Abstract
To analyze treatment and survival in a series of resected patients with primary or recurrent retroperitoneal sarcoma (RPS) treated and prospectively followed at a single institution. Between July 1994 and December 2015, 89 patients (36 M, 53 F; mean age 60 years, range 25–79) were evaluated. For the purpose of analysis, complete resection was defined as removal of gross tumor with histologically confirmed clear resection margins. Eighty-three out of the 89 patients (93%), 46 of whom affected by primary RPS, and 37 by recurrent RPS, underwent surgical exploration. Sixty-two had a grossly and microscopically complete resection. Fifty-three out of 83 patients (64%) underwent removal of contiguous intra-abdominal organs. Preoperative mortality was nil and significant preoperative complications occurred in six cases only (7%). High-grade tumor pointed out to be a significant variable for a worse survival in all 83 patients amenable to undergo surgical resection (57% 5 years survival for low grade vs 14% for high grade; P = 0.0004). Among completely resected patients, only histologic grade clearly affected disease-free survival (72% 5 years survival for low grade vs 50% for high grade; P = 0.04), while the role of preoperative blood transfusions (67% 5 years survival for non-transfused patients vs 29% for transfused patients; P = 0.05) has to be evaluated in connection to patient complexity. Histological grade and recurrence are the most valuable prognostic predictors; in this clinical subset, an aggressive surgical approach in both primary and recurrent RPS is associated with a best long-term survival and disease-free survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Retroperitoneal sarcoma (RPS) is a heterogeneous disease with about 1000 new cases reported annually in the USA alone [1]. Most are liposarcomas or, less frequently, leiomyosarcomas, and the only potential cure is complete resection with negative surgical margins [2, 3]. This remains technically difficult because of deep-seated location, multifocality, and necessity of multi-visceral resections [4]. The principal cause of failure is locally recurrent disease, [5] with debate concerning the value of adjuvant chemotherapy and/or radiotherapy [6]. Risk stratification is based upon the American Joint Committee on Cancer (AJCC) staging for soft tissue sarcomas (STS) of the extremity, where the main factors implicated in survival include the histologic tumor grade, the pathologic subtype, and the resection margins [7]. Given the small number of cases in many single-institution series, management nomograms have been developed for treatment and to predict survival rates [8, 9].
Literature concerning management and outcomes of RPS should be viewed cautiously. In fact, multi-visceral resection in RPS has no comparable morbidity and mortality when contrasted with more complex resections for peripheral extremity STS. Moreover, en bloc resections trade off morbidity and mortality with lower recurrence rates when compared with simple excision of the mass, although this may not always translate into an improved survival [10]. Finally, reported survival rates reflect heterogeneity concerning histology, differentiation, surgical volume, and follow-up periods, with differential expertise and multidisciplinary approach towards patient management. In specialized centers, primary RPS resection rates may approach 90% [11], secondary resection rates in recurrences 50% respectively [12]. Long-term survival rates following primary resection have been reported as between 50 and 66% [2, 11] and up to 40% in recurrent cases undergoing re-resection [13].
Patients and Methods
We report our experience of 89 patients presenting with primary or recurrent RPS referred to the European Institute of Oncology in Milan over a 21-year period (1994–2015), evaluating the principal prognostic factors.
Cases were identified by a computer-generated search of the institutional database, cross-checking separate pathology and clinical databases using the ICD-9 search code 158.0 for RPS, which identify both primary and recurrent disease [14]. Analysis included a total of 89 (36 males and 53 females) with an overall median age of 60 years (range 25–79 years). There were 46 presenting with primary RPS and 37 recurrent cases. Tumors were categorized by histology in accordance to WHO classification system for soft tissue tumors [15] with grade scored simply as either low or high (Table 1). All available pathologic slides were reviewed, and it was elected not to differentiate histologic subtypes of liposarcoma. Date of death was determined by review of the medical records and available death certificates.
