Abstract
Atherosclerosis is the primary cause of heart attacks, and while efforts to prevent its development or progression have historically focused largely on reducing cholesterol levels, there is now important proof-of-principle data that supports the role that inflammation plays in atherogenesis. Heat shock protein 27 (HSP27) is a novel biomarker of atherosclerosis that is also atheroprotective. Through a series of murine and in vitro experiments, an iterative narrative is emerging that demonstrates how HSP27 can act as an extracellular mediator that reduces plaque inflammation—either directly via transcriptional pathways, or indirectly via important effects on macrophage biology. While there is much more to learn about the biology of HSP27, we now review the strong foundation of knowledge that highlights the potential anti-inflammatory role of HSP27 as a novel therapeutic for not only atherosclerosis but potentially other inflammatory disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction: the Role of Inflammation in Atherogenesis
Obstruction of blood flow to vital organs such as the heart muscle or brain is the primary cause of mortality in the developed world, with the burden of disease steadily growing in developing countries [1]. The common cause of such arterial obstructions is atherosclerosis, a disease process that begins early in life, and may remain clinically silent until a plaque ruptures, resulting in thrombus formation, ischemia, and end-organ damage. Although the focus of study for centuries, the factors that transform a non-obstructive plaque into a late-stage atherosclerotic lesion are incompletely understood [2]. Much attention has been centered on understanding and modifying the role of lipoproteins in plaque development, instability, and quiescence. Though progress has been made with the widespread use of statins, the current standard of care for reducing cholesterol levels, there remains a substantial residual risk in these patients—even with the use of newer therapies that target PCSK9, an important negative regulator of cholesterol metabolism that drive plasma low-density lipoprotein cholesterol down to levels previously thought to be unattainable [3, 4]. Indeed, the 5-year risk of recurrent myocardial infarction, stroke, or cardiovascular death is > 20% in statin-treated patients, and although some of this risk may be due to suboptimal treatment of low-density cholesterol levels, it is now becoming clear that residual inflammatory risk is also important [5,6,7].
In the context of atherosclerosis, what is inflammation? In any disease process or injury, the inflammatory process is designed to contain the insult, initiate appropriate wound healing responses, and restore homeostasis. However, persistent (or chronic) inflammation indicates that this process is incomplete or lacks the cues to resolve—thereby signaling the transformation from a physiological to a pathological response [8]. Indeed, many of the steps that promote the transformation of benign intimal thickening to a complex lipid-laden plaque with a necrotic core that is vulnerable to rupture or ulceration are due to unbridled inflammation [9, 10]. While the role of inflammation in experimental atherosclerosis models is very well studied—it is only recently that the clinical evidence for the role of inflammation in the pathogenesis of atherosclerotic coronary artery disease (CAD) has emerged. As arterial inflammation is challenging to directly study, even by non-invasive means [11], there is a heavy reliance on the circulating inflammatory biomarker C-reactive protein (CRP; measured using a high sensitivity assay or hsCRP) to prognosticate cardiovascular events [12].
CRP is downstream from the inflammatory cytokine IL-1β, which is activated by the NLRP3 (NOD-like receptor P3) inflammasome and then released into the circulation [13]. Perhaps the importance of CRP in cardiovascular prevention trials was initially highlighted by JUPITER (Justification for the Use of Statins in Prevention: An Intervention Trial Evaluating Rosuvastatin) that showed how a statin (rosuvastatin) reduced the incidence of cardiovascular events in asymptomatic subjects with normal low-density lipoprotein cholesterol (LDL-C) but elevated hsCRP—as the degree of protection was proportional to the diminution in hsCRP [14]. However, with the concomitant reduction in LDL-C in JUPITER, it was impossible to conclusively attribute the improvement in CV outcomes to the attenuation of inflammation. While it is clear that statins can optimally reduce LDL-C (defined as < 70 mg/dL) and hsCRP (defined as < 2 mg/L) in symptomatic CAD patients—typically, only the minority of patients reach these goals. For example, in post hoc analyses of two large trials of acute coronary syndrome patients treated with aggressive statin therapy, the relative proportion of patients with residual inflammatory risk is significant (e.g., 29–33%) [15, 16].
Hence, the need to address inflammation as a major pathophysiological contributor to CAD is large. This is where novel biological therapies are now entering the CAD therapeutic landscape. In particular, there is a renewed interest in the cytokine IL-1β, as it is produced by macrophages in human atherosclerotic lesions in response to the presence of cholesterol crystals and plays an integral role in “inflammageing” [17, 18]. Inflammageing is essentially chronic inflammation and is characterized by elevated levels of blood inflammatory markers such as hsCRP and is associated with the development of persistent inflammatory conditions (such as atherosclerosis) that arise due to genetic, lifestyle, and co-morbidity factors [19].
