Abstract
Percutaneous coronary interventions (PCIs) are an effective treatment for obstructive coronary artery diseases. However, the procedure’s success is limited by remodeling and formation of neointima. In the present study, we engineered rat mesenchymal stem cells (MSCs) to express type 2 angiotensin II receptor (AT2R) using a tetracycline-regulated system that can strictly regulate AT2R expression. We tested the ability of the modified MSCs to reduce neointima formation following arterial injury. We subjected rats to balloon injury, and reverse transcriptase polymerase chain reaction (RT-PCR) indicated no significant AT2R expression in normal rat arteries. Low expression of AT2R was observed at 28 days after balloon-induced injury. Interestingly, MSCs alone were unable to reduce neointimal hyperplasia after balloon-induced injury; after transplantation of modified MSCs, doxycycline treatment significantly upregulated neointimal AT2R expression and inhibited osteopontin mRNA expression, as well as neointimal formation. Taken together, these results suggest that transplantation of MSCs conditionally expressing AT2R could effectively suppress neointimal hyperplasia following balloon-induced injury. Therefore, MSCs with a doxycycline-controlled gene induction system may be useful for the management of arterial injury after PCI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mechanisms involved in neointima formation are common to all injury-related vascular diseases and include endothelial cell defects, migration of vascular smooth muscle cells (VSMCs) from the tunica media into the intima, VSMC aggregation and hyperplasia, and secretion of large amounts of extracellular matrix (ECM) by intimal VSMCs. Restenosis due to neointima formation substantially decreases the effects of therapy and affects the prognosis of vascular diseases [1–3].
Vascular tissue renin-angiotensin system (RAS) is crucial for promoting restenosis [4–6]. Excessive expression of angiotensin II (Ang II) at the site of endothelial injury promotes intimal hyperplasia as well as VSMC migration and suppresses VSMC apoptosis through the angiotensin II type 1 receptor (AT1R) pathway. Ang II also promotes the secretion of ECM, thus contributing to vascular remodeling. The Ang II type 2 receptor (AT2R) antagonizes AT1R and decreases cell proliferation and migration [7, 8]. Our previous studies demonstrated that overexpression of AT2R significantly decreased neointimal hyperplasia in balloon-injured carotid arteries in rats [9]. In physiologic conditions, AT2R expression decreases rapidly after birth. In adult mammals, it is only expressed in the adrenal gland, uterus, ovaries, and specific functional sites of the brain at very low levels; it is not expressed at all in cardiovascular tissues [10, 11]. Serious consequences may arise if expression of an exogenous AT2R gene is not controlled. It has been reported that chronic overexpression of AT2R can result in impaired myocardial contractility in transgenic mice [12]. A high level of ventricular-specific expression of AT2R was reported to cause dilated cardiomyopathy and heart failure in transgenic mice [13]. A recent study also showed that AT2R induced cell apoptosis in a dose-dependent manner and that moderate cardiac-selective overexpression of AT2R protects cardiac functions from ischemic injury [14]. These findings suggest that the effects of AT2R may depend on the level of AT2R expression, and the in vivo expression of AT2R gene must then be tightly regulated. Mesenchymal stem cells (MSCs) are non-hematopoietic multipotent cells able to differentiate into a number of cell types, including VSMCs, endothelial cells (ECs), and cardiomyocytes [15]. Compared with other differentiated cells, MSCs show some advantages [16, 17]. MSCs can be easily obtained in an abundant manner from diverse tissues, such as the bone marrow. In addition, MSCs present tissue regeneration potential, anti-inflammatory abilities, immunomodulatory properties, and high injury homing abilities. Because of those characteristics, MSC-based therapies have been used for a variety of diseases, including cardiovascular diseases. Given the recent progresses in gene therapy, genetic engineering allows a further broadening of the therapeutic benefits of primary MSCs.
Our previous study showed that the use of a tetracycline-regulated system resulted in a tight control of transfected gene expression in VSMCs. Therefore, the present study was performed to engineer rat MSCs to express the AT2R gene in a tetracycline-regulated system and to investigate whether these engineered cells inhibit neointima formation after balloon-induced vascular injury in rat models.
Materials and Methods
Animals
Male Sprague–Dawley (SD) rats (80–100 g) were purchased from the Experimental Animal Center of the Third Military Medical University (Chongqing, China). We used animals conforming to the European Union’s guiding principles for the care and use of experimental animals.
