Abstract
Hypertrophic cardiomyopathy (HCM) is the most common genetic cardiomyopathy with substantial heterogeneity in phenotypic expression and clinical course. Traditionally, two-dimensional echocardiography has been the easiest and most reliable technique for establishing a diagnosis of HCM. However, cardiovascular magnetic resonance (CMR) has emerged as a novel, three-dimensional tomographic imaging technique, which provides high spatial and temporal resolution images of the heart in any plane and without ionizing radiation. As a result, CMR is particularly well suited to provide detailed characterization of the HCM phenotype, including precise assessment of the location and distribution of left ventricular (LV) wall thickening. In this regard, CMR can identify hypertrophy (particularly in the anterolateral free wall and apex), not well appreciated (or underestimated) by two-dimensional echocardiography, with important implications for diagnosis. CMR can also provide detailed characterization of other myocardial structures such as the papillary muscles, which may impact on preoperative management strategies for patients who are candidates for surgical myectomy. Furthermore, CMR enables an accurate assessment of total LV mass, a robust marker of the overall extent of hypertrophy, which may have implications for risk stratification. In addition, a subgroup of HCM patients have normal LV mass (with focal hypertrophy), suggesting that a limited extent of hypertrophy is consistent with a diagnosis of HCM. Finally, following the intravenous administration of gadolinium, first-pass perfusion sequences can identify myocardial perfusion abnormalities, while late gadolinium enhancement (LGE) sequences can characterize areas of myocardial fibrosis/scarring. LGE is associated with systolic dysfunction and likelihood for ventricular tachyarrhythmias on ambulatory Holter monitoring in patients with HCM. However, the precise clinical implications of myocardial perfusion abnormalities and LGE in HCM are still uncertain; this information may have important implications with regard to identifying HCM patients at risk of sudden death and adverse LV remodeling associated with systolic dysfunction. Therefore, at present, CMR provides important information impacting on diagnosis and clinical management strategies in patients with HCM and will likely have an expanding role in the evaluation of patients with this complex disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hypertrophic cardiomyopathy (HCM) is the most common genetic cardiomyopathy and is the leading cause of sudden cardiac death in young people and a major cause of heart failure symptoms at any age [1, 2]. Traditionally, two-dimensional echocardiography has been the primary imaging modality used for the diagnosis and evaluation of patients with HCM [2–5]. However, cardiovascular magnetic resonance (CMR) has emerged as a novel, three-dimensional tomographic imaging technique, which provides high spatial and temporal resolution images of the heart, in any plane and without ionizing radiation [6–14]. As a result, CMR is a robust technique which can provide detailed characterization of the HCM phenotype [11, 13–17]. With the use of gadolinium-based contrast agents, an assessment of myocardial blood flow (MBF) can be achieved using adenosine stress CMR. Late gadolinium enhancement (LGE-CMR) sequences can provide unique information on tissue characterization, specifically the identification of myocardial fibrosis/scarring [8, 15, 16, 18–23]. As a result, CMR currently serves an important role in the evaluation of HCM patients by providing information with regard to diagnosis, morphology, and clinical course in HCM patients.
CMR and Diagnosis
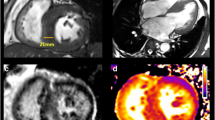
Contemporary cine CMR imaging sequences produce high spatial resolution images with sharp contrast between the myocardial border and blood pool (Fig. 1) [10, 13]. Furthermore, the left ventricular (LV) short-axis stack consists of thin myocardial slices providing complete tomographic coverage of the entire myocardium without obliquity. These particular strengths of CMR enable highly accurate wall thickness measurements in any location of the myocardium [24] and, therefore, provide a strong rationale for its use in characterizing the pattern and distribution of hypertrophy in HCM, particularly with consideration to diagnosis.
A spectrum of patterns of LV wall thickening typify the phenotypic expression in HCM. CMR end-diastolic short-axis and long-axis images demonstrate a hypertrophy involving the ventricular septum (VS), sparing the LV lateral wall (FW); b focal area of hypertrophy sharply confined to the basal anterior septum (arrows); c hypertrophy of the LV apex (asterisk); d segmental hypertrophy localized to the anterolateral LV free wall (asterisk), contiguous anterior septum is of normal thickness; e massive asymmetric hypertrophy of the anterior ventricular septum (wall thickness, 48 mm) with sparing of hypertrophy in the inferoseptum and LV lateral wall; and f diffuse hypertrophy involving most of the septal and lateral wall (reproduced with permission of Elsevier; from Maron et al. [17])
In this regard, the anterolateral LV free wall and apex are two regions of the LV myocardium in which hypertrophy may not be well visualized by traditional two-dimensional echocardiography but are reliably detected by CMR (Fig. 2) [11, 14, 17]. In a recent study, a small subset of patients suspected of having HCM were identified with segmental left ventricular hypertrophy (LVH) in the anterolateral free wall which was initially missed by echocardiography [17]. Additionally, CMR has also identified HCM patients with massive LVH (wall thickness >30 mm) localized to the anterolateral wall in whom the extent of hypertrophy in this region was substantially underestimated by two-dimensional echocardiography (i.e., the maximal wall thickness in these areas were considered to be significantly less than 30 mm). These observations illustrate one of the technical limitations related to echocardiographic imaging in which there is lateral ultrasound “dropout” of the epicardial border of the anterolateral free wall due to loss of spatial resolution in the lateral portions of the chamber in the short-axis plane, thereby obscuring differentiation from adjacent thoracic parenchyma [14, 17].