Given the importance of IL-1β in atherosclerosis, and the availability of a human monoclonal antibody that targets IL-1β (i.e., canakinumab, approved for use in patients with rheumatological disorders), the recently completed CANTOS trial (Canakinumab Anti-inflammatory Thrombosis Outcomes Study) was designed to test the inflammatory theory for the pathogenesis of atherosclerosis [20]. In approximately ten thousand myocardial infarction patients prescribed optimal statin therapy, subjects were randomized to receive one of three doses of canakinumab administered subcutaneously every 3 months for approximately 4 years. Only patients with an elevated hsCRP level (> 2 mg/L) were enrolled—as this was considered a surrogate marker for arterial wall inflammation. Briefly, with the intermediate (150 mg) dose of canakinumab, there was a reduction in the primary clinical endpoint (a composite of nonfatal myocardial infarction, nonfatal stroke, and cardiovascular death). Hence, this trial emphasizes the fact that inflammation is treatable and associated with improved cardiovascular outcomes. Moreover, it identified IL-1β as a therapeutic target for “atheroprotection.” There were other intriguing results from this trial, including a reduction in cancer mortality with canakinumab and, unfortunately, a higher death rate from an infection that was statistically significant but relatively low (a 1-year annual risk of 1/750 patients). Finally, the cost of this drug is currently prohibitive (approximately $64,000 per year) [21]. Although some [22, 23] but not all [24, 25] recent pre-clinical and clinical trials support the anti-inflammation approach for the treatment of atherosclerosis, CANTOS stands out as an intriguing proof-of-concept trial that highlights the need for additional anti-inflammatory studies. To this point, we now review the accrued knowledge of the anti-inflammatory properties of a specific heat shock protein as an anti-inflammatory modulator of atherogenesis and how it is being developed as a potential clinical therapy.
Heat Shock Protein 27 in the Context of Atherosclerotic Inflammation
Briefly, heat shock proteins are highly conserved proteins grouped according to their molecular size. HSP27 (205 amino acids, also known as HSPB1) is part of the small HSP (sHSP) family of proteins. sHSPs are ATP-independent molecular chaperones that are transiently upregulated in various cell types subjected to stress stimuli. Similar to other (larger) HSPs, sHSPs recognize and bind unfolded or misfolded proteins, thus preventing their irreversible aggregation—which is important for a variety of protein-misfolding disorders (e.g., Parkinson’s, Alzheimer’s diseases, and the inflammatory/apoptotic nature of atherosclerosis). To varying degrees, HSP27 is expressed in human cells, including vascular smooth muscle and endothelial cells.
Approximately 15 years ago, three independent laboratories (including our own) almost simultaneously published their findings on the potential role of HSP27 in atherosclerosis [26,27,28]. While looking for clues to the paradox that women are relatively protected against CAD until menopause, we discovered HSP27 as an estrogen receptor beta (ER-β)–associated protein [27, 29]. Importantly, we examined the expression of HSP27 in human CAD and noted a progressive diminution of protein expression as the stage of atherosclerosis progressed (Fig. 1). These results have subsequently been confirmed by two additional laboratories using objective proteomic approaches [30, 31]. Moreover, we and others noted that blood HSP27 levels were lower in atherosclerosis patients compared with healthy subjects and showed that lower HSP27 levels were predictive of subsequent major clinical events (i.e., heart attack, stroke, cardiovascular death) over a 5-year period [26, 32, 33]. Hence, HSP27 blood levels have also emerged as a new biomarker for atherosclerosis that is predictive of adverse cardiovascular events. With these clinical insights regarding HSP27 expression, we then developed an experimental platform to study HSP27 in vascular biology.
Photomicrographs of human coronary artery cross-sections: Left: Cross-section of benign intimal thickening in a coronary artery of a young individual free of atherosclerosis (top: Movat pentachrome stain, magnification × 40; bottom: immunolabeled for HSP27, magnification × 400). Right: Advanced atheroma with necrotic, cholesterol-laden intimal core (Movat pentachrome stain and α-smooth muscle actin immunolabeling). HSP27 immunolabeling is essentially negative (below right; magnification × 100). All positive immunolabeling yielded a brown color reaction product, with a hematoxylin nuclear counterstain. Adapted from [27]
Endogenous HSP27 Overexpression Attenuates Atherogenesis and Inflammation
To examine the functional significance of HSP27 in atherogenesis, we studied both the early and late phases of lesion development using a common murine model of inflammatory atherogenesis: the Apoe−/− mouse fed a high-fat diet (HFD). To determine if HSP27 would alter atherogenesis in this model, mice overexpressing human HSP27 (HSP27o/e) were crossbred with Apoe−/− mice [34]. After 4 weeks of the HFD, there was a 35% reduction in aortic atherosclerotic burden in female (but not male) Apoe−/− HSP27o/e vs. Apoe−/− control mice. While baseline HSP27 blood levels were virtually undetectable in all mice, after 4 weeks of the HFD, there was a > 10-fold increase in HSP27 blood levels in female Apoe−/− HSP27o/e mice (and little change in the levels in male mice). Moreover, there was an inverse correlation between HSP27 blood levels and the extent of atherosclerotic burden. With regard to inflammation, rHSP27 treatment of macrophages in vitro was associated with a reduction in foam cell formation, as reflected by decreased uptake of acetylated LDL (acLDL). These macrophages released less IL-1β (pro-inflammatory) and more IL-10 (anti-inflammatory) into their cell culture media. Hence, HSP27 had an indirect effect on inflammatory cytokine generation, likely due to a reduction in the transformation of macrophages into foam cells.
