Abstract
Cardiovascular genetic medicine is devoted to the identification and understanding of cardiac conditions resulting from genetic and genomic mechanisms and to the development and validation of diagnostic and treatment algorithms and guidelines. Cardiovascular genetic medicine clinics now provide expert cardiovascular subspecialty care, genetic counseling and clinical genetic testing, and will eventually provide disease-specific gene or genetic therapies. Currently, the most tractable diagnoses for cardiovascular genetic medicine are the single-gene disorders: the cardiomyopathies, the channelopathies, and others. The recent explosion of genetic knowledge within the single-gene disorders and consequent rapid proliferation of genetic testing enables far greater numbers of individuals to directly benefit from this progress. A compelling rationale exists for this approach: cardiovascular single-gene diseases commonly present with life-threatening events (e.g., sudden cardiac death, heart failure, stroke, etc.), but identification, evaluation, and treatment of individuals with presymptomatic genetic risk has the promise to prevent or ameliorate cardiovascular morbidity and mortality. Cardiovascular genetic medicine programs also anchor training and research, thereby enabling the next generation of academic specialists in cardiovascular genetic medicine to continue to improve cardiovascular health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular genetic medicine is an emerging area devoted to identifying and understanding cardiac conditions resulting from genetic and genomic mechanisms and to developing and validating diagnostic and treatment algorithms and guidelines.
A great deal of progress has been made in the past 20 years to understand the genetic basis of cardiovascular disease, fueled in part by the enormous enthusiasm from the human genome project. Although the implementation of new genetic knowledge into the day-to-day practice of cardiovascular medicine has been difficult, several areas are now ready to move briskly ahead.
Cardiovascular “Single-Gene” or “Mendelian” Diseases
The most tractable diagnoses to move ahead with cardiovascular genetic medicine are the “single-gene” or “Mendelian” diseases (Table 1), which are so categorized because they result from a mutation occurring within a single gene and usually exhibit characteristic inheritance patterns [1]. Common nomenclature (used herein) suggests that a mutation is a relatively rare change in the DNA sequence, occurring in <1% of individuals, whereas a polymorphism is a more commonly occurring variation observed in >1% of individuals [2].
Many of the cardiovascular Mendelian genetic diseases are most commonly caused by mutations in exonic DNA, that is, changes in protein coding (nonsynonymous mutations) with the most common being missense mutations. Small insertions or deletions or splice site mutations that affect protein coding or intron/exon splicing are also observed. Whereas the vast majority of known Mendelian cardiovascular disease-causing mutations are nonsynonymous, a variety of other genetic variation is possible and largely unexplored, including structural genomic changes [2], variations in micro-RNAs or their binding sites [3], epigenetic effects [4], and others.
Some of the more common and well-known cardiovascular single-gene disorders (Table 1) are the cardiomyopathies, including dilated cardiomyopathy (DCM) [5, 6], hypertrophic cardiomyopathy (HCM) [7–11], restrictive cardiomyopathy (RCM) [12–15], and arrhythmogenic right ventricular dysplasia/cardiomyopathy (ARVD/C) [16, 17]. Other single-gene disorders disrupt cardiac conduction and rhythm and are commonly referred to as the channelopathies (the long QT syndrome and related disorders) [18–20]. Single-gene disorders relevant to cardiovascular disease can affect tissues beyond the heart such as Marfan syndrome, a multisystem disease of connective tissue that particularly impacts the aorta [21, 22]. Primary pulmonary hypertension (PPH) aggregating in families is also a Mendelian genetic disease [23, 24]. Familial hypercholesterolemia (FH), caused by mutations in the LDL receptor or related pathways, results in diffuse atherosclerotic vascular disease particularly impacting the coronary circulation [25, 26].
In contrast to the single-gene disorders, complex genetic diseases (Table 1) are understood to result from simultaneous genetic variation in several genes with small effects (for review, see [1, 27]). In this paradigm, the contribution of any individual variant is minimal, but the summed genetic variation in conjunction with environmental factors mediates the disease phenotype. Common diseases postulated to follow this paradigm include coronary heart disease, hypertension, and others [1, 27]. At the present time, the relevance of current genetic information to predict risk in complex diseases such as coronary heart disease for individuals or at-risk family members is unclear [1, 27], an area not covered in this review. However, because of the population risk of complex disease such as coronary heart disease, intense interest in the area may rapidly lead to its inclusion in the practice of cardiovascular genetic medicine.
