Abstract
Approximately 80% of patients with pancreatic ductal adenocarcinoma (PDAC) have metastatic disease with poor prognosis, but clinically available biomarkers have not yet been identified. This study was to investigate the clinical significance of FZD1 and CAIX in PDACs. FZD1 and CAIX protein expression was measured using EnVision immunohistochemistry. Positive FZD1 or CAIX expression was significantly higher in PDAC than that in precursor lesions (p < 0.01). Positive FZD1 or CAIX expression was significantly lower in cases with well-differentiated adenocarcinoma, no-metastasis of the lymph node, no-invasion of regional tissues, and TNM I/II stage disease than in cases with poorly-differentiated adenocarcinoma, metastasis and invasion, and TNM stage III+ IV stage disease (p < 0.05 or p < 0.01). The expression of FZD1 positively correlated with CAIX in PDAC (P = 0.000). Univariate Kaplan-Meier analysis showed that FZD1 and/or CAIX expression (p < 0.001) was significantly associated with shorter overall survival (p < 0.05). Cox multivariate analysis showed that differentiation, tumor mass, lymph node metastasis, invasion, TNM stage, FZD1 and CAIX levels negatively correlated with overall survival. Positive FZD1 and CAIX expressions are poor prognostic factors in PDAC patients. FZD1 and CAIX might be important biological markers for the carcinogenesis, metastasis, invasion, and prognosis of PDAC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic ductal adenocarcinomas (PDACs) are highly malignant cancers with poor prognosis [1]. Due to the lack of specific symptoms, only approximately 20%–25% of PDAC patients being diagnosed at an early stage with potentially resectable tumor, whereas most PDACs are diagnosed at advanced stages with metastatic diseases. Palliative treatments, such as chemotherapy and radiotherapy, are the main available treatments for patients with unrectable tumors, but exhibit limited treatment efficacy [2]. The overall survival of patients with PDAC is about one year [3]. The poor prognosis may be partially because the current understanding of the molecular and genetic basis of PDAC is still rather limited.
Interactions between tumor and the tumor microenvironment play important roles in tumor growth and metastasis. Hypoxic microenvironment is a crucial characteristic of solid tumor with rapid growth nature which can promote tumor progression and resistance to therapy [4]. Due to the technical limitations in direct measure of O(2) in tumor tissues, several hypoxia-related endogenous proteins, such as HIF-1alpha, GLUT-1, and CAIX (Carbonic anhydrase IX) have been used as surrogate markers for tumor hypoxia [5]. CAIX is the most active carbonic anhydrases for the CO2 hydration reaction, but its expression in normal tissues is limited. In contrast, CAIX is overexpressed in a variety of solid tumors and exerts a dual role in the growth of hypoxic, CO2 excreting tumors [6]. For example, CAIX produces and maintains an alkyline pHi, a microenvironment favorable for tumor growth and tumor cell invasiveness [7, 8]. As a hypoxia-related marker, CAIX also regulate HIF-1 stabilization and activation of its downstream signaling. Moreover, constitutive CAIX expression has been demonstrated to lead to epithelial–mesenchymal transition (EMT) in cervical carcinoma cells [9]. Therefore, it is not surprising that CAIX expression is associated with the progression and metastasis of various human tumor types [10,11,12,13,14] and has been identified as marker for poor prognosis of some malignant lesions [15,16,17,18]. Although two recent studies investigated the expression of CAIX in pancreatic cancers, but its clinical significance in PDAC have not been addressed [19, 20].
