Abstract
To investigate the most commonly used technique, the wire-guided localization (WGL) in non-palpable breast cancer. To analyze the effective factors on positive surgical margins in our practice and determine the surgical learning curve of this method. Prospective consecutive study was performed from January 2005 to December 2011. Inclusion criteria was a non-palpable breast lesion with malignancy on preoperative histology. All lesions were localized by ultrasound or stereotactic guided wire placement. Margins 1 mm or closer were accepted as positive margins which required re-excision. To determine the learning curve of WGL method we investigated the change in the reoperation rate after primary procedure performed by “high-volume” surgeon. Two hundred and fourteen consecutive patients were enrolled. In 23 patients (10.7 %) reexcision was needed. Positive surgical margins were significantly influenced by the patient’s age (p = 0.03), tumor volume (p < =0.001), proportion of tumor volume/specimen volume (p < 0.001), presence of DCIS (p < 0.001), multifocality (p = 0.03) and the learning curve (p = 0.006) with univariate analysis. Only the tumor volume, presence of DCIS and the learning curve were proved as independent prognostic factor for reoperation by multivariate analysis. The reoperation rate decreased below 20 % after the fortieth operation. Results of our single institutional study suggest, that this localization technique can be performed safely with very good results after 40 procedures as a learning curve for surgeons.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
More than 1.1 million new patients are diagnosed with breast cancer every year in the world, one quarter of them in Europe [1]. The widespread application of breast screening programs resulted in an increased proportion of non-palpable breast cancers representing 25–35 % of all cases at diagnosis [2]. Most of these tumors are node negative so, this early detection can diminish the mortality rate by rates up to 20 % [3].
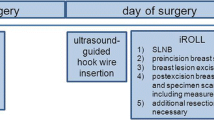
Removal of these lesions with clear surgical margin requires an adequate localization method. The wire-guided localization (WGL) and the radio-guided localization (RGL) are the most commonly used techniques.
Most of the randomized controlled trials demonstrated inacceptably high proportion of positive surgical margins (37.5–57.7 %) with the wire-guided localization (WGL) technique therefore they preffered the radio-guided localization (RGL) [4–6]. In addition, there is a heterogenety of study designs and endpoints, study sample sizes were small and there was an inconsistent use of definitions of a positive margin [7].
Based on these findings we started a prospective, single-institutional study to investigate our results of the most commonly used technique, the WGL method in more than 200 patients. We analyzed the factors associated with positive surgical margins, such as age of the patient, histological type of the tumor, size and volume of the lesion, volume of the removed specimen, position of the tumor, the presence of multifocality and the effect of learning curve period. We evaluated the number of reoperations according to the surgeon’s experience and tried to determine the learning curve of the WGL method as a change in the reoperation rate after primary procedure performed by “high-volume” surgeon.
Methods
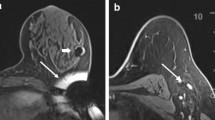
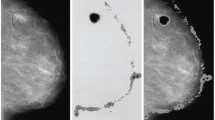
The study was conducted prospectively from January 2005 to December 2011 at the Department of General Surgery of Kenézy Teaching County Hospital, Debrecen, Hungary. Inclusion criteria was a non-palpable breast lesion with malignancy on preoperative histology. An informed consent form was signed by all patients, in compliance with the Helsinki Declaration of 1964. Mammography was done with GE Senograph 700 T Mammo Unit and later with GE alpha-RT Unit and Profect type (FUJI) phosphorous-disc digital technology. Complementary radiograms (aimed-enlarged and lateral ones), breast and axillary ultrasound (US) examination were done with Siemens Adara device. Core biopsies were done from the breast lesions, 2 to 5 cores per case were extracted with Bard Magnum 14G needle instrument. In cases with suspected axillary metastasis US guided fine needle aspiration biopsy (FNAB) were performed from the lymph nodes with 23G needle by Cameco syringe pistol in local anaesthesia. Two samples per patient were retrieved and fixed in alcohol immediately. These preoperative percutaneous biopsies were done by the same radiologist and were analysed by the same pathologist as well as the postoperative specimens.
