Abstract
Neovascularization has been linked to the progression and vulnerability of atherosclerotic lesions. Angiogenesis is increased in lipid-rich plaque. Hypoxia-inducible factor alpha (HIF-1α) is a key transcriptional regulator responding to hypoxia and activating genes, which promote angiogenesis, among them vascular endothelial growth factor (VEGF). Oxidized low-density lipoprotein (oxLDL) is generated in lipid-rich plaque by oxidative stress. It triggers an inflammatory response and was traditionally thought to inhibit endothelial cells. New data, however, suggest that oxLDL can activate HIF-1α in monocytes in a hypoxia-independent fashion. We hypothesized that HIF-1α activation in monocyte–macrophages could transmit proangiogenic effects of oxLDL linking hyperlipidemia, inflammation, and angiogenesis in atherosclerosis. First, we examined the effect of oxLDL on HIF-1α and VEGF expression in monocyte–macrophages and on their proangiogenic effect on endothelial cells in vitro in a monocyte–macrophage/endothelial co-culture model. OxLDL strongly induced HIF-1α and VEGF in monocyte–macrophages and significantly increased tube formation in co-cultured endothelial cells. HIF-1α inhibition reversed this effect. Second, we demonstrated a direct proangiogenic effect of oxLDL in an in vivo angiogenesis assay. Again, HIF-1α inhibition abrogated the proangiogenic effect of oxLDL. Third, in a rabbit atherosclerosis model, we studied the effect of dietary lipid lowering on arterial HIF-1α and VEGF expression. The administration of low-lipid diet significantly reduced the expression of both HIF-1α and VEGF, resulting in decreased plaque neovascularization. Our data point to oxLDL as a proangiogenic agent linking hyperlipidemia, inflammation, and angiogenesis in atherosclerosis. This effect is dependent on macrophages and, at least in part, on the induction of the HIF-1α pathway.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent observations have linked intimal neovascularization to atherosclerotic lesion progression and vulnerability [1–5]. Increased neovascularization and high numbers of inflammatory cells are a hallmark of lipid-rich plaque; however, the mechanisms linking hyperlipidemic conditions and enhanced angiogenesis are not well understood. Some investigators reported an association between intraplaque angiogenesis and deposition of lipoproteins from “leaky” microvessels [6]. LDL in its oxidized form is a strong chemoattractant for monocytes and it is abundant within lipid-rich lesions exerting powerful biological effects through multiple pathways [7–10]. Hypoxia-inducible factor alpha (HIF-1α) is also expressed in atheroma and is a key transcriptional regulator of genes promoting angiogenesis such as vascular endothelial growth factor (VEGF) [11–15]. Recent reports have linked hypoxia in human atherosclerotic tissue to HIF-1α and VEGF expression, even though the methodology of measuring tissue hypoxia is not trouble-free [12,16]. Of note, monocytes and macrophages have oxygen tension sensing capacity and respond to hypoxic stress in various tissues [17–19]. In addition to hypoxic signals driving intimal angiogenesis, oxidative stress is increasingly implicated as well [16,20–23]. A hypoxia-independent activation of HIF-1α by oxidized low-density lipoprotein (oxLDL) has been described in vitro in monocytes [24]. We hypothesized that oxLDL could transmit proangiogenic signals via monocyte–macrophages linking hyperlipidemia, inflammation, and angiogenesis. To test this hypothesis, we examined HIF-1α activation in monocyte–macrophages exposed to oxLDL and tested their proangiogenic effect in a co-culture model with endothelial cells. We also tested for a proangiogenic effect of oxLDL in vivo using the Matrigel plug assay. Lastly, we evaluated the effect of dietary lipid lowering on intimal HIF-1α and VEGF expression and on intimal neovascularization in a rabbit atherosclerosis model.
Materials and Methods
In Vitro Effects of OxLDL and Hypoxia on Human Monocyte–Macrophages
Mononuclear cells from peripheral blood of healthy human subjects were isolated by Ficoll Paque (Amersham Biosciences) density gradient centrifugation. A highly pure (>99 %) CD14+ monocyte population was obtained by MACS cell sorting (Miltenyi Biotec). Cell viability was verified by Trypan blue staining. Monocytes were seeded at a density of 1 × 106 cells/ml in eight-well chamber slides (Nalgene Nunc) containning RPMI 1640 (Gibco) with 1 % penicillin/streptomycin and 1 % heat-inactivated FCS. LDL (Sigma) was CuSO4-oxidized in vitro as previously published [7]. The oxidization of LDL was verified by agarose gel electrophoresis. Adherent monocytes were grown at 37 °C and then were treated either only with oxLDL (75 μg/ml) or with oxLDL combined with hypoxia for 6 h. Hypoxia was induced in a sealed modular incubator chamber (Billups-Rothenberg) flushed with 1 % O2, 5 % CO2, and 94 % N2 (1 % O2). Normoxia was maintained by placing the cells in a routine 5 % CO2 and 95 % room air incubator (20 % O2).
Transcriptional Activity Assay for HIF-1α
The transcriptional activity of HIF-1a was measured under normoxic conditions in cells treated either with oxLDL alone or with oxLDL and the antioxidant tiron (Sigma). Untreated cells or cells treated with tiron alone served as controls. Nuclear extracts of monocyte–macrophages were prepared. HIF-1α transcriptional activity was determined by an ELISA-based Trans-AM HIF-1α kit (Active Motif). Specificity of HIF-1α binding was confirmed by incubating nuclear extracts with immobilized AP-1 consensus-binding probe in the presence of excess WT or mutated oligonucleotide.
Immunocytochemistry
Quantitative evaluation of cellular expression of HIF-1α and VEGF was based on immunocytochemistry. Monocyte–macrophages cultured on chamberslides were washed and subsequently stained using immunofluorescent labeling with anti-HIF-1α and anti-VEGF primary antibodies in conjunction with secondary antibodies conjugated to FITC or Texas Red. DAPI was used for nuclear counterstaining of all cultured cells. Two different fields were chosen randomly in each well and photographs were taken with dark-field microscopy and appropriate excitation filters. The number of all DAPI-positive nuclei per field was counted as well as the number of DAPI-positive nuclei associated with Texas Red or FITC signals using Image Pro Plus software. Cells labeling positive for either antigen were expressed as percentage of total cells per microscopic field. For each experiment, at least three wells per condition were seeded and examined, and each experiment was replicated three times.