Chronic overexpression of HSP27 is also atheroprotective in Apoe−/− mice as it facilitates favorable plaque remodeling [35]. In Apoe−/− HSP27o/e mice of both sexes fed a HFD for 12 weeks, blood HSP27 levels rose by more than 16-fold from baseline. Of note, HSP27 blood levels were higher in the female mice—which is in keeping with our earlier in vitro and in vivo observations on the key role that estrogens play in promoting the extracellular release of HSP27 [34, 36]. Presumably, the rise in HSP27 blood levels in the male mice was due to prolonged exposure to the metabolic stress of an atherogenic HFD. While the reductions in atherogenesis were significant but modest in the Apoe−/− HSP27o/e compared with Apoe−/− counterpart mice (e.g., for both sexes, the reductions in aortic lesion area were 21–35% for en face and 24–30% for cross-sectional aortic sinus tissue sections), there were impressive changes in lesion morphology that are consistent with less inflamed plaques, including:
-
(a)
Reduced aortic lesion cholesterol content, as reflected by the number of intimal cholesterol clefts, as well as the areas occupied by lipid and free cholesterol (Fig. 2),
-
(b)
Reduced plaque macrophage content (Fig. 2),
-
(c)
Increased lesion smooth muscle and collagen content (Fig. 2), and
-
(d)
Increased lesion stiffness (as reflected in stress-strain curves generated during ex-vivo mechanical stretching experiments).
Chronic HSP27 overexpression in Apoe−/− mice reduces aortic lesion cholesterol content. a Cholesterol cleft area is reduced within lesions from Apoe−/− HSP27o/e vs. Apoe−/− mice as observed using the Masson’s trichrome stain. b Attenuated arterial wall unesterified cholesterol content in Apoe−/− HSP27o/e mice as denoted by fluorescent blue Filipin staining. Scale bars = 100 μm for a and b and 500 μm for insert photo for a; L lumen. c Reduction in arterial wall foamy macrophage content and apoptosis with overexpression of HSP27. Macrophages (brown anti-Mac-2 immunolabeling reaction product) localized mainly in luminal layers of aortic sinus cross-sections. Scale bars = 100 μm and 500 μm for insert photo. d Increased intimal collagen content with HSP27 overexpression as demonstrated by polarized microscopy on picrosirius red-stained sections. Bright yellow/orange birefringence of collagen, due to co-aligned molecules of type I collagen. Scale bars = 20 μm and 200 μm for insert photo; L lumen, I intima; dotted lines delineate the media. Figure reproduced with permission from [35]
Taken together, these histological changes are consistent with plaque inflammation that has not gone unabated and may in fact be in the process of resolving [37]. Further study of the long-term effects of HSP27 on atherogenesis is warranted. However, to date, we do know that Apoe−/− HSP27o/e mice fed a normal chow diet for 32 weeks show a persistent decrease (− 29%) in aortic lesion burden with a concomitant (−26%) reduction in total plasma cholesterol levels compared with Apoe−/− control mice [33]. Hence, it appears that HSP27 has a durable atheroprotective effect.
Exogenous HSP27 Is Atheroprotective and Attenuates Arterial Inflammation
As we demonstrated the secretion of HSP27 from macrophages in vitro, we sought to determine what cells were driving the increase in HSP27 blood levels in vivo by transplanting bone marrow from Apoe−/− HSP27o/e mice into Apoe−/− littermates, which do not have the HSPB1 gene encoding for HSP27 [33]. While serum HSP27 levels were undetectable in the control mice, transplantation of bone marrow from Apoe−/− HSP27o/e mice resulted in marked elevation of HSP27 blood levels and reductions in aortic lesion burden (e.g., − 50% for en face and − 28% for aortic sinus cross-sections). Again, other important salutary effects were noted in the plaques of the mice receiving the HSP27o/e marrow (e.g., reduced cholesterol cleft and necrotic core areas). Hence, the data from this experiment suggest that HSP27 derived from blood-borne cells is sufficient to attenuate de novo atherosclerotic lesion formation and perhaps overshadows the functional importance of the artery wall (i.e., smooth muscle or endothelial cell) expression of HSP27.
Additionally, we synthesized recombinant HSP27 (rHSP27) to explore its potential therapeutic effects in de novo lesion formation [33]. Twice-daily subcutaneous injections of either rHSP27 (100 μg) or vehicle for 3 weeks increased HSP27 blood levels and reduced total aortic lesion area (31% and 40% for aortic en face and sinus analyses, respectively). Interestingly, total plasma cholesterol levels were 42% lower with rHSP27 treatment (p < 0.001) due to reductions in very-low-density lipoprotein and intermediate-IDL/low-density sub-fractions. The mechanisms involved in lowering plasma cholesterol levels are now an active area of research in the O’Brien laboratory and appear to be due to important transcriptional effects on key mediators of cholesterol metabolism (unpublished data).
