Abstract
Comprehensive diagnostic criteria, accurate prognostic indicators, and effective treatment for patients with heart failure and a preserved ejection fraction (HFpEF) represent a critically important unmet need in cardiovascular medicine. Novel approaches to fill this unmet need are likely to be facilitated by targeting the underlying and unique pathophysiologic mechanisms that characterize patients with HFpEF. Two possible targets include hemodynamic overload evidenced by increased LV diastolic pressure (LVDP) and myocardial fibrosis evidenced by increased extracellular matrix fibrillar collagen. The measurement of LVDP and fibrosis generally requires either invasive procedures and/or complex and sophisticated imaging techniques. However, biomarkers measured in the plasma have been shown to accurately reflect changes in hemodynamic load and myocardial fibrosis and may have important application to the management of patients with HFpEF. The purpose of this review is to describe current and future applications of biomarkers in the management of patients with HFpEF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Diagnosis, Prognosis, and Management of HFpEF: Critical Unmet Needs
Diagnostic Criteria
Patients with heart failure (HF) can be divided into those with heart failure and a reduced ejection fraction (HFrEF) and those with heart failure and a preserved ejection fraction (HFpEF). Criteria necessary to make the diagnosis of HFpEF have been proposed both by the Heart Failure Society of America and the European Society of Cardiology. These criteria include symptoms and signs of heart failure, normal left ventricular (LV) volume, preserved EF (usually >50 %), evidence of diastolic dysfunction, and the absence of any non-cardiac cause for symptoms and signs. The use of these criteria has not been universally implemented, consensus on their use is incomplete, and their specificity has not been confirmed. Thus, the establishment of diagnostic criteria remains an unmet need. As described below, biomarkers that indicate the presence of diastolic dysfunction may help to facilitate and enhance the specificity and utility of these diagnostic criteria in HFpEF.
Prognosis
The prevalence of HFpEF (>50 % of all HF patients) continues to increase [1]; prognosis remains grim. HFpEF patients have a devastating 5-year mortality rate (approaching 60 %), costly morbidity (50 %, 6-month hospitalization rate), and debilitating symptoms (maximum myocardial oxygen consumption, MVO2, averaging 14 ml/gm/min) [1–5]. Predictors of morbid and mortal outcomes in HFpEF remain incompletely defined. Clinical, structural, and functional indices have been proposed. When present, LV remodeling and diastolic dysfunction portend poor outcomes. However, the frequency distribution of these finding varies in HFpEF populations, and these finding also occur in patients with antecedent or comorbid conditions such as hypertension, diabetes, and advanced age. Thus, the development of prognostic indices with necessary specificity remains an unmet need; biomarkers may help to fill this need.
Management
To date, standard HF therapy shown to be effective in HFrEF has not been shown to reduce morbidity or mortality in HFpEF patients [17–21]. In fact, recent HF guidelines have concluded that “no treatment has yet been shown, convincingly, to reduce morbidity or mortality in patients with HFpEF” [22]. Therefore, current treatment remains empiric, targets antecedent and comorbid diseases, and prevention and reduction of volume overload. This review explores possible novel developmental directions in the management of HFpEF which are based on biomarker directed selection of patient populations and guided management approaches.
Pathophysiology: Targets for Novel Therapeutic Strategies
As described above, comprehensive diagnostic criteria, accurate prognostic indicators, and effective treatment of HFpEF represent a singularly important unmet need in cardiovascular medicine. Novel approaches to fill this unmet need are likely to be facilitated by targeting the underlying and unique pathophysiologic mechanisms that characterize patients with HFpEF. While there are some features of the clinical HF syndrome that are shared by all HF patients regardless of ejection fraction (EF), there are clear and specific differences in cardiovascular structure and function between HFpEF and HFrEF [6–16]. The pathophysiological mechanisms that cause the development of HFpEF are reflected in changes in LV relaxation and filling, LV structural remodeling and geometry, and changes in LV and vascular compliance. Patients with HFpEF have normal LV end-diastolic volume, normal (or near normal) EF and chamber systolic properties, commonly have concentric remodeling of either the LV chamber or cardiomyocytes, decreased LV diastolic distensibility, and diffuse myocardial fibrosis [6–16]. While each of these mechanisms are important and contribute to the development of HFpEF, two consensus targets include hemodynamic overload evidenced by increased LV diastolic pressure (LVDP) and myocardial fibrosis evidenced by increased extracellular matrix (ECM) fibrillar collagen. The measurement of LVDP and fibrosis generally requires either invasive procedures and/or complex and sophisticated imaging techniques. However, biomarkers measured in the plasma have been shown to accurately reflect changes in hemodynamic load and myocardial fibrosis and may have important application to the management of patients with HFpEF.
Biomarkers in HFpEF that Reflect Pathophysiology
Biomarkers include proteins, peptides, and microRNAs that can be measured in the plasma and can be shown to represent changes in myocardial structure or function that reflect underlying pathophysiologic processes [23]. In this article, biomarkers that reflect changes in hemodynamic load and fibrosis in patients with HFpEF will be reviewed.
Hemodynamic Load
LVDP can be directly measured by cardiac catheterization. LVDP can be non-invasively estimated using echocardiographic, Doppler and Tissue Doppler echocardiographic methods, measurements of blood volume, and thoracic impedance. Neither these direct or indirect methods are easily applicable across a wide spectrum of clinical care, particularly in the outpatient setting, nor is their frequency of measurement currently sufficient to manage the rapidly changing hemodynamic status of HFpEF patients. However, plasma biomarkers such as the natriuretic peptides reflect hemodynamic load and can be measured relatively inexpensively, repetitively, and both in a point of care setting and at home setting [24]. Evidence to support this application and its utility in the management of HFpEF will be one purpose of this review article.
Myocardial Fibrosis
Myocardial fibrosis can be directly quantitated by myocardial biopsy and assessment of collagen volume fraction. Diffuse myocardial fibrosis can be non-invasively assessed using MRI late gadolinium enhancement and T1 mapping [25]. However, like the methods used to measure LVDP, these invasive and non-invasive methods have significant limitations. Fortunately, plasma biomarkers have been identified that reflect changes in collagen homeostatic mechanism responsible for fibrosis and the presence and extent of myocardial fibrosis. For example, matrix metalloproteinases (MMP), tissue inhibitors of MMPs (TIMPs), and collagen processing proteins collagen propeptides and collagen telopeptides reflect changes in collagen homeostasis and the transition from antecedent diseases like hypertension to clinically symptomatic HFpEF [26, 27]. Galectin-3 and ST-2 reflect the general extent of fibrosis and the severity of HFpEF [28–34]. Evidence to support this biomarker application and its utility in the management of HFpEF will be a second purpose of this review article.