In Vitro Monocyte–Macrophage and Endothelial Cell Co-culture System
Ice-cold growth factor-depleted Matrigel (Becton Dickinson) was placed into 24-well plates and polymerized for 30 min at 37 °C. Human umbilical vein endothelial cells (HUVECs), which were starved for 24 h in DMEM (Gibco) containing 5 % FCS but no VEGF, were seeded onto polymerized Matrigel (104 cells/well). After attachment of HUVECs, the in vitro co-culture model was assembled by placing transwell chambers (Corning) with or without monocytes (5 × 104 cells/well) on top of the endothelial cells (Fig. 1, panel 2). Six different experimental groups were prepared: group 1 consisted of HUVECs alone without stimulation, group 2 comprised HUVECs and monocyte–macrophages in co-culture without treatment, group 3 comprised HUVECs treated with oxLDL (20 μg/ml), group 4 included HUVECs and monocyte–macrophages in co-culture both treated with oxLDL, group 5 consisted of HUVECs alone treated with the HIF-1α inhibitor chetomin (Alexis Biochemicals) at a concentration of 50 nM [25], and group 6 included HUVECs and monocyte–macrophages in co-culture both treated with oxLDL and chetomin (Fig. 1, panel 2). After 12 h, transwell chambers were removed and evaluation of endothelial tube formation was performed. Two different fields were chosen randomly in each well and photographs were taken with a phase-contrast microscope. The length of the tubes was measured using Image Pro Plus software and expressed as average length (micrometer) per microscopic field. For each experiment, at least three wells per condition were seeded, and each experiment was replicated three times.
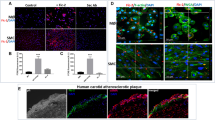
Panel 1: Effect of oxLDL on HIF-1α and VEGF in monocytes. a–h Representative pictures of HIF-1α (a–d) and VEGF (e–h) expression in monocytes cultured under normoxia without oxLDL (a, e), under normoxia with oxLDL (b, f), under hypoxia without oxLDL (c, g), and under hypoxia with oxLDL (d, h). A strong induction of HIF-1α and VEGF by oxLDL was observed independent of the presence of hypoxia (×400). i–k Double labeling for HIF-1α (i) and VEGF (j) showed clear co-localization of both antigens in single oxLDL-treated monocytes (overlay in k) (×1,000). l Quantitative evaluation confirmed the significant increase in HIF-1α and VEGF expression with oxLDL treatment to a degree similar to hypoxia-induced expression. Combining oxLDL and hypoxia further enhanced the expression of both HIF-1α and VEGF (ANOVA, P < 0.05). m Transcriptional activation of HIF-1α as measured by the Trans-AM assay was elevated significantly in monocytes treated with oxLDL. Of note, co-treatment with the antioxidant (tiron) abrogated HIF-1α transcriptional activation induced by oxLDL (ANOVA, P < 0.05). Panel 2: Effect of oxLDL on monocyte-mediated angiogenesis. a–f HUVECs were seeded onto growth factor-depleted Matrigel in a transwell co-culture setup (shown in g) in the presence of monocytes (b, d, f) or without monocytes (a, c, e). The monocytes were either left untreated (a, b), treated with oxLDL (c, d), treated with the HIF-1α inhibitor chetomin (e), or with oxLDL and chetomin (f). HUVECs grown alone on growth factor-depleted Matrigel did not show significant tube formation (a) and were used as negative control. HUVECs under the same conditions grown in the presence of untreated monocytes did not show tube formation either (b). Likewise, HUVECs grown alone but treated with oxLDL did also not show signs of tube formation (c). However, HUVECs grown in the presence of oxLDL-treated monocytes did show extensive tube formation (arrows) reflecting increased angiogenic activity (d). Of note, co-treatment of monocytes with the HIF-1α inhibitor chetomin significantly suppressed the proangiogenic effect of oxLDL treatment (f) and chetomin did not have an effect on HUVECs alone (e). g Schematic drawing of the monocyte endothelial co-culture system for determining capillary tube-like structure formation. h Bar graphs comparing the length of endothelial tube formation as measured in micrometers. In summary, groups 1–3 and 5 served as various controls, and groups 4 and 6 were the two treatment groups as described from a to f (ANOVA P < 0.01; error bars ± SEM)
In Vivo Matrigel Plug Assay
The five experimental groups for this in vivo angiogenesis assay consisted of two control groups with growth factor-depleted Matrigel (0.5 ml/plug) containing no VEGF (negative control), or containing VEGF at a concentration of 300 ng/ml (positive control) and three treatment groups with growth factor-depleted Matrigel containing oxLDL (20 μg/ml) alone, VEGF combined with chetomin, or oxLDL combined with chetomin [25] (Fig. 2). These Matrigel preparations were injected s.c. in the midventral abdominal region of 6-week-old C57BL/6 mice (n = 5/group). After 2 weeks, animals were euthanized and the plugs were removed. The plugs were fixed with formalin and paraffin-embedded. Five-micrometer-thick serial sections were stained with hemtaoxylin–eosin staining. The length of erythrocyte-filled blood vessels was measured at a magnification of ×200 as previously reported [26]. In addition, endothelial cells were labeled using vWF antibody (Dako) or Ulex lectin (B&D) staining. Alternatively, plugs were harvested and homogenized in RIPA lysis buffer. After the removal of debris by centrifugation, the hemoglobin concentration was measured using Drabkin’s reagent (Sigma-Aldrich).