All lesions were localized by ultrasound or stereotactic guided wire placement. A hooked wire was inserted into the non-palpable breast lesion by the radiologist just prior to surgery. The correct position of the wire was verified by mammography. Then all the lesions were excised with the guidance of the hook. The medial, lateral and superior surgical margins of the specimens were marked with sutures and the surgical specimens were sent to specimen mammography. Finally, all the specimens were sent for histopathological examination. Margins 1 mm or closer were considered as positive margins which required re-excision. Specimen volumes and tumor volumes were calculated by multiplying the three dimensions of the specimen and lesion mentioned in the pathology report.
In cases with indication of sentinel lymph node biopsy (SNB) the sentinel nodes were labeled with blue dye (Bleu Patenté V Sodique Guerbet 2,5 %, F-95943 Roissy CdG, cedex, France) and intraoperative frozen section examinations were performed [8].
To determine the learning curve of WGL method we analyzed only one surgeon’s (“high-volume” surgeon) practice from his first procedure till the end of study. The learning curve period was defined as the reoperation rate should be less than 20 %, constantly.
To evaluate the effect of surgical experience we compared the reoperation rate of different surgeons (residents, consultants, “high-volume” surgeon in and after the learning curve period).
Statistical analysis for unadjusted comparisons of the outcome groups (negative and positive margin rates) in terms of categorical variables, Fisher exact tests were used; Student’s t tests or Wilcoxon’s rank-sum tests were used for comparisons in terms of continuous variables, subject to normality assumptions being satisfied. Adjusted analysis was based on logistic regression with margin positivity as the outcome. Age was used as an a priori explanatory variable. Other variables were added and kept in the model unless found to have neutral behavior (no role as adjustment factors and no meaningful effect). Tumor volume was logarithmically (natural base) transformed to improve normality; quadratic and cubic terms of log tumor volume and age were included in the model to improve fit. Model checking was based on the Hosmer-Lemeshow goodness-of-fit test and marginal model plots. Significance was considered at p < 0.05.
Results
Patients
Two hundred and fourteen consecutive patients were enrolled with non-palpable breast cancer. Mean age of the patients was 59 years (range between 31 and 83 years). In 133 patients (62.1 %) invasive ductal carcinoma (IDC), in 25 patients (11.6 %) invasive lobular carcinoma (ILC), in 47 patients (22 %) ductal carcinoma in situ (DCIS), in one patient lobular carcinoma in situ (LCIS) and in 8 patients other types of invasive carcinoma were found.
The insertion of wire was performed under US or stereotactic guidance. The success rate was 100 %. In 11 patients two wires were inserted localizing the margins of extended DCIS with microcalcification. There were no such complications as displacing, migration of wire, or pneumothorax.
Tumor Characteristics
Mean pathological tumor size was 13*15 mm (range: 4 mm*1 mm – 43 mm*43 mm), mean pathological tumor volume was 3.23 ccm (range: 0.008 ccm – 72.1 ccm) and the mean removed breast specimen volume was 34.1 ccm (range: 11.1 ccm – 181.4 ccm). The mean proportion of tumor volume/specimen volume was 6.28 %. In 12 patients (5.6 %) multifocality of the tumor was proved. The T-stage, N-stage, receptor and c-erb2 status of lesions are presented in Table 1.
Procedures
During the period of this study (2005–2011) the number of primary operative procedures increased from 22 to 41 yearly, while the reoperation rate decreased from 27 to 9.7 %.
We performed breast conserving surgery (BCS) in 205 patients (95.3 %) and in 9 cases subcutaneous mastectomy was done (nipple-areola complex was preserved in 5 patients). Mean duration of surgical excision was 31.8 min (range: 21 min −54.9 min). Surgical site infection occured in 4 cases (1.86 %) and in 3 cases (1.4 %) reoperation was needed because of postoperative bleeding.
In 23 patients (10.7 %) positive surgical margins were proved by postoperative histological examination. In 5 cases mastectomy and in 17 cases reexcision were performed with adequate clear margins. One patient refused the reexcision. Residual tumor was found in 14/22 cases (63.6 %). In 3 patients low grade DCIS, in 4 patients high grade DCIS and in 7 cases invasive ductal carcinoma were found in the reexcised specimen.