Change in Biomarkers versus Diastolic Pressure-Volume Relationship
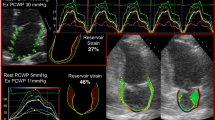
These two sets of biomarkers may have both independent and interdependent value in HFpEF. That is, because they reflect different but related aspects of the pathophysiology of HFpEF, they may be used separately or in combination. For example, myocardial fibrosis results in an overall shift in the position and slope of the diastolic pressure-volume curve indicating an overall increase in LV chamber stiffness (Fig. 1). Changes in chamber stiffness occur over a longer time period and should be detected by changes in biomarkers that reflect fibrosis. By contrast, changes in volume status may change the instantaneous operating stiffness (end diastolic pressure-volume ratio) along a given pressure-volume relationship (Fig. 1). Changes in operative stiffness occur over a shorter time period and will likely be reflected by changes in biomarkers that reflect LVDP. Finally, these factors may be interdependent; an increase in fibrosis will result in an increase in vulnerability to develop increased operative stiffness.
Changes in plasma biomarkers may reflect changes in the left ventricular (LV) diastolic pressure versus volume relationship (DPVR). Solid line represents a normal DPVR; dashed line represents the DPVR in patients with heart failure with a preserved ejection fraction (HFpEF). One mechanism that results in an increase in LV diastolic stiffness and a shift upwards and to the left of the DPVR is the development of fibrosis. Biomarkers such as Galectin 3 (Gal-3) may be reflective of this process. A change in hemodynamic load can result in an increase in the instantaneous operative stiffness and shift the diastolic pressure versus volume coordinants to a steeper portion of the DPVR. Biomarkers such as brain natriuretic peptide (BNP) may be reflective of this process. Adapted from Zile et al. [13]
Natriuretic Peptides: Use in Assessment of Hemodynamic Overload
The best characterized biomarkers in patients with HFpEF are the natriuretic peptides: B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP) [35–45]. Circulating levels of these proteins are elevated in patients with HFpEF as compared to subjects without HF, but are lower than levels seen in patients with HFrEF. In patients with HFpEF, increased BNP is directly related to increased LV diastolic filling pressure and end diastolic wall stress [46]. As shown in Fig. 2, there is a direct linear relationship between BNP and LVDP; the relationship is even more robust between BNP and LV diastolic wall stress. In addition, BNP and NT-proBNP fall when LVDP decreases in response to volume reduction. Therefore, natriuretic peptide levels are an accurate reflection of ambient LVDP.
Direct relationship between left ventricular end diastolic pressure (EDP) or end diastolic wall stress (EDWS) and brain natriuretic peptide (BNP) for all heart failure (HF) patients and patients with heart failure with a preserved ejection fraction (EF). From Iwanaga et al. [46]
Because HFpEF patients have a smaller LV cavity and thicker LV walls, their end diastolic wall stress is much lower than in HFrEF, even in the setting of high diastolic pressures, thus, producing a lower stimulus for BNP production. On average, HFpEF patients presenting with acute decompensated heart failure (ADHF) have a BNP value of 100–500 pg/ml vs. HFrEF patients with 500–1,500 pg/ml.
In addition, other factors, independent of LVDP and diastolic stress also affect BNP levels in HFpEF patients. For any given LVDP in HFpEF patients, BNP levels are lower in obese patients and higher in women, older patients, and patients with concomitant pulmonary disease (chronic obstructive disease, pulmonary hypertension, pulmonary embolus) and renal dysfunction. For example, expected values on BNP in obese patients with decompensated HFpEF with a body mass index > 35 Kg/m [2] will be significantly lower than the values mentioned above and may be close to the upper normal partition value. Because patients with heart failure have significant co-morbidities (including those that affect the right ventricle) HFpEF patients with pulmonary hypertension may have elevated BNP levels even when they are compensated. There is significant daily variability in BNP levels in otherwise stable patients which makes the determination of what constitutes a significant increase or decrease more challenging; however, recent advances in modeling of serial measurements is likely to address this challenge [40].
Thus, within the limitations described above, natriuretic peptide levels should have practical application to diagnostic, prognostic and management issues in HFpEF.
Natriuretic Peptides: Use in Diagnosis and Prognosis
Natriuretic Peptides as Diagnostic Criteria
The diagnostic criteria specified in current HF guidelines for HFpEF includes invasive or non-invasive assessment of LVDP such as an increased LA volume index > 40 ml/m [2], LVEDP > 16 mmHg, and PCWP >15 mmHg [22]. This requirement is based on epidemiologic studies, randomized clinical trials and mechanistic studies demonstrating significant abnormalities in diastolic function in patients with HFpEF. In addition, studies using implantable hemodynamic monitors (IHM) in patients with HFpEF have demonstrated that LVDP is increased even when HFpEF patients are considered compensated; LVDP further increases significantly when HFpEF patients make the transition to ADHF [47].
Like LVDP, BNP and NT-proBNP have become critical components of the diagnostic criteria for HFpEF proposed in HF guidelines [22]. In addition, BNP and NT-proBNP have become essential inclusion criteria in RCTs in HFpEF. The standard partition values for diagnostic criteria of BNP = 100 pg/ml and NT-proBNP =800 pg/ml have been suggested to support the diagnosis of HFpEF [22].
Natriuretic Peptides Predict Prognosis
Recent studies showed that both baseline LVDP and change in LVDP from baseline predict future HF events (Fig. 3) [47, 48]. Like LVDP, baseline values of NT-proBNP and change in NT-proBNP from baseline have prognostic value in patients with HFpEF (Fig. 4) [44, 45]. Thus, there are similar predictive patterns using LVDP and natriuretic peptides.Furthermore, in the Champion trial (CardioMEMS Heart Sensor Allows Monitoring of Pressure to Improve Outcomes in NYHA Class III Heart Failure Patients) management of HFpEF based on knowledge of LVDP resulted in a 152 % decrease in pressures and a 52 % decrease in HF events (both p < 0.001 vs. control) (Fig. 5) [49]. These data justify LVDP as practical therapeutic target. Thus, LVDP represents an important diagnostic and prognostic index and may be useful in developing novel management strategies in HFpEF. There is a remarkable parallel between these applications of LVDP to HFpEF and application of natriuretic peptides to HFpEF.
a Patients with heart failure and a preserved ejection fraction (HFpEF) have increased LV diastolic pressure (indexed here as estimated pulmonary artery diastolic pressure, ePAD) when considered compensated by their physician and have further increases in pressure when they develop acute decompensated heart failure requiring hospital admission (from Zile et al. [47]). b Both baseline LV diastolic filling pressure and changes in filling pressure are sensitive predictors of future ADHF events (from Stevenson et al. [48])
a Baseline values of NT-Pro BNP have significant prognostic value and predict morbid and mortal outcomes. The higher the baseline value of nt-proBNP, the higher endpoint rate of the primary and heart failure endpoint in the I-Preserve study (From: McKelvie et al. [44]). b Change form baseline values of NT-Pro BNP have significant prognostic value and predict morbid and mortal outcomes. Data from the I-Preserve study indicated that the directional change in NT-proBNP predicted primary and heart failure outcome rates (From Jhund et al. [45])
Results of the CHAMPION trial demonstrating a reduction in cumulative hospital admissions and increase in freedom from heart failure (HF) hospitalizations or all-cause mortality in HF with a reduced ejection fraction (HFrEF) and HF preserved EF (HFpEF) patients. From Abraham et al. [49]
Natriuretic Peptides: Use in Guided Management
Beyond their diagnostic and prognostic capabilities, tailoring therapy based on BNP values may also be efficacious. Three recent studies Habit, Protect and Battlescarred suggested that BNP or NT-proBNP measured in an outpatient setting (every 1–3 months) or measured daily at home was both feasible and efficacious in guiding treatment in patients across an EF spectrum [40, 41, 43]. In these studies, increased values of BNP were treated by augmenting diuresis and lowering LVDP. For example, Protect was an investigator initiated, prospective randomized study in HF patients with an EF ≤ 40 % (mean 28 ± 9 %) [42]. Total CV events were lower and time to first CV event was longer in patients in whom NT-proBNP was used to guide treatment compared with patients in the standard of care group in whom NT-proBNP was not used to guide treatment. In Habit I (Heart failure assessment with BNP in the home) patients with an EF median 30 % and IQR 20-45 %, daily home BNP testing was feasible and changes in BNP corresponded to significant changes in risk of CV event [40]. These concepts will be further tested in HABIT II in which management using BNP in patients across an EF spectrum will determine whether a strategy to lower baseline BNP < 200 pg/ml or lowest level attainable and/or prevent or respond to rise in BNP on CV events will be tested.
