules that mediate the exchange of materials between the blood and the tissues of the body. The adequate functioning of the microvascular compartment has been proven to be crucial for adequate organ function. Hence, microcirculatory compartment dysfunction has been associated with different life-threatening conditions, especially in critically ill patients [1,2,3].
Microcirculatory changes in patients who undergo cardiac surgery have been described in previous studies. However, most studies only involved adult patients subjected to coronary reperfusion surgery and heart valve replacement [4,5,6,7,8,9,10,11,12]. The literature on the impact of cardiopulmonary bypass (CPB) on microcirculation in pediatric patients undergoing cardiac surgery is scarce [13,14,15]. Compromised microcirculation secondary to CPB is associated with multiple factors such as the type of flow used for CPB, hemostatic alterations, hypothermia, and use of hemoderivatives or vasoactive drugs, to name a few.
The primary objective of this study was to describe changes in sublingual microcirculation using videomicroscopy during corrective surgery for congenital heart disease in pediatric patients. A secondary objective was to assess if the microcirculatory changes were associated with the postoperative course of patients. The influence of some surgical factors such as age and type of heart disease on perioperative microcirculatory changes was also evaluated.
Methods
A single-center, observational, prospective study was performed. The study was carried out in a tertiary care hospital, which is a national referral center for the treatment for pediatric patients with congenital heart disease. The study was approved by the Institutional Review Board. This manuscript adheres to the applicable STROBE guidelines for reporting observational studies.
The study included patients with ages ranging from 1 month to 18 years admitted to the pediatric intensive care unit (PICU) who underwent elective corrective surgery for congenital heart defects. Written informed consent was obtained from patients or their legal representative, as appropriate. Exclusion criteria included the presence of alterations in the oral cavity, a difficult airway, or refusal to take part in the study.
To calculate the sample size, the microcirculatory flow index (MFI) was defined as the main variable of interest. To detect a mean difference of 0.5 points between two groups with a standard deviation similar to that found in similar studies, establishing a statistical power of 80%, at least 22 patients should be included.
All patients were evaluated at three time points throughout the perioperative period:
-
Baseline evaluation (T0): prior to surgery and after endotracheal intubation and central venous and arterial catheterization. During evaluation, anesthesia/sedation had been induced with sevoflurane in all patients.
-
Intraoperative evaluation (T1): during CPB when the planned minimum core temperature was reached. Sublingual microcirculation was assessed by accessing the oral cavity under the surgical field from the head of the surgery bed.
-
Postoperative evaluation (T2): after surgery, once the surgical bed had been withdrawn and prior to planned extubation, when possible. Postoperative evaluation was carried out in the operating room prior to patient’s transfer to the PICU.
Anesthetic and surgical procedures were carried out according to the usual practice of the cardiovascular surgery team, who was blinded to microcirculatory measurements. All other variables collected are part of routine monitoring used during cardiovascular surgery procedures in our center. No clinical intervention was derived from the measurements performed for the study.
Variables Collected
The preoperative variables collected included age, height, body surface area, weight, and previous cardiologic diagnosis. Patients were classified as cyanotic when their heart defect allowed deoxygenated blood to bypass lung circulation reaching the systemic circulation and as non-cyanotic when systemic and pulmonary circulations were completely separated. Variables related to surgery included surgical complexity based on Aristotle Basic and Aristotle Comprehensive scale, duration of the procedure, duration of CPB, duration of aortic clamping, and minimum temperature reached during surgery. Variables related to the postoperative course of patients included length of PICU stay, length of hospital stay, need for and duration of vasoactive therapy in PICU, need for and duration of postoperative mechanical ventilation, and mortality.
Sublingual microcirculation was assessed at each time point (T0, T1, and T2) using a sidestream dark-field (SDF) microscope (MicroScan, MicroVision Medical Inc., Amsterdam, Netherlands). Five 10-s video sequences were recorded at each time point. Videomicroscopy images were recorded and analyzed using the Automated Vascular Analysis AVA 3.1 software (MicroVision Medical Inc., Amsterdam, Netherlands). Videomicroscopy sequences were recorded in accordance with standard recommendations [16, 17].
All sequences were recorded and analyzed by the same operator (R.G.) which was not participating in the surgical procedure. Patient’s identity data and the time point at which sequences had been recorded were eliminated from video sequences before evaluation.