Opportunities and Issues for Diagnosis of Cardiovascular Mendelian Diseases
Enormous progress has been made to identify and characterize the disease genes specific to the Mendelian cardiovascular diseases (for recent comprehensive reviews, see [5–20]). A molecular genetic diagnosis is usually considered definitive when a rare, protein-altering mutation is identified in a gene known to cause the condition, especially when the mutation segregates with the disease phenotype in multiple affected family members or has been previously reported in association with the phenotype [5]. The availability of genetic testing for many of these genes has recently dramatically expanded, and when accompanied with genetic counseling, makes it now possible to implement the practice of cardiovascular genetic medicine [1, 5, 28–30].
However, locus heterogeneity (many genes causing the same disease) has complicated investigative efforts and will continue to confound diagnostic strategies for the cardiovascular Mendelian diseases [5]. The channelopathies, encompassing the long QT syndrome and related genetic arrhythmic disorders, account for >10 genes [20]. Whereas the HCM genes MYH7, MYBPC3, and TNNT2 (encoding the beta-myosin heavy chain, cardiac myosin-binding protein C, and cardiac troponin T genes, respectively) account for 70–80% of HCM that is commonly diagnosed by molecular genetic approaches [10], an additional 19 genes have been implicated to rarely cause the HCM phenotype [11]. At this time >20 genes have been implicated in DCM [5, 31].
Furthermore, not all disease loci have been identified, which diminishes the sensitivity of molecular testing. Whereas it has been estimated that a mutation causing the long QT syndrome can be identified in up to three-quarters of index patients, other known cardiovascular single-gene disorders lag behind. For example, only 30–60% of the genetic cause of HCM has been identified [29, 32], although some series suggest that, with familial cases, a mutation can be identified in up to two-thirds of probands [10, 33]. For dilated cardiomyopathy, only 20–30% of genetic causation has been identified, principally with familial disease [5, 30].
Further complicating diagnostic strategies is allelic heterogeneity (many mutations within a single gene). For example, MYH7, consisting of 40 exons encoding the beta-myosin heavy chain protein, had 194 mutations listed associated with HCM on the Cardiogenomics website (http://genetics.med.harvard.edu∼seidman/cg3/muts/MYH7_mutations_TOC.html/). For diagnostic purposes, this necessitates sequencing the entire exonic (coding) sequence and intron/exon boundaries of each gene. Many of the contractile proteins have large numbers of exons, making sequencing a time- and effort-intensive undertaking. The current approach to sequencing (the Sanger method utilizing capillary arrays) has provided highly sensitive and reliable results. Newer chip-based sequencing methods, designed to improve speed and efficiency whereas decreasing cost, are now beginning to be introduced into diagnostic use but still face stringent assay validation and quality checks.
A further challenge to cardiovascular genetic medicine is that of syndromic cardiovascular disease. Syndromic disease represents multisystem genetic disease, including, for example, some forms of congenital heart disease and other established genetic conditions (Table 2). Most cardiovascular practitioners, even those emphasizing Mendelian cardiovascular genetic disease, will likely defer the evaluation and treatment of syndromic disease to geneticists who are expert in the particular condition. However, cardiovascular genetic medicine clinics may provide an ideal setting for collaboration between cardiologists with specialty interest in genetic disease and geneticists who care for patients with syndromic cardiovascular disease.