Plasmids and Cells
An AT2R gene fragment was cloned by homologous recombination into the expression vector pUHD10-3 containing TetO repeat sequences, to establish a doxycycline (Dox)-regulated mammalian expression system (Dox-On system) based on the regulator plasmid pUHD 17-1hyg (a kind gift from Dr. L. Ronnstrand, Ludwig Institute for Cancer Research, Sweden). pUHD 10-3 was a gift from Dr. C. Lindon (Cancer Research Institute, Cambridge, UK). The fluorescence reporter plasmid pUHC 13-3 was a gift from Dr. C. Lindon and Dr. L. Ronnstrand. The neomycin screening-resistant simple plasmid pSV2 neo was a gift from Dr. H.Y. Park (Boston University School of Medicine, MA, USA). MSCs were harvested from femurs and tibias of donor rats and isolated using a density gradient to eliminate unwanted cell types before subculturing, harvesting, and reinoculation. Single cell-derived colonies were expanded and used for experiments.
MSC Lines Expressing Dox-Regulated AT2R (C5 Cells)
Double-stable expression of a Dox-regulated AT2R gene in MSC lines was performed as previously described [18–20]. Briefly, MSCs were digested with trypsin and inoculated in 60-mm culture dishes at a density of 5 × 103 cells/ml. After the first round of transfection, MSCs were transfected with pUHD17-1hyg, according to the instructions of a liposome transfection kit (Roche Molecular Systems, Pleasanton, CA). Luciferase expression in 30 hygromycin-resistant MSC clones was detected by transient transfection assay, and MSC clones with the highest Dox-induced expression and the lowest background were considered Dox-On MSC lines. After a second round of transfection, Dox-On MSCs were co-transfected with pUHD10-3/AT2R or pSV2 neo plasmids; 30 large, healthy G418-resistant clones were preserved for reverse transcriptase polymerase chain reaction (RT-PCR) determination of AT2R mRNA expression. Primer sequences were as follows: rat AT2R primers (707 bp): sense 5′-TGA TAA TCT CAA CGC AAC TGG-3′ and antisense 5′-TCA AGA CTT GGT CAC GGG TAA-3′; GAPDH primers (452 bp): sense 5′-ACC ACA GTC CAT GCC ATC AC-3′ and antisense 5′-TCC ACC ACC CTG TTG CTG TA-3′. Clones with low background and high Dox-induced expression of AT2R mRNA were used for experiments. We designated these clones as C5 cells.
Balloon-Induced Carotid Artery Injury and MSC Transplantation
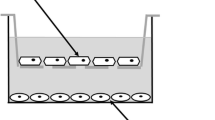
Rat models for balloon-induced carotid artery injury and MSC transplantation were generated as previously described [21–23]. For experimental groups, rats were randomly divided into five groups (n = 6 per group). Rats in the control group were not injured with balloon. Rats in the injury, MSC, C5, and C5+Dox groups were all submitted to balloon-induced injury. Rats from the MSC, C5, and C5+Dox groups were respectively transplanted with MSCs, C5 cells without Dox treatment, and C5 cells with Dox treatment.
To establish rat models of balloon-induced carotid artery injury and MSC transplant, male SD rats (380–450 g) were anesthetized by intraperitoneal injection of pentobarbital (30 mg/kg). After successful anesthesia, a median incision was performed in the neck. Heparin sodium (100 U/kg) was administered via the external jugular vein. The bifurcation of the left common carotid artery and the external and internal carotid arteries were exposed. The proximal segment of the left common carotid artery and the internal carotid artery were occluded using atraumatic vascular clamps, and the distal segment of the external carotid artery was ligated to temporarily block blood flow. The external carotid artery was incised, and a guide wire with a 2.0-F balloon catheter (2.0-mm diameter) was inserted into the left common carotid artery through the incision, with the guide wire tip reaching the level of the aortic arch. The balloon was inflated to a pressure of 1.5 atm (1 atm = 101.325 kPa) and pushed and pulled three times to strip the endothelium. The balloon and guide wire were withdrawn, and 50 μl of MSC suspension (cell density of 1 × 104/ml) was infused via a perfusion catheter into the injured segment. In the injury alone group, PBS was infused instead of cells. The perfusion catheter was kept in place for 30 min, and heparin sodium (100 U/kg) was injected into the carotid, followed by ligation of the external carotid artery, restoration of blood flow from the common carotid artery to the internal carotid artery, and closure of the incision. In the Dox-treated group, Dox (100 μg/kg) was injected daily via the vena caudalis from the day of operation to the day before sacrifice. The final Dox concentration was determined by pilot experiments according to AT2R mRNA expression in the arterial wall following treatment with various Dox concentrations (0, 1, 10, 100, or 1,000 μg/kg).