The Wingless-type (Wnt) genes encode 19 highly conserved secreted ligands that function through binding to 10 transmembrane receptors of the Frizzled (FZD1–10) family and two co-receptors, LRP5 and LRP6 [21]. The Wnt signaling pathway is widely known to play a key role in controlling proliferation and migration of tumor cells [21, 22]. The Wnt signaling is regulated by hypoxia and involved in EMT in tumors. For example, Wnt/beta-catenin was reported to be involved in the proliferation of hippocampal neural stem cells induced by hypoxia [23]. FZD1 gene was up-regulated in mesenchymal stromal cells after short-term hypoxic stress [24]. Liu et al. study in gastric cancer cells demonstrated that hypoxia regulates the Wnt/β-catenin pathway, whereas Wnt/β-catenin pathway can control HIF-1α expression [25]. In addition, upregulation of Wnt1 and FZD1–4 expression was observed to be associated with the EMT phenotype in radioresistant esophageal cancer cells, suggesting that acquisition of radioresistance and EMT in esophageal cancer cells is associated with the activation of the Wnt/β-catenin pathway [26]. Several studies have shown that overactivation of the Wnt signaling pathway is more prominently due to the overexpression of different FZD receptors in cancers [27,28,29]. The up-regulation of the FZD1 receptor was observed in breast cancer [8] and in poorly differentiated colon cancer [30]. However, the expression of FZD1 and its clinical significance in PDAC have not been reported. Importantly, both CAIX and FZD1 are associated with hypoxia and EMT. Investigation of their relationship in PDAC may provide a chance to understand the molecular and genetic basis of PDAC.
In this study, the expressions of FZD1 and CAIX in resection specimens, including adenocarcinoma, peritumoral tissue, precursor pancreatic lesions, and normal pancreatic tissues were examined using immunohistochemistry. The correlation of FZD1 and CAIX levels with the clinical characteristics of PDAC was analyzed.
Material and Methods
Ethics
This study was pre-approved by the Ethics Committee for Human Study of Central South University.
Sample Collections
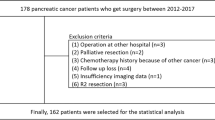
One hundred and six pancreatic ductal adenocarcinomas, thirty-five peritumoral tissues, fifty-five precursor pancreatic tissues, and thirteen normal pancreatic tissues were obtained at the Second and third Xiangya Hospitals, Central South University. Among the one hundred and six adenocarcinomas, sixty-one tissues were collected from male patients (57.5%) and forty-five from female patients (42.5%) with an average age of 54.50 ± 11.53 years. Histopathologic subtypes of the one hundred and six adenocarcinomas include: 38 well-differentiated adenocarcinomas (35.8%), 35 moderately-differentiated adenocarcinomas (33%), and 33 poorly-differentiated adenocarcinomas (31.1%). Invasion and lymphnode metastases were evaluated according to standard criteria [19]. Among the 106 cases with adenocarcinomas, 11 cases (10.4%) were T1, 41 cases (39.6%) were T2, 37 cases (34.9%) were T3, and 16 cases (15.1%) were T4 stage tumors. Of the 106 adenocarcinomas, 29 cases (27.5%) had regional lymph node metastasis, and 64 cases (60.4%) had invasion to surrounding organs and tissues. Thirty-five peritumoral tissues were collected ≥2 cm from the tumors of the 106 adenocarcinoma patients. Twelve of the 35 peritumoral tissues were normal, ten were PanINs (pancreatic intraepithelial neoplasms) grade I, eight were PanINs grade II, and five were PanINs grade III. Survival information was obtained through letters and phone calls from all patients with adenocarcinoma.
Fifty-five precursor pancreatic tissues were collected from 29 (52.7%) male and 26 (47.3%) female cases. Of the 55 cases, 13 (23.6%) had an age ≤ 45 years and forty-two (76.4%) had an age > 45 years. The 55 precursor tissues included 20 chronic pancreatitis tissues (36.4%), 20 adenomas (36.4%), and 15 intraepithelial neoplasias (27.3%). Ten, six, and four of the 20 chronic pancreatitis tissues were mild, moderate, and severe pancreatitis, respectively. The 20 adenomas included five mucinous adenomas and 15 serous adenomas. Four, three, and two of the 20 adenomas had mild, moderate, and severe dysplasia, respectively. Among the 15 intraepithelial neoplasias, six had grade I, five had grade II, and four had grade III intraepithelial neoplasia. Thirteen normal pancreatic tissues were collected from surgery of the twenty pancreatic adenomas. All tissues were treated with 4% formaldehyde for 24 to 48 h followed by 10% formalin solution, and were then embedded in paraffin.
Twenty fresh specimens of pancreatic ductal adenocarcinomas and 13 fresh normal pancreatic tissues were obtained at the Second and third Xiangya Hospitals, Central South University.
