Abstract
The biomarkers CXCR4/FLK-1 select cardiac progenitors from a stem cell pool in experimental models. However, the translational value of these cells in human ischemic heart disease is unknown. Here, flow-cytometry identified CD45−/CXCR4+/FLK-1+ cells in 30 individuals without ischemic heart disease and 33 first-time acute myocardial infarction (AMI) patients. AMI patients had higher CD45−/CXCR4+/FLK-1+ cell-load at 48-h and 3- and 6-months post-AMI (p = 0.003,0.04,0.04, respectively) than controls. Cardiovascular risk factors and left ventricular (LV) ejection fraction were not associated with cell-load. 2D-speckle-tracking strain echocardiography assessment of LV systolic function showed improvement in longitudinal strain and dyssynchrony during follow-up associated with longitudinal increases in and higher 48-h post-AMI CD45−/CXCR4+/FLK-1+ cell-load (r = −0.525, p = 0.025; r = −0.457, p = 0.029, respectively). In conclusion, CD45−/CXCR4+/FLK-1+ cells are present in adult human circulation, increased in AMI and associated with improved LV systolic function. Thus, CD45−/CXCR4+/FLK-1+ cells may provide a diagnostic tool to follow cardiac regenerative capacity and potentially serve as a prognostic marker in AMI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The self-renewal capacity of the heart is important for cardiac homeostasis but insufficient to ensure reconstitution of lost cardiomyocytes following massive cardiac injury [1–3]. Moreover, individual variation in the endogenous regenerative response may further contribute to long-term outcome following an acute event [4]. Autologous stem cell transplant to augment innate reparative mechanisms has proven to be feasible and safe but has been limited by disparate results [5–10]. This has been, in part, attributed to heterogeneity of cell populations delivered and the incomplete targeting of patient-specific regenerative deficiencies [11, 12]. Quantification and prediction of individual regenerative capacity through the development of theranostic cell therapy platforms to inform individualized patient management would therefore have both diagnostic and therapeutic value [13].
In this regard, mobilization of immature, tissue-specific progenitor cells into the peripheral circulation has been advocated as a marker of an organism’s regenerative capacity [14, 15]. Experimental and clinical studies have confirmed that circulating endothelial progenitor cells (EPC) identified by cell surface markers using flow sorting analysis [16] have a role in vascular regeneration [17]. EPC are capable of differentiating into endothelial cells [18, 19], are spontaneously mobilized hours to days following acute myocardial infarction (AMI) [20, 21], and are predictive of cardiovascular events and death in patients with stable coronary artery disease [22, 23]. Similarly, contributing at least in part to cardiac repair and homeostasis are extra-cardiac precursors as confirmed by the significant chimerism of female donor hearts in male transplant recipients of which 7–10 % of myocytes, coronary arterioles, and capillaries displayed Y chromosomes [24].
These findings have been further bolstered by the observation that the bone marrow harbors subpopulations of non-hematopoietic progenitor cells that are mobilized acutely in response to ST elevation myocardial infarction in a pattern similar to EPC [25]. The mobilization of these cells also mirrors a rise in endothelial, muscle and cardiac specific markers, while a subset of this population appears to be chemo-attracted to the ischemic myocardium in vitro [25, 26]. This suggests that a subpopulation of bone-marrow-derived cardiac progenitors may be mobilized for cardiac repair following AMI in humans.
Through comprehensive, whole-genome transcriptional profiling, we have previously shown that CXCR4, a chemokine receptor for the stromal derived factor-1 (SDF-1), in conjunction with the mesoderm-specific VEGF receptor type II, FLK-1, are stage and lineage specific biomarkers of cardiac progenitor cells [27]. Indeed, CXCR4+/FLK-1+ cells identified a pre-cardiac developmental transcriptome that distinguished this phenotype from the overall stem cell pool. Moreover, differentiation of CXCR4+/FLK-1+ progenitors yielded progeny with phenotypic characteristics consistent with nascent cardiac tissue such as nuclear translocation of myocardial transcription factors and robust sarcomerogenesis with beating activity and calcium transients [27]. The CXCR4+/FLK-1+ biomarker pair may therefore enable effective isolation of putative cardiac progenitor cells and quantification of cardiac regenerative capacity, although this has not been tested to date in humans.
We herein hypothesized that putative cardiac tissue-committed cells identified by cell surface markers CXCR4 and FLK-1 circulate in the peripheral blood of human subjects and can be mobilized in the setting of AMI. Utilizing flow-cytometry cell sorting analysis, non-hematopoietic CXCR4+/FLK-1+ progenitor cells were here identified in humans, were upregulated following AMI, and were associated with improved left ventricular systolic function. Circulating, non-hematopoietic CXCR4+/FLK-1+ cells may therefore represent a novel marker of cardiac regenerative capacity, and a potential prognostic indicator in the setting of ischemic heart disease.
Methods
Subjects and Control Subjects
All subjects with elevated troponin hospitalized at the Mayo Clinic, Rochester, MN were screened daily for study enrollment over the course of a 12-month period. Inclusion criteria included ages of 18–65 with first-time diagnosis of AMI, no known previous history of cardiac disease, and signed written informed consent. AMI was defined according to the Universal Definition of Myocardial Infarction consensus statement by the Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction as detection of a rise and/or fall of cardiac troponin with at least one value above the 99th percentile of the upper limit of normal in conjunction with evidence of myocardial ischemia such as symptoms of ischemia, ECG changes including ST-T changes, new left bundle branch block, or development of pathological Q waves or imaging evidence of new loss of viable myocardium or new wall motion abnormality [28]. STEMI was defined as new ST elevation at the J-point in two contiguous leads with the cutoff points: ≥0.2 mV in men or ≥0.15 mV in women in leads V2–V3 and/or ≥0.1 mV in other leads. NSTEMI was defined as new horizontal or down-sloping ST depression ≥0.05 mV in two contiguous leads; and/or T inversion ≥0.1 mV in two contiguous leads with prominent R-wave or R/S ratio >1 [28].