HSP27 Stabilizes Existing Plaques and Lowers Inflammation
As clinical therapies are often initiated in patients with established disease after events such as myocardial infarction or stroke, we tested the ability of rHSP27 to modulate the progression and morphology of established atherosclerotic lesions. Apoe−/− mice were fed an atherogenic diet for 4 weeks to establish a “baseline” atherosclerotic state, then switched to a normal chow diet to simulate lipid management strategies such as lifestyle modifications and/or the prescribing of statin therapy [33]. After developing these baseline lesions, rHSP27 (100 μg) or vehicle was administered twice daily for 3 weeks. Total plasma cholesterol levels were similar in both groups at baseline and decreased after switching to the chow diet, yet were 27% lower with rHSP27 treatment at the time of euthanasia (p = 0.004). Again, aortic lesion area was modestly but significantly reduced with rHSP27 vs. control treatment—and comparable with that of the baseline atherosclerotic state—thereby implying that lesion progression was halted. Moreover, rHSP27 therapy was associated with the genesis of intimal plaques with less inflammation (e.g., fewer macrophages, less free cholesterol accumulation, and less area occupied by cholesterol clefts) and structurally more resilient morphologies (e.g., more abundant collagen and smooth muscle content). Whether all of the salutary HSP27 effects on lesion morphology are directly related to the effect of this protein on macrophage biology is unclear. Certainly, there are other possible cellular effects to consider—including the role of HSP27 in accelerating re-endothelialization of arterial lesions via the upregulation of vascular endothelial growth factor [38].
HSP27 Modulation of Inflammatory Signaling
The reductions in atherosclerotic lesion formation with either endogenous HSP27 overexpression or the administration of exogenous rHSP27 occurred in the presence of modest lowering of plasma cholesterol levels. Given that the pathogenesis of atherosclerosis is broadly considered to be due to the dual effects of hypercholesterolemia and inflammation, we sought to focus on how HSP27 may interact with the NF-kB master transcriptional regulatory pathway that plays a key role in modulating inflammation. Briefly, NF-κB transcription factors regulate a vast number and diversity of gene targets, including those involved in cell proliferation, apoptosis, the cell stress response, inflammation, and both innate and adaptive immune responses [39, 40]. Normally found in the cytoplasm as inactive dimers associated with ΙκΒ, NF-κB translocates to the nucleus once IκB is phosphorylated by the upstream IκB kinase complex (IKK), leading to the transactivation of numerous gene targets—including many atherosclerosis-related gene programs [39, 41].
Hence, to remove the potential confounding HSP27 lipid-lowering effect and the resultant indirect effects on inflammation, we performed the following in vitro experiments. Studying macrophages in tissue culture, we observed that rHSP27 activates the NF-κB pathway and alters downstream transcription, resulting in up-/downregulation of the key genes for pro- and anti-inflammatory cytokines such as IL-6, GM-CSF, TNF, or IL-10 [42]. Such a result is not unexpected. While NF-kB is often regarded to have a pro-inflammatory role, this may be an oversimplification. Indeed, while a “pan-hematopoietic” knock-out of NF-kB reduces experimental atherogenesis, [43] knocking out macrophage [44] NF-kB actually worsens atherogenesis. As macrophages will of course produce anti-inflammatory factors such as IL-10 (in response to HSP27), activation of NF-kB is in some instances a critical determinant of inflammatory balance, yet may change over time, depending on the disease stage (e.g., early inflammatory stage of atherogenesis vs. later progressive plaque remodeling). Recently, it has been pointed out that perhaps, the macrophage functional response is determined by interactions between triggered transcription factors and depends on the microenvironment and interdependent signaling cascades [45]. Finally, it is important to note that many studies focus on the role of intracellular HSP27 on the NF-κB pathway and that we are only now beginning to better understand whether extracellular HSP27 has similar or different effects as an inter-cellular messenger.
Future Perspectives
While there has been much progress understanding the atheroprotective role of HSP27—including its important anti-inflammatory effects—several questions remain for future study:
-
(1)
How is HSP27 released from cells?
Initially thought to be exclusively an intracellular protein that plays a major role in facilitating the refolding of denatured proteins, it is now clear that HSP27 exits viable cells to serve inter-cellular signaling functions [46]. Lacking a classical N-terminus signal sequence required for conventional protein secretory pathways, HSP27 is released into the extracellular space via unconventional pathways. For example, we previously showed that HSP27 is released from macrophages treated with estrogens in vitro, especially estrogen receptor-β agonists [34, 36, 47]. This secretion to the extracellular space is not due to release from nonviable cells. Moreover, the pharmacological inhibitor of exosomal transport, dimethylamiloride, reduces HSP27 levels in the culture media. In contrast, inhibitors of the Golgi apparatus (brefeldin A), protein synthesis (cycloheximide), transcription (actinomycin D), or ABC transporters (glibenclamide) do not alter the secretion of HSP27 in response to estrogen receptor modulation. In addition, we recently demonstrated that HSP27 localizes to macrophage-derived extracellular vesicles (EVs) using 4 methods, including transmission electron microscopy with immuno-gold labeling (Fig. 3) [48]. When these EVs are treated (presumably coated) with excess HSP27, they activate NF-kB and release IL-10. Hence, these data suggest that HSP27 may be an important cargo protein for EVs that can participate in paracrine signaling processes that attenuate inflammation. Whether HSP27-laden EVs can be utilized as therapeutic agents—either endogenously upregulated or exogenously produced and administered—is currently being studied.