Natriuretic Peptides as Targets of Therapy
Natriuretic peptide levels themselves may also serve as a target for therapy in patients with HFpEF. Natriuretic peptide levels could be increased either by preventing their degradation by neutral endopeptidases (such as in the Paramount Study) or by using IV or SC infusion of BNP itself (such as in the Chronic Administration of Subcutaneous Brain Natriuretic Peptide [SQ BNP] on the Left Ventricular, Renal and Humoral Function and on the Integrated Response to Acute Sodium Loading study, nct 00405548) [50–53]. This review will focus on the Paramount study: Prospective comparison of ARNI vs. ARB on Management of Heart Failure with Preserved Ejection Fraction. PARAMOUNT was a phase 2, randomized, parallel-group, double-blind multicenter trial in patients with NYHA class II-III HFpEF (EF > 45 %), and NT-proBNP > 400 pg/mL [50]. 149 patients were assigned to LCZ696 (an angiotensin receptor and neprilysin inhibitor, 200 mg BID) or 152 patients to valsartan (160 mg BID) for 36 weeks. The primary endpoint was change in NT-proBNP from baseline to 12 weeks. At 12 weeks LCZ696 significantly reduced NT-proBNP by ∼15 % compared with valsartan (p = 0.005). At 36 weeks LCZ696 significantly reduced LA volume by ∼5 % compared with valsartan (p = 0.003). LCZ improved NHYA class vs. valsartan (p = 0.05). LCZ696 was well tolerated with adverse effects similar to those of valsartan. Whether these effects would translate into improved outcomes will be tested in a large randomized trial (PARAGON-HF).
Biomarkers Reflecting Collagen Homeostasis: Use in Assessment of Myocardial Fibrosis
Role of ECM in Progression from PO to HFpEF- Animal Models
The most common antecedent and co-morbid disease processes that lead to the development of HFpEF include pressure-overload (PO) conditions such as hypertension and aortic stenosis. While other metabolic conditions such as diabetes can contribute to the development of HFpEF, PO will be the primary focus in this review. Despite significant advances in diagnosis and management, PO remains one of the most important risk factors for the development of CV disease and a leading cause of CV morbidity and mortality. PO results in significant changes in LV structure and function, collectively termed myocardial remodeling [8]. This remodeling includes significant changes in cardiomyocytes, fibroblasts and the extracellular matrix (ECM), all of which contribute to structural remodeling and diastolic dysfunction of PO. Initially, PO leads to the development of LV chamber hypertrophy (LVH) [53, 54]. Once established, PO-induced LVH has significant long term consequences because it serves as a major independent risk factor for the development of myocardial fibrosis and HF, particularly HFpEF. Animal models of PO that reflect important elements of clinical HFpEF have shown that this remodeling process follows a temporal pattern [53, 54]. Initially, in response to a PO stimulus, rapid and progressive cardiomyocyte hypertrophy occurs during a period of relative compensation. During this initial phase, ECM fibrillar collagen is not significantly increased and diastolic function particularly diastolic distensibility remains normal. Once the level of hypertrophy reaches a steady state increase, ECM fibrillar collagen accumulation occurs together with the development of diastolic dysfunction, decreased distensibility, and decompensation. These pathophysiologic processes defined in animal models have relevance to the structural, functional and clinical progression that occurs in hypertensive heart disease (HHD).
Role of ECM in Progression from PO to HFpEF- Clinical HHD
Patients with hypertension can be categorized into 3 staged groups: 1) those with hypertension but no structural remodeling, 2) those with hypertension and structural remodeling (such as LVH) but no significant diastolic dysfunction and no HFpEF and 3) those with hypertension, LVH, diastolic dysfunction and HFpEF [55]. In this second phase of HHD there is little or no significant increases in ECM collagen content. The transition to the third phase HFpEF in HHD is associated with if not caused by a change in collagen homeostasis that leads to fibrosis. Once fibrosis develops in patients with PO, mortality and morbidity significantly increase. For example, studies using MRI technology to evaluate diffuse fibrosis in patients with aortic stenosis have shown that 5 year mortality is predicted by the extent of myocardial fibrosis present [25]. Therefore, identifying patients in each of the 3 stages of HHD described above, differentiating those with and without structural remodeling, diastolic dysfunction and HFpEF, and assessing ECM collagen processes represent an important and novel target for development of diagnostic, prognostic and therapeutic strategies in patients with HFpEF and the antecedent PO conditions that lead to HFpEF. There are a number of proteins, peptides and microRNAs that have been shown to reflect collagen homeostasis that hold promise as biomarkers that can play important roles in these novel strategies [55–59]. The role that these biomarkers play in collagen homeostasis are described below.
Collagen Composition
Myocardial fibrillar collagen is primarily composed of collagen I and III. Changes in collagen I may make the larger contribution to diastolic dysfunction and HFpEF because it has the higher stiffness properties, occurs in higher proportion and increases in response to PO. The regulatory control mechanisms are similar for both collagen I and III, therefore they will be considered together, but biomarkers specific to each will also be discussed. Fibrillar collagen content results from the balance in the following processes: procollagen synthesis, postsynthetic procollagen processing, post-translational collagen cross-linking and collagen degradation (Fig. 6A).
Collagen Synthesis
Collagen is synthesized as a procollagen molecule primarily in myocardial fibroblast (Fig. 6B). Procollagen is secreted into the ECM space where it must undergo a series of ordered sequential post-synthetic processing steps that are sensitive to both temporal and spatial parameters that create a mature cross-linked insoluble collagen fibril [60–62]. Procollagen is secreted as a soluble molecule with an NH2- (N) and a COOH (C)-terminal propeptide attached. Removal of these propeptides is the first of a number of essential steps that lead to efficient incorporation of soluble collagen into insoluble collagen fibrils.