Effect of oxLDL on in vivo angiogenesis in Matrigel plug assay. a–j Growth factor-depleted Matrigel was used in an in vivo angiogenesis assay (Matrigel plug assay). Representative pictures for each condition were taken at low (×100) (a–e) and at intermediate (×200) magnification (f–j). As negative control, growth factor-depleted Matrigel was used alone and no capillary networks were observed (a, f). As positive control, growth factor-depleted Matrigel containing 300 ng/ml VEGF was used, and extensive capillary networks were seen (b, g). When combining VEGF treatment with the HIF-1α inhibitor chetomin, the extensive capillary network formation induced by VEGF was unchanged (c, h). Using growth factor-depleted Matrigel containing oxLDL, capillary networks as extensive as those seen with VEGF treatment were noted (d, i). Importantly, when combining oxLDL treatment with the HIF-1α inhibitor chetomin, the increased capillary network formation induced by oxLDL was nearly completely abrogated (e, j). k–n High power magnification (×1,000) of serial sections of tissue containing oxLDL-treated Matrigel plug stained with anti-CD31 antibody (k, m) reveals that erythrocyte-filled capillary networks seen with H&E staining (l, n) are lined by endothelial cells. o Bar graph comparing the number of capillary networks identified by visual field for each condition. In summary, oxLDL-induced capillary network formation even exceeded that induced by VEGF and, most notably, in contrast to VEGF, was abrogated by treatment with the HIF-1α inhibitor chetomin (ANOVA, P < 0.01; error bars ± SEM). p Bar graph comparing Hgb concentration of Matrigel plugs identified by Drabkin’s reagent for each condition. In summary, oxLDL resulted in the highest Hgb concentration and its effect was abrogated by treatment with the HIF-1α inhibitor chetomin (ANOVA, P < 0.01; error bars ± SEM)
Atherosclerosis Induction in Rabbits and Study Design
Atherosclerosis was induced in male New Zealand White rabbits (n = 18, age 3 months, weight 3.5 ± 0.2 kg) by a combination of 9 months of high-cholesterol (HC) diet (0.2 % cholesterol) and double balloon endothelial denudation as previously described [27]. This model results in the induction of advanced aortic atherosclerotic lesions [27,28]. In brief, aortic endothelial denudations were performed at 1 and 3 months after HC diet initiation using a 4-F Fogarty embolectomy catheter introduced via the iliac artery. All procedures were performed under general anesthesia induced by an intramuscular ketamine injection (20 mg/kg) and xylazine (10 mg/kg). At the end of the 9 months of the atherosclerosis induction period, the rabbits were randomized to continued HC diet or to normal chow (NC) for six additional months. At the time of randomization, the serum cholesterol was 630 ± 125 mg/dl for the HC diet group and 721 ± 143 mg/dl for the NC diet group. At the end of the treatment, the serum cholesterol had remained high with HC diet at 526 ± 108 mg/dl and had steeply dropped with NC diet to 27 ± 10 mg/dl (P < 0.01 vs. time of randomization and vs. HC group). All procedures and animal care were approved by the Institutional Animal Care and Use Committee and were in accordance with the “Guide for the Care and Use of Laboratory Animals” (National Research Council, Washington, D.C.: National Academy Press 1996).
Tissue Preparation
Tissue harvesting and preparation was performed as previously described [27]. Briefly, the rabbits were euthanized using a 5-ml i.v. injection of “Sleepaway” (Fort Dodge Animal Health). Heparin at a dose of 100 U/kg was injected intravenously 5 min prior to euthanasia to prevent postmortem thrombosis. The aortic root was cannulated, and the aorta was immediately flushed with 250 ml of PBS at pH 7.4. The ascending aorta, arch, and thoracic aorta were excised and snap-frozen in liquid nitrogen. The abdominal aorta was further perfused with cold (4 °C) 4 % paraformaledhyde in PBS at 100 mmHg. Serial sections of the aorta immediately distal to the origin of the left renal artery were cut at 3 mm intervals and subsequently paraffin-embedded for histology and immunohistochemistry. To quantify the extent of atherosclerotic disease, serial sections (4 μm) of the aorta were prepared as previously described [27], and atherosclerotic lesions in the aortic root were examined at five locations.
Protein Extraction and Western Blot
Expression of HIF-1α and VEGF protein was evaluated by Western Blot. Briefly, aortic tissue was sonicated and lysed for 30 min on ice in lysis buffer supplemented with a mixture of proteinase inhibitors (Sigma). The samples were cleared by microcentrifugation (14,000 rpm, 30 min, 4 °C) and assessed for protein concentration. One hundred micrograms of protein per sample was electrophoresed in a 10 % sodium dodecyl sulfate–polyacrylamide gel and electroblotted onto nitrocellulose membranes. After incubation in 1 % casein blocking buffer, the membranes were exposed to antibodies against HIF-1α (R&D) and against VEGF (Santa Cruz). After washing, the appropriate secondary antibody was applied for 1 h at room temperature. The bound antibodies were visualized by enhanced chemiluminescence (Amersham Pharmacia Biotech). Beta-actin labeling was used for control of loading conditions.
Histology and Immunostaining
Serial sections of abdominal aorta were stained by the combined Masson’s elastin method. Immunohistochemistry was performed on adjacent sections for HIF-1α (Novus), VEGF (R&D Systems), and antirabbit macrophage clone RAM-11 (Dako). Primary antibodies were detected with a HRP-streptavidin/biotin secondary antibody system (Biogenex) and counterstained with hematoxylin. In negative controls, primary antibody was substituted with the appropriate control IgG. HIF-1α and VEGF co-expression was validated by immunofluoresence double labeling using FITC- and Texas Red-coupled secondary antibodies (Jackson Immuno Laboratories). Neovessels were detected by staining with anti-CD31 (Dako) and anti-vWF (Dako) antibody.
Morphometry
The percentage of plaque cells expressing HIF-1α, VEGF, and RAM-11 was determined by computer-assisted planimetry (Software: Image-Pro-Plus 3.0.1). Intimal neovascularization was defined as tubuloluminal CD31-positive/vWF-positive structures recognized in cross-sectional and longitudinal profiles as identified by double immunohistochemistry with CD31 and vWF at ×400 magnification. Neovessel density was calculated by taking the total number of neovessels and dividing it by plaque area. Neovessel area was the sum of cross-sectional area of all neovessels measured. Neovessel content is defined as percentage of total plaque area covered by neovessels. Quantification was calculated for three contiguous, nonoverlapping sites for each individual section. Investigators performing the analysis were blinded to the study groups.