Immunohistochemistry
Rabbit anti-human FZD1 and rabbit anti-human CAIX polyclonal antibody were purchased from Dako Corporation (Carpentaria, CA, USA). Immunohistochemistry of FZD1 and CAIX was performed using EnVision™ Detection kit from Dako Laboratories (CA, USA) by following the user manual. Positive controls were provided with the EnVision™ Detection Kit. Briefly, four μM-thick sections were cut from paraffin-embedded tissues. The sections were deparaffinized and then incubated with 3% H2O2 in the dark for 15 min. The antigen retrieval was conducted with sodium citrate buffer (10 mM Sodium citrate, 0.05%Tween 20, pH 6.0) at 96 °C for 30 min. The sections were incubated with rabbit anti-human FZD1 or CAIX primary antibody (1:100 dilution) for 1 h after soaked in PBS for 3 × 5 min. The sections were then incubated with several drops of Solution A (ChemMate™ EnVison+/HRP) for 30 min followed by DAB staining and haematoxylin counter-staining. The sections were dehydrated, soaked in xylene, and mounted with neutral balsam. Five hundred cells from ten random fields of each section were examined by two investigators independently. An average of the percentage from these two investigators was used for final evaluation. Cases with positive cells ≥25% were considered positive whereas cases with positive cells <25% were considered negative [25,26,27,28].
Western Blot
Total protein was extracted from 20 fresh specimens of pancreatic ductal adenocarcinomas and 13 fresh normal pancreatic tissues by lysing with RIPA sample buffer (50 mmol/1 Tris-HCL, pH 8.0, 150 mmol/1 NaCl, 1 mmol phenylmethylsulfony fluoride, 50 mmol/l DDT, and 1% Triton X-100) on ice for 30 min. The supernatant was collected after centrifugation at 14,000 g at 4 °C for 10 min. Protein concentration was determined using Bradford Protein Assay Kit (Beyotime Institute of Biotechnology, China). Fifty microgram of protein were mixed with 2 × SDS loading buffer and incubated at 100 °C for 10 min before electrophoresis in 11.5% polyacrylamide gels. Proteins were electrotransferred onto PVDF membranes (Invitrogen, USA). Membranes were blocked for 1 h at room temperature with 5% non-fat milk in Tris buffer saline buffer (TBS) (20 mmol/l tris-HCl, 150 mmol/l NaCl, and 0.1% Tween-20). Membranes were then incubated overnight at 4 °C with anti-FZD1 and anti-CAIX (Abgent Company, CA, USA), followed by incubation with horseradish peroxidase-conjugated secondary antibody (Protintech, USA) respectively. Membranes were then washed with TBS buffer and signals were visualized using the enhanced chemiluminescence system (Santa Cruz, USA). The visualized bands were quantified by BANDSCAN software. The signal intensity was normalized to beta-actin.
Statistical Analysis
Data were analyzed using the SPSS 17.0 (statistical package for the Social Sciences, Version 17.0). The inter-relationship of FZD1 and CAIX with histological or clinical factors was analyzed using χ2 test or Fisher’s exact test. The overall survival of patients with PDAC was analyzed using Kaplan-Meier univariate survival analysis and log-rank tests. Multivariate analysis was performed with Cox proportional hazards model and the 95% confidence interval was calculated. A p < 0.05 was considered statistically significant.
Results
FZD1 and CAIX Protein Expression in Adenocarcinoma and Normal Pancreatic Tissues
Western blots showed that the expression levels of FZD1 and CAIX were significantly higher in pancreatic ductal adenocarcinoma (0.865 ± 0.031, 0.934 ± 0.035, respectively) than that in normal pancreatic tissues (0.334 ± 0.023, 0.354 ± 0.029) (p < 0.01). FZD1 and CAIX expressions were significantly higher in pancreatic ductal adenocarcinoma than that in normal pancreatic tissues (Fig. 1).