Statistical Analysis
Table 2 shows the characteristics of tumors, the position of lesions and the learning curve’s results in correlation with surgical margins. Differences between the cohorts of patient with clear and positive surgical margins were statistically significant with univariate analysis in patients’ age (p = 0.036), tumor volume (p = 0.0007), proportion of tumor volume/specimen volume (p < 0.0001), presence of DCIS (p = 0.0007) and multifocality (p = 0.0283). The presence of IDC was a significant factor for clean margin (p = 0.0221). Neither the tumor size (<=5 mm or >5 mm) nor the position influenced the surgical margin (p > 0.99; p = 0.193). However, the 0.25 ccm of tumor volume has the lowest risk for reoperation, while the tumor volume is more or less than 0.25 ccm the risk increased significantly with multivariate analysis (Fig. 1). Logistic regression showed that beside of tumor volume the presence of DCIS was an independent prognostic factor of positive surgical margin too (Table 3).
Logistic regression estimates (solid curve) of log odds of repeat surgery due to positive surgical margins as a function of tumor volume for patients with sample average levels of other covariates (DCIS, operating surgeon, age at surgery). Horizontal reference line indicates log odds for a patient with sample average values of all covariates. CI confidence interval, TuV tumor volume, DCIS ductal carcinoma in situ
Learning Curve and Surgical Experience
We estimated the learning curve of WGL method by the proportion of reoperated cases in the operative serie of the “high-volume” surgeon. He reached a 20 % of reoperation rate first after 30 procedures; however, this rate decreased constantly below 20 % after the fortieth operation and after the seventieth procedure the reoperation rate decreased to 10 % (Fig. 2).
The “high-volume” surgeon’s reoperation rate along this study was 9.1 % (11/121), while the consultants’ rate was 10.1 % (7/69) and reoperation was needed in 20 % (5/25) of patients who were operated by residents. The difference between these reoperation rates were not significant (p = 0.277). However, the difference of “high-volume” surgeon’s reoperation rate between in the learning curve and after this period was statistically significant (p = 0.006) with univariate analysis. Logistic regression showed that the learning curve and resident versus “high-volume” surgeon (after learning curve) were independent prognostic factors of positive surgical margin (Table 3).
Discussion
Suspicious, clinically occult breast lesions are being found more and more frequently as a result of widespread mammographic screening programs of asymptomatic women and 15–20 % of these lesions are malignant, so they should be removed [9]. The aim of surgical treatment in a non-palpable breast cancer is to remove the marked lesion with negative surgical margins as well as achieving a good cosmetic result.
WGL is presently the most commonly used localization method for non-palpable breast lesions [9, 10]. However, the placement of the wire is difficult in dense breast tissue [11] and the wire may be displaced during surgery and a migration or rupture of the wire may lead to pneumothorax and patient discomfort has been described [12–14].
In our study, which is the one of the largest single institutional study in the literature representing WGL technique, the localization was successful in 100 % of patients. In 11 patients (5 %) 2 wires were needed to localize the margins because of extended DCIS lesions with microcalcification. This marking could not be performed adequately with RGL method because of superponation of radioactive foci, or an unacceptably large volume of healthy breast tissue should have been removed.
We found a 10.7 % of positive surgical margins in a series of 214 patients using the WGL method and we were able to manage most of these patients by reexcision with clear surgical margins and mastectomy was needed only in 20 %. This is a better result than in a cohort study of 55 297 patients analyzing the reoperation rate after BCS in English NHS trusts, where about 40 % of the patients requiring reoperation had mastectomy [15].