Collagen Processing
First, enzymatic cleavage of the C-terminal propeptide by bone morphogenic protein-1 (BMP) 1 (enhanced by procollagen C-proteinase enhancer) is required [62]. The rate of release of the C-terminal propeptide and its concentration in plasma as PICP (procollagen I C-terminal propeptide) and PIIICP (procollagen I C-terminal propeptide) reflect collagen synthesis. Second, enzymatic cleavage of the N-terminal propeptide by ADAMTS-2/3 (A Disintegrin-like and Metalloproteinase Domain with Thrombospondin Type Motif) is required. The rate of release of the N-terminal propeptide and its concentration in plasma as PINP (procollagen I N-terminal propeptide) and PIIINP (procollagen I N-terminal propeptide) reflect collagen synthesis.
Collagen Fibril Assembly
After the C and N terminal propeptides are cleaved, the resulting collagen molecules undergo covalent cross-link formation to form insoluble fibrils. The cross-links are formed spontaneously by oxidized reactive aldehydes on lysine and hydroxylysine catalyzed by the enzymes lysyl oxidase and hydroxylysyl oxidase. After this initial cross-linking, additional non-enzymatic cross-links can be formed by advanced glycation end product (AGE) formation. Increase AGE induced cross-links have been shown to result from PO. Signaling by AGEs through the receptor for AGEs (RAGE) has been shown to result in profibrotic pathway activation. Soluble RAGE (sRAGE), and AGE modified albumin can be measured in the plasma.
Matricellular Proteins
The spatial and temporal organization of procollagen processing in the extracellular space is critical for efficient and effective incorporation of insoluble collagen. A number of matricellular proteins such as SPARC, thrombospondin, osteopontin, and others are critical in the regulation of procollagen processing by facilitating fibril assembly, formation, and collagen deposition to insoluble ECM. Each of these matricellular proteins can be measured in the plasma.
Collagen Degradation
Insoluble collagen fibrils in the ECM undergo degradation into collagen telopeptides. Plasma concentrations of collagen telopeptides such as CITP (collagen I telopeptide) reflect the rates of collagen degradation and the ratio of propeptides to telopeptides reflect collagen turn-over rate. Degradation is caused by proteases such as MMPs. There are now approximately 23 MMP types expressed within humans, and the distribution, functionality, and substrates are diverse as discussed in several broader reviews [26, 27]. Initially, the MMPs were classified based upon recognized substrates, and while this nomenclature no longer holds relevance, it is still commonly used to group the MMP types. This classification scheme would include the Collagenases, such as MMP-1, MMP-13, and MMP-8; the Gelatinases which would include MMP-2 and MMP-9; the Stromelysins/Matrilysins which would include MMP-3 and MMP-7; and the Membrane Type MMPs which would include MMP-14. MMPs are in turn regulated by TIMPs. Each MMP and TIMP have multiple mechanisms of action and targets for activity. While in general it is true that some MMPs under specific circumstances primarily act to degrade fibrillar collagen, MMPs may also act on bioactive molecules within the ECM that result in profibrotic pathways to be activated. In general, TIMPs bind to active MMPs and inactivate their protease activity and lead to a reduction in collagen degradation. In addition, however, TIMPs may act on other bioactive molecules and effect myocardial growth, fibroblast proliferation, and activity. TIMPs increase fibroblast growth factors and stimulate profibrotic signaling cascades and contribute to fibrosis. MMPs and TIMPs can be measured in the plasma and have been shown to change significantly during the development of HHD.
Biomarkers that Reflect Collagen Homeostasis
Each of the proteins and peptides described above can be measured in the plasma and can be used as biomarkers to assess collagen synthesis, processing, and degradation rates. Myocardial collagen content, composition, and geometry are the result of the balance between these homeostatic mechanisms. For example, if collagen synthesis and collagen processing are increased (as evidenced by an increase in PICP and SPARC) but collagen degradation is also increased (as evidenced by an increase in CITP and MMP-13), there may be no net change in total collagen content. In patients with HFpEF, collagen synthesis, processing, and cross-linking have been shown to be increased, while collagen degradation is decreased resulting in a net increase in collagen content and fibrosis. Some but not all of the potential biomarkers described above have been tested and been found to be useful in HFpEF patients. These data are summarized in Table 1 and discussed below in the context of HHD. Clearly further studies are necessary.
Biomarkers that Reflect Collagen Content and Fibrosis
There are additional biomarkers such as galectin-3 and ST-2 which may reflect the degree and reversibility of fibrosis [28–34]. Galectin-3 is a beta-galactoside-binding lectin, secreted by macrophages, that may act to increase fibroblast proliferation, activity, and transformation into myofibroblast. In so doing, Gal-3 may promote a profibrotic fibroblast phenotype, increase collagen synthesis, and enable aldosterone signaling. ST2 is a member of the interleukin 1 receptor family; ST2 exists in both membrane bound and soluble forms. The functional ligand of ST2 is interleukin 33 (IL-33), a cardiac fibroblast protein. Binding of IL-33 to membrane ST2 produced by increased myocardial biomechanical elicits an antihypertrophic and antifibrotic response. This cardioprotective effect is negated by soluble ST2 which acts as a decoy, prevents binding of IL-33 to membrane-bound ST2.
Therefore, based on the information described above, these plasma biomarkers that reflect collagen homeostasis and the degree of fibrosis should be useful in defining the degree of remodeling in HHD, augmenting diagnostic criteria for HFpEF, providing prognostic information in HFpEF, and enhancing ability to develop tailored treatment in HFpEF (Table 1).
Biomarkers Reflecting Collagen Homeostasis: Use in Diagnosis and Prognosis
Biomarkers Reflect Antecedent Structural Remodeling
HF guidelines emphasize the fact that hypertension treatments aimed to prevent, identify, and regress LVH in patients with HFpEF are the only recommendations that have “level of evidence A” [22]. Therefore, it is important to be able to identify the presence of structural remodeling such as LVH and to be able to identify and/or predict the progression from LVH to HFpEF. The plasma biomarkers discussed below represent those that reflect changes in the collagen homeostasis and for which there is evolving evidence that they can in fact provide this diagnostic and prognostic information in LVH and HFpEF. While each biomarker can be considered as a single entity, data suggest that the predictive accuracy is significantly increased when these biomarkers are used together in a multi-biomarker panel. Data to support this approach with these biomarkers are described below.
While LVH is a pivotal step in the development of PO-induced heart disease, the detection of LVH is made difficult by several factors. First, in and of itself, the clinical disease processes causing PO do not cause symptoms; consequently, LV remodeling may remain an unrecognized and insidious process for a prolonged period of time. Second, LVH is not readily detectable using standard clinical means such as a history, physical exam or ECG, but rather requires costly, specialized testing approaches, and subspecialty expertise to perform and interpret. Therefore, a plasma biomarker profile was developed which could be utilized to identify patients with LVH and therefore identify patients with HHD at highest risk to develop HFpEF. Seventeen biomarkers (matrix metalloproteinase [MMP]-1, -2, -3, -7, -8, and -9; tissue inhibitors of MMPs [TIMPs] -1, -2, -3, and −4; N-terminal propeptide of brain natriuretic peptide (NT-proBNP); cardiotrophin; osteopontin; soluble receptor for advanced glycation end products; collagen I telopeptide; collagen I NT-proBNP; and collagen III N-terminal propeptide [PIIINP]) were examined. From these, a multi-biomarker panel which included MMP-7, MMP-9, TIMP-1, PIIINP, and NT-proBNP provided a robust prediction algorithm for LVH (AUC = 0.80) [55]. Each of these biomarkers was increased in patients with hypertension and LVH but no HFpEF compared with patients with hypertension with no LVH. These changes in collagen homeostasis likely represent an increase in collagen turnover during the hypertrophy process.