CMR can identify segmental LVH that may not be reliably visualized by two-dimensional echocardiography. a Normal two-dimensional echocardiogram in a patient with a family history of HCM. b This same patient then underwent CMR, which reveals an area of segmental hypertrophy in the anterolateral LV wall (asterisk) consistent with a diagnosis of HCM (reproduced with permission of the American Heart Association; from Rickers et al. [14]). The apex is another region of the LV in which hypertrophy may not be reliably visualized by two-dimensional echocardiography. c Echocardiography was considered nondiagnostic. d In the same patient, CMR clearly demonstrates segmental hypertrophy confined to the LV apex, consistent with a diagnosis of apical HCM
Likewise, CMR is not limited by constraints of thoracic or pulmonary parenchyma, which allows for accurate and reliable visualization of the LV apex, providing the opportunity to also identify morphologic abnormalities in this region of the myocardium. In this regard, hypertrophy confined to only the apical region can be identified by CMR in some HCM patients in whom the echocardiogram was considered normal (or nondiagnostic) [12]. Furthermore, due to its super spatial resolution in imaging the distal LV myocardium, CMR may also help clarify (and even alter) diagnosis by demonstrating the presence of prominent trabeculations (i.e., sinusoids) consistent with a diagnosis of LV noncompaction in patients initially diagnosed with apical HCM. In this regard, the LV trabeculations associated with LV noncompaction may appear as apical hypertrophy when imaged with lower spatial resolution two-dimensional echocardiography, potentially resulting in a misdiagnosis of apical HCM in these patients. This also has important implications for management strategies, as a diagnosis of LV noncompaction may have additional impact on treatment strategies (i.e., coumadin).
In addition, CMR can aid in the identification of another important subset of HCM patients who develop LV apical aneurysms [25]. This unique HCM phenotype is associated with midventricular hypertrophy with apposition of the septum and LV lateral wall, producing, in some patients, increased midcavitary systolic pressures which may be responsible for initiating a process of adverse LV remodeling associated with apical aneurysm formation. HCM patients with LV apical aneurysms have an adverse disease event rate of 11%/year (twofold greater than that of the general HCM population), including an increased risk of sudden death and thromboembolic events. Therefore, recognition of those HCM patients with LV apical aneurysm is critical, as this phenotype directly impacts management strategies, such as the recommendation of implantable cardioverter defibrillators (ICDs) for primary prevention of sudden death or anticoagulation to prevent stroke. However, just as apical hypertrophy can be missed with two-dimensional echocardiography in select HCM patients, the identification of LV apical aneurysms (particularly when small, <2 cm in maximal diameter) may also not be well appreciated by echocardiography (Fig. 3) and, therefore, CMR imaging should be strongly considered in patients in whom the LV apex is not well visualized or in whom the suspicion of an apical aneurysm is raised (i.e., patients with midventricular hypertrophy) [25].
Comparisons of echocardiography and CMR. a Two-dimensional echocardiogram at end-diastole in four-chamber view from a 32-year-old HCM patient shows normal apical contour without evidence of aneurysm formation (arrowheads). b From the same patient, two-chamber long-axis CMR image demonstrates a relatively small apical aneurysm with a thin rim (arrowheads), which was associated with regional transmural scarring on LGE images. LA left atrium, LV left ventricle, VS ventricular septum (reproduced with permission of the American Heart Association; from Maron et al. [25])
CMR and Phenotypic Expression
Pattern and Distribution of Hypertrophy
Due to its high spatial resolution and complete coverage of the entire LV myocardium with true tomographic imaging, CMR provides an accurate characterization of the pattern and distribution of LVH [10, 13, 14]. In this regard, the historical perception related to the HCM phenotype has been one of predominately massive and diffuse wall thickening [1, 4, 5]. However, in a recent large series of HCM patients who underwent CMR evaluation, approximately one half of HCM patients show areas of LVH confined to less than 50% of the overall LV chamber, including a substantial minority with particularly focal or regional areas of increased wall thickness [17]. In fact, approximately 10% of HCM patients had hypertrophied confined to only one or two LV segments. This observation with CMR supports the notion that limited hypertrophy is part of the phenotypic expression in HCM and focal wall thickening can be consistent with a clinical diagnosis of HCM.
Furthermore, increased LV wall thickness was most commonly located in the basal anterior free wall and contiguous anterior ventricular septum [17]. However, in the majority of HCM patients, hypertrophy involved both regions of the LV myocardium and, in a small but significant number of patients, the anterolateral wall was the predominate region of hypertrophy. This CMR observation that hypertrophy commonly extends from the basal anterior septum to involve the free wall has not been previously appreciated with two-dimensional echocardiography and further substantiates the ability of CMR to better characterize regions of hypertrophy which may be missed or substantially underestimated by two-dimensional echocardiography. These results, with implications on diagnosis and management strategies, support the growing role of CMR in the initial evaluation of HCM patients.