-
(2)
Potential sex-specific mechanisms involved in HSP27-mediated atheroprotection
Linked to the discovery of HSP27 as EV cargo, is the fact that estrogens facilitate the release of EVs. There has been a long-standing link between HSP27 and estrogen—particularly estrogen receptors [49]. Indeed, this association appears to be sex-specific, as female mice or women tend to have higher HSP27 levels than men—particularly pre-menopausal women [33, 34, 50, 51]. Moreover, while HSP27 overexpression protected mice from atherosclerosis, particularly in female mice [34]—this process was abrogated by ovariectomy but rescued by administration of exogenous estrogens [36]. Taken together, these data indicate that secretion of HSP27 into the circulation is at least facilitated by estrogens—which of course has implications for post-menopausal women, who are faced with a steep increase in symptomatic CAD once they surpass menopause [29]. Currently, we are studying the effects of “surgical menopause” (i.e., removal of ovaries because of an inherited risk of cancer) as a model for understanding the changes in HSP27, cholesterol, and other inflammatory markers when ovarian function ceases [51].
Transmission electron microscopic images of exosomes harvested from THP-1 monocytes in vitro. a Left and right showing × 50,000 and × 100,000 magnification, with scale bars of 100 and 50 nm; respectively. b Exosomes immunolabeled with anti-human HSP27 primary mouse antibody followed by anti-mouse IgG secondary antibody conjugated to 5-nm gold particles. Arrows indicate HSP27 immuno-gold labeling (black dots) on the exosome surface. Scale bar = 100 nm. Figure reproduced with permission from [48]
Summary
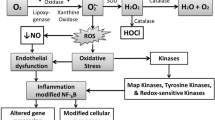
HSP27 represents an interesting extracellular molecule that plays a key role in atheroprotection, reducing not only cholesterol levels but also indices of inflammation. However, more research is needed to better characterize the cellular mechanisms by which extracellular HSP27 signals at the cell membrane, alters transcriptional regulation pathways, and reduces inflammation because of direct and indirect effects on macrophage biology (Fig. 4).
Top panel showing peritoneal macrophages isolated from Apoe−/− mice and subjected to treatment with rHSP27, rC1 (negative control peptide), or no treatment. rHSP27 but not rC1 treatment for 30 min resulted in increased nuclear localization of the NF-κB p65 subunit (green fluorescence with blue Hoechst nuclear stain). Scale bar = 10 μm. Figure reproduced with permission from [52]. The bottom panel is a schematic overview of HSP27 cellular release and signaling. As an ER-β binding protein HSP27 acts as a co-repressor of estrogen signaling. In response to estrogenic stimulation or to atherogenic stress induced by elevated serum cholesterol levels, HSP27 is released as EVs (e.g., exosomes). The proportion of extracellular HSP27 that is exosomal vs. non-exosomal is currently unclear. HSP27 may communicate with other cells via pattern recognition receptors like toll-like receptor 4 (TLR4) on macrophages to alter transcription via the NF-κB pathway. Shown here are various examples of HSP27-induced upregulation (IL-10, GM-CSF) and downregulation (IL-1, SR-A1) of gene expression. HSP27 can also competitively bind SR-A to reduce uptake of acLDL. GM-CSF can upregulate ABC transporters involved in reverse cholesterol transport
References
World Health, O. (2014). Global status report on noncommunicable diseases 2014. http://www.who.int/topics/womens_health/en/.
Schwartz, S. M., deBlois, D., & O’Brien, E. R. (1995). The intima. Soil for atherosclerosis and restenosis. Circulation Research, 77(3), 445–465.
Pradhan, A. D., Aday, A. W., Rose, L. M., & Ridker, P. M. (2018). Residual inflammatory risk on treatment with PCSK9 inhibition and statin therapy. Circulation, 138(2), 141–149. https://doi.org/10.1161/circulationaha.118.034645.
Ray, K. K., Corral, P., Morales, E., & Nicholls, S. J. (2019). Pharmacological lipid-modification therapies for prevention of ischaemic heart disease: current and future options. The Lancet, 394(10199), 697–708. https://doi.org/10.1016/S0140-6736(19)31950-6.
Fox, K. A., Carruthers, K., Steg, P. G., Avezum, A., Granger, C. B., Montalescot, G., et al. (2010). Has the frequency of bleeding changed over time for patients presenting with an acute coronary syndrome? The global registry of acute coronary events. European Heart Journal, 31(6), 667–675. https://doi.org/10.1093/eurheartj/ehp499.
Jernberg, T., Hasvold, P., Henriksson, M., Hjelm, H., Thuresson, M., & Janzon, M. (2015). Cardiovascular risk in post-myocardial infarction patients: nationwide real world data demonstrate the importance of a long-term perspective. European Heart Journal, 36(19), 1163–1170. https://doi.org/10.1093/eurheartj/ehu505.