After images were stabilized and gray balance was adjusted, the vessels observed were identified and outlined manually. The microcirculatory variables assessed were those established in current recommendations for the evaluation of microcirculation. Total vessel density (TVD), De Backer score (DB), perfused vessel density (PVD), proportion of perfused vessels (PPV), microcirculatory flow index (MFI), and heterogeneity index (HI) were determined in each set of video sequences. All microcirculation variables were measured in vessels below 20 μm diameter, which were classified as small vessels (SV), and all vessels (with a diameter above and below 20 μm) except for De Backer score, which was measured in all the vessels studied.
Other variables apart from microcirculatory parameters included macrohemodynamic parameters (systolic, diastolic, and mean arterial pressure; central venous pressure; and pump flow at the intraoperative measurement); variables related to mechanical ventilation (PEEP, PIP, and FiO2); variables of perfusion and tissue oxygenation (core temperature and brain and somatic oximetry by near infrared photospectrometry (NIRS) measured using INVOS 5100C, Medtronic Somanetics, Minneapolis, MN, USA); and analytical parameters in arterial blood (pH, pCO2, pO2, HCO3, base excess, arterial saturation of oxygen, glycemia, hematocrit and concentration of hemoglobin, lactate, sodium, potassium, chlorine, and ionic calcium). Additionally, the medication that patients were receiving at each assessment point was recorded and vasoactive inotropic score (VIS) was calculated for each time point [18] .
Statistical Analysis
The variables collected were entered into an electronic database and analyzed using the statistical analysis software SPSS Statistics for OsX (IBM Corp. Released 2013. Version 22.0. Armonk, NY). p values < 0.05 were considered statistically significant.
For a descriptive study of the sample, median values were used as a measure of central tendency, whereas interquartile range (IQR) was used as a measure of dispersion. Student’s t test was used to perform paired comparisons of mean values to study variations in continuous quantitative variables at the different measurement points. 95% confidence intervals (CI95%) were calculated to assess differences between means. Correlations between variables were assessed by Spearman’s correlation coefficient (Spearman’s rho) for simple correlations and by partial correlation coefficient in those correlations where adjustments were made as a function of other variables. Differences between subgroups were assessed using Student’s t test for continuous quantitative variables and chi-square test for qualitative variables.
Results
The study included 24 patients subjected to cardiac surgery with CPB, of whom 18 were male (75%). Table 1 shows the baseline characteristics of the patients. Thirteen patients (54.2%) had cyanotic heart disease. Details regarding congenital heart defect and surgical intervention for each patient are expressed in Table 2. No patient required inotropic support during the baseline evaluation. Median VIS during the intraoperative evaluation was 0 points (0–5), and 12 points (7–15) during the postoperative evaluation.
Changes in Microcirculatory Parameters During Surgery
Table 3 shows the changes in the different parameters during CPB and after the procedure with respect to baseline values. During CPB, a reduction was observed in vascular density parameters (TVD, PVD, and Backer’s score) and blood flow at microcirculatory level (MFI and PPV), while heterogeneity (HI) increased (Fig. 1). Differences were observed between cyanotic and acyanotic heart disease patients (Fig. 2): cyanotic patients had lower small vessel MFI and increased small vessel HI during the intraoperative evaluation. Variation on microcirculatory parameters between baseline and intraoperative evaluations was calculated for each patient. Patients with cyanotic heart defects showed greater decrease in small vessel PVD (p = 0.040), total PVD (p = 0.030), and small vessel MFI (p = 0.045) than acyanotic patients.
Comparison of microcirculatory parameters at the different time points of the study between patients with cyanotic heart disease and non-cyanotic heart disease. p values are referred to comparison of median between groups. TVD total vessel density, PVD perfused vessel density, PPV proportion of perfused vessels, MFI microvascular flow index, HI heterogeneity index
Microcirculatory changes were also compared between patients undergoing single ventricle repair (Glenn and Fontan procedures) and those undergoing biventricular repair. Patients undergoing single ventricle repair showed greater mean decrease between baseline and postoperative for TVD (4.5 mm2/mm2, IC95% 0.5–8.4; p = 0.047) and for small vessel PVD (5.9 mm2/mm2, CI95% 1.15–10.7; p = 0.047), as compared to patients with biventricular strategies. Patients with single ventricle surgical repair also showed a greater decrease in small vessel PVD during the intraoperative evaluation (difference of means of 7.5 mm2/mm2, CI95% 1.6–13.5; p = 0.044).