For purposes of definition, primary RPS was considered as a lesion being either untreated or biopsied prior to definitive surgical therapy, while recurrent RPS cases presented clinical, radiological, and/or histopathological proof of tumor bearing the same histology as the primary one (although not of necessity, the same histological grade), either within or contiguous to the previously treated tumor bed. Records were analyzed to assess survival and response to therapy based on patient demographic data including gender, age, preoperative symptoms, and symptom duration along with other clinic and pathological features such as measured tumor size and principal tumor location. Analysis included presence of infiltration into adjacent organ(s), metastatic disease at presentation, extent of surgical resection, use of adjuvant radiotherapy and/or chemotherapy or neoadjuvant chemo-radiation, and the number of repeat operative procedures where appropriate.
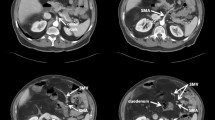
All patients underwent a contrast-enhanced thoracic-abdominopelvic CT scan with additional imaging (magnetic resonance (MR) imaging and FDG-PET scanning) where appropriate. Clinical post-surgical follow-up was conducted every 3 months for the first 2 years, then with radiological follow-up by thoracic-abdominopelvic CT and MRI (where appropriate) every 6 months or sooner considering symptomatology. Patients were censored until death or their last visit. Resection of recurrent disease and utilization of radiotherapy and/or chemotherapy for recurrent disease were separately evaluated.
Resection was regarded as “complete” (R0) if all grossly visible tumor tissue had been removed with confirmation of histologically clear margins. “Incomplete” resections were recorded if there was partial removal with residual gross disease. Resections with grossly surgical clear margins were also deemed to be incomplete if margins were found to be histologically involved (R1). Such cases are different from palliative resections as the latter may have been performed in presence of significant symptoms, without a curative intent. Recurrence was defined “local” if located within the retroperitoneum or peritoneal cavity following a prior complete resection. Distant recurrence was defined where there were discrete visceral sites of metastatic spread.
Operative mortality included any death within 30 days of surgery or within 6 months following surgery if directly related to surgical complications. Operative morbidity considered complications observed within 30 days of surgery or within 6 months following surgery if it was clearly related to any surgical procedure. Significant complications included wound infection and dehiscence, reactionary hemorrhage necessitating a repeat laparotomy, postoperative pneumonia, septicemia, (with positive blood culture), imaging identification of an intra-abdominal abscess, entero-cutaneous fistula, confirmed deep vein thrombosis, and/or pulmonary embolism. There was no uniform protocol for adjuvant radiotherapy but we generally mirrored the policy reported by Stojadinovic et al. [16], where patients with close macroscopic resection margins underwent adjuvant radiation with a preference where feasible for brachytherapy (BT). Target area was defined after intraoperatively; then, afterload catheters were placed percutaneously at 1–1.5-cm intervals and sutured to the target region with fixation to the skin using small buttons. Single-plane implant was generally preferred, with localization films performed in the immediate postoperative period and computerized dosimetry calculation. Catheters were loaded with a pulse (PDR) source of 192Iridium to provide a total dose of 10–15 Gy and dose rate of 0.5 Gy/h. In cases of anatomic preclusion to catheter placement, if adjuvant radiotherapy was deemed appropriate, external beam radiation therapy (EBRT) was utilized.
Statistical Analysis
Statistics were performed with SPSS software program (SPSS Inc., Chicago, IL, USA). Chi-squared test or Fisher’s exact test was used for categorical variables where appropriate and the Kaplan-Meier method estimated survival from time of primary treatment to the date of the most recent follow-up examination or death. Differences between survival rates were compared using the log-rank test. P values < 0.05 were considered to be significant.
Results
All primary RPSs were symptomatic at presentation with a mean duration of symptoms of 12 months (range 3–24 months). The commonest symptoms were abdominal pain (13 patients) and abdominal mass (23 patients). All patients underwent abdominal ultrasonography; CT scan was performed in 72 patients (81%), with subsequent MR imaging performed in 14 patients (16%) and with all patients undergoing a preoperative tumor biopsy. Intraoperative biopsy with frozen section was only utilized in accordance with the recommendations of Hajdu et al. [15] in cases deemed not resectable or in rare circumstances where a distinction from lymphoma was required. Eighty-three out of the 89 patients (93%) underwent resection (46 with primary RPS vs 37 with recurrent RPS). Six patients with recurrent disease were not operated surgery either by virtue of widespread metastatic disease or poor general condition at the time of presentation; all of them died within 15 months of presentation.