Exclusion criteria were enrollment in a cardiac rehabilitation program within the 6-months prior to the AMI event; history of cardiovascular diseases including previous coronary artery disease (CAD), coronary bypass surgery, heart failure, stroke or peripheral vascular disease, atrial fibrillation, pacemaker placement; clinical or biochemical evidence of other comorbidities such as cancer, rheumatoid arthritis, liver disease, myeloproliferative disorders; and inability to understand the consent form. Control subjects were recruited from the Mayo Clinic Rochester echocardiography laboratory and were matched by age and sex to the AMI patient cohort. Control subjects had no previous history of cardiac diseases or other comorbidities, and had a normal echocardiogram.
Following diagnostic work-up, patients underwent coronary interventions as indicated and standard medical management including initiation of aspirin, a second anti-platelet agent such as clopidogrel, a statin and a beta blocker at the Mayo Clinic inpatient Cardiology service. Furthermore, all patients were enrolled in and completed a cardiovascular rehabilitation program, during which medications were closely monitored; they received counseling for management of cardiovascular risk factors, and they participated in a structured cardiac rehabilitation exercise program. Within 48 h following recruitment (baseline), all AMI patients and control subjects underwent echocardiography. Follow-up evaluations were performed at 3 and 6 months after initial testing in AMI patients. All participants provided a signed informed consent. This study was approved by the Mayo Clinic Institutional Review Board.
Blood Sample Collection and Testing
Blood samples were obtained from AMI patients and control subjects within 48-h of enrollment and from AMI patients at 3 and 6 months post-AMI. Blood (10 mL) was collected at each time point in evacuated plastic tubes anticoagulated with ethylenediaminetetraacetic acid. Five milliliters of this blood was used to perform additional tests for glucose, creatinine, cardiac troponins, glycated hemoglobin, high sensitivity C-reactive protein, fibrinogen and a standard serum lipid profile including high-density lipoprotein (HDL), low-density lipoprotein, total cholesterol and triglycerides. The remaining 5 mL of blood sample was used for quantification of CD45−/CXCR4+/FLK-1+ cells as described below.
Quantification of CD45−/CXCR4+/FLK-1+ Cells
CD45−/CXCR4+/FLK-1+ cells obtained from AMI and control subjects at baseline and from AMI patients at 3 and 6 months were quantified by flow-cytometry [27]. Nucleated cells were fractionated from 5 mL of whole blood and immunostained with FITC-conjugated mouse anti-human CD45 monoclonal antibody (BD Biosciences), PE-conjugated mouse anti-human CD184 (anti-CXCR4; BD Biosciences), and APC-Cy7 conjugated rat anti-mouse FLK-1 monoclonal antibody (BD Biosciences). After incubation, cells were washed with PBS and resuspended in 3 % para-formaldehyde. Cell fluorescence was measured immediately after staining using a BD Biosciences FACSCalibur analog flow cytometer running CellQuest Pro software (FACSCalibur, BD Biosciences). Side and forward scatter parameters were used to gate on viable cell populations sorted into subpopulations. Absolute cell counts were obtained after measurement of 1,000,000 events. In order to specifically assess the extent of mobilization of CD45−/CXCR4+/FLK-1+ cells and their association with post-infarction myocardial recovery, total CD45−/CXCR4+/FLK-1+ cell count was standardized to the total CD45− population which includes the non-hematopoietic, mesenchymal stem cell population. This approach isolates the effect of CD45−/CXCR4+/FLK-1+ cell mobilization from that of total non-hematopoietic, mesenchymal stem cell mobilization, and total leukocyte count. In addition, assessment of the CD45− subset of CXCR4+/FLK-1+ cells specifically isolated non-hematopoietic, tissue-specific progenitors. Finally, a base 10 logarithmic transformation was applied to obtain a normalized cell-load distribution and to enable assessment of differences in variability of cell-load between cohorts. The standardized, log transformed cell count is herein referred to as CD45−/CXCR4+/FLK-1+ cell-load.
Definition of Risk Factors for AMI
Established cardiovascular risk factors were reviewed for all subjects at the time of recruitment into the study. History of smoking was defined as greater than a 2 pack-year history and/or smoking within the previous 12 months. History of hypertension was defined as multiple resting blood pressures at or above 140/90 mmHg on two different visits or greater than 1 year history of elevated blood pressure requiring initiation of anti-hypertensive therapy. Diagnosis of type II diabetes mellitus was defined as need for oral anti-diabetic drug therapy and/or insulin use. Family history of CAD required documented evidence of premature CAD in a first- or second-degree relative (men less than 55 and women less than 65 years of age). Body mass index (BMI) was calculated as weight/height2 (kg/m2). Any documented use of statins, aspirin, ACE inhibitors, and beta blocker prior to AMI was also determined. Use of these medications was reviewed at the 3- and 6-month follow-up. Cumulative risk factor burden was assessed for each patient by calculating a cardiovascular risk factor (CVRF) score as previously described [16]. Each of the following risk factors scored 1 point: male sex, BMI > 25, a positive history of hypertension, type II diabetes mellitus, history of smoking, family history of CAD, and an HDL cholesterol level below <40 mg/dL.
Echocardiographic Evaluation
AMI and control subjects had a transthoracic echocardiogram performed at baseline and AMI patients had follow-up echocardiograms at 3 and 6 months post-AMI. Echocardiograms were interpreted by an experienced cardiologist. Echocardiograms were performed with either a Sequoia (Siemens Medical Solutions USA, Inc.) or a Vivid 7 (GE Vingmed Ultrasound AS) system by a Registered Diagnostic Cardiac Sonographer following a standard imaging protocol in accordance with the ASE echocardiographic guidelines [29]. Left ventricular ejection fraction (LVEF) was measured by M-mode or 2D method at the parasternal long axis view using established clinical echocardiographic instruments. The cardiologist was blinded to subjects’ clinical records and cell-load measurements. Echocardiograms were reviewed to determine global LVEF as previously described [29].