Correlation Between Microcirculatory and Macrohemodynamic Parameters
Several multivariate models were developed to analyze the effect of the different surgery variables on microcirculatory parameters. Total hemoglobin values did not correlate with microcirculatory parameters after adjustment for mean blood pressure and core temperature. In contrast, core temperature correlated with microcirculatory parameters after adjustment for mean blood pressure and hemoglobin concentration (Table 4). Mean blood pressure showed a correlation with heterogeneity indices after adjustment for temperature and total hemoglobin concentration (Table 4). When all measurements were analyzed together, lactate values showed moderate correlation with MFI values (rho = − 0.338; p = 0.027) but did not show correlation with other microcirculatory parameters. Arterial partial pressure of oxygen did not show any correlation with microcirculatory parameters. Cerebral oxygenation index measured by NIRS showed moderate correlation with MFI (rho = 0.362; p = 0.016) but not with other microcirculatory parameters. Postoperative lactate values showed no correlation with microcirculatory parameters except for small vessel HI (rho = − 0.513; p = 0.030). Somatic oxygenation index showed no correlation with any microcirculatory variable.
Prognostic Capacity and Relationship of Microcirculatory Parameters and Surgical Variables
In the intraoperative period, none of the microcirculatory parameters studied showed a correlation with length of PICU or hospital stay, duration of vasoactive therapy, or mechanical ventilation during the postoperative period.
In the postoperative measurement, a higher MFI correlated with a lower length of hospital stay (rho = − 0.470; p = 0.036) and a lower duration of mechanical ventilation during the postoperative period (rho = − 0.785; p < 0.001). Postoperative MFI was also inversely related to Aristotle basic score (rho = − 0.653; p = 0.002) and Aristotle comprehensive score (rho = − 0.566; p = 0.009) and with the minimum temperature reached (rho = − 0.491; p = 0.033).
In the postoperative measurement, some surgical variables were associated with poorer values of microcirculation parameters with respect to baseline. Aristotle comprehensive score was higher in patients who showed a worsening of small vessel density (p = 0.03), De Backer score (p = 0.035), and perfused small vessel density (p = 0.03).
A worsening of small vessel TVD (p = 0.022), PVD (p = 0.009), and small vessels PVD (0.001) was associated with a longer duration of the surgical procedure. The worsening of small vessel PVD (p = 0.036) and MFI (p = 0.027) was associated with a lower minimum core temperature. No relationship was observed between duration of CPB or duration of aortic clamping and a worsening of microcirculatory parameters.
There was no correlation between ventilatory and microcirculatory parameters. VIS showed no correlation with microcirculatory parameters during the intraoperative measurement but correlated with MFI during the postoperative evaluation (rho = − 0.540, p = 0.017).
Microvascular Blood Flow
Altered MFI measurements were studied. A MFI was considered to be abnormal when < 2.6 as defined by Vellinga et al. [19].
Figure 3 shows the proportion of patients with MFI alterations at the different measurement points. None of the intraoperative variables showed a correlation with the existence of MFI or MFIsv alterations. MFIsv alterations were found to be more frequent during the intraoperative evaluation in cyanotic patients than in acyanotic patients (92.3% vs 45.5%, p = 0.023).
The existence of abnormal MFI or MFIsv was not related to higher lactate levels during the postoperative evaluation. The presence of an MFI or MFIsv below 2.6 in the postoperative evaluation was not associated with longer duration of admission to the PICU or hospital or with a longer time of use of mechanical ventilation or vasoactive drugs.
Influence of Age on Microcirculatory Parameters
Age correlated with baseline MFI (rho = 0.518; p = 0.010) and MFIsv (rho = 0.414; p = 0.044). None of the other microcirculatory parameters correlated with age at baseline, intraoperatively or postoperatively. Differences were not observed either in the median age of patients with MFI or MFIsv alterations and those without abnormal MFI or MFIsv.