Biomarkers Indicating the Diagnosis of HFpEF
There is a substantial rate of progression from PO-induced LVH to abnormal diastolic function and HFpEF. Myocardial remodeling, particularly changes in the structure and composition of the ECM, results in abnormal LV filling, a stiff noncompliant left ventricle, and increased diastolic pressures. However, identification of patients with LVH who have developed this form of HFpEF is difficult, requires extensive non-invasive and/or invasive testing, and complex algorithmic diagnostic criteria. Therefore, a plasma biomarker profile was developed which could be utilized to identify the patients with HFpEF. A multi-biomarker panel (selected from the same 17 biomarkers described above) which included MMP-2, MMP-8, TIMP-4, and PIIINP provided a prediction algorithm for HFpEF both with good sensitivity and acceptable specificity (AUC = 0.79, Fig. 7) [55]. Thus, a different plasma MMP profile emerged for HFpEF patients compared with LVH patients. Specifically, plasma MMP-2 and MMP-7 were increased, whereas MMP-8 levels were decreased. This likely reflects a local shift in cell type activation as well as ECM proteolytic events occurring in HFpEF patients. Specifically, increased plasma MMP-2 levels may act in concert with increased MT1-MMP and TIMP-2 to cause activation of profibrotic pathways linked to TGF-B. Increased MMP-7 levels have been associated with the wound healing response, are expressed in resident cells such as macrophages, and may be indicative of local alterations in the cell types and expression patterns occurring within the ECM. In addition, the decrease in MMP-8 in the HFpEF patients suggests a phenotypic change in cell types and MMP expression patterns. MMP-8, a neutrophil collagenase, may be reflective of changes in neutrophil synthesis and activation and result in decreased collagen degradation. The increase in TIMP-4 levels in HFpEF would imply a further induction of a myocardial profibrotic state by MMP inhibition. Taken together, the multi-biomarker panel in HFpEF patients suggested the presence of a shift in collagen homeostasis to a profibrotic condition.
Receiver operator curve (ROC) analysis for plasma biomarker detection of heart failure with a preserved ejection fraction (HFpEF). Observed area under the curve (AUC) for HFpEF using clinical covariates plus the four biomarker panel = 0.79 (0.73 to 0.86). From Zile et al. [55]
Galectin-3 and sST-2 Predict Prognosis
The prognostic utility of the MMP, TIMP, collagen, and matricellular biomarkers described above has not been examined. However, sST-2 and galectin-3 have been studied. A number of studies have demonstrated that Gal-3 is increased in HFpEF and predicts worse outcome in HFpEF. Because Gal-3 is related to aldosterone signaling, a high Gal-3 level may help identify those HFpEF patients that are most responsive to treatment with an aldosterone antagonist. Soluble ST2 is increased in HFpEF and is associated with diastolic dysfunction, fibrosis, and decompensation (Table 1).
MicroRNAs
In addition to protein and peptide biomarkers, a number of plasma microRNAs (miRs) were examined in these patient groups. MiRs are products of non-coding genes that act to repress protein translation. MiRs 29a, 1, 21, 133a were increased in patients with LVH but no HFpEF. These miRs have been associated with inhibition of myocardial fibrosis. MiRs 29a, 1, 21, 133a returned to normal levels in patients with LVH and HFpEF. These changes in miRs result in a removal of the suppression of translation of proteins that result in activation of profibrotic cascades and result in myocardial fibrosis. MiRs have not yet been applied as diagnostic or prognostic biomarkers in patients with HFpEF.
Biomarkers Reflecting Collagen Homeostasis: Biomarker-Guided Treatment—The Future
To date, biomarkers reflective of myocardial fibrosis and collagen homeostasis have not been used to guide management of patients with HFpEF. However, there are several factors that make this application both reasonable and expected.
Existing pharmaceutical approaches, novel drugs under development, and novel devices under development have mechanisms of action that alter or are likely to alter both collagen homeostasis and myocardial fibrosis. Therefore, biomarker profiling may allow individualization of treatment approach selective to specific processes present in each patient. One such example is the use of baseline Gal-3 levels to predict response to aldosterone antagonism. There is a significant positive relationship between Gal-3 levels and aldosterone signaling. Thus, a clinical trial is being planned (Reduction in events with galectin-3 and aldo blockade in acute heart failure, REGAL) which will test the hypothesis that Gal-3-guided therapy with spironolactone in patients admitted with ADHF will decrease heart failure-related events over subsequent 90 days of post-discharge follow-up. HFpEF patients with a high baseline Gal-3 will be selected for aldo antagonist treatment. A high Gal-3 level will identify those HFpEF patients that are most likely to be responsive to treatment with an aldosterone antagonist. A similar approach could be applied to selection of patients for treatment with neuromodulation devices. Another example is the use of treatment-induced changes in determinants of collagen homeostasis to tailor drug dose and choice during a course of treatment. After initiation of treatment, a change from baseline in biomarker content during treatment could be examined. An adequate response would be indicated if biomarker content were changed toward normal values. The utility of the use of baseline or change from baseline in these biomarkers would be suggested if this tailored therapy resulted in decreased events, improved clinical status, improvement diastolic function, and reduced fibrosis.
Unlike biomarkers of LVDP above, since a change in fibrosis would be time dependent, not instantaneous, and would require consideration of longer half-life of collagen protein itself, the frequency with which these would be measured would be weekly or monthly or quarterly. It is likely that multiple biomarkers used in combination would be most powerful in creating tailored therapy. The reasons for this include the fact that like all HF syndromes, the mechanisms causing HFpEF are numerous and they act independently and interdependently. This is true in HFrEF as well. For example, evidenced-based guidelines for the treatment of symptomatic patients with HFrEF include the use of multiple drugs and devices that target a number of different underlying pathophysiologic mechanisms that have been demonstrated to cause the development or progression of HFrEF. These facts should inform the development of novel and effective management strategies for HFpEF in the following manner. First, novel and effective management of HFpEF must target these pathophysiologic mechanisms including treatments that alter in both hemodynamic load and fibrosis. Second, comprehensive treatment will require multiple drugs and devices that individually target multiple independent mechanisms. This multi-targeted approach is necessary because each mechanism independent of other mechanisms likely contributes to disease progression. Therefore, HFpEF will require a multi-targeted approach that synergistically acts to improve morbidity and mortality in HFpEF. Therapy tailored both by the use of baseline and a change from baselines values of biomarkers will by necessity be based on a multi-biomarker panel approach.
References
Owan, T., Hodge, D., Herges, D., et al. (2006). Heart failure with preserved ejection fraction: trends in prevalence and outcomes. The New England Journal of Medicine, 355, 308.