At the 28th day after operation, the common carotid artery was isolated from six rats, and the injured vessel segments were harvested. Some vessel segments were washed three times with DEPC water and placed in liquid nitrogen. The remaining vessel segments were washed repeatedly with PBS, fixed 6 h in 4 % paraformaldehyde, and dehydrated in 30 % sucrose solution. Samples were subjected to frozen sectioning or paraffin embedding and sectioning.
Rats in the fluorescence labeling group were sacrificed at 4 days after operation. The cell-transplanted vessel segment was harvested, and the tunica adventitia was removed. Tissues were washed repeatedly with PBS and fixed 30 min in 4 % paraformaldehyde. Vessels were cut horizontally, spread onto a glass slide, covered with a coverslip, and observed under a TCS-NT 165123 laser confocal scanning microscopy (Leica Microsystems, Wetzlar, Germany).
Western Blotting
Immunoblotting was performed as previously described [24]. Double-stable MSC lines were treated with (1) 1 μg/ml Dox for 48 h or 72 h; (2) 0, 1 × 10−3, 1 × 10−2, 0.1, 1, 10, 102, 103, or 104 ng/ml Dox for 72 h; or (3) 1 μg/ml Dox for 72 h at 1, 2, 4, 6, or 8 weeks after transfection. Total proteins were extracted using a TriPureTM kit (Promega, Madison, WI, USA). Briefly, medium was removed, and the TriPure solution was added (1 ml/10 cm2 or 3 ml/5–10 × 106 cells) into culture flasks at room temperature. Cell protein extracts (50 μg) were collected for each group and subjected to SDS-PAGE, followed by transfer to nitrocellulose membranes. Membranes were blocked with 0.3 ml of rabbit anti-AT2R polyclonal antibody working solution (1:500, Santa Cruz Biotechnology, Santa Cruz, CA, USA) per square centimeter of membrane. Membranes were placed in a bag, shaken gently, and incubated at 4 °C overnight. Horseradish peroxidase-labeled secondary antibody (1:3,000) was added, and the membranes were incubated at room temperature for 1–1.5 h. Bands were visualized by chemiluminescence assay. Images were analyzed and protein expression was expressed in luminescence intensity.
RT-PCR
RT-PCR was performed as previously described [25]. Total RNA was extracted from rat carotid arteries 28 days after operation. Primer sequences were as described above. RT-PCR was performed with a Gene-Specific Relative RT-PCR kit (Promega, Madison, WI, USA), according to the manufacturer’s instructions.
Immunofluorescence
To analyze AT2R protein expression, frozen sections (2-μm thick) were transferred on glass slides, while cells were grown in chambers on glass slides. Briefly, sections and cells were incubated overnight at 4 °C with rabbit anti-AT2R polyclonal antibody (1:100, Santa Cruz Biotechnology, Santa Cruz, CA, USA). Sections and cells were washed and incubated with fluorescent probe-conjugated antibody for 30 min at room temperature. The absorbance was measured using the Image-Pro Plus 6.0 software (Media Cybernetics, Inc., Rockville, MD, USA).
Neointimal Hyperplasia Analysis
Carotid arteries were sectioned at a 7-μm thickness using a cryostat (Leica Microsystems, Wetzlar, Germany) from the middle segment of the vessels, at 0.5-mm intervals. Sections were stained with hematoxylin and eosin. Neointimal thickness was determined by subtracting the luminal surface area from the area of the internal elastic lamina. Thickness of tunica media was determined by subtracting the area of internal elastic lamina from the area of external elastic lamina. Morphometry was performed in a minimum of five sections of each arterial segment, and the lesion size was expressed as the intima/media (I/M) ratio. The thickness of intima or tunica media was measured using the Image-Pro Plus 6.0 software (Media Cybernetics, Inc., Rockville, MD, USA).
Statistical Analysis
All data are expressed as mean ± SD. All statistical analyses were performed using SPSS 13.0 (SPSS Inc., Chicago, IL, USA). Differences between groups were assessed using one-way ANOVA. Differences were considered significant if P < 0.05 or P < 0.01.
Results
Establishment of MSC Lines with Dox-Induced Double-Stable Expression of AT2R Gene (C5 Cells)
To establish the double-stable expression of a Dox-regulated AT2R gene in MSC lines, rat MSCs were subjected to two successive rounds of transfection with a tetracycline-inducible system. Transient luciferase expression was analyzed 48 h after the first round of transfection. MSC clones with low background expression and high Dox-induced luciferase expression were deemed Dox-On MSC lines. AT2R mRNA expression was analyzed by RT-PCR in several Dox-On MSC clones after the second round of transfection. Double-stable MSC lines were characterized by low background and high Dox-induced AT2R expression. These lines were screened, amplified, and designated as C5 cells.