Discussion
Changes in Microcirculation Related to Cardiac Surgery
This study describes microcirculatory changes in pediatric patients with a diversity of congenital heart diseases, who underwent cardiac surgery with CPB. Significant alterations occurred in all microcirculatory parameters during CPB. Thus, we observed a reduction in vascular density, proportion of perfused vessels, and microcirculatory blood flow, whereas heterogeneity increased. These alterations indicate a reduced supply of oxygen and nutrients to tissues. The changes observed suggest a diminished convective capacity (as a result of the reduced blood flow and decreased number of perfused vessels) and difussive capacity (as vascular density decreases and distance between vessels and cells increases). In contrast, heterogeneity in microcirculation was augmented.
In this study, microcirculatory parameters returned to baseline values after surgery. Our results are consistent with those of a recent systematic review that included 19 studies on adult cardiac surgery patients [20]. Some studies in adult patients report that functional capillary density or the proportion of perfused vessels decreases during CPB but reverts to baseline values after surgery [4, 6, 10]. Other studies document a worsening of microvascular blood flow index [12] or an increase in heterogeneity [10].
Some studies have explored microcirculatory changes by videomicroscopy in pediatric cardiac surgery patients [13, 14]. Scolletta et al. and Nussbaum et al. examined microcirculation by videomicroscopy prior to CPB and after the procedure. However, none of the authors examined variations in microcirculatory parameters during CPB. Scolletta did not observe any variations in microcirculatory parameters in baseline values after anesthesia induction and postoperative values (prior to transfer to the ICU) [14]. Nussbaum reported a reduced perfused vessel density and microvascular blood flow after surgery in the first hour of stay in the ICU with respect to baseline values [13]. Inconsistency of results may be explained by the fact that preoperative measurements were performed in different settings. In the study by Scolletta et al., baseline measurements were made after anesthesia induction, whereas in the study by Nussbaum et al. were made the day before the intervention. Several studies have documented that anesthesia induction has an impact on microcirculation [21,22,23,24,25].
Effect of Cardiac Surgery on Other Monitoring Parameters
In our study, we observed that the behavior of other parameters routinely used for monitoring cardiac surgery patients was different from that observed in microcirculatory parameters. The case of lactate deserves special attention. In our study, lactate was found to be altered in the intraoperative phase and remain abnormal in the postoperative phase. This indicates that the increase in lactate levels may persist although tissue hypoperfusion is solved. Additionally, postoperative lactate values showed negative correlation with microcirculatory heterogeneity: patients with higher small vessel heterogeneity (which is considered a sign of microcirculatory impairment) showed lower lactate levels. These findings suggest that the use of lactate alone as a guiding parameter of hemodynamic resuscitation may result in inadequate resuscitation [26,27,28].
Differences in the Microcirculatory Behavior According to the Type of Heart Disease
In our study, we compared the evolution during surgery of microcirculatory parameters between patients with cyanotic heart disease and patients with acyanotic heart disease. Cyanotic patients exhibited a higher baseline vascular density. This finding, which probably indicates a chronic adaptation to hypoxemia, had been previously described in a previous study [29]. However, the most striking difference between groups was that cyanotic patients exhibited lower microvascular blood flow and higher microcirculatory heterogeneity during CPB than acyanotic patients. This suggests that the microcirculation of cyanotic patients has a more limited capacity to respond to acute aggressions despite their higher vascular density. These findings are in agreement with those of Ugenti et al. [15]. Furthermore, patients undergoing single ventricle surgery showed greater microcirculatory changes.
Prognostic Capacity of Microcirculatory Parameters
In our study, we observed that postoperative microcirculatory parameters are associated with different prognostic variables. Although causality relationships cannot be established, in our series, the course of the patients with poorer postoperative microcirculation was less favorable than in other patients. The association of microcirculatory variables and prognostic variables opens an avenue for future research to determine whether a lower impact on microcirculation is associated with a favorable postoperative course, as in other diseases [2, 3].
Effect of Surgical Variables on Microcirculation
Further studies are needed to determine how to optimize microcirculatory parameters during cardiac surgery. In our study, we describe how baseline MFI prior to CPB is directly related to blood pressure. Similarly, a direct relationship was observed between higher hemoglobin concentrations and higher vascular density, whereas hemoglobin is indirectly related to the proportion of perfused vessels. These apparently contradictory findings can be explained by the fact that vascular density is higher in patients with cyanotic heart disease in the same way as hemoglobin concentrations are higher in patients with chronic hypoxemia. Likewise, in patients with cyanotic heart disease, a higher blood viscosity caused by higher hemoglobin concentrations may result in a lower proportion of perfused vessels.