Statistical Analysis
Results are expressed as mean ± SEM. For data analysis, the SPSS/PC+ software was used. After testing for normal distribution, ANOVA was used to compare variables. Correlation coefficients were determined by Pearson’s test. Probability values were two-tailed and corrected for ties. P values < 0.05 were considered significant.
Results
Effect of OxLDL on HIF-1α and VEGF Expression in Monocyte–Macrophages In Vitro
Untreated control monocyte–macrophages did not express HIF-1α at detectable levels and only very low levels of VEGF (Fig. 1, panel 1). In contrast, exposure to oxLDL, even at normoxic conditions, resulted in a significant upregulation of both HIF-1α (23 ± 5 vs. 0.0 ± 0 %; P < 0.05) and VEGF (37 ± 6 vs. 4 ± 2 %; P < 0.05) expression. Double labeling demonstrated colocalization of HIF-1α and VEGF in monocyte–macrophages treated with oxLDL (Fig. 1, panel 1). Cells treated with native LDL or oxidized albumin did not exhibit labeling for HIF-1α or VEGF (data not shown). These data corroborate the findings by Shatrov et al. [24]. The degree of the upregulation of HIF-1α and VEGF expression in response to oxLDL was comparable to the increase observed under hypoxic conditions (HIF-1α 28 ± 5 % and VEGF 38 ± 6 %). The combination of hypoxia and oxLDL treatment induced an even further increase in the expression of HIF-1α and VEGF (HIF-1α 38 ± 6 % and VEGF 53 ± 9 %). Assessing HIF-1α activation at the transcriptional level, we also found a strong enhancement of transcription after treatment with oxLDL (Fig. 1, panel 2). Interestingly, this stimulatory effect of oxLDLwas practically abolished by co-treatment with the antioxidant (tiron) (Fig. 1, panel 2).
Effect of OxLDL on Angiogenesis in Monocyte–Macrophage/Endothelial Cell Co-culture
We determined the effect of oxLDL on angiogenic activity in a co-culture assay with monocyte–macrophages and endothelial cells (HUVECs) as shown in Fig. 1, panel 2. HUVECs were seeded on growth factor-depleted Matrigel to avoid baseline tube formation. As expected, control wells containing HUVECs alone showed only minimal tube formation under these conditions and served as negative control. The addition of monocyte–macrophages to the transwell chamber did not change the absence of endothelial tube formation. However, co-culture of HUVECs and monocytes–macrophages in the presence of oxLDL (20 μg/ml) resulted in a dramatic increase in endothelial tube formation (Fig. 1, panel 2). Of note, exposure of HUVECs to oxLDL in the absence of monocyte–macrophages did not induce an increase in endothelial tube formation. Importantly, the HIF-1α inhibitor chetomin strongly reduced endothelial tube formation in the oxLDL-treated HUVEC/monocyte–macrophage co-culture (Fig. 1, panel 2). Chetomin did not show any effect on HUVECs alone.
Effect of OxLDL on Angiogenesis In Vivo
When growth factor-depleted Matrigel without VEGF was used in the Matrigel plug assay in vivo, as expected, practically no vascular channel formation was observed (Fig. 2a, f). In contrast, when oxLDL (20 μg/ml) was added to the growth factor-depleted Matrigel, a profound increase in vascular channel formation (29 ± 4 mm of blood vessels per high power field) was observed (Fig. 2d, i). For comparative purposes, the addition of VEGF (300 ng/ml) induced 22 ± 2 mm of blood vessels per high power field, illustrating the strength of the proangiogenic effect of oxLDL (Fig. 2b, g). Of note, the proangiogenic effect of oxLDL was strongly blunted by the HIF-1α inhibitor chetomin (from 29 ± 4 to 6 ± 1 mm; P < 0.05) (Fig. 2e, j). The addition of chetomin to VEGF-treated Matrigel did not modify vascular channel formation (Fig. 2c, h). Hemoglobin concentration in Matrigel plugs was the highest with oxLDL and VEGF treatment at 1.7 ± 0.2 and 1.4 ± 0.2 mg/ml, respectively, both significantly higher than the control group (0.2 ± 0.1 mg/ml; P < 0.05). Of note, the addition of chetomin to oxLDL in Matrigel plugs also signicantly reduced the hemoglobin concentration (1.7 ± 0.2 vs. 0.5 ± 0.2 mg/ml; P < 0.05) (Fig. 2).
Effect of Dietary Lipid Reduction on Angiogenesis and Expression of HIF-1α and VEGF in Experimental Atherosclerosis
Neovascularization, especially in plaque shoulder areas, was present in atherosclerotic lesions of hyperlipidemic animals on continued HC diet (Fig. 3a–d). In contrast, neovessels were only very rarely seen in the intima of normolipidemic animals that resumed regular chow diet (Fig. 3i–l). Robust and concordant expression of HIF-1α and VEGF was observed in the intima of hyperlipidemic rabbits in close association with RAM-11-positive macrophages (HIF-1α at 11 ± 4 % and VEGF at 16 ± 5 % of intimal cells) (Fig. 4). Both HIF-1α and VEGF expressions showed a significant positive correlation with neovessel density in the intima (r = 0.81, P < 0.01 and r = 0.89, P < 0.01, respectively). Colocalization of HIF-1α, VEGF, and RAM-11 signals was confirmed by immunofluorescence triple labeling identifying macrophages as a source of intimal HIF-1α and VEGF (Fig. 4). Dietary lipid reduction practically abolished the expression of HIF-1α and VEGF in the intima and diminished macrophage numbers (Fig. 4). Western blotting also showed a strong reduction in the amount of HIF-1α and VEGF protein in the atherosclerotic aorta of rabbits treated with dietary lipid reduction compared to animals on continued HC diet (Fig. 4).