Median time between primary surgical resection and presentation to visit in the 37 recurrent patients was 36 months (range 4–208 months). Six patients (7%) underwent surgery for a second recurrence, two patients (2%) for a third and a fourth ones, and three patients (4%) experienced a fifth presentation, two of whom being resected with curative intent. Tumors occupied the upper abdominal compartments in 29 patients (35%), the central mid-abdomen in 42 patients (51%), and the lower abdomen and pelvis in 12 cases (14%). Pathologic tumor size was < 10 cm in maximal diameter in 15/83 cases (18%), 10–20 cm in maximal diameter in 31/83 (37%), and > 20 cm in maximal diameter in 37/83 cases (45%). Histologic examination revealed that overall, 45/83 patients (54%) had high-grade tumors (24/46 or 52% of primary RPS cases vs 24/37 or 65% of recurrent RPS cases; P = 0.24).
In the entire cohort, 33 patients were transfused, with median 2000 mL of packed red blood cells (range 1000–7500 mL). Among resected patients, 18/46 (39%) with primary disease and 13/37 (35%) with recurrence received transfusion (P = 0.71), with no difference in blood requirement between low-grade and high-grade sarcomas (15/44 or 34% vs 17/39 or 44%, respectively; P = 0.37). Among the 62 patients undergoing complete resections, 11/29 (38%) with low-grade disease and 16/33 (48%) with high-grade disease were transfused (P = 0.40).
Resection with curative intent involved 62/83 cases (74%), while 16 patients underwent gross resection with the suspect of microscopically infiltrated margins (R1) or macroscopically disease remnant (R2). There were also five patients (all belonging to the recurrence group) deliberately treated with palliative resections after presenting with small or large bowel obstruction. Among this latter group, two patients had received ifosfamide chemotherapy but died from disease at 34 and 24 months from the time of diagnosis, respectively. The other three patients received external beam radiotherapy (EBRT) as adjuvant treatment, each dying at 24, 12, and 7 months respectively from the diagnosis. Among primary RPS patients resected for cure, 42 (91%) had histologically negative margins. Eight recurrent cases resected with curative intent presented histologically infiltrated margins, with a complete resection rate of 86% (71/83).
Fifty-three patients (64%) underwent removal of contiguous intra-abdominal organs (Table 2) including 31/46 (67%) with primary and 22/37 (59%) with recurrent disease. Four patients required extensive removal of either anterior or posterior abdominal wall. Of the total group with contiguous resections, 20 (38%) showed histologic infiltration of the resected organ.
In the entire cohort, there was one preoperative death in a patient with multiple preoperative comorbidities that undergone surgery for an angiosarcoma. An early postoperative hemoperitoneum was developed, needing repeat laparotomy with management as an open laparostomy; the patient died on the 23rd postoperative day from septic shock and multi-organ failure.
Significant postoperative complications occurred in 20 patients (24%), 17 of which involving those undergoing multi-visceral resections (Table 2). Although complicated patients were few, likelihood of a significant preoperative complication increased if blood transfusion was required (17/33 patients (52%) transfused vs 4/50 (8%) non-transfused; P < 0.01).
Overall 5-year survival rate regardless of the histologic resection margins was 51% (95% CI 41–63%). There was no effect played by gender, age, preoperative symptoms, symptom duration, tumor size, or location. Only presence of a high-grade tumor significantly predicted a worse overall survival in all 83 resected patients (low-grade overall 5-year survival 57% vs high-grade overall 5-year survival 14%; P = 0.0004; Fig. 1). Following complete resection, 5-year overall survival rate was 63% compared with 17% for incomplete resection (P = 0.003; Fig. 2). Absence of recurrence following complete resection predicted a significantly better 5-year overall survival (100%) than those who experienced recurrent disease (26%; P = 0.003).
A peculiar relation linked disease-free survival and blood transfusions in patients that undergone complete resection (59% 5-year disease-free survival in non-transfused patients vs 30% 5-year disease-free survival for transfused patients; P = 0.05).