Finally, a noncontiguous pattern of LV wall thickening can be observed in a subgroup of patients with HCM [17]. In this regard, patients can demonstrate a pattern of wall thickening in which hypertrophied segments are separated by regions of nonhypertrophied myocardium, often with abrupt changes in wall thickness (Fig. 4). This type of noncontiguous pattern of hypertrophy is not observed in patients with secondary forms of hypertrophy (such as hypertensive cardiomyopathy) and, therefore, could be used to help diagnostically differentiate patients in whom the diagnosis of primary (genetic) and secondary hypertrophy is uncertain.
Right Ventricular Hypertrophy
It has previously been uncertain whether morphologic abnormalities of the right ventricle (RV) are present in patients with HCM. Due to its advantages of tomographic imaging not limited by thoracic parenchyma, CMR is a particularly robust imaging technique for evaluation of the RV. In this regard, the application of CMR in HCM has demonstrated that over one third of patients have increased RV wall thickness and mass compared to controls. In addition, a small subset of HCM patients have extreme RV hypertrophy (≥10 mm) [26]. RV hypertrophy appears to be a predominantly diffuse process involving the entire or a significant proportion of the RV wall in the majority of patients. In addition, although uncommon, LGE has been observed in the RV free wall in HCM patients, suggesting that a similar process of adverse remodeling with myocardial fibrosis (which occurs frequently in the LV in patients with HCM) can also involve the RV [26]. These observations support the concept that morphologic abnormalities of the RV are part of the HCM disease spectrum, but longitudinal investigations are required to further characterize the clinical significance of RV pathology in this disease.
Papillary Muscles
CMR also provides an opportunity to characterize the papillary muscles in HCM. In this regard, papillary muscle number and mass index are greater in HCM patients compared to controls, including a substantial minority of HCM patients with markedly increased papillary muscle mass (≥2 standard deviations above the mean for controls; Fig. 5). Furthermore, there appears to be a small subset of HCM patients in whom LV wall hypertrophy is focal and limited (with normal LV mass) but who demonstrate substantially hypertrophied papillary muscles with increased mass [18]. In such patients, the predominant morphologic expression of the disease appears to involve the papillary muscles compared to the LV wall. Furthermore, LGE (i.e., fibrosis) of only the papillary muscles has been also been observed in HCM patients. The clinical significance of LGE confined to only the papillary muscles in HCM patients is uncertain. However, myocardial scarring confined to the papillary muscles was the only abnormal finding reported in a recent case of a young HCM patient who died suddenly with no conventional risk factors for sudden death, raising the possibility that scarring in the papillary muscle may be a nidus for the generation of ventricular tachyarrhythmias [27]. Finally, CMR assessment of papillary muscles has also provided insight into the mechanism of outflow obstruction in patients with HCM by demonstrating that the presence of an apically displaced anterolateral or double bifid papillary muscle is associated with a significantly higher likelihood of having a resting LV outflow gradient [28]. Therefore, in the similar manner as the RV, the LV papillary muscles also appear be part of the cardiomyopathic process in HCM and contribute to the mechanism of outflow obstruction as well.
Papillary muscles from HCM patient at the midventricular level in end-diastole by CMR. a The papillary muscles are greatly hypertrophied with extreme increase in mass (11 g/m2); b multiple accessory papillary muscles, four in number (arrows); c increased papillary muscle mass in a patient with normal LV mass; d anteriorly displaced accessory papillary muscle that was subsequently resected (arrow) during surgical septal myectomy. LV left ventricle, RV right ventricle, VS ventricular septum (reproduced with permission of the American Journal of Cardiology; from Harrigan et al. [18])
LV Mass
CMR provides a highly accurate in vivo method of calculating total LV mass without the technical limitations and geometric assumptions that were an inherent limitation to calculating LV mass with two-dimensional echocardiography. As expected, LV mass is significantly greater in HCM patients compared to controls. However, a significant proportion (up to 20%) of HCM patients, with only focal wall thickening, will demonstrate a LV mass that is within normal limits [29]. Therefore, it is should be emphasized that a normal LV mass does not exclude a diagnosis of HCM.
Furthermore, not all HCM patients with the same maximal LV wall thickness will have similar LV mass. Mismatches between absolute LV wall thickness and mass reflect the heterogeneity with regard to distribution of mass in HCM, with more extensive hypertrophy extending from the site of maximal wall thickness in some HCM patients and not in others (Fig. 6). Short-term prospective follow-up has demonstrated that HCM patients with extreme LV mass are more likely to experience adverse cardiovascular events compared to patients with normal or minimally increased LV mass [29]. However, additional long-term prospective CMR studies with larger number of patients are needed to help clarify LV mass as a risk marker and, therefore, at present, clinical management decisions should not be made solely based on LV mass alone.