During the intraoperative phase, we only found an association between diastolic blood pressure and MFI. It is necessary to investigate how the treatments and strategies used to modify vascular resistances with effects on blood pressure directly influence the microcirculatory flow [5, 30]. In our study, patients with higher postoperative use of vasoactive drugs showed decreased microcirculatory blood flow. However, the design of our study does not allow to establish causality in this relationship.
Decrease in body temperature was associated with impaired microcirculatory parameters, regardless of blood pressure and hemoglobin concentrations. Therapeutic hypothermia has been previously associated with a worsening of microcirculatory parameters in children after cardiac arrest [31] and in neonates with ischemic hypoxic encephalopathy [32]. In the two studies, alterations reverted after body temperature was restored. However, hypothermia induces a decrease in metabolic needs, which is why it has been used for a long time as a protective mechanism during CPB.
Finally, our study demonstrates that patients with a high surgical complexity were more likely to exhibit a lower postoperative microcirculatory flow and vascular density
Clinical Relevance and Future Implications of Our Findings
According to our findings, videomicroscopy microcirculatory assessment of pediatric patients during heart surgery might be useful to identify patients with microcirculatory disturbances, which may be at higher risk of poor postoperative evolution. Development of reliable, real-time, bed-side automatized analysis software of videomicroscopy images is needed to enable its routine use.
The effect of different parameters during CPB, such as temperature, blood product use, and drugs, on the microcirculation should be evaluated. Furthermore, implementation of specific strategies directed to minimize microcirculatory alterations during CPB should be considered. The establishment of such strategies could potentially reduce the risk of microcirculatory dysfunction and adverse outcomes.
Limitations
The observational design of our study hinders that direct causal relationships be established between microcirculatory alterations and the other parameters observed. Likewise, although it is a single-center observational study conducted in a center where standard anesthetic and surgical procedures were performed, there may have been variations according to the staff involved in each procedure.
Although the sample of patients is high as compared to other series, the significant heterogeneity of the cohort limits the generalization of results. The baseline clinical status of patients or the degree of cyanosis was not considered in the analysis of the evolution of microcirculatory parameters. However, these factors may influence significantly the development and function of the microvascular compartment. Different subgroup analyses were performed in order to offset the heterogeneity of this study’s cohort. Additional studies including a greater and less heterogeneous sample size are necessary to adequately characterize the microcirculatory changes that occur during cardiac surgery in children.
Given the difficulty in assessing microcirculation in conscious pediatric patients, all measurements were made with the patients sedated in the context of surgery. Therefore, the results obtained may be influenced by the anesthetic procedures.
The acquisition and analysis of videomicroscopy sequences were performed in accordance with current recommendations [16, 17]. During image acquisition, the researchers avoided the presence of artifacts from secretions, pressure on vessels, or inadequate illumination. The sequences that did not meet quality standards were not considered for analysis.
The deferred analysis of videomicroscopy sequences was performed using a semi-automated software. All sequences were analyzed by the same operator. Although this could be a potential source of bias, the operator has extensive experience in the semi-automated analysis of videomicroscopy sequences as he has analyzed more than 500 sequences in previous studies [29, 33, 34]. This could reduce the risk of bias associated with the presence of different operators. To prevent additional bias, images were anonymized prior to the analysis of images.
Conclusions
CPB in a heterogeneous group of pediatric patients was associated with alterations in the microcirculatory compartment, including a reduced vascular density and microvascular blood flow and an increased heterogeneity. These alterations reversed after surgery and were associated with prognostic variables and clinical outcomes. The response of the microvascular compartment was different in cyanotic and acyanotic patients.
Abbreviations
- CHD:
-
Congenital heart defects
- CI95%:
-
95% confidence interval
- DB:
-
De Backer score
- FiO2 :
-
Fraction of inspired oxygen
- HI:
-
Heterogeneity index
- IQR:
-
Interquartile range
- MFI:
-
Microcirculatory flow index
- NIRS:
-
Near infrared photospectrometry
- PEEP:
-
Positive end expiratory pressure
- PICU:
-
Pediatric intensive care unit
- PIP:
-
Peak inspiratory pressure
- PPV:
-
Proportion of perfused vessels
- PVD:
-
Perfused vessel density
- SDF:
-
Sidestream dark-field imaging
- SV:
-
Small vessels
- TVD:
-
Total vessel density
- VIS:
-
Vasoactive inotropic score
References
Vellinga, N. A. R., Boerma, E. C., Koopmans, M., Donati, A., Dubin, A., Shapiro, N. I., et al. (2017). Mildly elevated lactate levels are associated with microcirculatory flow abnormalities and increased mortality: A microSOAP post hoc analysis. Critical Care, 21(1), 255. https://doi.org/10.1186/s13054-017-1842-7.