Steinberg, B. A., Zhao, X., Heidenreich, P. A., et al. (2012). Trends in patients hospitalized with heart failure and preserved left ventricular ejection fraction: prevalence, therapies, and outcomes. Circulation, 126, 65–75.
Campbell, R., Jhund, P. S., Castagno, D., Hawkins, N. M., Petrie, M. C., & McMurray, J. J. V. (2012). What have we learnt about patients with heart failure and preserved ejection fraction (HF-PEF) from DIG-PEF, CHARM-Preserved and I-Preserve? Journal of the American College of Cardiology, 60, 2349–2356.
Farr, M. J., Lang, C. C., Lamanca, J. J., Zile, M. R., Francis, G., Tavazzi, L., et al. (2008). Cardiopulmonary exercise variables in diastolic versus systolic heart failure. The American Journal of Cardiology, 102, 203–206.
Rector, T. S., Carson, P. E., Anand, I. S., McMurray, J. J., Zile, M. R., McKelvie, R. S., et al. (2012). Assessment of long-term effects of irbesartan on heart failure with preserved ejection fraction as measured by the Minnesota Living with Heart Failure Questionnaire in the I-PRESERVE Trial. Circulation. Heart Failure, 5, 217–225.
Zile, M.R., Kjellstrom, B., Bennett, T., Cho, Y., Baicu, C., Aaron, M., Abraham, W., Bourge, R.C., Kueffer, F. (2013). Effects of exercise on left ventricular systolic and diastolic properties in patients with heart failure and a preserved ejection fraction versus heart failure and a reduced ejection fraction. Circulation. Heart Failure. doi:10.1161/CIRCHEARTFAILURE.112.000216.
Little, W. C., & Zile, M. R. (2012). HFpEF: cardiovascular abnormalities not just co-morbidities. Circulation Heart Fail., 5, 669–671.
Gaasch, W. H., & Zile, M. R. (2011). Left ventricular structural remodeling in health and disease: with special emphasis on volume, mass, and relative wall thickness. Journal of the American College of Cardiology, 58, 1733–1740.
Zile, M. R., Gottdiener, J. S., Hetzel, S. J., McMurray, J. J., Komajda, M., McKelvie, R., et al. (2011). Prevalence and significance of alterations in cardiac structure and function in patients with heart failure and a preserved ejection fraction. Circulation, 124, 2491–2501.
Gaasch, W. H., Delorey, D. E., Kueffer, F. J., & Zile, M. R. (2009). Distribution of left ventricular ejection fraction in patients with ischemic and hypertensive heart disease and chronic heart failure. The American Journal of Cardiology, 104, 1413–1415.
Aurigemma, G. P., Zile, M. R., & Gaasch, W. H. (2006). Contractile behavior in the left ventricle in diastolic heart failure: with emphasis on regional systolic function. Circulation, 113, 296–304.
Baicu, C. F., Zile, M. R., Aurigemma, G. P., & Gaasch, W. H. (2005). Left ventricular systolic performance, function, and contractility in patients with diastolic heart failure. Circulation, 111, 2306–2312.
Zile, M. R., Baicu, C. F., & Gaasch, W. H. (2004). Diastolic heart failure—abnormalities in active relaxation and passive stiffness of the left ventricle. The New England Journal of Medicine, 350, 1953–1959.
Borbely, A., van der Velden, J., Papp, Z., Bronzwaer, J. G., Edes, I., Stienen, G. J., et al. (2005). Cardiomyocyte stiffness in diastolic heart failure. Circulation, 111, 774–781.
van Heerebeek, L., Hamdani, N., Handoko, M. L., Falcao-Pires, I., Musters, R. J., Kupreishvili, K., et al. (2008). Diastolic stiffness of the failing diabetic heart: importance of fibrosis, advanced glycation end products, and myocyte resting tension. Circulation, 117, 43–51.
Westermann, D., Kasner, M., Steendijk, P., Spillmann, F., Riad, A., Weitmann, K., et al. (2008). Role of left ventricular stiffness in heart failure with normal ejection fraction. Circulation, 117, 2051–2060.
Ahmed, A., Rich, M. W., Fleg, J. L., Zile, M. R., Young, J. B., Kitzman, D. W., et al. (2006). Effects of digoxin on morbidity and mortality in diastolic heart failure: The Ancillary Digitalis Investigation Group Trial. Circulation, 114, 397–403.
Yusuf, S., Pfeffer, M. A., Swedberg, K., Granger, C. B., Held, P., McMurray, J. J., et al. (2003). Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM Preserved Trial. The Lancet, 362, 777–781.
Cleland, J. G. F., Tendera, M., Adamus, J., Freemantle, N., Polonski, L., & Taylor, J. (2006). The Perindopril in Elderly People with Chronic Heart Failure (PEP-CHF) Study. European Heart Journal, 27, 2338–2345.
Massie, B. M., Carson, P. E., McMurray, J. J., Komajda, M., McKelvie, R., Zile, M. R., et al. (2008). Irbesartan in patients with heart failure and preserved ejection fraction. The New England Journal of Medicine, 359, 2456–2467.
van Veldhuisen, D. J., Cohen-Solal, A., Böhm, M., Anker, S. D., Babalis, D., Roughton, M., et al. (2009). Beta-blockade with nebivolol in elderly heart failure patients with impaired and preserved left ventricular ejection fraction: data from SENIORS (Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors With Heart Failure). Journal of the American College of Cardiology, 53, 2150–2158.
McMurray, J. J., Adamopoulos, S., Anker, S. D., Auricchio, A., Bohm, M., Dickstein, K., et al. (2012). ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. European Heart Journal, 33, 1787–1847.
Braunwald, E. (2008). Biomarkers in heart failure. The New England Journal of Medicine, 358, 2148–2159.
van Kimmenade, R. R., & Januzzi, J. L. (2012). Emerging biomarkers in heart failure. Clinical Chemistry, 58, 127–138.
Azevedo, C. F., Nigri, M., Higuchi, M. L., Pomerantzeff, P. M., Spina, G. S., Sampaio, R. O., et al. (2010). Prognostic significance of myocardial fibrosis quantification by histopathology and magnetic resonance imaging in patients with severe aortic valve disease. Journal of the American College of Cardiology, 56, 278–287.
Spinale, F. G., Janicki, J. S., & Zile, M. R. (2013). Membrane-associated matrix proteolysis and heart failure. Circulation Research, 112, 195–208.
Spinale, F.G., Zile, M.R. (2013) Heart failure progression and recognition—categorical considerations for translation research. Circ Res (in press).
Wang, T. J., Wollert, K. C., Larson, M. G., Coglianese, E., McCabe, E. L., Cheng, S., et al. (2012). Prognostic utility of novel biomarkers of cardiovascular stress; The Framingham Heart Study. Circulation, 126, 1596–1604.
Wang, Y. C., Yu, C. C., Chiu, F. C., Tsai, C. T., Lai, L. P., Hwang, J. J., et al. (2013). Soluble ST2 as a biomarker for detecting stable heart failure with a normal ejection fraction in hypertensive patients. J Cardiol Fail., 19, 163–168.