Effect of dietary lipid lowering on in vivo angiogenesis in experimental atherosclerosis. a–l Representative pictures of the effect of dietary lipid lowering on intimal neovascularization in a rabbit atherosclerosis model (a–d arteries of animals with high-lipid diet; i–l arteries of animals on low-lipid diet). With increasing magnification, the extent of neovascularization (arrows) especially in shoulder areas (asterisk) of large and foam cell-rich atherosclerotic lesions of animals with hyperlipidemia becomes visible on serial sections stained with Masson Trichrome and vWF antibody (a–d). In contrast, after normalization of serum lipids, the microvascular structures are nearly completely absent from a largely fibrotic intima and vWF immunostaining is only seen at the luminal endothelial layer (i–l). m Bar graphs comparing neovessel content (percent intimal area covered with neovessels) and neovessel density (intimal neovessels per square millimeter) with high- vs. low-lipid diet. Hyperlipidemia resulted in strikingly enhanced neovascularization compared to animals with normolipidemic conditions (independent sample t test, P < 0.01; error bars ± SEM). f–g High power magnification showing double immunofluorescence labeling for CD31 (f) and for vWF (g) with significant overlay (h) of both signals confirming the endothelial lining of microvascular structures of hyperlipidemic animals
Effect of dietary lipid lowering on in vivo macrophage expression of HIF-1α and VEGF in experimental atherosclerosis. Representative pictures of the effect of dietary lipid lowering on the expression of HIF-1α and VEGF in macrophages in a rabbit atherosclerosis model (a–h arteries of animals with continued high-lipid diet; i–o arteries of animals on low-lipid diet). a–h Nuclear HIF-1α (a, e) and cytoplasmic VEGF (c, g) expressions (arrows) are both located in intimal areas (ni) with a strong macrophage presence as indicated by RAM-11 immunostaining (b, f) (arrows) in atheroma of rabbits on high-lipid diet. i–o In atheroma of rabbits on low-lipid diet, HIF-1α (i, m) and VEGF (k, o) were nearly absent and only a few macrophages labeled by RAM-11 could be found (j, n). l Bar graph comparing the percentage of intimal cells expressing HIF-1α, VEGF, and RAM-11 in atheroma of rabbits on high- vs. low-lipid diet (independent sample t test, P < 0.01; error bars indicate ± SEM). p–t High power magnification showing triple immunofluorescence labeling for HIF-1α blue (q) (note the nuclear staining pattern also seen by conventional peroxidase labeling as shown in a), for VEGF in red (r) and for macrophages in green (s) with significant overlay (t) of all three signals in foam cell-rich intima of hyperlipidemic animals. u, v Arterial protein analysis using Western blot shows a strong reduction in the amount of HIF-1α(u) and VEGF (v) protein as a result of dietary lipid normalization with low-lipid diet (lanes C and D) compared to continued high-lipid diet (lanes A and B). Beta-actin is shown as a loading control
Discussion
Overall, our observations suggest a strong proangiogenic effect of oxLDL, which is transmitted by monocyte–macrophages and involves HIF-1α activation. Initially, using in vitro conditions, we described that oxLDL upregulates HIF-1α transcriptional activity and VEGF expression in monocyte–macrophages in a hypoxia-independent manner, confirming data by Shartov et al. [24]. In essence, oxLDL converted ordinary monocytes, at least in part via HIF-1α activation, into VEGF-enriched cells with possible potent proangiogenic potential. The antioxidant tiron significantly blunted the increase in HIF-1α transcriptional activity after oxLDL treatment, suggesting oxidative stress-mediated oxLDL effects.
The effect of oxLDL on HIF-1α and VEGF expression in monocyte–macrophages was comparable to the effect of hypoxia. Hypoxia-induced VEGF expression in monocytes—via the HIF-1α pathway—has been established by several groups [12,15,29]. However, the physiologic relevance of hypoxia as the main cause for increased angiogenic activitity in atherosclerotic plaque remains controversial. This is partly due to methodological difficulties in assessing tissue hypoxia in vivo and ex vivo [16]. In addition, evidence is mounting that oxidative stressors, in addition to hypoxia, are key contributors to angiogenesis in atherosclerosis [16,20–23]. These recent data also would better explain prior observations attributing differing degrees of neovascularization rather to differences in atherosclerotic lesion composition (especially lipid content) than to lesion size and oxygen diffusion distances alone [3].
To determine if monocyte–macrophages exposed to oxLDL can exert the postulated proangiogenic effect on endothelial cells, we devised a monocyte–macrophage/endothelial cell co-culture assay on growth factor-depleted Matrigel. In this system, endothelial tube formation was very low at baseline, and exposure of endothelial cells to oxLDL in the absence of monocytes did not enhance endothelial tube formation. However, when endothelial cells and monocyte–macrophages together were exposed to oxLDL, a dramatic increase in endothelial tube formation was observed. This indicates to us the induction of a truly functional proangiogenic monocyte–macrophage phenotype by oxLDL.
Our data showing strong proangiogenic effects of oxLDL in the monocyte–macrophage/endothelial cell co-culture system stand in contrast to previous data showing the inhibition of VEGF-mediated angiogenesis by oxLDL via decreased Akt phosphorylation in endothelial cells and in endothelial progenitor cells [30–32]. In recent years, evidence of complex and angiogenesis enhancing interactions between macrophages and endothelial cells has been increasing. Activated macrophages secrete a multitude of growth factors and inflammatory cytokines that can stimulate the activation and proliferation of endothelial cells. These include several proangiogenic mediators beyond the VEGF family such as interleukin-1β, TNFα, and basic fibroblast growth factor [33]. In addition, macrophages have been shown to release molecules guiding angiogenesis, like semaphorins [34]. Recent findings also indicate that macrophages secrete microvesicles, which are capable of modulating endothelial cell biology [35]. This set of tools allowing communication between macrophages and endothelial cells is likely involved in our co-culture system, making it very plausible, that activating signals from oxLDL-treated macrophages outweigh any direct inhibitory effects of oxLDL on the nearby endothelial cells. Further studies are needed to determine the contribution of the individual pathways involved beyond the activation of HIF-1α and VEGF expression reported in our study.
In this context of divergent data on the effect of oxLDL on angiogenesis, recent in vitro data also suggested direct proangiogenic effects of oxLDL, but only when given at a very low concentration (5 μg/ml) [36]. In our hands, oxLDL at a higher concentration (20 μg/ml) was not proangiogenic per se but required the presence of monocyte–macrophages to exert its angiogenic effect on HUVECs. This observation is relevant for the physiology of atherosclerosis, where the presence of macrophages is closely linked to plaque progression. The ability of oxLDL to convert monocyte–macrophages into cells with strong proangiogenic properties is, at least in part, mediated by the HIF-1α pathway, since co-treating oxLDL-treated endothelial cells and macrophages with the HIF-1α inhibitor chetomin suppressed endothelial tube formation.