Koenig, W. (2018). Low-grade inflammation modifies cardiovascular risk even at very low LDL-C levels. Are We Aiming for a Dual Target Concept?, 138(2), 150–153. https://doi.org/10.1161/circulationaha.118.035107.
Tabas, I., & Glass, C. K. (2013). Anti-inflammatory therapy in chronic disease: challenges and opportunities. Science, 339(6116), 166–172. https://doi.org/10.1126/science.1230720.
Schwartz, S. M., deBlois, D., & O’Brien, E. R. (1995). The intima: soil for atherosclerosis and restenosis. Circulation Research, 77, 445–465.
Libby, P., Tabas, I., Fredman, G., & Fisher, E. A. (2014). Inflammation and its resolution as determinants of acute coronary syndromes. https://doi.org/10.1161/CIRCRESAHA.114.302699.
Al-Mashhadi, R. H., Tolbod, L. P., Bloch, L. Ø., Bjørklund, M. M., Nasr, Z. P., Al-Mashhadi, Z., et al. (2019). Fluorodeoxyglucose accumulation in arterial tissues determined by PET signal analysis. Journal of the American College of Cardiology, 74(9), 1220–1232. https://doi.org/10.1016/j.jacc.2019.06.057.
Ridker, P. M. (2007). C-reactive protein and the prediction of cardiovascular events among those at intermediate risk: moving an inflammatory hypothesis toward consensus. Journal of the American College of Cardiology, 49(21), 2129–2138. https://doi.org/10.1016/j.jacc.2007.02.052.
Ridker, P. M. (2016). From C-reactive protein to interleukin-6 to interleukin-1: moving upstream to identify novel targets for atheroprotection. Circulation Research, 118(1), 145–156. https://doi.org/10.1161/CIRCRESAHA.115.306656.
Ridker, P. M., Danielson, E., Fonseca, F. A., Genest, J., Gotto, A. M., Kastelein, J. J., et al. (2008). Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med, 359. https://doi.org/10.1056/NEJMoa0807646.
Ridker, P. M., Morrow, D. A., Rose, L. M., Rifai, N., Cannon, C. P., & Braunwald, E. (2005). Relative efficacy of atorvastatin 80 mg and pravastatin 40 mg in achieving the dual goals of low-density lipoprotein cholesterol <70 mg/dl and C-reactive protein <2 mg/l: an analysis of the PROVE-IT TIMI-22 trial. Journal of the American College of Cardiology, 45(10), 1644–1648. https://doi.org/10.1016/j.jacc.2005.02.080.
Bohula, E. A., Giugliano, R. P., Cannon, C. P., Zhou, J., Murphy, S. A., White, J. A., et al. (2015). Achievement of dual low-density lipoprotein cholesterol and high-sensitivity C-reactive protein targets more frequent with the addition of ezetimibe to simvastatin and associated with better outcomes in IMPROVE-IT. Circulation, 132(13), 1224–1233. https://doi.org/10.1161/CIRCULATIONAHA.115.018381.
Galea, J., Armstrong, J., Gadsdon, P., Holden, H., Francis, S. E., & Holt, C. M. (1996). Interleukin-1 beta in coronary arteries of patients with ischemic heart disease. Arteriosclerosis, Thrombosis, and Vascular Biology, 16(8), 1000–1006. https://doi.org/10.1161/01.atv.16.8.1000.
Ferrucci, L., & Fabbri, E. (2018). Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nature Reviews Cardiology, 15(9), 505–522. https://doi.org/10.1038/s41569-018-0064-2.
Furman, D., Campisi, J., Verdin, E., Carrera-Bastos, P., Targ, S., Franceschi, C., et al. (2019). Chronic inflammation in the etiology of disease across the life span. Nature Medicine, 25(12), 1822–1832. https://doi.org/10.1038/s41591-019-0675-0.
Ridker, P. M., Everett, B. M., Thuren, T., MacFadyen, J. G., Chang, W. H., Ballantyne, C., et al. (2017). Antiinflammatory therapy with canakinumab for atherosclerotic disease. New England Journal of Medicine. https://doi.org/10.1056/NEJMoa1707914.
Ibañez, B., & Fuster, V. (2017). CANTOS. A gigantic proof-of-concept trial, 121(12), 1320–1322, doi:https://doi.org/10.1161/circresaha.117.312200.
Vromman, A., Ruvkun, V., Shvartz, E., Wojtkiewicz, G., Santos Masson, G., Tesmenitsky, Y., et al. (2019). Stage-dependent differential effects of interleukin-1 isoforms on experimental atherosclerosis. European Heart Journal, 40(30), 2482–2491. https://doi.org/10.1093/eurheartj/ehz008.
Tardif, J.-C., Kouz, S., Waters, D. D., Bertrand, O. F., Diaz, R., Maggioni, A. P., et al. (2019). Efficacy and safety of low-dose colchicine after myocardial infarction. New England Journal of Medicine. https://doi.org/10.1056/NEJMoa1912388.