Bhardwaj, A., & Januzzai, J. L. (2010). ST2: a novel biomarker for heart failure. Expert Review of Molecular Diagnostics, 10, 459–464.
deFilippi, C. R., & Felker, G. M. (2010). Galectin-3 in heart failure—linking fibrosis, remodeling and progression. Euro Cardiology, 6, 33–36.
de Boer, R. A., Lok, D. J., Jaarsma, T., van der Meer, P., Voors, A. A., Hillege, H. L., et al. (2011). Predictive value of plasma galectin-3 levels in heart failure with reduced and preserved ejection fraction. Annals of Medicine, 43, 60–68.
Yu, L., Ruifrok, W. P., Meissner, M., Bos, E. M., van Goor, H., Sanjabi, B., et al. (2013). Genetic and pharmacological inhibition of galectin-3 prevents cardiac remodeling by interfering with myocardial fibrogenesis. Circulation. Heart Failure, 6, 107–117.
van der Velde, A. R., Gullestad, L., Ueland, T., Aukrust, P., Guo, Y., Adourian, A., et al. (2013). Prognostic value of changes in galectin-3 levels over time in patients with heart failure: data from CORONA and COACH. Circulation Heart Failure, 6, 219–226.
van Veldhuisen, D. J., Linssen, G. C., Jaarsma, T., van Gilst, W. H., Hoes, A. W., Tijssen, J. G., et al. (2013). B-type natriuretic peptide and prognosis in heart failure patients with preserved and reduced ejection fraction. Journal of the American College of Cardiology, 61, 1498–1506.
Januzzi, J. L., Jr., Rehman, S. U., Mohammed, A. A., Bhardwaj, A., Barajas, L., Barajas, J., et al. (2011). Use of amino-terminal pro-b-type natriuretic peptide to guide outpatient therapy of patients with chronic left ventricular systolic dysfunction. Journal of the American College of Cardiology, 58, 1881–1889.
Maisel, A. (2011). Biomonitoring and biomarker-guided therapy: the next step in heart failure and biomarker research. Journal of the American College of Cardiology, 58, 1890–1892.
Van Kimmenade, R. R. J., & Januzzi, J. L. (2012). Using natriuretic peptides to ‘guide’ therapy in heart failure. Euro Cardiology., 8, 36–39.
Richards, A. M. (2008). Serial measurements of plasma b-type natriuretic peptides: what do they tell us? Journal of the American College of Cardiology, 52, 1004–1005.
Maisel, A., Barnard, D., Jaski, B., Frivold, G., Marais, J., Azer, M., et al. (2013). Primary results of the HABIT (HF Assessment with Bnp In The Home) Trial. Journal of the American College of Cardiology, 61, 1726–1735.
Lainchbury, J. G., Troughton, R. W., Strangman, K. M., Frampton, C. M., Pilbrow, A., Yandle, T. G., et al. (2009). N-Terminal pro-B-type natriuretic peptide-guided treatment for chronic heart failure: results from the BATTLESCARRED (NT-proBNP-Assisted Treatment To Lessen Serial Cardiac Readmissions and Death) Trial. Journal of the American College of Cardiology, 55, 53–60.
Weiner, R. B., Baggish, A. L., Chen-Tournoux, A., Marshall, J. E., Gaggin, H. K., Bhardwaj, A., et al. (2013). Improvement in structural and functional echocardiographic parameters during chronic heart failure therapy guided by natriuretic peptides: mechanistic insights from the ProBNP Outpatient Tailored Chronic Heart Failure (PROTECT) Study. European Journal of Heart Failure, 15, 342–351.
Anand, I. S., Rector, T. S., Cleland, J. G., Kuskowski, M., McKelvie, R. S., Persson, H., et al. (2011). Prognostic value of baseline plasma amino-terminal pro-brain natriuretic peptide and its interactions with irbesartan treatment effects in patients with heart failure and preserved ejection fraction: findings from the I-PRESERVE Trial. Circulation. Heart Failure, 4, 569–577.
McKelvie, R. S., Komajda, M., McMurray, J., Zile, M. R., Ptaszynska, A., Donovan, M., et al. (2010). Baseline plasma NT-proBNP and clinical characteristics: results from the Irbesartan In Heart Failure With Preserved Ejection Fraction Trial. Journal of Cardiac Failure, 16(2), 128–134.
Jhund PS, Anand IS, Komajda M, McKelvie RS, Zile MR, Massie B, Carson PE, McMurray JJV. (2013). Change in N-terminal pro-B-type natriuretic peptide levels and outcomes in heart failure with preserved ejection fraction: an analysis of the I-PRESERVE study. Eur Heart J (in press).
Iwanaga, Y., Nishi, I., Furuichi, S., Noguchi, T., Sase, K., Kihara, Y., et al. (2006). B-type natriuretic peptide strongly reflects diastolic wall stress in patients with chronic heart failure: comparison between systolic and diastolic heart failure. Journal of the American College of Cardiology, 47(4), 742–748.
Zile, M. R., Bennett, T. D., St. John Sutton, M., Cho, Y. K., Adamson, P. B., Aaron, M. F., et al. (2008). Transition from chronic compensated to acute decompensated heart failure: pathophysiologic insights obtained from continuous monitoring of intracardiac pressures. Circulation, 118(14), 1433–1441.
Stevenson, L. W., Zile, M., Bennett, T. D., Kueffer, F. J., Jessup, M. L., Adamson, P., et al. (2010). Chronic ambulatory intracardiac pressures and future heart failure events. Circulation. Heart Failure, 3, 580–587.
Abraham, W. T., Adamson, P. B., Bourge, R. C., Aaron, M. F., Costanzo, M. R., Stevenson, L. W., et al. (2011). Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. The Lancet, 377, 658–666.
Solomon, S. D., Zile, M. R., Pieske, B., Voors, A., Shah, A., Kraigher-Krainer, E., et al. (2012). The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase II randomized-controlled trial. The Lancet, 380, 1387–1395.
Chen, H. H., Glockner, J. F., Schirger, J. A., Cataliotti, A., Redfield, M. M., & Jr. Burnett, J. C. (2012). Novel protein therapeutics for systolic heart failure: chronic subcutaneous B-type natriuretic peptide. Journal of the American College of Cardiology, 60, 2305–2312.
O’Connor, C. M., Starling, R. C., Hernandez, A. F., et al. (2011). Effect of nesiritide in patients with acute decompensated heart failure. The New England Journal of Medicine, 365, 32–43.
Baicu, C. F., Li, J., Zhang, Y., Kasiganesan, H., Cooper, G., Zile, M. R., et al. (2012). Time course of right ventricular pressure-overload induced myocardial fibrosis: relationship to changes in fibroblast dependent post-synthetic procollagen processing. American Journal of Physiology-Heart and Circulatory Physiology, 303, H1128–H1134. PMCID: In Progress.