Histologic grade proved to be a significant predictor in disease-free survival (DFS, 62% 5-year DFS for low-grade tumors vs 50% 5-year DFS for high-grade tumors; P = 0.04, Fig. 3). Five-year DFS in R0 cases was 58% (95% CI 46–73%) and was 68% for primary RPS and 37% for recurrent cases.
Histologic subtype also proved to be predictive: all diseases with a histology different from liposarcoma (angiosarcoma, leiomyosarcoma, fibrosarcoma, synovial sarcoma) relapsed within 10 months to 5 years after surgery, while, among liposarcomas, the different was played by histologic grade.
Fourteen patients received postoperative EBRT (39–54 Gy); 15 patients, EBRT plus multidrug chemotherapy (ifosfamide with or without either adriamycin or epirubicin); and 12, multidrug chemotherapy alone. Seven patients received brachytherapy (10–15 Gy), five of whom in combination with EBRT. Total received dose was 45–54 Gy. The use of adjuvant radiotherapy or chemotherapy in such small numbers had no impact on overall or disease-free cancer-specific survival. Among the 44 patients receiving chemotherapy, radiotherapy, or both, 7 remained alive at 7 years of follow-up.
Discussion
Seventy-four percent of patients underwent surgery with curative intent, with a 91% incidence of R0 resections. There was a greater likelihood of R0 resection in primary than recurrent cases. Most patients undergoing surgery required extirpation of contiguous structures with two-thirds of them showing histologically clear resection margins. Likelihood of preoperative complications was increased in presence of multi-visceral resections.
High histologic grade predicted a worse cancer-specific survival, while there was prognostic advantage in patients that undergone complete resections and in cases which did not relapse over follow-up.
Impact of transfusion on survival has to be carefully evaluated: transfusion acts more likely as the consequence of complex morbidity subset than a survival predictor and involves patients in worse clinical condition, with a worse prognosis itself.
No effect was noted in either overall or disease-free survival between resections performed for primary or recurrent RPS, provided that there was no further recurrence.
Retroperitoneal space is the second commonest site for malignant mesenchymal tumors, with up to two-thirds of cases proving malignant and one-third being classified as sarcomas. As in other reports, our cases were largely comprised of liposarcomas [17] with nearly half being massive (> 20 cm in maximal diameter) in size. Half the cases were high grade in type without any difference noted in between the primary and recurrent tumors. Other studies reported that the majority of cases tend to be of low or intermediate grade [3, 13].
Although histological grade was the principal independent variable affecting overall and disease-free survival, as described in many studies [18], still there is currently no consensus concerning standardization and reporting for RPS management. The clinical effect of grade in RPS management is conditional upon histological subtype, reflecting a presumptive predictability of clinical behavior. Lower grade liposarcomas tend to show greater propensity towards local as opposed to distant tumor recurrence, provided they are not pleomorphic [19]. Given these specific findings, survival impact of tumor differentiation may suggest a strong link between greater tumor dedifferentiation and multi-visceral resections, this one having a greater risk of histological margin involvement themselves [20].
In our cohort, all non-liposarcoma-like histologic types showed early recurrence. The specific role played by histologic subtype deserves further investigation, being non-liposarcoma cases less frequent than liposarcomas.
The finding that an incomplete resection compromises cancer-specific survival has previously been reported [17] with pooled data from the Johns Hopkins University School of Medicine and the Anderson Cancer Center—Houston combining 2456 patients and showing that the single most important survival factor is the completeness of resection [7]. As in our study, average life expectancy in incomplete resection is comparatively poor. By contrast, deliberate palliative resection may in selected cases prove beneficial [21]. We also showed that proper multi-visceral resection can prove beneficial although associated with a greater likelihood of margin involvement. No difference was found in the need for multi-visceral resection between primary or recurrent RPS cases.