A new method that evaluates myocardial mechanics called two-dimensional speckle-tracking echocardiography (2D-STE), which utilizes frame-by-frame tracking of discrete echodensities within the myocardium (speckles) to derive myocardial deformation and rate of deformation, termed strain and strain rate, has become an important echocardiographic tool for quantitative assessment of ventricular function [30, 31]. A distinct advantage of 2D-STE is the semi-automated and quantitative approach by which regional and global ventricular function is measured. In vivo and in vitro models of 2D strain and strain rate have demonstrated correlation and are in agreement with tagged magnetic resonance imaging and sonomicrometry [32–34]. Reference values for strain and strain rate have also been validated in a normal cohort without a prior history of cardiovascular disease [35].
Post-systolic shortening is myocardial deformation that occurs following aortic valve closure and is a sensitive marker of myocardial ischemia and tissue viability [36–39]. Dyssynchrony is the occurrence of strain after aortic valve closure and in the literature is used interchangeably with post-systolic shortening. Here, dyssynchrony was used in conjunction with strain and strain rate to evaluate myocardial mechanics.
Digital images were obtained from the three apical views (apical four-chamber, two-chamber, and long axis) for measurement of systolic peak longitudinal strain and strain rate. These images were analyzed offline by an experienced cardiologist board certified in echocardiography on a syngo Velocity Vector Imaging workstation (Siemens Medical Solutions USA, Inc, Malvern, PA). Images were manually traced at the myocardium close to the endocardial surface, with avoidance of papillary muscles and trabeculations. After satisfactory tracking was obtained, numerical and graphical displays of deformation parameters were generated automatically for a total of 16 segments. Peak global longitudinal strain was obtained by calculating the mean longitudinal strain for all segments. Each of the three apical views was also divided into three regions—apical, mid, and basal—and peak regional longitudinal strain was derived for each one. Dyssynchrony was calculated as the mean of the standard deviation of time to peak longitudinal strain (from the onset of the QRS complex) for all LV segments. Two standard deviations were added to this to obtain the 95th percentile value. A value above this was considered abnormal, and a normal population (without significant LV dyssynchrony) was defined as having <2 % of values above this cutoff [35].
LVEF, global longitudinal strain, the three composite measures of regional longitudinal strain, and dyssynchrony were correlated with cell-load at baseline, 3 months, 6 months, and with change in cell-load over time. Negative strain values indicate improved systolic function while positive values indicate worse systolic function.
Statistical Analyses
Comparison of baseline demographic, clinical and laboratory characteristics were conducted using the Mann–Whitney U test as all comparisons were between non-parametric continuous variables. Comparison of binary categorical variables was generated using the Pearson’s χ 2 test. Spearman’s rank correlation analysis was used to assess bivariate non-parametric correlations of cell-load versus cardiovascular risk factors and strain functional measures. To account for baseline differences in cardiovascular risk factors between AMI patients and control subjects, we conducted multivariate linear regression analyses with binary variable, history of AMI, as the primary predictor and adjusting for individual risk factors. Adjusted mean log cell-load values along with the respective coefficient of determination (R 2) and p-value for the beta-coefficient are reported for each adjustment. All hypothesis tests were conducted with a type I error rate of <5 % considered statistically significant. Analyses were all conducted using JMP 9 software (version 9.0.0.).
Results
Patient Demographic and Clinical Characteristics
Thirty-eight first-time AMI patients and 32 control subjects with no prior heart disease met eligibility criteria and provided written informed consent (Fig. 1). Following withdrawal or exclusion from the study, a total of 33 AMI patients and 30 control subjects were available for analysis at baseline. Four AMI patients were excluded from 3- and 6-month analysis due to coronary artery bypass graft surgery (2), withdrawal from study (1), and loss to follow-up (1), leaving 29 for follow-up analysis at 3- and 6-months.
The baseline demographic and clinical characteristics of the 33 AMI patients and 30 control subjects are summarized in Table 1. AMI and control cohorts were of similar age (53 [38.0–65.0] vs. 53.5 [33.0–65.0] years, p = 0.71, respectively). Patients who suffered an AMI had predictably higher number of risk factors as measured by the CVRF score (4 vs. 3, p < 0.001), higher prevalence of arterial hypertension (73 vs. 23 %, p < 0.001), greater BMI (31.9 vs. 28.6 kg/m2, p = 0.006) and lower HDL cholesterol (37 [24–172] vs. 44 [27–113], p = 0.012) than control subjects. However, there were no significant difference in other classical cardiovascular risk factors such as history of type II diabetes mellitus, history of smoking and family history of coronary artery disease. In addition, there were no differences with respect to use of statins, aspirin, ACE inhibitor and beta blocker therapy between control and AMI patient immediately prior to AMI. Moreover, the severity of ischemia was relatively mild as a majority of these patients suffered non-ST elevation MI (NSTEMI) as compared to ST elevation MI (STEMI; 22 vs. 12, respectively). Peak Troponin T was elevated in all AMI patients and ranged between 0.04–16.0 ng/mL. While AMI patients did have a lower baseline LVEF compared to control subjects (57 vs. 65 %, p = 0.005; Table 1), the majority retained significant global cardiac function after AMI. Furthermore, LVEF in AMI patients recovered within 3-months as there was no longer any differences between AMI patients and control subjects at either 3- or 6-months (64 vs. 65, p = 0.82; 66 vs. 65, p = 0.54, respectively; Fig. 2). Change in LVEF as well as 2D strain, strain rate, and dyssynchrony between baseline and 3 and 6 months was not associated with peak Troponin T levels indicating that change in LV systolic function over time was independent of baseline infarct severity. AMI patients had preserved LVEF and increased prevalence of NSTEMI versus STEMI likely resulting from a combination of early percutaneous coronary intervention, relatively young age and absence of previous history of CAD.