LV mass in HCM. CMR four-chamber end-diastolic images from two HCM patients with identical maximal LV wall thickness (i.e., 33 mm in the anterior ventricular septum), but markedly different LV mass index values (a 184 g/m2; b 92 g/m2). The difference in mass is due to the extensive distribution of increased LV thickness beyond the ventricular septum and into the LV lateral wall in a, while the patient in b shows hypertrophy confined to the septum. FW lateral LV wall, RV right ventricular cavity, VS ventricular septum (reproduced with permission of Elsevier; from Olivotto et al. [29])
Preclinical HCM
At present, the role of CMR in the evaluation and identification of preclinical HCM patients (genotype positive/phenotype negative) is uncertain. In one recent report, cine CMR identified a substantial number of preclinical HCM patients with crypt formations localized predominately in the inferoseptum [30]. However, further investigations are required to clarify the etiology and significance of crypt formations in this subgroup of patients. In addition, whether LGE can be identified prior to the development of LVH in preclinical patients has also not been determined. However, a recently published case report identified a young asymptomatic preclinical HCM patient with extensive and diffuse LGE throughout the LV despite an otherwise structurally normal ventricle with preserved systolic function [31].
CMR and the Assessment of Myocardial Ischemia
In patients with HCM, morphologic abnormalities of the intramural coronary arterioles represent the primary morphologic substrate for microvascular dysfunction which can lead to blunted MBF during stress (i.e., microvascular ischemia). In HCM patients, positron emission tomography (PET) studies have demonstrated blunted MBF after dipyridamole infusion, while resting MBF is similar to that of normal controls [32–34]. The identification of myocardial ischemia by PET in patients with HCM is a powerful independent predictor of cardiovascular mortality and may identify patients who are more likely to suffer progressive adverse LV remodeling including development of the end-stage phase of HCM (ejection fraction [EF] < 50%) [33, 34]. These observations support a growing role for the assessment of ischemia to identify HCM patients at risk.
In this regard, advances in CMR perfusion sequences now permit accurate qualitative and quantitative assessment of MBF at rest and during pharmacologic stress (typically adenosine) and with superior spatial resolution to PET. Similar to PET, stress CMR has also demonstrated blunted MBF in response to vasodilator stress in patients with HCM [35]. Reduction in MBF appears greatest in the subendocardium compared to the subepicardial layer and is present in both hypertrophied and nonhypertrophied segments. However, an association is present between the degree of abnormal perfusion and magnitude of wall thickness, with the thickest segments demonstrating the greatest reduction MBF. As greater magnitudes of wall thickness increase sudden death risk in HCM, these observations suggest that myocardial ischemia may provide an important pathophysiologic explanation for this increase in risk [35]. As stress CMR for the assessment of active ischemia is an evolving area, only a few CMR centers currently have the expertise to perform this imaging. As a result, there are currently no data relating CMR-derived measures of myocardial ischemia to clinical outcome. Therefore, for those HCM patients without access to a CMR center that routinely performs stress imaging, PET for the clinical assessment of MBF could also be considered.
However, CMR studies have begun to provide insight into the pathophysiology of HCM. In this regard, areas of myocardium with reduced MBF are often present in segments associated with fibrosis (as determined by contrast-enhanced CMR) [35]. MBF is also substantially reduced in LV segments situated adjacent to myocardial fibrosis [36]. In addition, in HCM patients undergoing surgical myectomy, the degree of abnormal intramural coronary arterioles has been correlated with extent of septal scarring on contrast-enhanced CMR [37]. The totality of these observations suggest an association between ischemia and myocardial fibrosis, providing further support for the principle that abnormal MBF due to microvascular dysfunction is responsible for myocardial ischemia-mediated myocyte death and, ultimately, repair in the form of replacement fibrosis.
Contrast-Enhanced CMR for Identification of Myocardial Fibrosis
After a delay of approximately 10 min following the intravenous administration of gadolinium, contrast-enhanced CMR sequences can be used to detect areas of abnormal myocardium where gadolinium has accumulated [6, 7, 9, 10, 13, 38–40]. Gadolinium will temporarily redistribute in areas of the myocardium with expanded extracellular space which are represented on LGE-CMR sequences as bright or “hyperenhanced” regions (Fig. 7). Areas of LGE can be planimetered and the amount quantified and expressed as a percentage of the total LV mass. Selected reports in native hearts following transplantation of patients with end-stage HCM have demonstrated concordance between in vivo LGE-CMR images and gross and histopathologic evidence of fibrosis. These studies suggest that LGE in such patients are specific to areas of myocardial scarring, rather than other histopathology, such as myocyte disarray.
LGE in HCM. a Focal area (arrow) of LGE at right ventricular (RV) insertion with anterior (big arrow) and posterior (small arrow) portion of septum (VS). b Focal area of subepicardial LGE in the inferior wall (arrows). c Predominate transmural LGE in basal anterior septum extending into anterior free wall (arrows)
Approximately 50–80% of HCM patients demonstrate LGE, occupying on average 10% of the overall LV myocardial volume [12, 16, 22]. Importantly, virtually any pattern, distribution, and location of LGE can be observed in HCM. However, as opposed to coronary artery disease, the pattern of LGE in HCM does not typically correspond to a coronary vascular distribution. There is an association between hypertrophy and LGE, as LGE is more common in LV wall segments which are thick and HCM patients with LGE have greater maximal LV wall thickness and LV mass index than patients without LGE [12, 16, 22]. LGE is most commonly located in both ventricular septum and lateral wall but can be confined, less commonly, to the lateral wall, septum, the area of right ventricular insertion into ventricular septum, and LV apex [16].