Even following macroscopically complete resection, local recurrence may occur in 25–75% cases, being the principal cause of cancer-related death. The role of adjuvant radiotherapy is not established although most units advocate its use in cases where there is margin involvement as well as in large tumors undergoing resection with curative intent. Several retrospective, single-institution studies have shown survival advantage for postoperative radiotherapy after tumor resection over resection alone [22,23,24,25]. The American College Surgical Oncology Group (ACOSOG) initiated the phase III randomized, controlled Z9031 trial in order to examine the effect of preoperative radiotherapy combined with R0 resection surgery over surgery alone; however, this trial was closed prematurely because of poor patient accrual. It has been replaced by the current EORTC 62092-22092 (STRASS) trial designed to examine any radio-therapeutic benefit in RPS. As outcomes of this trial are awaited, in lieu of this data, a recent retrospective analysis of the National Cancer Database by Nussbaum et al. [22] of preoperative and postoperative radiotherapy compared with surgery alone showed significant survival advantage for both techniques. Reduction of radiation dose (to 45–54 Gy) with a normal tissue displacement characteristic would currently favor preoperative radiation followed by an R0 resection for the highest chance of success, permitting safer delivery of multimodal therapy. Selective impact of alternative new radiation modalities needs to be determined. These include dose escalation and selective integrative boosts for “at risk” margin cases so as to deliver higher doses (> 60 Gy), highly conformal techniques such as intensity-modulated radiotherapy (IMRT) and particle beam (proton) therapy. Proton beam therapy will allow better distribution to irregularly shaped target volumes and provide a better dose tailoring per case sparing normal tissues [23]. Any improvement in survival with these approaches is more likely to be noted, however, in recurrence-free rather than overall survival [24].
Redoing RPS surgery is particularly challenging, but may be associated with long-term survival. R0 resection rates in recurrences are inferior to rates obtained in primary cases, more frequently requiring the need for multi-visceral resections. However, there appears to be clinical benefit and long-term survival of repeat even third (and beyond) re-resections in selected cases [12, 25]. Although patients frequently die from disease, the primary site of failure still remains the local one, particularly in high-grade cases. Consequently, disease biology needs to be taken into account. In repeated recurrences, in fact, disease-free interval, as well as the rate of progression, may influence the indication for further aggressive ablative surgery in particular histologic cases [26].
The majority of local recurrence occurs within the first 2–3 years of follow-up; however, recurrence after 10–15 years has also been reported [27]. Our finding of similar survival between primarily resected RPS and repeat resection cases has been previously reported [28]. Among recurrences, prognostic factors really affecting ultimate survival remain controversial. In this regard, Grobmeyer et al. [24] found no association between overall survival after repeat resection and tumor size, patient age, primary histology, or tumor multifocality. Other groups (including ours) have, however, reported that multifocality, principal histology, blood loss during resection, tumor growth rate, and disease-free are important in survival of recurrent cases [4, 29]. In general, second and third recurrences tend to occur at progressively shorter intervals with reduced ability to achieve complete resections.
Notwithstanding the small numbers in some subgroups, the retrospective nature, and a non-uniform policy towards the use of adjuvant therapies, our study shows advantage in repeated resection of recurrent RPS cases where there is an aggressive surgical policy. This effect is seen regardless of whether the patient has a primary or a recurrent RPS tumor.