Left ventricular ejection fraction (LVEF) in acute myocardial infarction (AMI) patients less than 48-h post-AMI and 3 and 6 months post-AMI and in control subjects at time of referral to echocardiography clinic. Large and small bars perpendicular to data points represent median and interquartile range, respectively. Statistical significance was considered to be p<0.05. Asterisks represent statistically significant difference between groups
CD45−/CXCR4+/FLK-1+ Cell-Load is Upregulated in AMI Patients
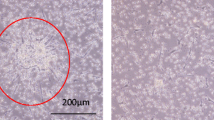
Flow-cytometry analysis isolated CD45− cells expressing CXCR4 and FLK-1 in the peripheral blood of AMI patients and control subjects (Fig. 3). Standardized to total CD45− cell count, CD45−/CXCR4+/FLK-1+ cell-load was increased in AMI patients compared to control subjects (p = 0.003). In contrast, analysis of total CD45−/CXCR4+ cell-load did not reveal a statistically significant difference between controls and AMI patients. Moreover, CD45−/CXCR4+/FLK-1+ cell-load remained significantly elevated in the circulation at 3- and 6-months (p = 0.04 for both time points) as compared to control subjects indicating prolonged, specific upregulation of CD45−/CXCR4+/FLK-1+ cells following myocardial infarction.
CD45−/CXCR4+/FLK-1+ cell-load is upregulated in acute myocardial infarction (AMI) patients less than 48-h post-AMI and 3 and 6 months post-AMI compared to control subjects at time of referral to echocardiography clinic. Large and small bars perpendicular to data points represent median and interquartile range, respectively. Statistical significance was considered to be p < 0.05. Asterisks represent statistically significant difference between groups
CD45−/CXCR4+/FLK-1+ Cell-Load is Independent of Cardiovascular Risk Factors
The two cohorts at baseline had differences in overall CVRF score, BMI, and HDL. Despite adjustment for these baseline differences in individual cardiovascular factors CD45−/CXCR4+/FLK-1+, cell-load remained significantly elevated in AMI patients compared to control subjects for all variables (Table 2). Cumulative risk factors, measured by the CVRF score were not associated with CD45−/CXCR4+/FLK-1+ cell-load in either control subjects or AMI patients (p = 0.62; p = 0.30; respectively; Fig. 4). These findings indicate that differences in individual risk factors do not account for observed differences in CD45−/CXCR4+/FLK-1+ cell-load and that CD45−/CXCR4+/FLK-1+ cell-load is independent of both individual and total number of cardiovascular risk factors.
CD45−/CXCR4+/FLK-1+ cell-load is independent of cardiovascular risk factors. Spearman’s rank correlation of number of cardiovascular risk factors versus CD45−/CXCR4+/FLK-1+ cell-load in control subjects at time of referral to echocardiography lab (a) and in patients with acute myocardial infarction within 48-h of AMI (b). Cardiovascular risk factors included in the analysis are male sex, BMI > 25 kg/m2, HDL < 40 mg/dL, arterial hypertension, ever smoker, type II diabetes mellitus, and positive family history of coronary artery disease. Correlation coefficient (r) and corresponding p value are presented. Statistical significance was considered to be p < 0.05
CD45−/CXCR4+/FLK-1+ Cell-Load is Associated with Improved Cardiac Function
To assess possible association of CD45−/CXCR4+/FLK-1+ cells with outcome at 6-months, we correlated echocardiographic features of cardiac function with CD45−/CXCR4+/FLK-1+ cell-load. Analysis of global cardiac function as measured by LVEF showed no association with CD45−/CXCR4+/FLK-1+ cell-load. In contrast, 2D-STE demonstrated that AMI patients that had an increase in CD45−/CXCR4+/FLK-1+ cell-load over the first 6 months following the incident had improved systolic function after 6 months as measured by regional longitudinal strain function (r = −0.525, p = 0.025; Fig. 5). Similarly, there was an improvement in synchrony from 3 to 6 months associated with increased baseline levels of CD45−/CXCR4+/FLK-1+ cell-load (r = −0.457, p = 0.029) These measurements identified improvement in myocardial function associated with increases in CD45−/CXCR4+/FLK-1+ cell-load.
Change in CD45−/CXCR4+/FLK-1+ cell-load is associated with improvement in cardiac function. Spearman’s rank correlation of change in regional longitudinal strain from baseline to 6-months in AMI patients versus change in CD45−/CXCR4+/FLK-1+ cell-load over the same time period (a). Correlation coefficient and corresponding p value are presented. Statistical significance was considered to be p < 0.05. Bar graph showing change in CD45−/CXCR4+/FLK-1+ cell-load from baseline to 6-months in AMI patients versus change in cardiac function as measured by regional longitudinal strain (b). The right and left bars represent those with an improvement and deterioration in regional longitudinal strain, respectively. A positive change in strain indicates deterioration in cardiac function while a negative change indicates improvement in cardiac function. Error bars represent one standard error of the mean (SE)
Discussion
Mobilization of immature, tissue-specific progenitor cells into the peripheral circulation has been suggested as a marker of innate regenerative capacity [14]. Cells expressing early cardiac tissue-specific mRNA have been identified in a non-hematopoietic subpopulation of bone marrow mononuclear cells [25, 26], providing evidence for a mobile subpopulation of cardiac progenitors that may be capable of cardiac regeneration. To this end, stem cell derived progeny selected according to the CXCR4 cell surface marker, in combination with FLK-1, have been demonstrated to be uniquely equipped for de novo cardiac differentiation during embryonic development [27]. As demonstrated here, cell surface markers CXCR4+ and FLK-1+ selected for cells that are mobilized following AMI and associated with improvement in left ventricular systolic function and tissue viability in humans.
Previous experimental models of myocardial infarction have suggested that a subpopulation of bone marrow CXCR4+ progenitors cells that express endothelial, muscle, and cardiac tissue-specific markers are mobilized within 12-h following experimental myocardial infarction [25]. Here, quantification of CD45−/CXCR4+/FLK-1+ cell-load revealed significant upregulation in the peripheral blood of AMI patients within 48-h of AMI as compared to normal controls. This upregulation was unique to CD45−/CXCR4+/FLK-1+ cells and was not observed for the broader pool of CD45−/CXCR4+ cells suggesting a restricted mobilization response following AMI that does not include all subsets of non-hematopoietic CXCR4+ cells but does include the CD45−/CXCR4+/FLK-1+ subset. Moreover, compared to controls, CD45−/CXCR4+/FLK-1+ cell-load remained elevated at 3 and 6 month follow-up suggesting that these progenitors are mobilized into the peripheral blood following myocardial infarction. These findings are collectively supported by the known biological role of the CXCR4 receptor and its ligand SDF1 which are involved in stem cell migration, homing and intra-tissue retention [40, 41]. In fact, it has been shown that secretion of SDF1 by the ischemic myocardium enables site-specific localization of specific CXCR4+ progenitors to the injured myocardium raising the possibility that CD45−/CXCR4+/FLK-1+ cells are involved in myocardial regeneration [42, 43].