Gomez, D., Baylis, R. A., Durgin, B. G., Newman, A. A. C., Alencar, G. F., Mahan, S., et al. (2018). Interleukin-1β has atheroprotective effects in advanced atherosclerotic lesions of mice. Nature Medicine, 24(9), 1418–1429. https://doi.org/10.1038/s41591-018-0124-5.
Ridker, P. M., Everett, B. M., Pradhan, A., MacFadyen, J. G., Solomon, D. H., Zaharris, E., et al. (2019). Low-dose methotrexate for the prevention of atherosclerotic events. New England Journal of Medicine, 380(8), 752–762. https://doi.org/10.1056/NEJMoa1809798.
Martin-Ventura, J. L., Duran, M. C., Blanco-Colio, L. M., Meilhac, O., Leclercq, A., Michel, J. B., et al. (2004). Identification by a differential proteomic approach of heat shock protein 27 as a potential marker of atherosclerosis. Circulation, 110, 2216–2219.
Miller, H., Poon, S., Hibbert, B., Rayner, K., Chen, Y. X., & O’Brien, E. R. (2005). Modulation of estrogen signaling by the novel interaction of heat shock protein 27, a biomarker for atherosclerosis, and estrogen receptor beta. Arteriosclerosis Thrombosis and Vascular Biology, 25(3), E10–E14. https://doi.org/10.1161/01.ATV.0000156536.89752.8e.
Park, H. K., Park, E. C., Bae, S. W., Park, M. Y., Kim, S. W., Yoo, H. S., et al. (2006). Expression of heat shock protein 27 in human atherosclerotic plaques and increased plasma level of heat shock protein 27 in patients with acute coronary syndrome. Circulation, 114(9), 886–893.
Chiu, M. H., Heydari, B., Batulan, Z., Maarouf, N., Subramanya, V., Schenck-Gustafsson, K., et al. (2018). Coronary artery disease in post-menopausal women: are there appropriate means of assessment? Clinical Science (London, England), 132(17), 1937–1952. https://doi.org/10.1042/CS20180067.
Lepedda, A. J., Cigliano, A., Cherchi, G. M., Spirito, R., Maggioni, M., Carta, F., et al. (2009). A proteomic approach to differentiate histologically classified stable and unstable plaques from human carotid arteries. Atherosclerosis, 203(1), 112–118. https://doi.org/10.1016/j.atherosclerosis.2008.07.001.
Liang, W., Ward, L. J., Karlsson, H., Ljunggren, S. A., Li, W., Lindahl, M., et al. (2016). Distinctive proteomic profiles among different regions of human carotid plaques in men and women. Scientific Reports, 6, 26231. https://doi.org/10.1038/srep26231.
Jin, C., Phillips, V. L., Williams, M. J., van Rij, A. M., & Jones, G. T. (2014). Plasma heat shock protein 27 is associated with coronary artery disease, abdominal aortic aneurysm and peripheral artery disease. Springerplus, 3, 635. https://doi.org/10.1186/2193-1801-3-635.
Seibert, T. A., Hibbert, B., Chen, Y. X., Rayner, K., Simard, T., Hu, T., et al. (2013). Serum heat shock protein 27 levels represent a potential therapeutic target for atherosclerosis: observations from a human cohort and treatment of female mice. Journal of the American College of Cardiology, 62(16), 1446–1454. https://doi.org/10.1016/j.jacc.2013.05.041.
Rayner, K., Chen, Y. X., McNulty, M., Simard, T., Zhao, X., Wells, D. J., et al. (2008). Extracellular release of the atheroprotective heat shock protein 27 is mediated by estrogen and competitively inhibits acLDL binding to scavenger receptor-A. Circulation Research, 103(2), 133–141. https://doi.org/10.1161/circresaha.108.172155.
Cuerrier, C. M., Chen, Y. X., Tremblay, D., Rayner, K., McNulty, M., Zhao, X., et al. (2013). Chronic over-expression of heat shock protein 27 attenuates atherogenesis and enhances plaque remodeling: a combined histological and mechanical assessment of aortic lesions. PLoS One, 8(2), e55867.
Rayner, K., Sun, J., Chen, Y. X., McNulty, M., Simard, T., Zhao, X., et al. (2009). Heat shock protein 27 protects against atherogenesis via an estrogen-dependent mechanism: role of selective estrogen receptor beta modulation. Arteriosclerosis, Thrombosis, and Vascular Biology, 29(11), 1751–1756. https://doi.org/10.1161/ATVBAHA.109.193656.
Fredman, G. (2019). Resolving atherosclerosis and Alzheimer disease. Nature Reviews Cardiology, 16(5), 259–260. https://doi.org/10.1038/s41569-019-0182-5.
Ma, X., Hibbert, B., McNulty, M., Hu, T., Zhao, X., Ramirez, F. D., et al. (2014). Heat shock protein 27 attenuates neointima formation and accelerates reendothelialization after arterial injury and stent implantation: importance of vascular endothelial growth factor up-regulation. The FASEB Journal, 28(2), 594–602. https://doi.org/10.1096/fj.13-230417.