Rationale for the Implementation of Cardiovascular Genetic Medicine
Despite the present limitations outlined above, sufficient knowledge and experience within the field of single-gene (Mendelian) disorders (Table 1) is now available to move briskly ahead to implement the practice of cardiovascular genetic medicine. This field offers a compelling rationale: conventional intervention, treatment, and prevention strategies now available offer enormous opportunity to decrease morbidity and mortality. The cardiovascular genetic diseases presented in this paper almost universally cause early mortality or major morbidity, yet almost all diagnoses offer specific, established interventions to extend survival and diminish morbidity. For example, implantable cardiac defibrillators can prevent sudden cardiac death and its devastating consequences resulting from the genetic cardiomyopathies and arrhythmias [9, 29, 34]. Medical therapy may ameliorate the progression of genetic DCM. Prospective identification of those yet asymptomatic but at greater risk to develop DCM enables close surveillance and early intervention. Both medical or defibrillator therapies can decrease the risk of sudden cardiac death, improve quality of life, and prolong the time to cardiac transplantation or avoid it altogether. Furthermore, it is conceivable, if not likely, that gene-specific therapies will emerge to further ameliorate genetic disease.
Is this recommendation to more formally develop cardiovascular genetic medicine clinics and programs necessary? Some patients already receive outstanding care from geneticists who traditionally assist with diagnosis and counseling and cardiologists who provide cardiovascular treatment options within specific areas such as hypertrophic cardiomyopathy [29, 35, 36] or the long QT syndrome [20, 37, 38]. Notably, both of these conditions have more mature molecular genetic knowledge than the remainder of the field, and hence a more substantial literature base including guidelines for medical practice.
What is new now and what drives the current emphasis to develop cardiovascular genetic medicine is the explosion of genetic knowledge in cardiovascular disease noted above and the consequent extensive proliferation of genetic testing [1, 30]. All of this will enable a far greater number of individuals and their families to benefit from genetic diagnosis and treatment. Within this environment, systematic approaches are warranted. Bringing together cardiovascular subspecialty physicians and genetic counseling expertise within a program broadly designed to diagnose, evaluate, and treat cardiovascular genetic disease for large numbers of patients and families will provide the environment for high-quality clinical care, research, and training, as discussed below in greater detail.
Essential Clinical Components of Cardiovascular Genetic Medicine
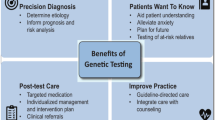
The three core components of cardiovascular genetic medicine include expert medical care, genetic counseling, and clinical genetic testing.
Expert medical care from subspecialty cardiovascular physicians
Medical care within the context of a cardiovascular genetic medicine program ideally embodies a cardiovascular specialist who is a clinical expert in the disease of interest and who is also fully informed regarding the genetics of the disease. For example, the genetic arrhythmias are ideally handled by an electrophysiologist with experience, background, and training in the genetics of arrhythmia. Thus, the physician is not only knowledgeable in the latest approaches and guidelines for arrhythmia evaluation, diagnosis, and treatment, but is also able to offer specific and comprehensive insight and recommendations for the evaluation and intervention with genetically based arrhythmias. Analogously for DCM, a cardiomyopathy or heart failure specialist steeped in the genetic knowledge of DCM would be ideal. Other examples include cardiovascular lipid specialists who interface with families carrying mutations that cause elevated cholesterol and premature atherosclerosis, or experts in HCM (cardiovascular imaging or interventional specialists), all of whom have extensive genetic knowledge of their field.
Genetic counseling and clinical genetic testing
Genetic counseling is imperative for the conduct of a cardiovascular genetic medicine clinic [30]. Regardless of the availability of genetic testing for a disorder, counseling is indicated for pedigree assessment, to determine inheritance patterns, and to ensure adequate knowledge of modes of transmission and risks to offspring [31]. If genetic testing for the condition is available, the careful construction of the family pedigree is essential to select the optimal individual for testing [31]. Counseling regarding genetic testing is also mandatory. It should include discussions regarding positive and negative results and the possibility that variants of unknown significance may be identified [30]. If testing is undertaken, communication of posttest results is conducted within a counseling environment [30, 36, 39].
How will we develop or acquire the requisite genetics expertise for cardiovascular specialists who may not have clinical genetics background or training? A collaborative approach between cardiovascular and genetics specialists has been recommended [5, 36, 40]. With the advent of Master’s trained genetic counselors as a profession, the most tractable solution is to engage genetic counselors to work with subspecialty cardiovascular medicine physicians to provide genetic counseling and testing information. The counseling and testing issues of Mendelian cardiovascular diseases, including the informational and counseling needs related to clinical genetic testing, are well within the training and experience of genetic counselors [30]. Genetic counselors, trained within clinical genetics programs, can also facilitate collaboration and consultation from geneticists for difficult or complex cases or for syndromic disease that requires additional expertise.