The precise clinical implications related to LGE in HCM are largely unresolved. Nevertheless, several cross-sectional studies have demonstrated a relationship between the amount of LGE and LV EF [12, 16, 22]. In this regard, HCM patients with EF ≤50% (i.e., end-stage phase) have significantly greater %LGE than those with low–normal (EF 50–65%) or normal systolic function (>65%; Fig. 8). However, HCM patients with low–normal systolic function often have an amount of LGE which overlaps substantially with those patients in the end-stage. Although it still remains uncertain whether the amount of LGE can be used to identify HCM patients who may be at risk of developing the end-stage phase, this observation suggests it remains possible that HCM patients with low–normal EF may represent a transition phase that could be a marker for subsequent evolution to the end-stage phase of HCM. This observation may have important implications for clinical management since earlier anticipation of evolution into the end-stage may alert clinicians to consider alteration in therapeutic strategies: including closer surveillance to detect further changes in systolic function and morphologic remodeling as well as transitioning medical therapy to antiremodeling agents such as ACE inhibitors or aldosterone blocker, consideration of primary prevention ICD therapy as a bridge to transplant and evaluation for heart transplantation.
Relation of delayed enhancement to LV systolic function. Comparison of percent delayed enhancement of LV in HCM patients with EF ≤50%, 51–59%, and ≥60% (reproduced with permission of the American Heart Association; from Maron et al. [16])
Although there appears to be a statistically significant (although weak) relationship between LGE and heart failure symptoms, a substantial number of asymptomatic HCM patients (with preserved EF) also demonstrate extensive amount of LGE [16]. Many of these HCM patients with LGE have achieved advanced ages without adverse disease consequences such as progressive heart failure symptoms or arrhythmic events. This observation substantiate the concept that adverse disease consequences in HCM is a complex process related to a number of important aspects of disease pathophysiology and that fibrosis may not be the predominate determinant of adverse prognosis in all patients. Nevertheless, given the totality of the data relating to LGE in HCM, it would still seem reasonable at this time for HCM patients with LGE to undergo regular clinical surveillance for prospective detection of changes in symptoms and LV remodeling.
As contrast-enhanced CMR can identify the abnormal myocardial substrate of fibrosis, it is not unreasonable to consider whether LGE could serve as a novel marker for the identification of HCM patients at risk of sudden death. In this regard, LGE has been associated with ventricular tachyarrhythmias (including rapid ventricular tachycardia) on ambulatory 24-h Holter electrocardiography (ECG; Fig. 9) [21, 41]. Currently, it remains uncertain whether the extent of LGE provides a more robust predictor of increased risk of ventricular arrhythmias compared to the presence of LGE alone. However, the extent of LGE is greater in HCM patients with multiple conventional risk factors for sudden death [12]. These cross-sectional studies suggest that contrast-enhanced CMR may define the unstable arrhythmogenic substrate in HCM. However, recent prospective (short-term) outcome data obtained over an average of 2 years shows a nonstatistically significant trend toward an increased adverse cardiovascular event rate in those HCM patients with LGE [16]. Therefore, at the present time, it remains uncertain as to whether the identification of LGE by contrast-enhanced CMR identifies HCM patients at risk of adverse consequences such as sudden death. In this regard, it would be premature at this early juncture to make management decisions about ICD therapy for primary prevention solely based on the results of the CMR study. In this regard, future studies with greater number of HCM patients studied with contrast-enhanced CMR with longer follow-up are required in this low event rate disease to help clarify if LGE is an independent risk factor of sudden death in HCM.
Relation between delayed enhancement and ventricular tachyarrhythmias. Prevalence of arrhythmias on 24-h ambulatory Holter ECG with respect to presence or absence of delayed enhancement in HCM patients (reproduced with permission of Elsevier; from Adabag et al. [21])
CMR and Invasive Septal Reduction Therapy
Surgical Septal Myectomy
HCM patients with advanced heart failure symptoms refractory to medical therapy and a LV outflow gradient ≥50 mmHg at rest (or with exercise) are candidates for invasive septal reduction therapy (i.e., surgical myectomy or alcohol septal ablation [ASA]) to relieve outflow obstruction and improve limiting symptoms [1, 2]. Surgical myectomy is considered the “gold standard” for the treatment of outflow obstruction and is performed through an aortotomy and a total of 3–12 g of septal muscle is removed in order to widen the outflow diameter and eliminate the abnormal hemodynamic forces which contribute to obstruction. In addition, abnormalities of the mitral valve or subvalvular apparatus are often repaired during the operation in order to provide optimal relief of gradients. In this regard, submitral structures including anteriorly displaced accessory papillary muscles judged to contribute substantially to LV outflow tract obstruction (by virtually tethering the anterior leaflet of the mitral valve toward the septum) are often resected as part of the septal myectomy [28]. In those HCM patients who are candidates for surgical myectomy, CMR can identify accessory papillary muscles which are thought to be contributing to obstruction and require resection for optimal relief of outflow gradients and, therefore, CMR may be useful to guide preoperative surgical planning.