Since absolute progenitor cell numbers in the peripheral blood are very low even after an acute event, interpretation of precursor numbers requires careful adjustment for factors that can modulate progenitor cell mobilization such as age, medications and cardiovascular risk factors [15]. AMI patients in the present cohort had increased prevalence of arterial hypertension, higher BMI, and lower HDL cholesterol levels than controls at the time of myocardial infarction. Despite these differences, CD45−/CXCR4+/FLK-1+ cell-load remained significantly elevated in AMI patients after adjustment suggesting that upregulation of CD45−/CXCR4+/FLK-1+ cells is independent of individual cardiovascular risk factors. In addition, CD45−/CXCR4+/FLK-1+ cell-load was not associated with cumulative cardiovascular risk factors. This is in contrast with a study of 45 patients with CAD and 15 healthy controls that demonstrated an inverse correlation between cumulative risk factors and EPC level and function [44]. The association between cardiovascular risk factors and EPCs has since been confirmed in other studies [16, 45]. However, to our knowledge, this is the first demonstration of the relationship between non-hematopoietic CXCR4+ cells and those risk factors in patients with acute coronary syndrome.
Analysis of data from this study showed no relationship between baseline global LVEF or change in LVEF over time and CD45−/CXCR4+/FLK-1+ progenitor levels in AMI patients. 2D-STE has recently been shown to be a particularly useful tool for assessing regional myocardial dysfunction especially in patients with normal LVEF [46]. When we evaluated left ventricular function using 2D-STE and compared with progenitor cell numbers, we found that an increase in CD45−/CXCR4+/FLK-1+ progenitors from baseline to 6-months is associated with an improvement in regional longitudinal strain over the same time period. Improvement in dyssynchrony (post-systolic shortening) from 3 to 6 months was also associated with higher levels of CD45−/CXCR4+/FLK-1+ progenitors at baseline, indicating a quantitative improvement of myocardial mechanics despite a normal global LVEF [47, 48]. Taken together, these observations suggest that perhaps patients capable of initiating and maintaining a robust regenerative response through early mobilization of CD45−/CXCR4+/FLK-1+ cells are most likely to experience improvement in systolic function. These data establish the initial evidence for the role of CD45−/CXCR4+/FLK-1+ cells in myocardial recovery following AMI. They justify larger, appropriately powered validation studies that, in light of the magnitude of confounding compensatory and remodeling mechanisms, further evaluate the clinical significance of CD45−/CXCR4+/FLK-1+ progenitor cell mobilization in the regenerative response following AMI.
Although bioengineered stem cells have been a focus in the development of theranostic platforms [49], the putative role of CD45−/CXCR4+/FLK-1+ cells in cardiac regeneration as demonstrated herein offers a practical strategy to harness the endogenous prognostic and therapeutic value of autologous cells that may prove useful in optimization of care for patients following AMI. Measurement of endogenous regenerative capacity provides a unique opportunity to quantify the predisposition of a patient towards impaired self-renewal of damaged tissues. Subsequently, this regenerative deficiency due to insufficient progenitor cell-load would enable targeted cell therapy to augment and enhance the innate reparative mechanisms required to slow or reverse the disease course. This emerging theranostic approach would thus aim to develop stem cell platforms that can have both diagnostic and therapeutic purposes in disease management [13].
In summary, we show herein that circulating cells identified by the biomarker pair CXCR4+/FLK-1+ are present in humans, are increased in patients after myocardial infarction compared to control subjects, and are associated with improvement in left ventricular function as measured by 2D speckle-tracking echocardiography. Cell surface markers CXCR4+ and FLK-1+ may therefore select for circulating progenitors involved in cardiac regeneration following myocardial infarction. This initial study provides a foundation to advance the development of a novel theranostic platform that could improve prognostication in AMI patients and refine targeting of cell-based therapies to supplement underlying deficiencies in regenerative capacity. These findings warrant larger prognostic cohort studies to adjust for potential confounders of clinical outcome, to confirm the role of CD45−/CXCR4+/FLK-1+ cells in predicting cardiac regenerative capacity and to demonstrate that these cells can regenerate damaged myocardium in vivo.
References
Anversa, P., Kajstura, J., Leri, A., & Bolli, R. (2006). Life and death of cardiac stem cells: a paradigm shift in cardiac biology. Circulation, 113(11), 1451–1463. doi:10.1161/circulationaha.105.595181.
Bergmann, O., Bhardwaj, R. D., Bernard, S., Zdunek, S., Barnabe-Heider, F., Walsh, S., Zupicich, J., Alkass, K., Buchholz, B. A., Druid, H., Jovinge, S., & Frisen, J. (2009). Evidence for cardiomyocyte renewal in humans. Science, 324(5923), 98–102. doi:10.1126/science.1164680.
Kajstura, J., Rota, M., Cappetta, D., Ogorek, B., Arranto, C., Bai, Y., Ferreira-Martins, J., Signore, S., Sanada, F., Matsuda, A., Kostyla, J., Caballero, M. V., Fiorini, C., D’Alessandro, D. A., Michler, R. E., del Monte, F., Hosoda, T., Perrella, M. A., Leri, A., Buchholz, B. A., Loscalzo, J., & Anversa, P. (2012). Cardiomyogenesis in the aging and failing human heart. Circulation, 126(15), 1869–1881. doi:10.1161/circulationaha.112.118380.
Nelson, T. J., Behfar, A., Yamada, S., Martinez-Fernandez, A., & Terzic, A. (2009). Stem cell platforms for regenerative medicine. Clinical and Translational Science, 2(3), 222–227. doi:10.1111/j.1752-8062.2009.00096.x.
