Abstract
Telementoring as a subset of telemedicine has evolved over the past few years, but it is yet to be utilized to its full potential. The technology holds promise in bridging divides of distance and enables far-flung areas to be mentored in operative advances. It thus has a special bearing in countries like India where health care is short staffed and many areas lack availability of quality care. We describe the setting up of a telementoring facility at our centre. As against a ‘routine’ facility with dedicated equipments which cost heavily, our facility was set up using mostly equipments commonly available in an operating room. The facility is presently functional and allows telementoring through an encrypted Web-based service. Our set-up design can be emulated in centres with financial constraint and can help raise the standard of surgical care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Telemedicine, a term first used in 1970, is a fast-emerging global phenomenon. The WHO defines it as “The delivery of healthcare services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnoses, treatment and prevention of diseases and injuries, research and evaluation and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities” [1].
With the continuing expansion in population worldwide and the near-fixed rate of medical student enrollments, there is an expected increase in surgical work between 2001 and 2020. A near 10 % shortage of general surgical workforce is expected by the year 2030 with subspeciality services being affected much worse [2]. Surgical telementoring is a concept within telemedicine where an expert physician guides another at a different geographical location. It is a vastly under-utilized technique and could be a new way to impart and improve upon surgical education.
Objective
The set-up was envisioned as an innovative program where surgeons from this institute could make themselves available to their colleagues across the world. The aim was to improve access to surgeons in remote areas and help develop a good surgical team trained in contemporary surgical procedures.
General Set-up Requirements in Telementoring for the ‘Mentor’
The set-up requires a network which could vary among the WAN/LAN/VPN or I.P. service. The mentor needs to relay with a minimum upstreaming bandwidth of 1 Mbps and a downstreaming of 2 Mbps. The availability of a static I.P. allows reliable, secure and fast streaming and is preferable to a dynamic I.P.
A good-quality video capture device, able to capture at least 25 frames per second, is desirable. A good high-definition display unit and an amplified audio connection and microphone are also needed. Video conferencing services can be of two types, viz. point-to-point services and virtual meeting point services. Point-to-point services involve two parties only, where one calls the other and are quickly established. Virtual meeting point services involve multiple members. They also allow for changing work teams and are preferred if the members keep joining and leaving the video conference. Technical solution for video conferencing ranges from satellite connections, Internet protocol-based services, Integrated System Data Network (ISDN) and mobile networks (3G and 4G-LTE). The various services such mentioned offer several pros and cons of their own [3].
General Set-up Requirements in Telementoring for the ‘Participants’
The participants require a software set-up of Windows Win 7 (32 bit) or higher running on a core of Pentium 4/core 2 duo/INTEL i3/i5/i7 or above. A 2 GB random access memory (RAM) and 100 MB of available hard disc drive space are needed with a network interface card (NIC) of 100 MB or higher. The participants must have video conferencing software or service and a high-speed broadband (at least 512 kbps upstream and 1 Mbps downstream). Lastly, a display, a video input device and an audio input device are needed for the participants.
Journey of Our Set-up
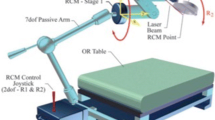
The idea was conceived in the division of surgical oncology at SMS Medical College and Hospital, Jaipur. The transmission was first attempted using the in-hospital broadband line from the Department of Medical Oncology and then a mobile-based 3G service. We progressed to a dynamic I.P. use and finally started using a static I.P. connection provided by the National Knowledge Network. It may be brought to notice here that the National Knowledge Network is a multi-gigabyte Pan-India network providing high-speed Internet network to educational institutions. An out of use, a laparoscopic camera unit was modified to be used as an over-head video capture device (Figs. 1 and 2) and another old Sony compact processor was used as an adjunct for the same. The connections were tweaked to be made functional with the laparoscopic high-definition display unit in use in the operation room, and a conventional collar microphone was associated with the set-up. A digital video recording (DVR) system was purchased which allowed for synchronous recording and asynchronous transmission of the feed from the camera.
Cost-effectiveness of Our Set-up
The generic telementoring systems in software along with the complete installation range from 50,000 to 80,000 USD. The annual costs for maintenance and broadband services range from 10,000 to 20,000 USD [4]. Since the basic premise of a mentoring set-up is to provide for the lesser-privileged health-care centers, the sharp costs defeat much of the purpose. The instruments used at our set-up, e.g. a laparoscopic camera (Fig. 1) and display unit, are freely available even in modest settings. The additional costs incurred included a collar microphone for 20 USD, the DVR system for 130 USD and installation and service charges of 75 USD approximately. The value for money nature of our set-up allows that high-quality streaming can be made at a reasonable cost to the centre (Fig. 3).
The Pros and Cons of Telementoring
At the outset, telementoring facilitates procedures that would otherwise have not been attempted in certain remote set-ups due to their complexity or the lack of experienced skill. The facility is also useful for timely guidance in the face of unexpected intra-operative findings and can be used to assist emergencies. Asynchronous (store-and-forward) relay can also be used for trainee education and can help shorten the training curve for complex procedures cutting down overall health-care costs incurred.
The concept, however, faces steep challenges in the form of need for infrastructure where a minimum modest investment is required on the participant’s end to view the relay. Few issues specific to the concept involve the need for secure transmission of the feed. The relays suffer from technical problems like latency in transmission, and a minimum bandwidth must be maintained. Ethical and legal considerations must be looked into, and issues regarding medical liability should be addressed beforehand to clarify the responsibility of each member of the set-up (the patient, the mentor and the treating clinician). Similarly, patient privacy matters need to be paid attention to and a secure encrypted connection must be used [5].
Conclusion
Telementoring offers vast opportunities, which if used judiciously, could be very useful in imparting timely expert advice to facilitate improved patient care. In countries like India which face the challenge of providing quality care to remote areas while utilizing an over-burdened medical task force, a cost-effective set-up like ours can be instrumental in bringing the paradigm shift.
References
Introduction: overview of telemedicine. In: Telemedicine: opportunities and developments in member states: report of the second global survey on e-health 2009. (2010). Global Observatory for eHealth Series, 2; Geneva: World Health Organisation. 8–9.
Williams TE Jr, Satiani B (2009) The impending shortage and the estimated cost of training the future surgical workforce. Ann Surg 250:590–597
Augestad KM, Lindsetmo RO (2009) Overcoming distance: videoconferencing as a clinical and educational tool among surgeons. World J Surg 33:1356–1365
Bogen EM, Augestad KM, Patel HRH (2014) Telementoring in education of laparoscopic surgeons: an emerging technology. World J Gastrointest Endosc 6(5):148–155
Challacombe B, Kavoussi L, Patriciu A (2006) Technology insight: telementoring and telesurgery in urology. Nat Clin Pract Urol 3(11):611–617, Review
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Singh, S., Sharma, V., Patel, P. et al. Telementoring: an Overview and Our Preliminary Experience in the Setting Up of a Cost-effective Telementoring Facility. Indian J Surg 78, 70–73 (2016). https://doi.org/10.1007/s12262-015-1429-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-015-1429-y