Training the Next Generation of Cardiovascular Genetic Medicine Specialists
Cardiovascular genetic medicine clinics will also serve as a training opportunity for the next generation of cardiovascular specialists interested in becoming experts in the field. One approach is to develop formal training programs with concentrations in general clinical genetics and cardiovascular genetics for subspecialty fellows in heart failure/cardiac transplantation or electrophysiology, preventive cardiology, or cardiovascular epidemiology. Clinical experience from the cardiovascular genetic medicine clinic will anchor the training. Additional clinical training will be undertaken in rotations with clinical geneticists in molecular genetic testing laboratories that will include methods and test interpretation. Trainees will also rotate with genetic counselors to understand their role, approach, and the key genetic information transmitted with the counseling process. Participation in cardiovascular genetics seminars and case conferences will augment the experience. Participation in ongoing genetics research will also prepare trainees for careers in academic cardiology.
The Imperative of Ongoing Research and the Promise of Gene or Genetic Therapies
Cardiovascular genetic medicine clinics also provide the foundations for the conduct of a wide array of research critical to moving the field ahead. Perhaps most relevant continues to be the assembly of large clinical databases to be correlated with genetic information. Although in most cases Mendelian cardiovascular diseases have not yet shown predictive genotype/phenotype relationships, it is possible that much larger cohorts with much richer genetic information may yet reveal important relationships. Also presently lacking in the field are outcomes studies of early interventions for presymptomatic at-risk individuals based on genetic testing. These are critically important studies, as cardiovascular genetic disease commonly presents with advanced life-threatening disease (sudden cardiac death, heart failure, stroke, etc.), as noted above, and early presymptomatic diagnosis and intervention may prevent these devastating events.
Continued investigative efforts are warranted for ongoing and emerging issues with the field. Examples include the extent and impact of compound or double mutations on disease [41–45], the lack of segregation in family LMNA DCM mutations suggesting a greater degree of bilineal inheritance than previously understood [46], gene frequencies within DCM [47] or other diagnoses, and cross-over phenotypes between cardiomyopathies (e.g., ARVD [16] or RCM [14]).
Finally, although the promise of targeted therapies for genetic disease has not yet been met, these clinics will also provide the intellectual and clinical infrastructure to initiate clinical trials of targeted therapies to ameliorate genetic disease.
Conclusion
The explosion of recent genetic information for the cardiomyopathies, arrhythmias, and other single-gene cardiovascular disorders enables the practice of cardiovascular genetic medicine. Based upon clinical cardiovascular expertise, combined with robust knowledge of cardiovascular genetic disease, genetic counseling, and genetic testing when available, enormous progress is now possible.
References
Robin, N.H., Tabereaux, P.B., Benza, R., & Korf, B.R. (2007). Genetic testing in cardiovascular disease. Journal of the American College of Cardiology, 50, 727–737.
Pollex, R.L., & Hegele, R.A. (2007). Copy number variation in the human genome and its implications for cardiovascular disease. Circulation, 115, 3130–3138.
Latronico, M.V., Catalucci, D., & Condorelli, G. (2007). Emerging role of microRNAs in cardiovascular biology. Circulation Research, 101, 1225–1236.
Gluckman, P.D., Hanson, M.A., & Beedle, A.S. (2007). Non-genomic transgenerational inheritance of disease risk. Bioessays, 29, 145–154.
Burkett, E.L., & Hershberger, R.E. (2005). Clinical and genetic issues in familial dilated cardiomyopathy. Journal of the American College of Cardiology, 45, 969–81.
Morita, H., Seidman, J., & Seidman, C.E. (2005). Genetic causes of human heart failure. Journal of Clinical Investigation, 115, 518–526.
Taylor, M.R., Carniel, E., & Mestroni, L. (2004). Familial hypertrophic cardiomyopathy: Clinical features, molecular genetics and molecular genetic testing. Expert Review of Molecular Diagnostics, 4, 99–113.