Western blots of FZD1 and CAIX protein expression. a Representative Western blot of CAIX, FZD1, and β-actin expression. b Semi-quantitative analysis of FZD1 protein expression in Western blot. c Semi-quantitative analysis of CAIX protein expression in Western blot. PDAC: Pancreatic ductal adenocarcinoma tissues. NPT: normal pancreatic tissues
FZD1 and CAIX Protein Expression in Adenocarcinoma, Peritumoral, Precursor, and Normal Pancreatic Tissues
Immunohistochemical staining showed that positive FZD1 and CAIX expressions were located in the cytoplasm (Figs. 2 and 3). Of the 106 adenocarcinomas, 58 and 60 were FZD1 (54.7%) and CAIX (56.6%) positive, respectively. In the 35 peritumoral tissues, ten and nine were FZD1 (28.6%) and CAIX (25.7%) positive, respectively. Of the 55 precursor pancreatic lesions, 11 and 13 were FZD1 (20.0%) and CAIX (23.6%) positive, respectively. FZD1 and CAIX was negatively expressed in all 13 normal tissues. The positive rates of FZD1 or CAIX was significantly higher in adenocarcinomas than that in peritumoral (P = 0.006 and P = 0.001, respectively), precursor (P = 0.000), and normal pancreatic tissues (P = 0.000) (Table 1). Peritumoral tissues and precursor pancreatic lesions with positive FZD1 and/or CAIX expression exhibited moderate to severe dysplasia and grade II or III intraepithelial neoplasia (Table 1). Among the 55 precursor lesions, the positive rate of FZD1 and CAIX in chronic pancreatitis, adenomas, and intraepithelial neoplasia were 15.0% (3/20) and 10.0% (2/20), 20.0% (4/20) and 20.0% (4/20), 26.7% (4/15), and 20.0% (3/15), respectively. No significant differences in the positive rate of FZD1 and CAIX were observed between three types of precursor lesions (P > 0.05).
Immunohistological staining of FZD1 protein expression. a Positive expression of FZD1 in moderately-differentiated PDAC, magnification ×200. b Negative FZD1 expression in well differentiated PDAC, magnification ×200. c The positive FZD1 expression in serous adenoma, magnification ×200. d The positive FZD1 expression in chronic pancreatitis, magnification ×200
Immunohistological staining of CAIX protein expression. a Positive CAIX expression in poor-differentiated PDAC, magnification ×200. b Negative CAIX expression in well differentiated PDAC, magnification ×200. c The positive CAIX expression in intraepithelial neoplasia II, magnification ×200. d The positive CAIX expression in peritumoral tissue, magnification ×200
FZD1 and CAIX Protein Expressions Were Associated with Clinicopathological Characteristics of Pancreatic Ductal Adenocarcinomas
As shown in Table 2, positive rates of FZD1 and CAIX expression were significantly lower in cases with well-differentiated adenocarcinoma, no metastasis in lymph node, no invasion to surrounding tissues and organs, and TNM I + II stage disease compared to cases with poorly-differentiated adenocarcinoma, lymph node metastasis, invasion, and TNM III or IV stage disease (p < 0.05 or p < 0.01). The expressions of FZD1 and CAIX exhibited no significant association with sex, age and tumor mass (p > 0.05). Among the 58 cases with positive FZD1 expression, 46 cases had positive CAIX expression. Among the 48 cases with negative FZD1 expression, 34 cases had negative CAIX expression. The expression of FZD1 was positively correlated with CAIX (P = 0.000).
FZD1 and CAIX Protein Expressions Correlated with Overall Survival in Patients with Pancreatic Ductal Adenocarcinomas
Survival information was collected from all PDAC patients. Twenty-nine patients survived over one year, but 77 patients died within one year. The mean overall survival time of 106 PDAC patients was 9.44 ± 0.69 months. Kaplan-Meier survival analysis revealed that the differentiation, tumor size, lymph node metastasis, invasion, and TNM stage were significantly associated with the average overall survival time of patients with pancreatic ductal adenocarcinoma (P < 0.05 or P < 0.01) (Table 3). Average overall survival time for FZD1 or/ and CAIX positive patients was significantly lower than those with negative FZD1 / and CAIX expression (P < 0.05) (Table 3, Fig. 4). Cox multivariate analysis showed that tumor mass > 5 cm, poor differentiation, lymph node metastasis, invasion, and high TNM stage (III or IV) negatively correlated with overall survival and positively correlated with mortality. Positive FZD1 and CAIX expression negatively correlated with overall survival and positively correlated with mortality. Both FZD1 and CAIX positive expression are independent prognostic factors (Table 4).