Alcohol Septal Ablation
An alternative to surgical myectomy is ASA. In this percutaneous procedure, 1–2 ml of alcohol is injected into an anatomically appropriate septal perforator artery supplying the basal septum (at the point of SAM–septal contact) inducing a myocardial infarction and resulting in septal thinning, widening of the LV outflow area, and ultimately, elimination of outflow obstruction [2]. Contrast-enhanced CMR has demonstrated that ASA produces a myocardial infarction of significant size, totaling on average 10% of total LV mass [42]. In addition, CMR has provided additional insight into the differing effects on septal morphology of both ASA and surgical myectomy. In this regard, surgical myectomy invariably results in resected muscle from the basal anterior septum. However, ASA has a more variable effect in which tissue necrosis is often transmural in extent and located more posterior and inferiorly in the septum compared to surgery and can even involve the RV portion of the inferior septum at the mid-LV level. The finding that ASA can produce myocardial necrosis more inferiorly in the basal septum (and, therefore, distal to the point of SAM–septal contact) likely explains the higher residual gradients found after this procedure compared to surgery [42]. In such circumstances, CMR can also show persistent LV outflow obstruction. These CMR-derived observations may ultimately impact on patient selection issues for those who are candidates for invasive septal reduction therapy.
Limitations of CMR
There are several practical limitations which should be considered with regard to applying CMR to routine clinical cardiology practice. In this regard, one of the most important contraindications to CMR imaging includes previous implantation of device therapy, such as pacemakers and ICDs. This is particularly important, as a small but important number of HCM patients may require ICD therapy for either primary or secondary prevention of sudden death and, therefore, CMR may not be applicable for the initial or follow-up evaluation of some patients. In addition, other contraindications to CMR include renal failure (only with the use of gadolinium), ocular implants, vascular clips (for aneurysm repairs), and claustrophobia, although practically these limitations will apply to only a very small number of patients. In addition, the cost–benefit ratio for the use of CMR in a patient population such as HCM remains uncertain. Future clinical investigations will help further clarify the role of CMR in the diagnosis of HCM, as well as its value in improving risk stratification strategies, providing an opportunity to better appreciate the cost effectiveness of this technique in the routine evaluation of patients with HCM.
Conclusions
In conclusion, CMR is an important addition to the imaging armamentarium for HCM. As a comprehensive tomographic technique with high spatial resolution, CMR provides complete reconstruction of the LV chamber and a precise definition of the distribution and pattern of hypertrophy. In this regard, CMR can identify areas of hypertrophy in the LV that are not visualized (or are under-recognized) by two-dimensional echocardiography and, therefore, represents an important tool in the noninvasive diagnosis of HCM. The opportunity to accurately calculate LV mass provides an opportunity for CMR to provide a more robust measure of hypertrophy, with future implications for risk stratification strategies. The unique ability of CMR to characterize the abnormal myocardial substrate of fibrosis (as well as myocardial ischemia) may eventually aid in identifying HCM patients at risk of sudden death as well as disease progression. Taken together, these observations underscore an important and expanding role for CMR in the contemporary evaluation of patients with HCM.
References
Maron, B. J. (2002). Hypertrophic cardiomyopathy: A systematic review. JAMA, 287(10), 1308–1320.
Maron, B. J., McKenna, W. J., Danielson, G. K., Kappenberger, L. J., Kuhn, H. J., Seidman, C. E., et al. (2003). American College of Cardiology/European Society of Cardiology clinical expert consensus document on hypertrophic cardiomyopathy. A report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the European Society of Cardiology Committee for Practice Guidelines. Journal of the American College of Cardiology, 42(9), 1687–1713.
Wigle, E. D., Rakowski, H., Kimball, B. P., & Williams, W. G. (1995). Hypertrophic cardiomyopathy. Clinical spectrum and treatment. Circulation, 92(7), 1680–1692.
Shapiro, L. M., & McKenna, W. J. (1983). Distribution of left ventricular hypertrophy in hypertrophic cardiomyopathy: A two-dimensional echocardiographic study. Journal of the American College of Cardiology, 2(3), 437–444.
Wigle, E. D., Sasson, Z., Henderson, M. A., Ruddy, T. D., Fulop, J., Rakowski, H., et al. (1985). Hypertrophic cardiomyopathy. The importance of the site and the extent of hypertrophy. A review. Progress in Cardiovascular Diseases, 28(1), 1–83.
Judd, R. M., Lugo-Olivieri, C. H., Arai, M., Kondo, T., Croisille, P., Lima, J. A., et al. (1995). Physiological basis of myocardial contrast enhancement in fast magnetic resonance images of 2-day-old reperfused canine infarcts. Circulation, 92(7), 1902–1910.
Kim, R. J., Fieno, D. S., Parrish, T. B., Harris, K., Chen, E. L., Simonetti, O., et al. (1999). Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation, 100(19), 1992–2002.
Kim, R. J., & Judd, R. M. (2003). Gadolinium-enhanced magnetic resonance imaging in hypertrophic cardiomyopathy: In vivo imaging of the pathologic substrate for premature cardiac death? Journal of the American College of Cardiology, 41(9), 1568–1572.