AT2R Protein Expression in Dox-Induced Double-Stable MSC Lines
Immunofluorescence assay demonstrated the absence of the AT2R protein in the control and C5 groups (P > 0.05 vs. the control group). Dox-induced AT2R protein expression was observed in the C5 group after 48 h of 1 μg/ml Dox treatment (P < 0.05 vs. the control group) (Fig. 1a), and the expression was further enhanced after 72 h of 1 μg/ml Dox treatment (P < 0.05 vs. C5+Dox group after 48 h) (Fig. 1a).
Expression of AT2R in MSCs. a AT2R protein expression in double-stable MSC lines. *P < 0.05 vs. C5 group; # P < 0.05 vs. C5+Dox group after 48 h. b Cells were incubated with Dox for the indicated times to detect AT2R by Western blot. *P < 0.05 vs. 1-week time point without Dox. c Cells were incubated with various concentrations of Dox (10−3 to 104 ng/ml) for 72 h, and AT2R expression was determined by Western blot. *P < 0.05 vs. 0 ng/ml Dox
Meanwhile, sustained induced AT2R expression was determined in MSC lines. Results indicated that at 1, 2, 4, 6, and 8 weeks after transfection, treatment with 1 μg/ml Dox significantly induced AT2R protein expression in MSCs (P < 0.05 vs. 1-week time point without Dox), that there was no time effect on the expression (P > 0.05, between the Dox treatment groups at various time points), suggesting that AT2R gene expression was tightly regulated by Dox in the cell lines, and that it was stable within at least 8 weeks (Fig. 1b).
AT2R protein expression induced by various concentrations of Dox was determined in the MSC lines. Results demonstrated that Dox dose-dependently increased AT2R protein expression within the range of 1 × 10−3 to 104 ng/ml in MSC lines. Induced AT2R protein expression reached a peak at 1 × 102 ng/ml Dox and decreased at higher Dox concentrations (Fig. 1c).
Analysis of AT2R mRNA Expression in Arterial Wall
No AT2R mRNA expression was detected in the intact right common carotid artery in all groups. In the C5+Dox group, AT2R mRNA expression was dose-dependently increased from 10 to 1,000 μg/kg Dox. Compared to the group treated with 10 μg/kg Dox, the AT2R mRNA expression level was significantly higher in the groups treated with 100 or 1,000 μg/kg Dox, but there was no significant difference between the 100- and 1,000-μg/kg groups (data not shown). Results indicated that 100 μg/kg was the optimal Dox concentration for AT2R induction. Hence, 100 μg/kg Dox was used in the subsequent experiments. At 28 days after balloon-induced injury, low levels of AT2R mRNA expression were detected in the injury, MSC, and C5 groups (Fig. 3). Levels of AT2R mRNA expression were not significantly different between the three groups (P > 0.05). Results also demonstrated that treatment with C5 cells and Dox significantly increased AT2R mRNA expression in the vascular wall at 28 days after injury, compared to other groups (P < 0.01; Fig. 2).
Analysis of Osteopontin mRNA Expression in Arterial Wall
As shown in Fig. 3, a weak mRNA expression of osteopontin was detected in control groups. At 28 days after balloon-induced injury, mRNA expression of osteopontin increased significantly in injury, MSC, and C5 groups (P < 0.05 vs. the control group). The mRNA expression of osteopontin was lower in the C5+Dox group than the injury, MSC, and C5 groups (P < 0.05).
Analysis of AT2R Protein Expression in Arterial Wall
Immunofluorescence showed low AT2R expression in the intima, tunica media, and tunica adventitia at 28 days after injury in injury, MSC, and C5 groups. AT2R expression was significantly higher in the neointima of the Dox-treated group compared with the others (P < 0.01; Fig. 4).
Analysis of Neointimal Hyperplasia in Rat Carotid Arteries
At 28 days after balloon injury, neointima with varying degrees of hyperplasia was observed. Neointimal hyperplasia and luminal stenosis were observed in the injury, MSC, and C5 groups. The I/M ratio showed no significant differences between the three groups (P > 0.05). Neointimal hyperplasia was also observed in the C5+Dox group, but it was significantly milder than in any of the other injured groups. The I/M ratio was significantly lower in the C5+Dox group compared with the injury, MSC, and C5 groups (P < 0.01; Fig. 5).
Discussion
Post-percutaneous coronary intervention (PCI) restenosis is a complex and multifactorial process. Preventing excessive proliferation and migration of VSMCs following PCI is a major research focus. With the development of molecular biology, gene therapy became a promising option for managing post-PCI restenosis [26].