To test the relevance of these in vitro findings for the possible in vivo proangiogenic potential of oxLDL, we applied a similar experimental design to the well-established Matrigel plug assay [37]. Under in vivo conditions, oxLDL again showed strong proangiogenic effects compared to growth factor-depleted Matrigel (Fig. 2). To our knowledge, this is the first evidence of a direct proangiogenic effect of oxLDL in vivo. The extent and quality of neovascular networks observed with oxLDL treatment closely matched those seen in VEGF-treated Matrigel plugs. When quantified by Hgb content measurements, the amount of oxLDL-induced angiogenesis even surpassed VEGF-induced angiogenesis (Fig. 2). Of note, also in vivo, the proangiogenic effect of oxLDL was blunted by the HIF-1a inhibitor chetomin. The addition of chetomin to VEGF-treated Matrigel did not show inhibitory effects pointing to HIF-1α activation as a prerequisite unique to oxLDL-mediated angiogenesis.
Dietary lipid lowering is an approach that has been effectively used to lower oxLDL levels in humans and different animal models [38–41]. To test for a possible lipid-mediated modulation of HIF-1α and VEGF expression in atherosclerosis, we performed dietary lipid lowering in the rabbit atherosclerosis model. This approach avoids confounding effects of the postulated “pleiotropic effects” of lipid-lowering drugs [42]. Six months of regular chow diet resulted in a dramatic reduction in intimal neovascularization, which was paralleled by a strong concomitant reduction of HIF-1α and VEGF expression, in pre-established atherosclerotic lesions (Figs. 3 and 4). In contrast, continued hyperlipidemia resulted in high expression of HIF-1α and VEGF in macrophages closely correlating with the further increase in intimal neovascularization (Fig. 3) in the pre-established lesions. Colocalization of HIF-1α and VEGF in RAM-11-positive macrophages was observed by immunofluorescence triple labeling (Fig. 4). The decrease in macrophage HIF-1α and VEGF expression with dietary lipid lowering was complemented by a strong reduction in the amount of aortic HIF-1α and VEGF protein as seen by Western blotting.
Taken together, oxLDL seems to serve as a critical link between lipids, inflammation, and angiogenesis in atherosclerosis. The proangiogenic effect of oxLDL is not possible without the presence of macrophages and, at least in part, depends on the induction of HIF-1α transcriptional activity converting monocyte–macrophages into potent proangiogenic cells. This mechanism could be underlying the previously reported ability of oxLDL to be a marker of atherosclerosis progression in patients with CAD and its suggested possible prognostic significance [43–45]. Conversely, any intervention reducing oxLDL, such as dietary lipid lowering or other lifestyle changes, might reduce not only inflammation but also intraplaque angiogenic activity. Future therapeutic modulation of angiogenesis in atherosclerosis should selectively target the conversion of monocyte–macrophages into the proangiogenic phenotype and, thus, the main source of local VEGF, rather than systemically block this growth factor, which is of great physiological importance to maintain luminal endothelial integrity in the vascular system.
References
Burke, A. P., Farb, A., Malcom, G. T., Liang, Y. H., Smialek, J., & Virmani, R. (1997). Coronary risk factors and plaque morphology in men with coronary disease who died suddenly. The New England Journal of Medicine, 336(18), 1276–1282. doi:10.1056/NEJM199705013361802.
Michel, J. B., Virmani, R., Arbustini, E., & Pasterkamp, G. (2011). Intraplaque haemorrhages as the trigger of plaque vulnerability. European Heart Journal, 32(16), 1977–1985. doi:10.1093/eurheartj/ehr054. 1985a, 1985b, 1985c.
Moreno, P. R., Purushothaman, K. R., Sirol, M., Levy, A. P., & Fuster, V. (2006). Neovascularization in human atherosclerosis. Circulation, 113(18), 2245–2252. doi:10.1161/CIRCULATIONAHA.105.578955.
Moreno, P. R., Sanz, J., & Fuster, V. (2009). Promoting mechanisms of vascular health: circulating progenitor cells, angiogenesis, and reverse cholesterol transport. Journal of the American College of Cardiology, 53(25), 2315–2323. doi:10.1016/j.jacc.2009.02.057.
Moulton, K. S., Vakili, K., Zurakowski, D., Soliman, M., Butterfield, C., Sylvin, E., et al. (2003). Inhibition of plaque neovascularization reduces macrophage accumulation and progression of advanced atherosclerosis. Proceedings of the National Academy of Sciences of the United States of America, 100(8), 4736–4741. doi:10.1073/pnas.0730843100.
Groszek, E., & Grundy, S. M. (1980). The possible role of the arterial microcirculation in the pathogenesis of atherosclerosis. Journal of Chronic Diseases, 33(11–12), 679–684.
Hutter, R., Valdiviezo, C., Sauter, B. V., Savontaus, M., Chereshnev, I., Carrick, F. E., et al. (2004). Caspase-3 and tissue factor expression in lipid-rich plaque macrophages: evidence for apoptosis as link between inflammation and atherothrombosis. Circulation, 109(16), 2001–2008. doi:10.1161/01.CIR.0000125526.91945.AE.
Palinski, W., Rosenfeld, M. E., Yla-Herttuala, S., Gurtner, G. C., Socher, S. S., Butler, S. W., et al. (1989). Low density lipoprotein undergoes oxidative modification in vivo. Proceedings of the National Academy of Sciences of the United States of America, 86(4), 1372–1376.
Parthasarathy, S., Quinn, M. T., Schwenke, D. C., Carew, T. E., & Steinberg, D. (1989). Oxidative modification of beta-very low density lipoprotein. Potential role in monocyte recruitment and foam cell formation. Arteriosclerosis, 9(3), 398–404.