Kim, R. J., Wu, E., Rafael, A., Chen, E. L., Parker, M. A., Simonetti, O., et al. (2000). The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. New England Journal of Medicine, 343(20), 1445–1453.
Lima, J. A., & Desai, M. Y. (2004). Cardiovascular magnetic resonance imaging: Current and emerging applications. Journal of the American College of Cardiology, 44(6), 1164–1171.
Moon, J. C., Fisher, N. G., McKenna, W. J., & Pennell, D. J. (2004). Detection of apical hypertrophic cardiomyopathy by cardiovascular magnetic resonance in patients with non-diagnostic echocardiography. Heart, 90(6), 645–649.
Moon, J. C., McKenna, W. J., McCrohon, J. A., Elliott, P. M., Smith, G. C., & Pennell, D. J. (2003). Toward clinical risk assessment in hypertrophic cardiomyopathy with gadolinium cardiovascular magnetic resonance. Journal of the American College of Cardiology, 41(9), 1561–1567.
Pennell, D. J. (2003). Cardiovascular magnetic resonance: Twenty-first century solutions in cardiology. Clinical Medicine, 3(3), 273–278.
Rickers, C., Wilke, N. M., Jerosch-Herold, M., Casey, S. A., Panse, P., Panse, N., et al. (2005). Utility of cardiac magnetic resonance imaging in the diagnosis of hypertrophic cardiomyopathy. Circulation, 112(6), 855–861.
Rochitte, C. E., Tassi, E. M., & Shiozaki, A. A. (2006). The emerging role of MRI in the diagnosis and management of cardiomyopathies. Current Cardiology Reports, 8(1), 44–52.
Maron MS AE, H. C., Buros, J., Gibson, C. M., Hanna, C., Lesser, J. R., Udelson, J. E., et al. (2008). Clinical profile and significance of delayed enhancement in hypertrophic cardiomyopathy. Circulation: Heart Failure, 2008(1), 184–191.
Maron, M. S., Maron, B. J., Harrigan, C., Buros, J., Gibson, C. M., Olivotto, I., et al. (2009). Hypertrophic cardiomyopathy phenotype revisited after 50 years with cardiovascular magnetic resonance. Journal of the American College of Cardiology, 54(3), 220–228.
Harrigan, C. J., Appelbaum, E., Maron, B. J., Buros, J. L., Gibson, C. M., Lesser, J. R., et al. (2008). Significance of papillary muscle abnormalities identified by cardiovascular magnetic resonance in hypertrophic cardiomyopathy. American Journal of Cardiology, 101(5), 668–673.
Harris, K. M., Spirito, P., Maron, M. S., Zenovich, A. G., Formisano, F., Lesser, J. R., et al. (2006). Prevalence, clinical profile, and significance of left ventricular remodeling in the end-stage phase of hypertrophic cardiomyopathy. Circulation, 114(3), 216–225.
Moon, J. C., Reed, E., Sheppard, M. N., Elkington, A. G., Ho, S. Y., Burke, M., et al. (2004). The histologic basis of late gadolinium enhancement cardiovascular magnetic resonance in hypertrophic cardiomyopathy. Journal of the American College of Cardiology, 43(12), 2260–2264.
Adabag, A. S., Maron, B. J., Appelbaum, E., Harrigan, C. J., Buros, J. L., Gibson, C. M., et al. (2008). Occurrence and frequency of arrhythmias in hypertrophic cardiomyopathy in relation to delayed enhancement on cardiovascular magnetic resonance. Journal of the American College of Cardiology, 51(14), 1369–1374.
Choudhury, L., Mahrholdt, H., Wagner, A., Choi, K. M., Elliott, M. D., Klocke, F. J., et al. (2002). Myocardial scarring in asymptomatic or mildly symptomatic patients with hypertrophic cardiomyopathy. Journal of the American College of Cardiology, 40(12), 2156–2164.
Kramer, C. M. (2006). The expanding prognostic role of late gadolinium enhanced cardiac magnetic resonance. Journal of the American College of Cardiology, 48(10), 1986–1987.
Grothues, F., Smith, G. C., Moon, J. C., Bellenger, N. G., Collins, P., Klein, H. U., et al. (2002). Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. American Journal of Cardiology, 90(1), 29–34.
Maron, M. S., Finley, J. J., Bos, J. M., Hauser, T. H., Manning, W. J., Haas, T. S., et al. (2008). Prevalence, clinical significance, and natural history of left ventricular apical aneurysms in hypertrophic cardiomyopathy. Circulation, 118(15), 1541–1549.
Maron, M. S., Hauser, T. H., Dubrow, E., Horst, T. A., Kissinger, K. V., Udelson, J. E., et al. (2007). Right ventricular involvement in hypertrophic cardiomyopathy. American Journal of Cardiology, 100(8), 1293–1298.
Maron, B. J., Maron, M. S., Lesser, J. R., Hauser, R. G., Haas, T. S., Harrigan, C. J., et al. (2008). Sudden cardiac arrest in hypertrophic cardiomyopathy in the absence of conventional criteria for high risk status. American Journal of Cardiology, 101(4), 544–547.