Bartunek, J., Vanderheyden, M., Vandekerckhove, B., Mansour, S., De Bruyne, B., De Bondt, P., Van Haute, I., Lootens, N., Heyndrickx, G., & Wijns, W. (2005). Intracoronary injection of CD133-positive enriched bone marrow progenitor cells promotes cardiac recovery after recent myocardial infarction: feasibility and safety. Circulation, 112(9 SUPPL.), I178–I183.
Janssens, S., Dubois, C., Bogaert, J., Theunissen, K., Deroose, C., Desmet, W., Kalantzi, M., Herbots, L., Sinnaeve, P., Dens, J., Maertens, J., Rademakers, F., Dymarkowski, S., Gheysens, O., Van Cleemput, J., Bormans, G., Nuyts, J., Belmans, A., Mortelmans, L., Boogaerts, M., & Van De Werf, F. (2006). Autologous bone marrow-derived stem-cell transfer in patients with ST-segment elevation myocardial infarction: double-blind, randomised controlled trial. The Lancet, 367(9505), 113–121.
Lunde, K., Solheim, S., Forfang, K., Arnesen, H., Brinch, L., Bjørnerheim, R., Ragnarsson, A., Egeland, T., Endresen, K., Ilebekk, A., Mangschau, A., & Aakhus, S. (2008). Anterior myocardial infarction with acute percutaneous coronary intervention and intracoronary injection of autologous mononuclear bone marrow cells. safety, clinical outcome, and serial changes in left ventricular function during 12-months’ follow-up. Journal of the American College of Cardiology, 51(6), 674–676.
Meyer, G. P., Wollert, K. C., Lotz, J., Steffens, J., Lippolt, P., Fichtner, S., Hecker, H., Schaefer, A., Arseniev, L., Hertenstein, B., Ganser, A., & Drexler, H. (2006). Intracoronary bone marrow cell transfer after myocardial infarction: eighteen months’ follow-up data from the randomized, controlled BOOST (Bone marrow transfer to enhance ST-elevation infarct regeneration) trial. Circulation, 113(10), 1287–1294.
Schächinger, V., Erbs, S., Elsässer, A., Haberbosch, W., Hambrecht, R., Hölschermann, H., Yu, J., Corti, R., Mathey, D. G., Hamm, C. W., Süselbeck, T., Werner, N., Haase, J., Neuzner, J., Germing, A., Mark, B., Assmus, B., Tonn, T., Dimmeler, S., & Zeiher, A. M. (2006). Improved clinical outcome after intracoronary administration of bone-marrow-derived progenitor cells in acute myocardial infarction: final 1-year results of the REPAIR-AMI trial. European Heart Journal, 27(23), 2775–2783.
Tendera, M., Wojakowski, W., Ruyłło, W., Chojnowska, L., Kpka, C., Tracz, W., Musiałek, P., Piwowarska, W., Nessler, J., Buszman, P., Grajek, S., Brborowicz, P., Majka, M., & Ratajczak, M. Z. (2009). Intracoronary infusion of bone marrow-derived selected CD34 + CXCR4+ cells and non-selected mononuclear cells in patients with acute STEMI and reduced left ventricular ejection fraction: results of randomized, multicentre myocardial regeneration by intracoronary infusion of selected population of stem cells in acute myocardial infarction (REGENT) trial. European Heart Journal, 30(11), 1313–1321.
Bartunek, J., Behfar, A., Dolatabadi, D., Vanderheyden, M., Ostojic, M., Dens, J., El Nakadi, B., Banovic, M., Beleslin, B., Vrolix, M., Legrand, V., Vrints, C., Vanoverschelde, J. L., Crespo-Diaz, R., Homsy, C., Tendera, M., Waldman, S., Wijns, W., & Terzic, A. (2013). Cardiopoietic stem cell therapy in heart failure: the C-CURE (Cardiopoietic stem Cell therapy in heart failURE) multicenter randomized trial with lineage-specified biologics. Journal of the American College of Cardiology, 61(23), 2329–2338. doi:10.1016/j.jacc.2013.02.071.
Rosenzweig, A. (2006). Cardiac cell therapy—mixed results from mixed cells. The New England Journal of Medicine, 355(12), 1274–1277.
Nelson, T. J., & Terzic, A. (2011). Induced pluripotent stem cells: an emerging theranostics platform. Clinical Pharmacology and Therapeutics, 89(5), 648–650.
Blau, H. M., Brazelton, T. R., & Weimann, J. M. (2001). The evolving concept of a stem cell: entity or function? Cell, 105(7), 829–841.
Wojakowski, W., Landmesser, U., Bachowski, R., Jadczyk, T., & Tendera, M. (2012). Mobilization of stem and progenitor cells in cardiovascular diseases. Leukemia, 26(1), 23–33. doi:10.1038/leu.2011.184.
Schmidt-Lucke, C., Fichtlscherer, S., Aicher, A., Tschope, C., Schultheiss, H. P., Zeiher, A. M., & Dimmeler, S. (2010). Quantification of circulating endothelial progenitor cells using the modified ISHAGE protocol. PLoS One, 5(11), e13790. doi:10.1371/journal.pone.0013790.
Wojakowski, W., Kucia, M., Kazmierski, M., Ratajczak, M. Z., & Tendera, M. (2008). Circulating progenitor cells in stable coronary heart disease and acute coronary syndromes: relevant reparatory mechanism? Heart, 94(1), 27–33. doi:10.1136/hrt.2006.103358.
Peichev, M., Naiyer, A. J., Pereira, D., Zhu, Z., Lane, W. J., Williams, M., Oz, M. C., Hicklin, D. J., Witte, L., Moore, M. A. S., & Rafii, S. (2000). Expression of VEGFR-2 and AC133 by circulating human CD34+ cells identifies a population of functional endothelial precursors. Blood, 95(3), 952–958.
Urbich, C., & Dimmeler, S. (2004). Endothelial progenitor cells: characterization and role in vascular biology. Circulation Research, 95(4), 343–353. doi:10.1161/01.res.0000137877.89448.78.