Recent studies showed that following vascular injury, MSCs adhere to the site of vascular injury and initiate site-specific expression of VSMC SM-α-actin or endothelial cell VIII factor [27–29]. These changes, along with VSMC migration from the tunica media, may contribute to restenosis after vascular injury. Although MSCs have been demonstrated to differentiate into endothelial cells or VSMCs under certain conditions, whether MSCs contribute to repair or to hyperplasia after vascular intimal injury is still controversial [30, 31]. In the present study, we established rat models for balloon-induced endothelial injury of the common carotid artery and isolated, purified, and DAPI-labeled rat MSCs. To allow MSCs to adhere to the site of vascular injury, blood flow was blocked for 30 min, during which the purified MSCs were infused into blood vessels. Laser confocal scanning microscopy 4 days after cell transplantation indicated blue fluorescence-emitting cells on the vascular luminal surface, suggesting that the transplanted MSCs adhered to and grew at the site of vascular injury. At the 28th day after cell transplantation, significant neointimal hyperplasia was observed in the injury group, but there were no significant differences in the degree of neointimal hyperplasia between the MSCs and the injury groups. These results demonstrated that MSCs contributed to neointimal formation after balloon-induced injury but did not significantly influence the degree of neointimal hyperplasia or the ultimate luminal area. The causes for this phenomenon may be attributed to the fact that MSCs adhered to the vascular wall and differentiated into VSMCs or endothelial cells. A temporary increase in the number of VSMCs may result in intimal hyperplasia; meanwhile, accelerated endothelialization can antagonize intimal hyperplasia. As a result, MSC transplantation alone was unable to inhibit intimal formation after vascular injury, which is in agreement with a previous study demonstrating that bone marrow monoclonal cell transplantation does not influence restenosis incidence after PCI [32].
Many cytokines and vasoactive substances participate in the development of restenosis. Ang II induces VSMCs to proliferate, migrate, and secrete extracellular matrix mainly via AT1R, which can result in neointima formation and subsequent restenosis [33–36]. Most of the biological effects of Ang II are mediated by AT1R. Therefore, restenosis might be prevented and treated by inhibiting the rennin-angiotensin system through the use of angiotensin-converting enzyme (ACE) inhibitors or AT1R blockers. Animal experiments demonstrated that inhibiting the rennin-angiotensin system significantly attenuates neointimal formation and restenosis. Nevertheless, effective doses of ACE inhibitors or angiotensin receptor blockers (ARBs) used in animal experiments were too high to use in a clinical setting and for patients to tolerate. Though conventional doses of ACE inhibitors or ARBs decrease the incidence of cardiovascular events, restenosis incidence is not reduced accordingly [37].
AT2R function is less well defined. Studies suggest that many biological effects mediated by AT2R antagonize those of AT1R [11, 12]. Increasing AT2R expression may prevent excessive intimal hyperplasia following vascular injury [38]. Our previous studies also showed that adenovirus-mediated transfection of the AT2R gene relieves intima proliferation in injured carotid arteries in rats. Taken together, enhancing AT2R expression and activity at the site of vascular injury may be a new method for preventing restenosis following PCI. However, AT2R expression is normally low or absent in cardiovascular tissues, and expression of the introduced AT2R may be uncontrolled. Therefore, active control of the introduced AT2R gene is desired.
In clinical applications, the expression of exogenous genes used in gene therapy must be regulated according to therapeutic goals and to the nature of the diseases. Product concentration must be held within a therapeutic window to achieve optimal therapeutic outcomes. Excessive or inappropriate expression of the AT2R gene would have no effect on intimal hyperplasia and might even cause adverse consequences. The Tet-On gene expression regulation system is safe, precise, efficient, and tightly regulated, showing promising advantages for gene therapy development [39, 40]. Using in vitro transfection and screening, we obtained MSCs with Dox-regulated double-stable expression of the AT2R gene and introduced them at the sites of vascular injury. Significant AT2R gene expression was observed in the injured vessels, particularly in neointima, even at the 28th day after AT2R gene transfection and Dox treatment, which was significantly higher than in the other groups. AT2R gene expression differences were not significant between the injury, MSC, and C5 groups at various time points. However, at the 28th day after transplantation of AT2R gene-modified MSCs combined with Dox treatment, the neointima area and I/M ratio were significantly decreased compared with the other groups. These results suggest that AT2R gene expression in injured vessels is precisely regulated by exogenous Dox and that excessive neointima hyperplasia at these sites was significantly suppressed, even 28 days after vascular injury.