FZD1and CAIX expression and survival in patients with PDAC. a Kaplan-Meier plots of overall survival in patients with PDAC and with positive and negative FZD1 expression. b Kaplan-Meier plots of overall survival in patients with PDAC and with positive and negative CAIX expression. c Kaplan-Meier plots of overall survival in patients with PDAC and with FZD1(+) + CAIX(+) and FZD1(−) + CAIX (−) expression
Discussion
The attempts to identify biomarkers for the diagnosis, target therapy, and prognosis prediction of cancers including pancreatic cancer have recently been widely reported. However, a clinically available biomarker for the indication of malignancy has not been established in PDAC. Thus, it is significant to continuously identify biomarkers in PDAC. This study suggests that CAIX and FZD1 are two closely associated molecules involved in the progression of PDAC and can be a predictive biomarker for the poor prognosis of patients with PDAC.
Previous studies revealed some interactions between CAIX, hypoxia, and Wnt signaling. For example, both CAIX and FZD1 are regulated by hypoxia [5, 6, 23,24,25]. In addition, these two molecules are associated with EMT in tumor cells [9, 26]. These findings may imply that changes in O(2) and pH in the microenvironment of tumor tissues may collaborate in tumor cell proliferation, tumor growth, and tumor cell metastasis. In this study, both CAIX and FZD1 protein were overexpressed in PDAC tumor tissues compared to the benign and normal pancreatic tissues. Moreover, the expression of FZD1 significantly correlated with CAIX expression in PDAC tumor tissues (P = 0.000). The positive rates of FZD1 and CAIX expression were significantly higher in PDAC patients with poorly-differentiated adenocarcinoma, with lymph node metastasis, invasion and high TNM stage, suggesting that both FZD1 and CAIX expression are associated with the progression and an advanced disease of PDAC. Therefore, pH and hypoxia are the crucial factors affecting tumor microenvironment, and subsequently affect the malignancy of PDAC.
The Wnt/β-catenin pathway serves important functions in multiple biological processes, including regulation of cell proliferation, differentiation, and migration [31]. FZD receptors are responsible for the overactivation of the Wnt signaling pathway [27,28,29]. Upregulation of the FZD1 receptor was previously observed in several cancers, such as breast cancer and poorly differentiated colon cancer [30]. As a result, β-catenin accumulates in the cytoplasm and subsequently translocates into the nucleus, where it regulates the transcription of target genes, including genes related to activation of EMT. This study in first showed that FZD1 was involved in the differentiation, metastasis, invasion, and poor prognosis.
CAIX is activated by hypoxia inducible factor-1(HIF1), and can regulate the pH within and outside cells. Via intracellular alkalization and extracellular acidification, CAIX can help tumor cells adapting to acidic and hypoxic environments, thereby contributing to tumor growth and progression [12, 16, 17]. CAIX is rarely expressed In normal human tissues, but is overexpressed in many malignant tumors such as hepatocellular and renal cell carcinoma, cervical and lung cancer [12, 16,17,18]. Through interaction with β-catenin, CAIX can also reduce E-cadherin expression. Reduction or loss of E-cadherin, an important adhesion molecule, weakens intercellular adhesion, strengthening tumor cell metastases and invasiveness [32, 33]. Although the expression of CAIX in pancreatic tumor tissues has previously been reported, its association with the differentiation, invasion, metastasis, and prognosis has not been addressed. This study first demonstrated that CAIX is associated with the progression and advanced disease of PDAC and a poor prognostic marker in patients with PDAC.
This study also found that peritumoral tissues and precursor pancreatic lesions with positive FZD1 and CAIX expressions exhibited moderate to severe dysplasia or grade II or III intraepithelial neoplasia, suggesting that both FZD1 and CAIX play a role in the carcinogenesis. This study also demonstrated that not only the percentage of positive FZD1 and CAIX was significantly increased in PDAC patients, but also the FZD1 and CAIX protein expression was significantly elevated in tumor tissues. Together with the findings that positive FZD1 and CAIX expression was associated with the progression and poor prognosis, FZD1 and CAIX may function as a oncogene in PDAC and a biomarker for the diagnosis, progression, and poor prognosis of PDAC.