Massa, M., Rosti, V., Ferrario, M., Campanelli, R., Ramajoli, I., Rosso, R., De Ferrari, G. M., Ferlini, M., Goffredo, L., Bertoletti, A., Klersy, C., Pecci, A., Moratti, R., & Tavazzi, L. (2005). Increased circulating hematopoietic and endothelial progenitor cells in the early phase of acute myocardial infarction. Blood, 105(1), 199–206. doi:10.1182/blood-2004-05-1831.
Shintani, S., Murohara, T., Ikeda, H., Ueno, T., Honma, T., Katoh, A., Sasaki, K., Shimada, T., Oike, Y., & Imaizumi, T. (2001). Mobilization of endothelial progenitor cells in patients with acute myocardial infarction. Circulation, 103(23), 2776–2779.
Schmidt-Lucke, C., Rossig, L., Fichtlscherer, S., Vasa, M., Britten, M., Kamper, U., Dimmeler, S., & Zeiher, A. M. (2005). Reduced number of circulating endothelial progenitor cells predicts future cardiovascular events: proof of concept for the clinical importance of endogenous vascular repair. Circulation, 111(22), 2981–2987. doi:10.1161/circulationaha.104.504340.
Werner, N., Kosiol, S., Schiegl, T., Ahlers, P., Walenta, K., Link, A., Bohm, M., & Nickenig, G. (2005). Circulating endothelial progenitor cells and cardiovascular outcomes. The New England Journal of Medicine, 353(10), 999–1007. doi:10.1056/NEJMoa043814.
Quaini, F., Urbanek, K., Beltrami, A. P., Finato, N., Beltrami, C. A., Nadal-Ginard, B., Kajstura, J., Leri, A., & Anversa, P. (2002). Chimerism of the transplanted heart. The New England Journal of Medicine, 346(1), 5–15. doi:10.1056/NEJMoa012081.
Wojakowski, W., Tendera, M., Michalowska, A., Majka, M., Kucia, M., Maslankiewicz, K., Wyderka, R., Ochala, A., & Ratajczak, M. Z. (2004). Mobilization of CD34/CXCR4+, CD34/CD117+, c-met + stem cells, and mononuclear cells expressing early cardiac, muscle, and endothelial markers into peripheral blood in patients with acute myocardial infarction. Circulation, 110(20), 3213–3220. doi:10.1161/01.cir.0000147609.39780.02.
Kucia, M., Dawn, B., Hunt, G., Guo, Y., Wysoczynski, M., Majka, M., Ratajczak, J., Rezzoug, F., Ildstad, S., Bolli, R., & Ratajczak, M. (2004). Cells expressing early cardiac markers reside in the bone marrow and are mobilized into the peripheral blood after myocardial infarction. Circulation Research, 95(caf8c22e-7f28-fab8-2a7c-2477f9bdeb5d), 1191–1200. doi:10.1161/01.RES.0000150856.47324.5b.
Nelson, T. J., Faustino, R. S., Chiriac, A., Crespo-Diaz, R., Behfar, A., & Terzic, A. (2008). CXCR4+/FLK-1+ biomarkers select a cardiopoietic lineage from embryonic stem cells. Stem Cells, 26(6), 1464–1473.
Thygesen, K., Alpert, J. S., & White, H. D. (2007). Universal definition of myocardial infarction. Journal of the American College of Cardiology, 50(22), 2173–2195. doi:10.1016/j.jacc.2007.09.011.
Cheitlin, M. D., Armstrong, W. F., Aurigemma, G. P., Beller, G. A., Bierman, F. Z., Davis, J. L., Douglas, P. S., Faxon, D. P., Gillam, L. D., Kimball, T. R., Kussmaul, W. G., Pearlman, A. S., Philbrick, J. T., Rakowski, H., Thys, D. M., Antman, E. M., Smith, S. C., Jr., Alpert, J. S., Gregoratos, G., Anderson, J. L., Hiratzka, L. F., Hunt, S. A., Fuster, V., Jacobs, A. K., Gibbons, R. J., & Russell, R. O. (2003). ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Journal of the American Society of Echocardiography, 16(10), 1091–1110. doi:10.1016/s0894-7317(03)00685-0.
Leitman, M., Lysyansky, P., Sidenko, S., Shir, V., Peleg, E., Binenbaum, M., Kaluski, E., Krakover, R., & Vered, Z. (2004). Two-dimensional strain-a novel software for real-time quantitative echocardiographic assessment of myocardial function. Journal of the American Society of Echocardiography, 17(10), 1021–1029. doi:10.1016/j.echo.2004.06.019.
Mor-Avi, V., Lang, R. M., Badano, L. P., Belohlavek, M., Cardim, N. M., Derumeaux, G., Galderisi, M., Marwick, T., Nagueh, S. F., Sengupta, P. P., Sicari, R., Smiseth, O. A., Smulevitz, B., Takeuchi, M., Thomas, J. D., Vannan, M., Voigt, J. U., & Zamorano, J. L. (2011). Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. Journal of the American Society of Echocardiography, 24(3), 277–313. doi:10.1016/j.echo.2011.01.015.
Korinek, J., Wang, J., Sengupta, P. P., Miyazaki, C., Kjaergaard, J., McMahon, E., Abraham, T. P., & Belohlavek, M. (2005). Two-dimensional strain—a Doppler-independent ultrasound method for quantitation of regional deformation: validation in vitro and in vivo. Journal of the American Society of Echocardiography, 18(12), 1247–1253. doi:10.1016/j.echo.2005.03.024.
Pirat, B., Khoury, D. S., Hartley, C. J., Tiller, L., Rao, L., Schulz, D. G., Nagueh, S. F., & Zoghbi, W. A. (2008). A novel feature-tracking echocardiographic method for the quantitation of regional myocardial function: validation in an animal model of ischemia–reperfusion. Journal of the American College of Cardiology, 51(6), 651–659. doi:10.1016/j.jacc.2007.10.029.
Reant, P., Labrousse, L., Lafitte, S., Bordachar, P., Pillois, X., Tariosse, L., Bonoron-Adele, S., Padois, P., Deville, C., Roudaut, R., & Dos Santos, P. (2008). Experimental validation of circumferential, longitudinal, and radial 2-dimensional strain during dobutamine stress echocardiography in ischemic conditions. Journal of the American College of Cardiology, 51(2), 149–157. doi:10.1016/j.jacc.2007.07.088.