In addition, vascular remodeling also participates in restenosis. Previous studies reported that osteopontin contributes to vascular remodeling after vascular injury [41]. Our results showed that osteopontin mRNA expression levels were significantly increased after balloon-induced injury. Treatment with C5 and Dox inhibited injury-inducible osteopontin mRNA expression, suggesting that controlled AT2R expression can modulate vascular remodeling.
In the present study, MSCs transfected with the AT2R gene were transplanted to injured vessels to achieve a high-efficiency and targeted gene expression. Dox was successfully used to regulate in vivo AT2R expression. Dox-On-regulated mammalian gene expression system allowed AT2R to be expressed under a tight active control and could be applied to patients developing restenosis following vascular injury. The Dox-On-regulated mammalian gene expression system could maximize the positive effects of AT2R gene expression and minimize negative effects. In future studies, the underlying molecular mechanisms of these protective effects of MSCs transfected with AT2R in vascular injury should be explored, as well as long-term AT2R gene expression. The present study suggests that transplantation of MSCs with a conditional AT2R gene expression could be an effective method for preventing neointimal formation in vascular injury-associated diseases.
References
Zargham, R., & Thibault, G. (2005). Alpha 8 beta1 integrin expression in the rat carotid artery: involvement in smooth muscle cell migration and neointima formation. Cardiovascular Research, 65(4), 813–822.
Lee, S., Lim, H. J., Park, H. Y., Lee, K. S., Park, J. H., & Jang, Y. (2006). Berberine inhibits rat vascular smooth muscle cell proliferation and migration in vitro and improves neointima formation after balloon injury in vivo. Berberine improves neointima formation in a rat model. Atherosclerosis, 186(1), 29–37.
Zhang, L., Sivashanmugam, P., Wu, J. H., Brian, L., Exum, S. T., Freedman, N. J., et al. (2008). Tumor necrosis factor receptor-2 signaling attenuates vein graft neointima formation by promoting endothelial recovery. Arteriosclerosis, Thrombosis, and Vascular Biology, 28(2), 284–289.
Yamada, T., Kondo, T., Numaguchi, Y., Tsuzuki, M., Matsubara, T., Manabe, I., et al. (2007). Angiotensin II receptor blocker inhibits neointimal hyperplasia through regulation of smooth muscle-like progenitor cells. Arteriosclerosis, Thrombosis, and Vascular Biology, 27(11), 2363–2369.
Brassard, P., Amiri, F., & Schiffrin, E. L. (2005). Combined angiotensin II type 1 and type 2 receptor blockade on vascular remodeling and matrix metalloproteinases in resistance arteries. Hypertension, 46(3), 598–606.
Huang, F., Thompson, J. C., Wilson, P. G., Aung, H. H., Rutledge, J. C., & Tannock, L. R. (2008). Angiotensin II increases vascular proteoglycan content preceding and contributing to atherosclerosis development. Journal of Lipid Research, 49(3), 521–530.
Lemarié, C. A., & Schiffrin, E. L. (2010). The angiotensin II type 2 receptor in cardiovascular disease. Journal of the Renin-Angiotensin-Aldosterone System, 11(1), 19–31.
Zhu, Y. C., Zhu, Y. Z., Lu, N., Wang, M. J., Wang, Y. X., & Yao, T. (2003). Role of angiotensin AT1 and AT2 receptors in cardiac hypertrophy and cardiac remodelling. Clinical and Experimental Pharmacology and Physiology, 30(12), 911–918.
Tang, B., Ma, S., Yang, Y., Yang, D., Chen, J., Su, X., et al. (2011). Overexpression of angiotensin II type 2 receptor suppresses neointimal hyperplasia in a rat carotid arterial balloon injury model. Molecular Medica Report, 4(2), 249–254.
Takeda-Matsubara, Y., Matsubara, K., Ochi, H., Ito, M., Iwai, M., & Horiuchi, M. (2003). Expression of endothelial angiotensin II receptor mRNA in pregnancy-induced hypertension. American Journal of Hypertension, 16(12), 993–999.
Perlegas, D., Xie, H., Sinha, S., Somlyo, A. V., & Owens, G. K. (2005). ANG II type 2 receptor regulates smooth muscle growth and force generation in late fetal mouse development. American Journal of Physiology - Heart and Circulatory Physiology, 288(1), H96–102.
Nakayama, M., Yan, X., Price, R. L., Borg, T. K., Ito, K., Sanbe, A., et al. (2005). Chronic ventricular myocyte-specific overexpression of angiotensin II type 2 receptor results in intrinsic myocyte contractile dysfunction. American Journal of Physiology - Heart and Circulatory Physiology, 288(1), H317–327.