Logistic regression analysis showed that positive surgical margins were significantly influenced by the presence of DCIS, the tumor volume and the learning curve period only. The presence of DCIS means a 4.4 odds ratio for reoperation. This finding demonstrated a higher odds ratio, than in the literature [15]. In our study the lesion’s position and tumor size (<=5 mm or >5 mm) were not significant risk factors for failure (p = 0.193; p > 0.99) as opposed to other RGL studies [16, 17]. However, we found that the 0.25 ccm of tumor volume was a critical size for the minimal risk for reoperation (Fig. 1). Less than 0.25 ccm (0.0625 ccm vs 0.25 ccm) or more than 0.25 ccm (4 ccm or more) of tumor volume were an independent prognostic factor of positive surgical margin (Table 3). This effect -as a larger size tumors are prognostic factors for reexcision- is well known from the literature. Extensive intraductal component, lymphovascular invasion, presence of DCIS or simply the larger tumor size are the most important factors regarding margin positivity [18–20]. On the other hand, surgeons are forced to perform BCS with good cosmetic outcome in patients with larger tumors too, and it can result a higher rate of involved surgical margin.
Specimen volume in wire-guided breast biopsy is determined by two contradictory aspects. The surgeon aims to obtain histologically clear margins without jeopardizing the previously mentioned cosmesis with an unnecessarily wide excision of surrounding normal breast tissue.
In this study, the mean specimen volume was 34.1 ccm and it was compatible with that of other studies ranging from 9.5 to 73.5 ccm [21].
We demostrated a specific role of patient’s age. The difference for reoperation between young patients (45 years) and 60 years old patients was not statistically significant as a difference between patients with 75 years and 60 years. But the odds ratios (OR:2.14, OR:0.75) for positive surgical margins showed that the elderly patients have a lower risk for reoperation. These results could be origined from the wider surgical excisions, because of the cosmetic results were not so decisive in this cohort of patients.
In the European Society of Breast Cancer Specialists (EUSOMA) statement on quality indicators of breast cancer care it was considered 80 % as minimum standard and 90 % as the target the proportion of patients who received a single (breast) operation for the primary tumor (excluding reconstruction) [22]. To reach this 20 % of reoperation rate in non-palpable breast cancers we investigated the learning curve of WGL method by a “high-volume” surgeon’s experience, as standardizing the circumstances. He reached a 20 % of reoperation rate first after 30 procedures; however, this rate decreased constantly below 20 % after the fortieth operation. While the latest systematic review and meta-analysis demonstrated a 27.5 % of positive surgical margin with WGL method [23], Postma found only 10 % of positive margin in a multicentric study, where the all participated surgeons were dedicated breast surgeons with a great experience with both WGL and ROLL methods [24]. So, we consider, at least forty operations are mandatory for the adequate surgical excision and seventy procedures make the surgeon sure of mastering this method.
Evaluating the effect of learning curve period for positive surgical margin we found that these 40 primary procedures have a significantly higher reoperation rate than procedures after the learning curve period with uni- and multivariate analysis too (p = 0.006; p = 0.0266 odds ratio = 6.04; 95 % confidence interval: 1.23–29.6).
The difference of reoperation rate between “high-volume” surgeon (9.1 %), consultants (10.1 %) and residents (20 %) was not statistically significant and it was similar to results described in the literature [25, 26]. This non-significant difference could be origined from the small size of sample of residents’ cases and the influence of experienced surgeons’ assistance. However the residents’ rate was twice more than dedicated surgeons’ rate, and we proved the significant effect of learning curve, so these procedures should be reserved for experienced surgeons.
On the other hand, we confirmed that the reoperation rate between experienced consultans and “high-volume” surgeon (after the learning curve) was different with a 3.64 odds ratio for failure. We proved the difference also, between residents and “high-volume” surgeon (after the learning curve) with a 6.33 odds ratio, which was statistically significant (p = 0.042). Based on these findings we found, that the radicality of resection is strongly influenced by the adequate surgical experience, which could be reached after forty operations as a learning curve in patients with non-palpable breast cancer.
Conclusion
Our single institutional study of wire-guided localization method demonstrated a 10.7 % of reoperation rate in a series of 214 consecutive patients with non-palpable breast cancer. This localization technique can be performed safely with very good short term results. Positive surgical margins were significantly influenced by the presence of DCIS, the tumor volume and the learning curve with multivariate analysis. The reoperation rate decreased constantly below 20 % after the fortieth operation. So, we consider, that forty operations are mandatory for mastering the adequate surgical excision after wire-guided localization.