Elliott, P., & McKenna, W.J. (2004). Hypertrophic cardiomyopathy. Lancet, 363, 1881–1891.
Nishimura, R.A., & Holmes Jr., D.R. (2004). Clinical practice. Hypertrophic obstructive cardiomyopathy. New England Journal of Medicine, 350, 1320–1327.
Ho, C.Y., & Seidman, C.E. (2006). A contemporary approach to hypertrophic cardiomyopathy. Circulation, 113, e858–e862.
Bos, J.M., Poley, R.N., Ny, M., Tester, D.J., Xu, X., Vatta, M., et al. (2006). Genotype–phenotype relationships involving hypertrophic cardiomyopathy-associated mutations in titin, muscle LIM protein, and telethonin. Molecular Genetics and Metabolism, 88, 78–85.
Kubo, T., Gimeno, J.R., Bahl, A., Steffensen, U., Steffensen, M., Osman, E., et al. (2007). Prevalence, clinical significance, and genetic basis of hypertrophic cardiomyopathy with restrictive phenotype. Journal of the American College of Cardiology, 49, 2419–2426.
Marian, A.J. (2007). Phenotypic plasticity of sarcomeric protein mutations. Journal of the American College of Cardiology, 49, 2427–2429.
Hoedemaekers, Y.M., Caliskan, K., Majoor-Krakauer, D., van de Laar, I., Michels, M., Witsenburg, M., et al. (2007). Cardiac beta-myosin heavy chain defects in two families with non-compaction cardiomyopathy: Linking non-compaction to hypertrophic, restrictive, and dilated cardiomyopathies. European Heart Journal, 28, 2732–2737.
Morimoto, S. (2008). Sarcomeric proteins and inherited cardiomyopathies. Cardiovascular Research, 77, 659–666.
Sen-Chowdhry, S., Syrris, P., & McKenna, W.J. (2007). Role of genetic analysis in the management of patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy. Journal of the American College of Cardiology, 50, 1813–1821.
Moric-Janiszewska, E., & Markiewicz-Loskot, G. (2007). Review on the genetics of arrhythmogenic right ventricular dysplasia. Europace, 9, 259–266.
Roberts, R. (2006). Genomics and cardiac arrhythmias. Journal of the American College of Cardiology, 47, 9–21.
Priori, S.G., & Napolitano, C. (2006). Role of genetic analyses in cardiology: Part I: Mendelian diseases: Cardiac channelopathies. Circulation, 113, 1130–1135.
Lehnart, S.E., Ackerman, M.J., Benson Jr., D.W., Brugada, R., Clancy, C.E., Donahue, J.K., et al. (2007). Inherited arrhythmias: A National Heart, Lung, and Blood Institute and Office of Rare Diseases workshop consensus report about the diagnosis, phenotyping, molecular mechanisms, and therapeutic approaches for primary cardiomyopathies of gene mutations affecting ion channel function. Circulation, 116, 2325–2345.
Robinson, P.N., Arteaga-Solis, E., Baldock, C., Collod-Beroud, G., Booms, P., De Paepe, A., et al. (2006). The molecular genetics of Marfan syndrome and related disorders. Journal of Medical Genetics, 43, 769–787.
Mizuguchi, T., & Matsumoto, N. (2007). Recent progress in genetics of Marfan syndrome and Marfan-associated disorders. Journal of Human Genetics, 52, 1–12.
Chan, S.Y., & Loscalzo, J. (2008). Pathogenic mechanisms of pulmonary arterial hypertension. Journal of Molecular and Cellular Cardiology, 44, 14–30.
Newman, J.H., Phillips 3rd, J.A., & Loyd, J.E. (2008). Narrative review: The enigma of pulmonary arterial hypertension: New insights from genetic studies. Annals of Internal Medicine, 148, 278–283.
Hegele, R.A. (2006). Genetic susceptibility to heart disease in Canada: Lessons from patients with familial hypercholesterolemia. Genome, 49, 1343–1350.
Soutar, A.K., & Naoumova, R.P. (2007). Mechanisms of disease: Genetic causes of familial hypercholesterolemia. Nature Clinical Practice Cardiovascular Medicine, 4, 214–225.