Perkins, N. D. (2007). Integrating cell-signalling pathways with NF-kappaB and IKK function. Nature Reviews. Molecular Cell Biology, 8(1), 49–62. https://doi.org/10.1038/nrm2083.
Pahl, H. L. (1999). Activators and target genes of Rel/NF-kappaB transcription factors. Oncogene, 18(49), 6853–6866. https://doi.org/10.1038/sj.onc.1203239.
Karin, M. (1999). How NF-kappaB is activated: the role of the IkappaB kinase (IKK) complex. Oncogene, 18(49), 6867–6874. https://doi.org/10.1038/sj.onc.1203219.
Salari, S., Seibert, T., Chen, Y. X., Hu, T., Shi, C., Zhao, X., et al. (2013). Extracellular HSP27 acts as a signaling molecule to activate NF-kappaB in macrophages. Cell Stress & Chaperones, 18(1), 53–63. https://doi.org/10.1007/s12192-012-0356-0.
Kanters, E., Gijbels, M. J., van der Made, I., Vergouwe, M. N., Heeringa, P., Kraal, G., et al. (2004). Hematopoietic NF-kappaB1 deficiency results in small atherosclerotic lesions with an inflammatory phenotype. Blood, 103(3), 934–940. https://doi.org/10.1182/blood-2003-05-1450.
Kanters, E., Pasparakis, M., Gijbels, M. J., Vergouwe, M. N., Partouns-Hendriks, I., Fijneman, R. J., et al. (2003). Inhibition of NF-kappaB activation in macrophages increases atherosclerosis in LDL receptor-deficient mice. The Journal of Clinical Investigation, 112(8), 1176–1185. https://doi.org/10.1172/JCI18580.
Kuznetsova, T., Prange, K. H. M., Glass, C. K., & de Winther, M. P. J. (2019). Transcriptional and epigenetic regulation of macrophages in atherosclerosis. Nature Reviews Cardiology. https://doi.org/10.1038/s41569-019-0265-3.
Batulan, Z., Pulakazhi Venu, V. K., Li, Y., Koumbadinga, G., Alvarez-Olmedo, D. G., Shi, C., et al. (2016). Extracellular release and signaling by heat shock protein 27: role in modifying vascular inflammation. Frontiers in Immunology, 7(JUL), https://doi.org/10.3389/fimmu.2016.00285.
Sun, J., Ma, X., Chen, Y. X., Rayner, K., Hibbert, B., McNulty, M., et al. (2011). Attenuation of atherogenesis via the anti-inflammatory effects of the selective estrogen receptor beta modulator 8beta-VE2. Journal of Cardiovascular Pharmacology, 58(4), 399–405.
Shi, C., Ulke-Lemee, A., Deng, J., Batulan, Z., & O’Brien, E. R. (2018). Characterization of heat shock protein 27 in extracellular vesicles: a potential anti-inflammatory therapy. FASEB J, fj201800987R. https://doi.org/10.1096/fj.201800987R.
Ciocca, D. R., & Luque, E. H. (1991). Immunological evidence for the identity between the hsp27 estrogen-regulated heat shock protein and the p29 estrogen receptor-associated protein in breast and endometrial cancer. Breast Cancer Research and Treatment, 20(1), 33–42.
Rayner, K., Chen, Y. X., Siebert, T., & O’Brien, E. R. (2010). Heat shock protein 27: clue to understanding estrogen-mediated atheroprotection? Trends in Cardiovascular Medicine, 20(2), 53–57.
Batulan, Z., Maarouf, N., Shrivastava, V., & O’Brien, E. (2018). Prophylactic salpingo-oophorectomy & surgical menopause for inherited risks of cancer: the need to identify biomarkers to assess the theoretical risk of premature coronary artery disease. [journal article]. Women’s Midlife Health, 4(1), 7. https://doi.org/10.1186/s40695-018-0037-y.
Pulakazhi Venu, V. K., Adijiang, A., Seibert, T., Chen, Y. X., Shi, C., Batulan, Z., et al. (2017). Heat shock protein 27-derived atheroprotection involves reverse cholesterol transport that is dependent on GM-CSF to maintain ABCA1 and ABCG1 expression in ApoE(−/−) mice. The FASEB Journal, 31(6), 2364–2379. https://doi.org/10.1096/fj.201601188R.
Funding
This manuscript was supported by research grants to E.R. O’Brien from the Canadian Institutes of Health Research (CIHR; ISO-110836 & PJT-149015), by an Advancing Science Through Pfizer-Investigator Research Exchange (ASPIRE; WI218510) Cardiovascular Grant, and through the generous research funding support from Libin Cardiovascular Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed and are listed in all studies performed by the O’Brien laboratory and cited in this review manuscript.
All procedures performed in human studies performed by the O’Brien laboratory and cited in this review manuscript were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in any research studies from the O’Brien laboratory that are cited in this review manuscript.
Additional information
Associate Editor Saskia de Jager oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Inia, J.A., O’Brien, E.R. Role of Heat Shock Protein 27 in Modulating Atherosclerotic Inflammation. J. of Cardiovasc. Trans. Res. 14, 3–12 (2021). https://doi.org/10.1007/s12265-020-10000-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-020-10000-z