Abbreviations
- RPS:
-
Retroperitoneal sarcoma
- STS:
-
Soft tissue sarcoma
- ICD:
-
International Classification for Diseases
- DFS:
-
Disease-free survival
- CT:
-
Computerized tomography
- MRI:
-
Magnetic resonance imaging
- EBRT:
-
External beam radiotherapy
- BT:
-
Brachytherapy
- AJCC:
-
American Joint Committee on Cancer
References
Kotilingam D, Lev DC, Lazar AJ et al (2006) Staging soft tissue sarcoma: evolution and change. CA Cancer J Clin 56(5):282–291
Chiappa A, Zbar AP, Biffi R, Bertani E, Biella F, Viale G, Pace U, Pruneri G, Orecchia R, Lazzari R, Poldi D, Andreoni B (2006) Effect of resection and outcome in patients with retroperitoneal sarcoma. ANZ J Surg 76(6):462–466. https://doi.org/10.1111/j.i445-2197.2006.03753.x
Olimpiadi Y, Song S, Hu JS, Matcuk GR, Chopra S, Eisenberg BL, Sener SF, Tseng WW (2015) Contemporary management of retroperitoneal soft tissue sarcomas. Curr Oncol Rep 17(8):39. https://doi.org/10.1007/s11912-015-0462-0
Anaya DA, Lahat G, Liu J et al (2009) Multi-focality in retroperitoneal sarcoma: a prognostic factor critical to surgical decision-making. Ann Surg 249:137–142
Hogg H, Manas DM, Lee D, Dildey P, Scott J, Lunec J, French JJ (2016) Surgical outcome and patterns of recurrence for retroperitoneal sarcoma at a single centre. Ann R Coll Surg Engl 98(03):192–197. https://doi.org/10.1308/rcsann.2016.0057
Cheng H, Miura JT, Lalehzari M, Rajeev R, Donahue AE, Bedi M, Gamblin TC, Turaga KK, Johnston FM (2016) Neoadjuvant radiotherapy for retroperitoneal sarcoma: a systematic review. J Surg Oncol 113(6):628–634. https://doi.org/10.1002/jso.24221
Nathan H, Raut CP, Thornton K, Herman JM, Ahuja N, Schulick RD, Choti MA, Pawlik TM (2009) Predictors of survival after resection of retroperitoneal sarcoma: a population-based analysis and critical appraisal of the AJCC staging system. Ann Surg 250(6):970–976. https://doi.org/10.1097/SLA.0b013e3181b25183
Gronchi A, Miceli R, Shurell E et al (2013) Outcome prediction in primary resected retroperitoneal soft tissue sarcoma: histology-specific overall survival and disease-free survival nomograms built on major sarcoma center data sets. J Clin Oncol 31:1649–1655
Chou Y-S, Liu C-Y, Chang Y-H, King K-L, Chen PC-H, Pan C-C, Shen S-H, Liu Y-M, Chen K-K, Shyr Y-M, Lee R-C, Chao T-C, Yang M-H, Chan C-H, You J-Y, Yen C-C (2016) Prognostic factors of primary resected retroperitoneal soft tissue sarcoma: analysis from a single Asian tertiary center and external validation of Gronchi’s nomogram. J Surg Oncol 113(4):355–360. https://doi.org/10.1002/jso.24155
Gronchi A, Lo Vullo S, Fiore M et al (2009) Aggressive surgical policies in a retrospectively reviewed single-institution case series of retroperitoneal soft tissue sarcoma patients. J Clin Oncol 27:24–30
Karakousis CP, Velez AF, Gerstenbluth R, Driscoll DL (1996) Resectability and survival in retroperitoneal sarcomas. Ann Surg Oncol 3(2):150–158. https://doi.org/10.1007/BF02305794
Lochan R, French JJ, Manas DM (2011) Surgery for retroperitoneal soft tissue sarcomas: aggressive re-resection of recurrent disease is possible. Ann R Coll Surg Engl 93(1):39–43. https://doi.org/10.1308/003588410X12771863936729
Erzen D, Sencar M, Novak J (2005) Retroperitoneal sarcoma: 25 years of experience with aggressive surgical treatment at the Institute of Oncology, Ljubljana. J Surg Oncol 91:1–9
ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification, 2005), text book in 2 volumes edited by Los Angeles, CA: Practice Management Information Corporation. (PMIC), ©2004
Hajdu SI, Shiu MH, Brennan MF (1988) The role of the pathologist in the management of soft tissue sarcomas. World J Surg 12(3):326–331. https://doi.org/10.1007/BF01655665
Stojadinovic A, Leung DH, Hoos A et al (2002) Analysis of the prognostic significance of microscopic margins in 2,084 localized primary adult soft tissue sarcomas. Ann Surg 235(3):424–434. https://doi.org/10.1097/00000658-200203000-00015