Arnett, D.K., Baird, A.E., Barkley, R.A., Basson, C.T., Boerwinkle, E., Ganesh, S.K., et al. (2007). Relevance of genetics and genomics for prevention and treatment of cardiovascular disease: A scientific statement from the American Heart Association Council on Epidemiology and Prevention, the Stroke Council, and the Functional Genomics and Translational Biology Interdisciplinary Working Group. Circulation, 115, 2878–901.
Fatkin, D. (2007). Guidelines for the diagnosis and management of familial dilated cardiomyopathy. Heart, Lung and Circulation, 16, 19–21.
Semsarian, C. (2007). Guidelines for the diagnosis and management of hypertrophic cardiomyopathy. Heart, Lung and Circulation, 16, 16–18.
Cowan, J., Morales, A., Dagua, J., & Hershberger, R.E. (2008). Genetic testing and genetic counseling in cardiovascular genetic medicine: Overview and preliminary recommendations. Congestive Heart Failure, 14, 105–113.
Morales, A., Cowan, J., Dagua, J., & Hershberger, R.E. (2008). Family history: An essential tool for cardiovascular genetic medicine. Congestive Heart Failure, 14, 37–45.
Van Driest, S.L., Ommen, S.R., Tajik, A.J., Gersh, B.J., & Ackerman, M.J. (2005). Yield of genetic testing in hypertrophic cardiomyopathy. Mayo Clinic Proceedings, 80, 739–744.
Richard, P., Charron, P., Carrier, L., Ledeuil, C., Cheav, T., Pichereau, C., et al. (2003). Hypertrophic cardiomyopathy: Distribution of disease genes, spectrum of mutations, and implications for a molecular diagnosis strategy. Circulation, 107, 2227–2232.
Maron, B.J., McKenna, W.J., Danielson, G.K., Kappenberger, L.J., Kuhn, H.J., Seidman, C.E., et al. (2003). American College of Cardiology/European Society of Cardiology clinical expert consensus document on hypertrophic cardiomyopathy. A report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the European Society of Cardiology Committee for Practice Guidelines. Journal of the American College of Cardiology, 42, 1687–1713.
Charron, P., Heron, D., Gargiulo, M., Richard, P., Dubourg, O., Desnos, M., et al. (2002). Genetic testing and genetic counselling in hypertrophic cardiomyopathy: The French experience. Journal of Medical Genetics, 39, 741–746.
Michels, M., Hoedemaekers, Y.M., Kofflard, M.J., Frohn-Mulder, I., Dooijes, D., Majoor-Krakauer, D., et al. (2007). Familial screening and genetic counselling in hypertrophic cardiomyopathy: The Rotterdam experience. Netherlands Heart Journal, 15, 184–190.
van Langen, I.M., Hofman, N., Tan, H.L., & Wilde, A.A. (2004). Family and population strategies for screening and counselling of inherited cardiac arrhythmias. Annals of Medicine, 36(Suppl 1), 116–124.
Skinner, J.R. (2007). Guidelines for the diagnosis and management of familial long QT syndrome. Heart, Lung and Circulation, 16, 22–24.
Hendriks, K.S., Grosfeld, F.J., van Tintelen, J.P., van Langen, I.M., Wilde, A.A., van den Bout, J., et al. (2005). Can parents adjust to the idea that their child is at risk for a sudden death?: Psychological impact of risk for long QT syndrome. American Journal of Medical Genetics, 138, 107–112.
van Langen, I.M., Birnie, E., Schuurman, E., Tan, H.L., Hofman, N., Bonsel, G.J., et al. (2005). Preferences of cardiologists and clinical geneticists for the future organization of genetic care in hypertrophic cardiomyopathy: A survey. Clinical Genetics, 68, 360–368.
Keating, M.T., & Sanguinetti, M.C. (2001). Molecular and cellular mechanisms of cardiac arrhythmias. Cell, 104, 569–580.
Ingles, J., Doolan, A., Chiu, C., Seidman, J., Seidman, C., & Semsarian, C. (2005). Compound and double mutations in patients with hypertrophic cardiomyopathy: Implications for genetic testing and counselling. Journal of Medical Genetics, 42, e59.