Fine, N. M., Shah, A. A., Han, I. Y., Yu, Y., Hsiao, J. F., Koshino, Y., Saleh, H. K., Miller, F. A., Jr., Oh, J. K., Pellikka, P. A., & Villarraga, H. R. (2013). Left and right ventricular strain and strain rate measurement in normal adults using velocity vector imaging: an assessment of reference values and intersystem agreement. The International Journal of Cardiovascular Imaging, 29(3), 571–580. doi:10.1007/s10554-012-0120-7.
Asanuma, T., Uranishi, A., Masuda, K., Ishikura, F., Beppu, S., & Nakatani, S. (2009). Assessment of myocardial ischemic memory using persistence of post-systolic thickening after recovery from ischemia. JACC. Cardiovascular Imaging, 2(11), 1253–1261. doi:10.1016/j.jcmg.2009.07.008.
Okuda, K., Asanuma, T., Hirano, T., Masuda, K., Otani, K., Ishikura, F., & Beppu, S. (2006). Impact of the coronary flow reduction at rest on myocardial perfusion and functional indices derived from myocardial contrast and strain echocardiography. Journal of the American Society of Echocardiography, 19(6), 781–787. doi:10.1016/j.echo.2005.10.016.
Pislaru, C., Belohlavek, M., Bae, R. Y., Abraham, T. P., Greenleaf, J. F., & Seward, J. B. (2001). Regional asynchrony during acute myocardial ischemia quantified by ultrasound strain rate imaging. Journal of the American College of Cardiology, 37(4), 1141–1148.
Voigt, J. U., Exner, B., Schmiedehausen, K., Huchzermeyer, C., Reulbach, U., Nixdorff, U., Platsch, G., Kuwert, T., Daniel, W. G., & Flachskampf, F. A. (2003). Strain-rate imaging during dobutamine stress echocardiography provides objective evidence of inducible ischemia. Circulation, 107(16), 2120–2126. doi:10.1161/01.cir.0000065249.69988.aa.
Hernandez, P. A., Gorlin, R. J., Lukens, J. N., Taniuchi, S., Bohinjec, J., Francois, F., Klotman, M. E., & Diaz, G. A. (2003). Mutations in the chemokine receptor gene CXCR4 are associated with WHIM syndrome, a combined immunodeficiency disease. Nature Genetics, 34(1), 70–74. doi:10.1038/ng1149.
Ratajczak, M. Z., Zuba-Surma, E., Kucia, M., Reca, R., Wojakowski, W., & Ratajczak, J. (2006). The pleiotropic effects of the SDF-1-CXCR4 axis in organogenesis, regeneration and tumorigenesis. Leukemia, 20(11), 1915–1924. doi:10.1038/sj.leu.2404357.
Abbott, J. D., Huang, Y., Liu, D., Hickey, R., Krause, D. S., & Giordano, F. J. (2004). Stromal cell-derived factor-1alpha plays a critical role in stem cell recruitment to the heart after myocardial infarction but is not sufficient to induce homing in the absence of injury. Circulation, 110(21), 3300–3305. doi:10.1161/01.cir.0000147780.30124.cf.
Chiriac, A., Terzic, A., Park, S., Ikeda, Y., Faustino, R., & Nelson, T. J. (2010). SDF-1-enhanced cardiogenesis requires CXCR4 induction in pluripotent stem cells. Journal of Cardiovascular Translational Research, 3(6), 674–682. doi:10.1007/s12265-010-9219-1.
Vasa, M., Fichtlscherer, S., Aicher, A., Adler, K., Urbich, C., Martin, H., Zeiher, A. M., & Dimmeler, S. (2001). Number and migratory activity of circulating endothelial progenitor cells inversely correlate with risk factors for coronary artery disease. Circulation Research, 89(1), E1–E7.
Hill, J. M., Zalos, G., Halcox, J. P., Schenke, W. H., Waclawiw, M. A., Quyyumi, A. A., & Finkel, T. (2003). Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. The New England Journal of Medicine, 348(7), 593–600. doi:10.1056/NEJMoa022287.
Kalogeropoulos, A. P., Georgiopoulou, V. V., Gheorghiade, M., & Butler, J. (2012). Echocardiographic evaluation of left ventricular structure and function: new modalities and potential applications in clinical trials. Journal of Cardiac Failure, 18(2), 159–172. doi:10.1016/j.cardfail.2011.10.019.
Asanuma, T., Fukuta, Y., Masuda, K., Hioki, A., Iwasaki, M., & Nakatani, S. (2012). Assessment of myocardial ischemic memory using speckle tracking echocardiography. JACC. Cardiovascular Imaging, 5(1), 1–11. doi:10.1016/j.jcmg.2011.09.019.
Belohlavek, M. (2012). Post-systolic shortening: a functional window into ischemic memory? JACC. Cardiovascular Imaging, 5(1), 12–14. doi:10.1016/j.jcmg.2011.09.014.
Triller Vrtovec, K., & Vrtovec, B. (2013). Patent eligibility of induced pluripotent stem cell theranostics. Clinical Pharmacology and Therapeutics. doi:10.1038/clpt.2013.11.
Acknowledgments
We gratefully acknowledge the technical contributions of Jay Hiddinga, Ph.D. and Lisa Nesbitt.
Funding
This work was supported in part by the Todd and Karen Wanek Program for Hypoplastic Left Heart Syndrome, Marriott Regenerative Medicine Award, and Mayo Clinic. It was also supported by CTSA Grant Number UL1 TR000135 and TL1 TR000137 from the National Center for Advancing Translational Science (NCATS).
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Lorrie Kirshenbaum oversaw the review of this article.
Rahul Suresh and Anca Chiriac are co-first authors.
Rights and permissions
About this article
Cite this article
Suresh, R., Chiriac, A., Goel, K. et al. CXCR4+ and FLK-1+ Identify Circulating Cells Associated with Improved Cardiac Function in Patients Following Myocardial Infarction. J. of Cardiovasc. Trans. Res. 6, 787–797 (2013). https://doi.org/10.1007/s12265-013-9502-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-013-9502-z