Yan, X., Price, R. L., Nakayama, M., Ito, K., Schuldt, A. J., Manning, W. J., et al. (2003). Ventricular-specific expression of angiotensin II type 2 receptors causes dilated cardiomyopathy and heart failure in transgenic mice. American Journal of Physiology - Heart and Circulatory Physiology, 285(5), H2179–2287.
Qi, Y., Li, H., Shenoy, V., Li, Q., Wong, F., Zhang, L., et al. (2012). Moderate cardiac-selective overexpression of angiotensin II type 2 receptor protects cardiac functions from ischaemic injury. Experimental Physiology, 97(1), 89–101.
Durik, M., Sevá Pessôa, B., & Roks, A. J. (2012). The renin-angiotensin system, bone marrow and progenitor cells. Clinical Science (London), 123(4), 205–223.
Wu, H., Ye, Z., & Mahato, R. I. (2011). Genetically modified mesenchymal stem cells for improved islet transplantation. Molecular Pharmaceutics, 8(5), 1458–1470.
Godoy, J. A., Block, D. B., Tollefsen, D. M., Werneck, C. C., & Vicente, C. P. (2011). Dermatan sulfate and bone marrow mononuclear cells used as a new therapeutic strategy after arterial injury in mice. Cytotherapy, 13(6), 695–704.
Freundlieb, S., Schirra-Muller, C., & Bujard, H. (1999). A tetracycline controlled activation/repression system with increased potential for gene transfer into mammalian cells. The Journal of Gene Medicine, 1(1), 4–12.
Baron, U., & Bujard, H. (2000). Tet repressor-based system for regulated gene expression in eukaryotic cells: principles and advances. Methods in Enzymology, 327, 401–421.
Koponen, J. K., Kankkonen, H., Kannasto, J., Wirth, T., Hillen, W., Bujard, H., et al. (2003). Doxycycline-regulated lentiviral vector system with a novel reverse transactivator rtTA2S-M2 shows a tight control of gene expression in vitro and in vivo. Gene Therapy, 10(6), 459–466.
Ando, H., Fukuda, N., Kotani, M., Si, Y., Kunimoto, S., Matsumoto, K., et al. (2004). Chimeric DNA-RNA hammerhead ribozyme targeting transforming growth factor-bete 1 mRNA inhibits neointima formation in rat carotid artery after balloon injury. European Journal of Pharmacology, 483(2–3), 207–214.
Ohtani, K., Egashira, K., Usui, M., Ishibashi, M., Hiasa, K. I., Zhao, Q., et al. (2004). Inhibition of neointimal hyperplasia after balloon injury by cis-element decoy of early growth response gene-1 in hypercholesterolemic rabbits. Gene Therapy, 11(2), 126–132.
Kang, H. J., Kim, H. S., Zhang, S. Y., Park, K. W., Cho, H. J., Koo, B. K., et al. (2004). Effects of intracoronary infusion of peripheral blood stem-cells mobilised with granulocyte-colony stimulating factor on left ventricular systolic function and restenosis after coronary stenting in myocardial infarction: the MAGIC cell randomised clinical trial. Lancet, 363(9411), 751–756.
Spak, E., Ewert, S., Vieth, M., Fändriks, L., Aneman, A., Olausson, M., et al. (2006). Angiotensin II receptor expression following intestinal transplantation in mice. Journal of Surgical Research, 135(1), 144–149.
An, S. J., Boyd, R., Wang, Y., Qiu, X., & Wang, H. D. (2006). Endothelin-1 expression in vascular adventitial fibroblasts. American Journal of Physiology - Heart and Circulatory Physiology, 290(2), H700–708.
Li, W., Tanaka, K., Ihaya, A., Fujibayashi, Y., Takamatsu, S., Morioka, K., et al. (2005). Gene therapy for chronic myocardial ischemia using platelet-derived endothelial cell growth factor in dogs. American Journal of Physiology - Heart and Circulatory Physiology, 288(1), H408–415.
Sahara, M., Sata, M., Morita, T., Nakamura, K., Hirata, Y., & Nagai, R. (2007). Diverse contribution of bone marrow-derived cells to vascular remodeling associated with pulmonary arterial hypertension and arterial neointimal formation. Circulation, 115(4), 509–517.
Soda, T., Suzuki, H., Iso, Y., Kusuyama, T., Omori, Y., Sato, T., et al. (2007). Bone marrow cells contribute to neointimal formation after stent implantation in swine. International Journal of Cardiology, 121(1), 44–52.
Schroeter, M. R., Leifheit, M., Sudholt, P., Heida, N. M., Dellas, C., Rohm, I., et al. (2008). Leptin enhances the recruitment of endothelial progenitor cells into neointimal lesions after vascular injury by promoting integrin-mediated adhesion. Circulation Research, 103(5), 536–544.