Zile, M. R., Baicu, C. F., Stroud, R. E., Van Laer, A., Arroyo, J., Mukherjee, R., et al. (2012). Pressure-overload department membrane-type 1 matrix metalloproteinase induction: relationship to LV remodeling and fibrosis. American Journal of Physiology - Heart and Circulatory Physiology, 302, H1429–H1437.
Zile, M. R., DeSantis, S. M., Baicu, C. F., Stroud, R. E., Thompson, S. B., McClure, C. D., et al. (2011). Plasma biomarkers that reflect determinants of matrix composition identify the presence of left ventricular hypertrophy and diastolic heart failure. Circulation. Heart Failure, 4, 246–256.
Martos, R., Baugh, J., Ledwidge, M., O'Loughlin, C., Conlon, C., Patle, A., et al. (2007). Diastolic heart failure: evidence of increased myocardial collagen turnover linked to diastolic dysfunction. Circulation, 115, 888–895.
López, B., González, A., & Díez, J. (2010). Circulating biomarkers of collagen metabolism in cardiac diseases. Circulation, 121, 1645–1654.
González, A., López, B., Querejeta, R., Zubillaga, E., Echeverría, T., & Díez, J. (2010). Filling pressures and collagen metabolism in hypertensive patients with heart failure and normal ejection fraction. Hypertension, 55, 1418–1424.
Krum, H., Elsik, M., Schneider, H. G., Ptaszynska, A., Black, M., Carson, P., et al. (2011). Relation of peripheral collagen markers to death and hospitalisation in patients with heart failure and preserved ejection fraction: results of the I-PRESERVE collagen sub-study. Cir Heart Fail, 4, 561–568.
Bradshaw, A. D., Baicu, C. F., Rentz, T. J., Van Laer, A. O., Boggs, J., Lacy, J. M., et al. (2009). Pressure-overload induced alterations in fibrillar collagen content and myocardial diastolic function: role of SPARC in post-synthetic procollagen processing. Circulation, 119, 269–280.
Bradshaw, A. D., Baicu, C. F., Rentz, T. J., Van Laer, A. O., Bonnema, D. D., & Zile, M. R. (2010). Age-dependent alterations in fibrillar collagen content and myocardial diastolic function: role of SPARC in post-synthetic procollagen processing. American Journal of Physiology - Heart and Circulatory Physiology, 298, H614–H622.
Baicu, C. F., Zhang, Y., Van Laer, A. O., Renaud, L., Zile, M. R., & Bradshaw, A. D. (2012). Effects of the absence of procollagen C-endopeptidase enhancer-2 (PCOLCE-2) on myocardial collagen accumulation in chronic pressure-overload. American Journal of Physiology - Heart and Circulatory Physiology, 303, H234–H240.
Bartunek, J., Delrue, L., Van Durme, F., Muller, O., Casselman, F., De Wiest, B., et al. (2008). Nonmyocardial production of ST2 protein in human hypertrophy and failure is related to diastolic load. Journal of the American College of Cardiology, 52(25), 2166–2174.
Manzano-Fernández, S., Mueller, T., Pascual-Figal, D., Truong, Q. A., & Januzzi, J. L. (2011). Usefulness of soluble concentrations of interleukin family member ST2 as predictor of mortality in patients with acutely decompensated heart failure relative to left ventricular ejection fraction. The American Journal of Cardiology, 107(2), 259–267.
Rehman, S. U., Mueller, T., & Januzzi, J. L., Jr. (2008). Characteristics of the novel interleukin family biomarker ST2 in patients with acute heart failure. Journal of the American College of Cardiology, 52(18), 1458–1465.
Gopal, D. M., Kommineni, M., Ayalon, N., Christian Koelbl, C., Rivka Ayalon, R., Andreia Biolo, A., et al. (2012). Relationship of plasma galectin-3 to renal function in patients with heart failure: effects of clinical status, pathophysiology of heart failure, and presence or absence of heart failure. J Am Heart Assoc., 1, e000760. doi:10.1161/JAHA.112.000760.
Shah, R. V., Chen-Tournoux, A. A., Picard, M. H., van Kimmenade, R. R., & Januzzi, J. L. (2010). Galectin-3, cardiac structure and function, and long-term mortality in patients with acutely decompensated heart failure. European Journal of Heart Failure, 12(8), 826–832.
van Kimmenade, R. R., Januzzi, J. L., Jr., Ellinor, P. T., Sharma, U. C., Bakker, J. A., Low, A. F., et al. (2006). Utility of amino-terminal pro-brain natriuretic peptide, galectin-3, and apelin for the evaluation of patients with acute heart failure. Journal of the American College of Cardiology, 48(6), 1217–1224.
de Boer RA, Van Veldhuisen DJ, deFilippi C, Muntendam P, Adourian AS, Guo Y, Januzzi JL. (2011). Plasma galectin-3 is associated with near-term rehospitalization in heart failure. Poster Abstract #297, 15th Annual Scientific Meeting of the Heart Failure Society of America, Boston, MA, 18–21 Sept
Martos, R., Baugh, J., Ledwidge, M., O'Loughlin, C., Murphy, N. F., Conlon, C., et al. (2009). Diagnosis of heart failure with preserved ejection fraction: improved accuracy with the use of markers of collagen turnover. European Journal of Heart Failure, 11(2), 191–197.
Barasch, E., Gottdiener, J. S., Aurigemma, G., Kitzman, D. W., Han, J., Kop, W. J., et al. (2009). Association between elevated fibrosis markers and heart failure in the elderly: the Cardiovascular Health Study. Circulation. Heart Failure, 2(4), 303–310.
Kitahara, T., Takeishi, Y., Arimoto, T., Niizeki, T., Koyama, Y., Sasaki, T., et al. (2007). Serum carboxy-terminal telopeptide of type I collagen (ICTP) predicts cardiac events in chronic heart failure patients with preserved left ventricular systolic function. Circulation Journal, 71(6), 929–935.
Barasch, E., Gottdiener, J. S., Aurigemma, G., Kitzman, D. W., Han, J., Kop, W. J., et al. (2011). The relationship between serum markers of collagen turnover and cardiovascular outcome in the elderly: the Cardiovascular Health Study. Circulation. Heart Failure, 4(6), 733–739.
Ahmed, S. H., Clark, L. L., Pennington, W. R., Webb, C. S., Bonnema, D. D., Leonardi, A. H., et al. (2006). Matrix metalloproteinases/tissue inhibitors of metalloproteinases: relationship between changes in proteolytic determinants of matrix composition and structural, functional, and clinical manifestations of hypertensive heart disease. Circulation, 113(17), 2089–2096.
Acknowledgments
Dr. Michael Zile is supported by the Research Service of the Department of Veterans Affairs (5101CX000415-02 and 5101BX000487-04).
Conflict of Interest
Dr. Zile is a consultant to and receives research support from Alere, BG Medicine, Medtronic, and Novartis. Dr. Baicu has no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zile, M.R., Baicu, C.F. Biomarkers of Diastolic Dysfunction and Myocardial Fibrosis: Application to Heart Failure with a Preserved Ejection Fraction. J. of Cardiovasc. Trans. Res. 6, 501–515 (2013). https://doi.org/10.1007/s12265-013-9472-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-013-9472-1