In conclusion, positive FZD1 and CAIX are important prognostic factors for poor prognosis of patients with PDAC.
References
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ (2009) Cancer statistics, 2009. CA Cancer J Clin 59:225–249
Puleo F, Maréchal R, Demetter P, Bali MA, Bali MA, Calomme A, Closset J, Bachet JB, Deviere J, Van Laethem JL (2015) New challenges in perioperative management of pancreatic cancer. World J Gastroenterol 21:2281–2293
Von Hoff DD, Ervin T, Arena FP et al (2013) Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med 369:1691–1703
Kahlert UD, Mooney SM, Natsumeda M, Steiger HJ, Maciaczyk J (2017) Targeting cancer stem-like cells in glioblastoma and colorectal cancer through metabolic pathways. Int J Cancer 140:10–22
Eckert AW, Kappler M, Schubert J, Taubert H (2012) Correlation of expression of hypoxia-related proteins with prognosis in oral squamous cell carcinoma patients. Oral Maxillofac Surg 16:189–196
McDonald PC, Winum JY, Supuran CT, Dedhar S (2012) Recent developments in targeting carbonic anhydrase IX for cancer therapeutics. Oncotarget 3:84–97
Parks SK, Chiche J, Pouyssegur J (2011) pH control mechanisms of tumor survival and growth. J Cell Physiol 226:299–308
Swietach P, Patiar S, Supuran CT, Harris AL, Vaughan-Jones RD (2009) The role of carbonic anhydrase 9 in regulating extracellular and intracellular ph in three-dimensional tumor cell growths. J Biol Chem 284:20299–20310
Shin HJ, Rho SB, Jung DC, Han IO, Oh ES, Kim JY (2011) Carbonic anhydrase IX (CA9) modulates tumor-associated cell migration and invasion. J Cell Sci 124:1077–1087
Pastorekova S, Parkkila S, Pastorek J, Supuran CT (2004) Carbonic anhydrases:current state of the art, therapeutic applications and future prospects. J Enz Inhib Med Chem 19:199–229
Potter C, Harris AL (2004) Hypoxia inducible carbonic anhydrase IX, a marker of tumour hypoxia, survival pathway and therapy target. Cell Cycle 3:164–167
Lehtonen J, Shen B, Vihinen M, Casini A, Scozzafava A, Supuran CT, Parkkila AK, Saarnio J, Kivela AJ, Waheed A, Sly WS, Parkkila S (2004) Characterization of CAXIII, a novel member of the carbonic anhydrase isozyme family. J Biol Chem 279:2719–2727
Tureci O, Sahin U, Vollmar E, Siemer S, Gottert E, Seitz G, Parkkila AK, Shah GN, Grubb JH, Pfreundschuh M, Sly WS (1998) Human carbonic anhydrase XII: cDNA cloning, expression, and chromosomal localization of a carbonic anhydrase gene that is overexpressed in some renal cell cancers. Proc Natl Acad Sci USA 95:7608–7613
Opavsky R, Pastorekova S, Zelnik V, Gibadulinova A, Stanbridge EJ, Zavada J, Kettmenn R, Pastorek J (1996) Human MN/CA9 gene, a novel member of the carbonic anhydrase family: structure and exon to protein domain relationships. Genomics 33:480–487
Supuran CT (2008) Carbonic anhydrases-an overview. Curr Pharm Des 14:603–614
Leppilampi M, Saarnio J, Karttunen TJ, Kivelä J, Pastoreková S, Pastorek J, Waheed A, Sly WS, Parkkila S (2003) Carbonic anhydrase isozymes IX and XII in gastric tumors. World J Gastroenterol 9:1398–1403
Span PN, Bussink J, Manders P (2003) Carbonic anhydrase IX expression levels and prognosis in human breast cancer: association with treatment outcome. Br J Cancer 89:271–276
Liao SY, Darcy KM, Randall LM, Tian C, Monk BJ, Burger RA, Fruehauf JP, Peters WA, Stock RJ, Stanbridge EJ (2010) Prognostic relevance of carbonic anhydrase-IX in high-risk, early-stage cervical cancer:a Gynecologic Oncology Group study. Gynecol Oncol 116:452–458