Yla-Herttuala, S., Palinski, W., Rosenfeld, M. E., Parthasarathy, S., Carew, T. E., Butler, S., et al. (1989). Evidence for the presence of oxidatively modified low density lipoprotein in atherosclerotic lesions of rabbit and man. The Journal of Clinical Investigation, 84(4), 1086–1095. doi:10.1172/JCI114271.
Vink, A., Schoneveld, A. H., Lamers, D., Houben, A. J., van der Groep, P., van Diest, P. J., et al. (2007). HIF-1 alpha expression is associated with an atheromatous inflammatory plaque phenotype and upregulated in activated macrophages. Atherosclerosis, 195(2), e69–75. doi:10.1016/j.atherosclerosis.2007.05.026.
Sluimer, J. C., Gasc, J. M., van Wanroij, J. L., Kisters, N., Groeneweg, M., Sollewijn Gelpke, M. D., et al. (2008). Hypoxia, hypoxia-inducible transcription factor, and macrophages in human atherosclerotic plaques are correlated with intraplaque angiogenesis. Journal of the American College of Cardiology, 51(13), 1258–1265. doi:10.1016/j.jacc.2007.12.025.
Kai, H., Kuwahara, F., Tokuda, K., Shibata, R., Kusaba, K., Niiyama, H., et al. (2002). Coexistence of hypercholesterolemia and hypertension impairs adventitial vascularization. Hypertension, 39(2 Pt 2), 455–459.
Karshovska, E., Zernecke, A., Sevilmis, G., Millet, A., Hristov, M., Cohen, C. D., et al. (2007). Expression of HIF-1alpha in injured arteries controls SDF-1alpha mediated neointima formation in apolipoprotein E deficient mice. Arteriosclerosis, Thrombosis, and Vascular Biology, 27(12), 2540–2547. doi:10.1161/ATVBAHA.107.151050.
Higashida, T., Kanno, H., Nakano, M., Funakoshi, K., & Yamamoto, I. (2008). Expression of hypoxia-inducible angiogenic proteins (hypoxia-inducible factor-1alpha, vascular endothelial growth factor, and E26 transformation-specific-1) and plaque hemorrhage in human carotid atherosclerosis. Journal of Neurosurgery, 109(1), 83–91. doi:10.3171/JNS/2008/109/7/0083.
Mayr, M., Sidibe, A., & Zampetaki, A. (2008). The paradox of hypoxic and oxidative stress in atherosclerosis. Journal of the American College of Cardiology, 51(13), 1266–1267. doi:10.1016/j.jacc.2008.01.005.
Bosco, M. C., Puppo, M., Blengio, F., Fraone, T., Cappello, P., Giovarelli, M., et al. (2008). Monocytes and dendritic cells in a hypoxic environment: spotlights on chemotaxis and migration. Immunobiology, 213(9–10), 733–749. doi:10.1016/j.imbio.2008.07.031.
Deguchi, J. O., Yamazaki, H., Aikawa, E., & Aikawa, M. (2009). Chronic hypoxia activates the Akt and beta-catenin pathways in human macrophages. Arteriosclerosis, Thrombosis, and Vascular Biology, 29(10), 1664–1670. doi:10.1161/ATVBAHA.109.194043.
Elbarghati, L., Murdoch, C., & Lewis, C. E. (2008). Effects of hypoxia on transcription factor expression in human monocytes and macrophages. Immunobiology, 213(9–10), 899–908. doi:10.1016/j.imbio.2008.07.016.
Poitz, D. M., Augstein, A., Weinert, S., Braun-Dullaeus, R. C., Strasser, R. H., & Schmeisser, A. (2011). OxLDL and macrophage survival: essential and oxygen-independent involvement of the Hif-pathway. Basic Research in Cardiology, 106(5), 761–772. doi:10.1007/s00395-011-0186-8.
Ribatti, D., Levi-Schaffer, F., & Kovanen, P. T. (2008). Inflammatory angiogenesis in atherogenesis—a double-edged sword. Annals of Medicine, 40(8), 606–621. doi:10.1080/07853890802186913.
West, X. Z., Malinin, N. L., Merkulova, A. A., Tischenko, M., Kerr, B. A., Borden, E. C., et al. (2010). Oxidative stress induces angiogenesis by activating TLR2 with novel endogenous ligands. Nature, 467(7318), 972–976. doi:10.1038/nature09421.
Yu, S., Wong, S. L., Lau, C. W., Huang, Y., & Yu, C. M. (2011). Oxidized LDL at low concentration promotes in-vitro angiogenesis and activates nitric oxide synthase through PI3K/Akt/eNOS pathway in human coronary artery endothelial cells. Biochemical and Biophysical Research Communications, 407(1), 44–48. doi:10.1016/j.bbrc.2011.02.096.
Shatrov, V. A., Sumbayev, V. V., Zhou, J., & Brune, B. (2003). Oxidized low-density lipoprotein (oxLDL) triggers hypoxia-inducible factor-1alpha (HIF-1alpha) accumulation via redox-dependent mechanisms. Blood, 101(12), 4847–4849. doi:10.1182/blood-2002-09-2711.
Kessler J, Hahnel A, Wichmann H, Rot S, Kappler M, Bache M, Vordermark D (2010) HIF-1alpha inhibition by siRNA or chetomin in human malignant glioma cells: effects on hypoxic radioresistance and monitoring via CA9 expression. BMC cancer 10:605. doi:10.1186/1471-2407-10-605
Bouvard, C., De Arcangelis, A., Dizier, B., Galy-Fauroux, I., Fischer, A. M., Georges-Labouesse, E., et al. (2012). Tie2-dependent knockout of alpha6 integrin subunit in mice reduces post-ischaemic angiogenesis. Cardiovascular Research. doi:10.1093/cvr/cvs153.
Corti, R., Osende, J. I., Fallon, J. T., Fuster, V., Mizsei, G., Jneid, H., et al. (2004). The selective peroxisomal proliferator-activated receptor-gamma agonist has an additive effect on plaque regression in combination with simvastatin in experimental atherosclerosis: in vivo study by high-resolution magnetic resonance imaging. Journal of the American College of Cardiology, 43(3), 464–473. doi:10.1016/j.jacc.2003.08.048.