Gemici K, Buldu I, Acar T, Alptekin H, Kaynar M, Tekinarslan E, Karatag T, Efe D, Çolak H, Kuçukkartallar T, Istanbulluoglu O (2015) Management of patients with retroperitoneal tumours and a review of the literature. World J Surg Oncol 13(1):143. https://doi.org/10.1186/s12957-015-0548-z
Eilber FC, Brennan MF, Eilber FR, Dry SM, Singer S, Kattan MW (2004) Validation of the postoperative nomogram for 12-year sarcoma-specific mortality. Cancer 101(10):2270–2275. https://doi.org/10.1002/cncr.20570
Neuhaus SJ, Barry P, Clark MA, Hayes AJ, Fisher C, Thomas JM (2005) Surgical management of primary and recurrent retroperitoneal liposarcoma. Br J Surg 92(2):246–252. https://doi.org/10.1002/bjs.4802
Lahat G, Anaya DA, Wang X, Tuvin D, Lev D, Pollock RE (2008) Resectable well-differentiated versus dedifferentiated liposarcomas: two different diseases possibly requiring different treatment approaches. Ann Surg Oncol 15(6):1585–1593. https://doi.org/10.1245/s10434-007-9805-x
Shibata D, Lewis JJ, Leung DH, Brennan MF (2001) Is there a role for incomplete resection in the management of retroperitoneal liposarcomas? J Am Coll Surg 193(4):373–379. https://doi.org/10.1016/S1072-7515(01)01024-9
Nussbaum DP, Rushing CN, Lane WO, Cardona DM, Kirsch DG, Peterson BL, Blazer DG 3rd (2016) Preoperative or postoperative radiotherapy versus surgery alone for retroperitoneal sarcoma: a case-control, propensity score-matched analysis of a nationwide clinical oncology database. Lancet Oncol 17(7):966–975. https://doi.org/10.1016/S1470-2045(16)30050-X
Mohindra P, Neuman HB, Kozak KR (2013) The role of radiation in retroperitoneal sarcoma. Curr Treat Options in Oncol 14(3):425–441. https://doi.org/10.1007/s11864-013-0236-6
Grobmeyer SR, Wilson JP, Apel B, Knapik J, Bell WC, Kim T, Bland KI, Copeland EM, Hochwald SN, Heslin MJ (2010) Recurrent retroperitoneal sarcoma: impact of biology and therapy on outcomes. J Am Coll Surg 210(5):602–610. https://doi.org/10.1016/j.jamcollsurg.2009.12.024
Gyorki DF, Brennan MF (2014) Management of recurrent retroperitoneal sarcoma. J Surg Oncol 109(1):53–59. https://doi.org/10.1002/jso.23463
Park JO, Qin L, Prete FP et al (2009) Predicting outcome by growth rate of locally recurrent retroperitoneal liposarcoma: the one centimetre per month rule. Ann Surg 250:977–982
TransAtlantic RPSWG (2015) Management of primary retroperitoneal sarcoma (RPS) in the adult: a consensus approach from the Trans-Atlantic RPS Working Group. Ann Surg Oncol 22(1):256–263. https://doi.org/10.1245/s10434-014-3965-2
van Dalen T, Hoekstra HJ, van Geel AN, van Coevorden F, Albus-Lutter C, Slootweg PJ, Hennipman A, Dutch Soft Tissue Sarcoma Group (2001) Locoregional recurrence of retroperitoneal soft tissue sarcoma: second chance of cure for selected patients. Eur J Surg Oncol 27(6):564–568. https://doi.org/10.1053/ejso.2001.1166
Chiappa A, Zbar AP, Biffi R et al (2004) Primary and recurrent retroperitoneal sarcoma: factors affecting survival and long-term outcome. Hepato-Gastroenterology 51(59):1304–1309
Author information
Authors and Affiliations
Contributions
All authors have taken part to all stages of this work, design, execution, and analysis.
Corresponding author
Ethics declarations
All the phases of the work have been carried out with the approval of the ethics committee and under the edge of a written consensus to use clinical and biomedical data for scientific purposes, signed by patients during pre-hospitalization visit.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Chiappa, A., Bertani, E., Pravettoni, G. et al. Aggressive Surgical Approach for Treatment of Primary and Recurrent Retroperitoneal Soft Tissue Sarcoma. Indian J Surg 80, 154–162 (2018). https://doi.org/10.1007/s12262-018-1722-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-018-1722-7