Yokoyama S, Higashi M, Kitamoto S et al (2016) Aberrant methylation of MUC1 and MUC4 promoters are potential prognostic biomarkers for pancreatic ductal adenocarcinomas. Oncotarget 7:42553–42565
Yu M, Zhou Q, Zhou Y, Fu Z, Tan L, Ye X, Zeng B, Gao W, Zhou J, Liu Y, Li Z, Lin Y, Lin Q, Chen R (2015) Metabolic phenotypes in pancreatic cancer. PLoS One 10:e0115153
Hoang BH, Kubo T, Healey JH, Sowers R, Mazza B, Yang R, Huvos AG, Meyers PA, Gorlick R (2004) Expression of LDL receptor-related protein 5 (LRP5) as a novel marker for disease progression in high-grade osteosarcoma. Int J Cancer 109:106–111
Salsano E, Paterra R, Figus M, Menghi F, Maderna E, Pollo B, Solero CL, Massimi L, Finocchiaro G (2012) Expression profile of frizzled receptors in human medulloblastomas. J Neuro oncol 106:271–280
Udartseva OO, Andreeva ER, Buravkova LB (2015) WNT-associated gene expression in human mesenchymal stromal cells under hypoxic stress. Dokl Biochem Biophys 465:354–357
Cui XP, Xing Y, Chen JM, Dong SW, Ying DJ, Yew DT (2011) Wnt/beta-catenin is involved in the proliferation of hippocampal neural stem cells induced byhypoxia. Ir J Med Sci 180:387–393
Liu HL, Liu D, Ding GR, Liao PF, Zhang JW (2015) Hypoxia-inducible factor-1α and Wnt/β-catenin signaling pathways promote the invasion of hypoxic gastriccancer cells. Mol Med Rep 12:3365–3373
Su H, Jin X, Zhang X, Zhao L, Lin B, Li L, Fei Z, Shen L, Fang Y, Pan H, Xie C (2015) FH535 increases the radiosensitivity and reverses epithelial-to-mesenchymal transition of radioresistant esophageal cancer cell line KYSE-150R. J Transl Med 13:104
Milovanovic T, Planutis K, Nguyen A, Marsh JL, Lin F, Hope C, Holcombe RF (2004) Expression of Wnt genes and frizzled 1 and 2 receptors in normal breast epithelium and infiltrating breast carcinoma. Int J Oncol 25:1337–1342
Merle P, Kim M, Herrmann M, Gupte A, Lefrançois L, Califano S, Trépo C, Tanaka S, Vitvitski L, de la Monte S, Wands JR (2005) Oncogenic role of the frizzled-7/beta-catenin pathway in hepatocellular carcinoma. J Hepatol 43:854–862
Ueno K, Hiura M, Suehiro Y, Hazama S, Hirata H, Oka M, Imai K, Dahiya R, Hinoda Y (2008) Frizzled-7 as a potential therapeutic target in colorectal cancer. Neoplasia 10:697–705
Holcombe RF, Marsh JL, Waterman ML, Lin F, Milovanovic T, Truong T (2002) Expression of Wnt ligands and frizzled receptors in colonic mucosa and in colon carcinoma. Mol Pathol 55:220–226
Liu H, Chen Y, Zhou F, Jie L, Pu L, Ju J, Li F, Dai Z, Wang X, Zhou S (2014) Sox9 regulates hyperexpression of Wnt1 and Fzd1 in human osteosarcoma tissues and cells. Int J Clin Exp Pathol 7:4795–4805
Svastova E, Zilka N, Zat’ovicova M, Gibadulinová A, Ciampor F, Pastorek J, Pastoreková S (2003) Carbonic anhydrase IX reduces E-cadherin-mediated adhesion of MDCK cells via interaction with b-catenin. Exp Cell Res 290:332–345
Jain RK (1999) Transport of molecules, particles, and cells in solid tumours. Annu Rev Biomed Eng 1:241–321
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, L., Yang, Z., Li, D. et al. Overexpression of FZD1 and CAIX are Associated with Invasion, Metastasis, and Poor-Prognosis of the Pancreatic Ductal Adenocarcinoma. Pathol. Oncol. Res. 24, 899–906 (2018). https://doi.org/10.1007/s12253-017-0284-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-017-0284-5