Giannarelli, C., Cimmino, G., Connolly, T. M., Ibanez, B., Ruiz, J. M., Alique, M., et al. (2012). Synergistic effect of liver X receptor activation and simvastatin on plaque regression and stabilization: an magnetic resonance imaging study in a model of advanced atherosclerosis. European Heart Journal, 33(2), 264–273. doi:10.1093/eurheartj/ehr136.
Lewis, C., & Murdoch, C. (2005). Macrophage responses to hypoxia: implications for tumor progression and anti-cancer therapies. The American Journal of Pathology, 167(3), 627–635. doi:10.1016/S0002-9440(10)62038-X.
Chavakis, E., Dernbach, E., Hermann, C., Mondorf, U. F., Zeiher, A. M., & Dimmeler, S. (2001). Oxidized LDL inhibits vascular endothelial growth factor-induced endothelial cell migration by an inhibitory effect on the Akt/endothelial nitric oxide synthase pathway. Circulation, 103(16), 2102–2107.
Wu, Y., Wang, Q., Cheng, L., Wang, J., & Lu, G. (2009). Effect of oxidized low-density lipoprotein on survival and function of endothelial progenitor cell mediated by p38 signal pathway. Journal of Cardiovascular Pharmacology, 53(2), 151–156. doi:10.1097/FJC.0b013e318197c637.
Haddad, P., Dussault, S., Groleau, J., Turgeon, J., Maingrette, F., & Rivard, A. (2011). Nox2-derived reactive oxygen species contribute to hypercholesterolemia-induced inhibition of neovascularization: effects on endothelial progenitor cells and mature endothelial cells. Atherosclerosis, 217(2), 340–349. doi:10.1016/j.atherosclerosis.2011.03.038.
Squadrito, M. L., & De Palma, M. (2011). Macrophage regulation of tumor angiogenesis: implications for cancer therapy. Molecular Aspects of Medicine, 32(2), 123–145. doi:10.1016/j.mam.2011.04.005.
Casazza, A., Fu, X., Johansson, I., Capparuccia, L., Andersson, F., Giustacchini, A., et al. (2011). Systemic and targeted delivery of semaphorin 3A inhibits tumor angiogenesis and progression in mouse tumor models. Arteriosclerosis, Thrombosis, and Vascular Biology, 31(4), 741–749. doi:10.1161/ATVBAHA.110.211920.
Baer, C., Squadrito, M. L., Iruela-Arispe, M. L., & De Palma, M. (2013). Reciprocal interactions between endothelial cells and macrophages in angiogenic vascular niches. Experimental Cell Research. doi:10.1016/j.yexcr.2013.03.026.
Khaidakov, M., Mitra, S., Wang, X., Ding, Z., Bora, N., Lyzogubov, V., et al. (2012). Large impact of low concentration oxidized LDL on angiogenic potential of human endothelial cells: a microarray study. PloS One, 7(10), e47421. doi:10.1371/journal.pone.0047421.
Norrby, K. (2006). In vivo models of angiogenesis. Journal of Cellular and Molecular Medicine, 10(3), 588–612.
Jeanpierre, E., Le Tourneau, T., Six, I., Zawadzki, C., Van Belle, E., Ezekowitz, M. D., et al. (2003). Dietary lipid lowering modifies plaque phenotype in rabbit atheroma after angioplasty: a potential role of tissue factor. Circulation, 108(14), 1740–1745. doi:10.1161/01.CIR.0000089370.84709.51.
Srimahachota, S., Wunsuwan, R., Siritantikorn, A., Boonla, C., Chaiwongkarjohn, S., & Tosukhowong, P. (2010). Effects of lifestyle modification on oxidized LDL, reactive oxygen species production and endothelial cell viability in patients with coronary artery disease. Clinical Biochemistry, 43(10–11), 858–862. doi:10.1016/j.clinbiochem.2010.04.056.
Tonstad, S., Sundfor, T., & Seljeflot, I. (2005). Effect of lifestyle changes on atherogenic lipids and endothelial cell adhesion molecules in young adults with familial premature coronary heart disease. The American Journal of Cardiology, 95(10), 1187–1191. doi:10.1016/j.amjcard.2005.01.047.
Verhamme, P., Quarck, R., Hao, H., Knaapen, M., Dymarkowski, S., Bernar, H., et al. (2002). Dietary cholesterol withdrawal reduces vascular inflammation and induces coronary plaque stabilization in miniature pigs. Cardiovascular Research, 56(1), 135–144.
Inoue, T., Hayashi, M., Takayanagi, K., & Morooka, S. (2002). Lipid-lowering therapy with fluvastatin inhibits oxidative modification of low density lipoprotein and improves vascular endothelial function in hypercholesterolemic patients. Atherosclerosis, 160(2), 369–376.
Inoue, T., Yaguchi, I., Uchida, T., Kamishirado, H., Nakahara, S., Hayashi, T., et al. (2002). Clinical significance of the antibody against oxidized low-density lipoprotein in acute myocardial infarction. Cardiology, 98(1–2), 13–17.
Shimada, K., Mokuno, H., Matsunaga, E., Miyazaki, T., Sumiyoshi, K., Kume, A., et al. (2004). Predictive value of circulating oxidized LDL for cardiac events in type 2 diabetic patients with coronary artery disease. Diabetes Care, 27(3), 843–844.
Shimada, K., Mokuno, H., Matsunaga, E., Miyazaki, T., Sumiyoshi, K., Miyauchi, K., et al. (2004). Circulating oxidized low-density lipoprotein is an independent predictor for cardiac event in patients with coronary artery disease. Atherosclerosis, 174(2), 343–347. doi:10.1016/j.atherosclerosis.2004.01.029.
Acknowledgments
We thank Renata Hutter for her continued support.
Funding
This study was supported by NIH-Training Grant 5 T32 HL 7824-13 to Randolph Hutter.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hutter, R., Speidl, W.S., Valdiviezo, C. et al. Macrophages Transmit Potent Proangiogenic Effects of oxLDL In Vitro and In Vivo Involving HIF-1α Activation: a Novel Aspect of Angiogenesis in Atherosclerosis. J. of Cardiovasc. Trans. Res. 6, 558–569 (2013). https://doi.org/10.1007/s12265-013-9469-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-013-9469-9