Kwon, D. H., Setser, R. M., Thamilarasan, M., Popovic, Z. V., Smedira, N. G., Schoenhagen, P., et al. (2008). Abnormal papillary muscle morphology is independently associated with increased left ventricular outflow tract obstruction in hypertrophic cardiomyopathy. Heart (British Cardiac Society), 94(10), 1295–1301.
Olivotto, I., Maron, M. S., Autore, C., Lesser, J. R., Rega, L., Casolo, G., et al. (2008). Assessment and significance of left ventricular mass by cardiovascular magnetic resonance in hypertrophic cardiomyopathy. Journal of the American College of Cardiology, 52(7), 559–566.
Germans, T., Wilde, A. A., Dijkmans, P. A., Chai, W., Kamp, O., Pinto, Y. M., et al. (2006). Structural abnormalities of the inferoseptal left ventricular wall detected by cardiac magnetic resonance imaging in carriers of hypertrophic cardiomyopathy mutations. Journal of the American College of Cardiology, 48(12), 2518–2523.
Strijack, B., Ariyarajah, V., Soni, R., Jassal, D. S., Greenberg, C. R., McGregor, R., et al. (2008). Late gadolinium enhancement cardiovascular magnetic resonance in genotyped hypertrophic cardiomyopathy with normal phenotype. Journal of Cardiovascular Magnetic Resonance, 10(1), 58.
Camici, P., Chiriatti, G., Lorenzoni, R., Bellina, R. C., Gistri, R., Italiani, G., et al. (1991). Coronary vasodilation is impaired in both hypertrophied and nonhypertrophied myocardium of patients with hypertrophic cardiomyopathy: a study with nitrogen-13 ammonia and positron emission tomography. Journal of the American College of Cardiology, 17(4), 879–886.
Cecchi, F., Olivotto, I., Gistri, R., Lorenzoni, R., Chiriatti, G., & Camici, P. G. (2003). Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. New England Journal of Medicine, 349(11), 1027–1035.
Olivotto, I., Cecchi, F., Gistri, R., Lorenzoni, R., Chiriatti, G., Girolami, F., et al. (2006). Relevance of coronary microvascular flow impairment to long-term remodeling and systolic dysfunction in hypertrophic cardiomyopathy. Journal of the American College of Cardiology, 47(5), 1043–1048.
Petersen, S. E., Jerosch-Herold, M., Hudsmith, L. E., Robson, M. D., Francis, J. M., Doll, H. A., et al. (2007). Evidence for microvascular dysfunction in hypertrophic cardiomyopathy: New insights from multiparametric magnetic resonance imaging. Circulation, 115(18), 2418–2425.
Sotgia, B., Sciagra, R., Olivotto, I., Casolo, G., Rega, L., Betti, I., et al. (2008). Spatial relationship between coronary microvascular dysfunction and delayed contrast enhancement in patients with hypertrophic cardiomyopathy. Journal of Nuclear Medicine, 49(7), 1090–1096.
Kwon, D. H., Smedira, N. G., Rodriguez, E. R., Tan, C., Setser, R., Thamilarasan, M., et al. (2009). Cardiac magnetic resonance detection of myocardial scarring in hypertrophic cardiomyopathy: Correlation with histopathology and prevalence of ventricular tachycardia. Journal of the American College of Cardiology, 54(3), 242–249.
Fieno, D. S., Kim, R. J., Chen, E. L., Lomasney, J. W., Klocke, F. J., & Judd, R. M. (2000). Contrast-enhanced magnetic resonance imaging of myocardium at risk: Distinction between reversible and irreversible injury throughout infarct healing. Journal of the American College of Cardiology, 36(6), 1985–1991.
Simonetti, O. P., Kim, R. J., Fieno, D. S., Hillenbrand, H. B., Wu, E., Bundy, J. M., et al. (2001). An improved MR imaging technique for the visualization of myocardial infarction. Radiology, 218(1), 215–223.
Wilson, J. M., Villareal, R. P., Hariharan, R., Massumi, A., Muthupillai, R., & Flamm, S. D. (2002). Magnetic resonance imaging of myocardial fibrosis in hypertrophic cardiomyopathy. Texas Heart Institute Journal, 29(3), 176–180.
Kwon, D. H., Setser, R. M., Popovic, Z. B., Thamilarasan, M., Sola, S., Schoenhagen, P., et al. (2008). Association of myocardial fibrosis, electrocardiography and ventricular tachyarrhythmia in hypertrophic cardiomyopathy: A delayed contrast enhanced MRI study. The International Journal of Cardiovascular Imaging, 24(6), 617–625.
Valeti, U. S., Nishimura, R. A., Holmes, D. R., Araoz, P. A., Glockner, J. F., Breen, J. F., et al. (2007). Comparison of surgical septal myectomy and alcohol septal ablation with cardiac magnetic resonance imaging in patients with hypertrophic obstructive cardiomyopathy. Journal of the American College of Cardiology, 49(3), 350–357.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maron, M.S. The Current and Emerging Role of Cardiovascular Magnetic Resonance Imaging in Hypertrophic Cardiomyopathy. J. of Cardiovasc. Trans. Res. 2, 415–425 (2009). https://doi.org/10.1007/s12265-009-9136-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-009-9136-3