Trzeciak, S., Dellinger, R. P., Parrillo, J. E., Guglielmi, M., Bajaj, J., Abate, N. L., et al. (2007). Early microcirculatory perfusion derangements in patients with severe sepsis and septic shock: Relationship to hemodynamics, oxygen transport, and survival. Annals of Emergency Medicine, 49(1), 88–98.e2. https://doi.org/10.1016/j.annemergmed.2006.08.021.
De Backer, D., Donadello, K., Sakr, Y., Ospina-Tascon, G., Salgado, D., Scolletta, S., & Vincent, J.-L. (2013). Microcirculatory alterations in patients with severe sepsis: Impact of time of assessment and relationship with outcome. Critical Care Medicine, 41(3), 791–799. https://doi.org/10.1097/CCM.0b013e3182742e8b.
Bauer, A., Kofler, S., Thiel, M., Eifert, S., & Christ, F. (2007). Monitoring of the sublingual microcirculation in cardiac surgery using orthogonal polarization spectral imaging: preliminary results. Anesthesiology, 107(6), 939–945. https://doi.org/10.1097/01.anes.0000291442.69337.c9.
Maier, S., Hasibeder, W. R., Hengl, C., Pajk, W., Schwarz, B., Margreiter, J., et al. (2009). Effects of phenylephrine on the sublingual microcirculation during cardiopulmonary bypass. British Journal of Anaesthesia, 102(4), 485–491. https://doi.org/10.1093/bja/aep018.
De Backer, D., Dubois, M.-J., Schmartz, D., Koch, M., Ducart, A., Barvais, L., & Vincent, J.-L. (2009). Microcirculatory alterations in cardiac surgery: Effects of cardiopulmonary bypass and anesthesia. The Annals of Thoracic Surgery, 88(5), 1396–1403. https://doi.org/10.1016/j.athoracsur.2009.07.002.
Elbers, P. W. G., Wijbenga, J., Solinger, F., Yilmaz, A., van Iterson, M., van Dongen, E. P. A., & Ince, C. (2011). Direct observation of the human microcirculation during cardiopulmonary bypass: Effects of pulsatile perfusion. Journal of Cardiothoracic and Vascular Anesthesia, 25(2), 250–255. https://doi.org/10.1053/j.jvca.2010.06.014.
Yuruk, K., Almac, E., Bezemer, R., Goedhart, P., de Mol, B., & Ince, C. (2011). Blood transfusions recruit the microcirculation during cardiac surgery. Transfusion, 51(5), 961–967. https://doi.org/10.1111/j.1537-2995.2010.02971.x.
O’Neil, M. P., Alie, R., Guo, L. R., Myers, M.-L., Murkin, J. M., & Ellis, C. G. (2018). Microvascular responsiveness to pulsatile and nonpulsatile flow during cardiopulmonary bypass. The Annals of Thoracic Surgery, 105(6), 1745–1753. https://doi.org/10.1016/j.athoracsur.2018.01.007.
Koning, N. J., Vonk, A. B. A., Vink, H., & Boer, C. (2016). Side-by-side alterations in glycocalyx thickness and perfused microvascular density during acute microcirculatory alterations in cardiac surgery. Microcirculation, 23(1), 69–74. https://doi.org/10.1111/micc.12260.
Dekker, N. A. M., Veerhoek, D., Koning, N. J., van Leeuwen, A. L. I., Elbers, P. W. G., van den Brom, C. E., et al. (2019). Postoperative microcirculatory perfusion and endothelial glycocalyx shedding following cardiac surgery with cardiopulmonary bypass. Anaesthesia, 74(5), 609–618. https://doi.org/10.1111/anae.14577.
den Uil, C. A., Lagrand, W. K., Spronk, P. E., van Domburg, R. T., Hofland, J., Lüthen, C., et al. (2008). Impaired sublingual microvascular perfusion during surgery with cardiopulmonary bypass: A pilot study. The Journal of Thoracic and Cardiovascular Surgery, 136(1), 129–134. https://doi.org/10.1016/j.jtcvs.2007.10.046.