Westenskow, P., Splawski, I., Timothy, K.W., Keating, M.T., & Sanguinetti, M.C. (2004). Compound mutations: A common cause of severe long-QT syndrome. Circulation, 109, 1834–1841.
Schwartz, P.J., Priori, S.G., & Napolitano, C. (2003). How really rare are rare diseases?: The intriguing case of independent compound mutations in the long QT syndrome. Journal of Cardiovascular Electrophysiology, 14, 1120–1121.
Van Driest, S.L., Vasile, V.C., Ommen, S.R., Will, M.L., Tajik, A.J., Gersh, B.J., et al. (2004). Myosin binding protein C mutations and compound heterozygosity in hypertrophic cardiomyopathy. Journal of the American College of Cardiology, 44, 1903–1910.
Parks, S., Kushner, J.D., Nauman, D., Burgess, D., Ludwigsen, S., Peterson, A., et al. (2008). Lamin A/C mutation analysis in a cohort of 324 unrelated patients with idiopathic or idiopathic dilated cardiomyopathy. American Heart Journal, in press.
Hershberger, R., Parks, S., Kushner, J.D., Li, D., Ludwigsen, S., Jakobs, P., et al. (2008). Coding sequence mutations identified in MYH7, TNNT2, SCN5A, CSRP3, LBD3, and TCAP from 313 patients with familial or idiopathic dilated cardiomyopathy. Clinical and Translational Science, in press.
Nussbaum, R. L., McInnes, R. R., & Willard, H. F. (2004). Thompson & Thompson genetics in medicine, revised reprint edition (6th ed.). Philadelphia, PA: Saunders.
GeneReviews at GeneTests: Medical genetics information resource. GeneTests/GeneClinics. Retrieved March 17, 2008, from http://www.genetests.org.
Manning, N., Kaufman, L., & Roberts, P. (2005). Genetics of cardiological disorders. Seminars in Fetal and Neonatal Medicine, 10, 259–269.
Harper, P.S. (2004). Practical genetic counseling (6th ed.). London: Oxford University Press.
OMIMÔ—Online Mendelian Inheritance in Man. Retrieved March 17, 2008, from http://www.ncbi.nlm.nih.gov/omim/.
Allanson, J.E. (2008). Noonan syndrome. In: GeneReviews at GeneTests: Medical genetics information resource. GeneTests/GeneClinics 2007. Retrieved March 17, 2008, from http://www.genetests.org.
Dietz, H.C. (2008). Marfan syndrome. In: GeneReviews at GeneTests: Medical genetics information resource. GeneTests/GeneClinics 2005. Retrieved March 17, 2008, from http://www.genetests.org.
Hejtmancik, J.F., Brink, P.A., Towbin, J., Hill, R., Brink, L., Tapscott, T., et al. (1991). Localization of gene for familial hypertrophic cardiomyopathy to chromosome 14q1 in a diverse US population. Circulation, 83, 1592–1597.
Wimalasundera, R.C., & Gardiner, H.M. (2004). Congenital heart disease and aneuploidy. Prenatal Diagnosis, 24, 1116–1122.
Rimoin, D.L., Connor, M.J., Pyeritz, R.E., Korf, B.R., eds. (2007). Emery and Rimoin’s principles and practice of medical genetics (5th ed., vol. 1). Philadelphia, PA: Elsevier.
Pajkrt, E., Weisz, B., Firth, H.V., & Chitty, L.S. (2004). Fetal cardiac anomalies and genetic syndromes. Prenatal Diagnosis, 24, 1104–1115.
Ho, K.K.L., Anderson, K.M., Kannel, W.B., Grossman, W., & Levy, D. (1993). Survival after the onset of congestive heart failure in Framingham heart study subjects. Circulation, 88, 107–115.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hershberger, R.E. Cardiovascular Genetic Medicine: Evolving Concepts, Rationale, and Implementation. J. of Cardiovasc. Trans. Res. 1, 137–143 (2008). https://doi.org/10.1007/s12265-008-9031-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-008-9031-3