Hu, Y., Davison, F., Ludewig, B., Erdel, M., Mayr, M., Url, M., et al. (2002). Smooth muscle cells in transplant atherosclerotic lesions are originated from recipients, but not bone marrow progenitor cells. Circulation, 106(14), 1834–1839.
Shoji, M., Sata, M., Fukuda, D., Tanaka, K., Sato, T., Iso, Y., et al. (2004). Temporal and spatial characterization of cellular constituents during neointimal hyperplasia after vascular injury: potential contribution of bone-marrow-derived progenitor to arterial remodeling. Cardiovascular Pathology, 13(6), 306–312.
Wollert, K. C., Meyer, G. P., Lotz, J., Ringes-Lichtenberg, S., Lippolt, P., Breidenbach, C., et al. (2004). Intracoronary autologous bone marrow cell transfer after myocardial infarction: the BOOST randomized controlled clinical trial. Lancet, 364(9429), 141–148.
Zheng, Y., Song, H. J., Kim, C. H., Kim, H. S., Kim, E. G., Sachinidis, A., et al. (2004). Inhibitory effect of epigallocatechin 3-O-gallate on vascular smooth muscle cell hypertrophy induced by angiotensin II. Journal of Cardiovascular Pharmacology, 43(2), 200–208.
Sales, V. L., Sukhova, G. K., Lopez-Ilasaca, M. A., Libby, P., Dzau, V. J., & Pratt, R. E. (2005). Angiotensin type 2 receptor is expressed in murine atherosclerotic lesions and modulates lesion evolution. Circulation, 112(21), 3328–3336.
Browatzki, M., Larsen, D., Pfeiffer, C. A., Gehrke, S. G., Schmidt, J., Kranzhofer, A., et al. (2005). Angiotensin II stimulates matrix metalloproteinase secretion in human vascular smooth muscle cells via nuclear factor-kappaB and activator protein 1 in a redox-sensitive manner. Journal of Vascular Research, 42(5), 415–423.
Jugdutt, B. I., & Menon, V. (2003). Upregulation of angiotensin II type 2 receptor and limitation of myocardial stunning by angiotensin II type 1 receptor blockers during reperfused myocardial infarction in the rat. Journal of Cardiovascular Pharmacology and Therapeutics, 8(3), 217–226.
Dendorfer, A., Dominiak, P., & Schunkert, H. (2005). ACE inhibitors and angiotensin II receptor antagonists. Handbook of Experimental Pharmacology, 170, 407–442.
Bove, C. M., Yang, Z., Gilson, W. D., Epstein, F. H., French, B. A., Berr, S. S., et al. (2004). Nitric oxide mediates benefits of angiotensin II type 2 receptor overexpression during post-infarct remodeling. Hypertension, 43(3), 680–685.
Gossen, M., & Bujard, H. (1992). Tight control of gene expression in mammalian cells by tetracycline-responsive promoters. Proceedings of the National Academy of Sciences of the United States of America, 89(12), 5547–5551.
Gossen, M., Freundlieb, S., Bender, G., Müller, G., Hillen, W., & Bujard, H. (1995). Transcriptional activation by tetracyclines in mammalian cells. Science, 268(5218), 1766–1769.
Isoda, K., Nishikawa, K., Kamezawa, Y., Yoshida, M., Kusuhara, M., et al. (2002). Osteopontin plays an important role in the development of medial thickening and neointimal formation. Circulation Research, 91(1), 77–82.
Acknowledgments
The authors thank Dr. L. Ronnstrand (Ludwig Institute for Cancer Research), Dr. C. Lindon (Cancer Research UK Institute, Cambridge, UK), and Dr. H.Y. Park (Boston University School of Medicine, Boston, MA, USA) for supplying the plasmids. This study was supported by the National Natural Science Foundation of China (Nos. 30400180, 31300946, and 81370212).
Conflict of Interest
The authors report no conflict of interest.
Statement
No human studies were carried out by the authors for this article. All institutional and national guidelines for the care and use of laboratory animals were followed and approved by the appropriate institutional committees.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Paul J. R. Barton oversaw the review of this article
Jian Feng and Jian-Ping Liu contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Feng, J., Liu, JP., Miao, L. et al. Conditional Expression of the Type 2 Angiotensin II Receptor in Mesenchymal Stem Cells Inhibits Neointimal Formation After Arterial Injury. J. of Cardiovasc. Trans. Res. 7, 635–643 (2014). https://doi.org/10.1007/s12265-014-9576-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-014-9576-2