Nussbaum, C., Haberer, A., Tiefenthaller, A., Januszewska, K., Chappell, D., Brettner, F., et al. (2015). Perturbation of the microvascular glycocalyx and perfusion in infants after cardiopulmonary bypass. The Journal of Thoracic and Cardiovascular Surgery, 150(6), 1474–1481.e1. https://doi.org/10.1016/j.jtcvs.2015.08.050.
Scolletta, S., Marianello, D., Isgrò, G., Dapoto, A., Terranova, V., Franchi, F., et al. (2016). Microcirculatory changes in children undergoing cardiac surgery: A prospective observational study. British Journal of Anaesthesia, 117(2), 206–213. https://doi.org/10.1093/bja/aew187.
Ugenti, V., Romano, A. C., & Tibirica, E. (2018). Microvascular endothelial dysfunction during cardiopulmonary bypass in surgery for correction of cyanotic and acyanotic congenital heart disease. Microvascular Research, 120, 55–58. https://doi.org/10.1016/j.mvr.2018.06.004.
De Backer, D., Hollenberg, S., Boerma, C., Goedhart, P., Büchele, G., Ospina-Tascon, G., et al. (2007). How to evaluate the microcirculation: Report of a round table conference. Critical Care, 11(5), R101. https://doi.org/10.1186/cc6118.
Ince, C., Boerma, E. C., Cecconi, M., De Backer, D., Shapiro, N. I., Duranteau, J., et al. (2018). Second consensus on the assessment of sublingual microcirculation in critically ill patients: Results from a task force of the European Society of Intensive Care Medicine. Intensive Care Medicine, 44(3), 281–299. https://doi.org/10.1007/s00134-018-5070-7.
Gaies, M. G., Gurney, J. G., Yen, A. H., Napoli, M. L., Gajarski, R. J., Ohye, R. G., et al. (2010). Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatric Critical Care Medicine, 11(2), 234–238. https://doi.org/10.1097/PCC.0b013e3181b806fc.
Vellinga, N. A. R., Boerma, E. C., Koopmans, M., Donati, A., Dubin, A., Shapiro, N. I., et al. (2015). International study on microcirculatory shock occurrence in acutely ill patients. Critical Care Medicine, 43(1), 48–56. https://doi.org/10.1097/CCM.0000000000000553.
den Os, M. M., van den Brom, C. E., van Leeuwen, A. L. I., & Dekker, N. A. M. (2020). Microcirculatory perfusion disturbances following cardiopulmonary bypass: A systematic review. Critical Care, 24(1), 218. https://doi.org/10.1186/s13054-020-02948-w.
De Blasi, R. A., Palmisani, S., Boezi, M., Arcioni, R., Collini, S., Troisi, F., & Pinto, G. (2008). Effects of remifentanil-based general anaesthesia with propofol or sevoflurane on muscle microcirculation as assessed by near-infrared spectroscopy. British Journal of Anaesthesia, 101(2), 171–177. https://doi.org/10.1093/bja/aen136.
Koch, M., De Backer, D., Vincent, J. L., Barvais, L., Hennart, D., & Schmartz, D. (2008). Effects of propofol on human microcirculation. British Journal of Anaesthesia, 101(4), 473–478. https://doi.org/10.1093/bja/aen210.
Liu, X., Zhang, K., Wang, W., Xie, G., Cheng, B., Wang, Y., et al. (2016). Dexmedetomidine versus propofol sedation improves sublingual microcirculation after cardiac surgery: A randomized controlled trial. Journal of Cardiothoracic and Vascular Anesthesia, 30(6), 1509–1515. https://doi.org/10.1053/j.jvca.2016.05.038.
Riedijk, M. A., & Milstein, D. M. J. (2018). Imaging sublingual microcirculatory perfusion in pediatric patients receiving procedural sedation with propofol: A pilot study. Microcirculation, e12484. https://doi.org/10.1111/micc.12484
Özarslan, N. G., Ayhan, B., Kanbak, M., Çelebioğlu, B., Demircin, M., Ince, C., & Aypar, Ü. (2012). Comparison of the effects of sevoflurane, isoflurane, and desflurane on microcirculation in coronary artery bypass graft surgery. Journal of Cardiothoracic and Vascular Anesthesia, 26(5), 791–798. https://doi.org/10.1053/j.jvca.2012.03.019.
Maar, S. P. (2008). Searching for the Holy Grail: A review of markers of tissue perfusion in pediatric critical care. Pediatric Emergency Care, 24(12), 883–887. https://doi.org/10.1097/PEC.0b013e31819112b7.
Englehart, M. S., & Schreiber, M. A. (2006). Measurement of acid-base resuscitation endpoints: Lactate, base deficit, bicarbonate or what? Current Opinion in Critical Care, 12(6), 569–574. https://doi.org/10.1097/MCC.0b013e328010ba4f.
Holley, A., Lukin, W., Paratz, J., Hawkins, T., Boots, R., & Lipman, J. (2012). Review article: Part two: Goal-directed resuscitation--Which goals? Perfusion targets. Emergency Medicine Australasia, 24(2), 127–135. https://doi.org/10.1111/j.1742-6723.2011.01515.x.
González, R., Urbano, J., Solana, M. J., Hervías, M., Pita, A., Pérez, R., et al. (2019). Microcirculatory differences in children with congenital heart disease according to cyanosis and age. Frontiers in Pediatrics, 7, 264. https://doi.org/10.3389/fped.2019.00264.
Boerma, E. C., & Ince, C. (2010). The role of vasoactive agents in the resuscitation of microvascular perfusion and tissue oxygenation in critically ill patients. Intensive Care Medicine, 36(12), 2004–2018. https://doi.org/10.1007/s00134-010-1970-x.
Buijs, E. A. B., Verboom, E. M., Top, A. P. C., Andrinopoulou, E.-R., Buysse, C. M. P., Ince, C., & Tibboel, D. (2014). Early microcirculatory impairment during therapeutic hypothermia is associated with poor outcome in post-cardiac arrest children: A prospective observational cohort study. Resuscitation, 85(3), 397–404. https://doi.org/10.1016/j.resuscitation.2013.10.024.
Ergenekon, E., Hirfanoğlu, I., Beken, S., Turan, O., Kulali, F., Koç, E., & Gücüyener, K. (2013). Peripheral microcirculation is affected during therapeutic hypothermia in newborns. Archives of Disease in Childhood. Fetal and Neonatal Edition, 98(2), F155–F157. https://doi.org/10.1136/archdischild-2012-301647.
González, R., Urbano, J., López, J., Solana, M. J., Botrán, M., García, A., et al. (2016). Microcirculatory alterations during haemorrhagic shock and after resuscitation in a paediatric animal model. Injury, 47(2), 335–341. https://doi.org/10.1016/j.injury.2015.10.075.
González, R., López, J., Urbano, J., Solana, M. J., Fernández, S. N., Santiago, M. J., & López-Herce, J. (2017). Evaluation of sublingual microcirculation in a paediatric intensive care unit: Prospective observational study about its feasibility and utility. BMC Pediatrics, 17(1), 75. https://doi.org/10.1186/s12887-017-0837-5.
Acknowledgements
The authors would like to acknowledge the contribution to the study of all members of the infant heart area of Gregorio Marañón General University Hospital. The authors would like to specially acknowledge the patients and their families who decided to collaborate with our study.
Funding
This study was partially funded by the Mutua Madrileña Foundation (grant FMM 14/02), by the Spanish Society of Paediatric Intensive Care (Francisco Ruza’s grant 2017), and by the Carlos III Health Institute Subdirectorate General for Research Assessment and Promotion, and the European Regional Development Fund (ERDF) (grant PI17/01319).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human Subjects/Informed Consent Statement
The study was approved by Gregorio Marañón General University Hospital Institutional Review Board. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients or their legal representatives for being included in the study
Conflict of Interest
The authors declare no competing interests.
Additional information
Associate Editor Junjie Xiao oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
González Cortés, R., Urbano Villaescusa, J., Solana García, M.J. et al. Microcirculatory Changes in Pediatric Patients During Congenital Heart Defect Corrective Surgery. J. of Cardiovasc. Trans. Res. 14, 1173–1185 (2021). https://doi.org/10.1007/s12265-021-10132-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-021-10132-w