References
Parkin M, Bray F, Ferlay J, Pisani P (2002) Global cancer statistics. Cancer J Clin 55:74–108
Skinner KA, Silberman H, Sposto R, Silverstein MJ (2001) Palpable breast cancers are inherently different from nonpalpable breast cancers. Ann Surg Oncol 8(9):705–710
Blanks RG, Moss SM, McGahan CE, Quinn MJ, Babb PJ (2000) Effect of NHS breast screening programme on mortality from breast cancer in England and Wales, 1990–8: comparison of observed with predicted mortality. BMJ 321:665–669
Gray RJ, Salud C, Nguyen K et al (2001) Randomized prospective evaluation of a novel technique for biopsy or lumpectomy of nonpalpable breast lesions: radioactive seed versus wire localization. Ann Surg Oncol 8(9):711–715
Medina-Franco H, Abarca-Pérez L, García-Alvarez MN, Ulloa-Gómez JL, Romero-Trejo C, Sepúlveda-Méndez J (2008) Radioguided occult lesion localization (ROLL) versus wire-guided lumpectomy for non-palpable breast lesions: a randomized prospective evaluation. J Surg Oncol 97(2):108–111
Ocal K, Dag A, Turkmenoglu O, Gunay EC, Yucel E, Duce MN (2011) Radioguided occult lesion localization versus wire-guided localization for non-palpable breast lesions: randomized controlled trial. Clinics (Sao Paulo) 66(6):1003–1007
Lovrics PJ, Cornacchi SD, Farrokhyar F et al (2009) The relationship between surgical factors and margin status after breast-conservation surgery for early stage breast cancer. Am J Surg 197(6):740–746
Tóth D, Sebő É, Sarkadi L, Kovács I, Kiss C, Damjanovich L (2012) Role of core needle biopsy in the treatment of radial scar. Breast 21(6):761–763
Postma EL, Witkamp AJ, van den Bosch MA, Verkooijen HM, van Hillegersberg R (2011) Localization of nonpalpable breast lesions. Expert Rev Anticancer Ther 11(8):1295–1302
Besic N, Zgajnar J, Hocevar M et al (2002) Breast biopsy with wire localization: factors influencing complete excision of nonpalpable carcinoma. Eur Radiol 12(11):2684–2689
Davis PS, Wechsler RJ, Feig SA, March DE (1988) Migration of breast biopsy localization wire. AJR Am J Roentgenol 150(4):787–788
Rahusen FD, Bremers AJ, Fabry HF, van Amerongen AH, Boom RP, Meijer S (2002) Ultrasound-guided lumpectomy of nonpalpable breast cancer versus wire-guided resection: a randomized clinical trial. Ann Surg Oncol 9:994–998
Homer MJ (1983) Transection of the localization hooked wire during breast biopsy. Am J Roentgenol 141:929–930
Tykka H, Castren-Person M, Sjoblom M (1993) Pneumothorax caused by hooked wire localization of an impalpable breast lesion detected by mammography. Breast 2:52–53
Jeevan R, Cromwell DA, Trivella M et al (2012) Reoperation rates after breast conserving surgery for breast cancer among women in England: retrospective study of hospital episode statistics. BMJ 345:e4505
Takács T, Paszt A, Simonka Z et al (2013) Radioguided occult lesion localisation versus wire-guided lumpectomy in the treatment of non-palpable breast lesions. Pathol Oncol Res 19(2):267–273
Bernardi S, Bertozzi S, Londero AP, Gentile G, Giacomuzzi F, Carbone A (2012) Incidence and risk factors of the intraoperative localization failure of nonpalpable breast lesions by radio-guided occult lesion localization: a retrospective analysis of 579 cases. World J Surg 36(8):1915–1921
Wazer DE, Schmidt-Ullrich RK, Ruthazer R et al (1999) The influence of age and extensive intraductal component histology upon breast lumpectomy margin assessment as a predictor of residual tumor. Int J Radiat Oncol Biol Phys 45(4):885–891
Smitt MC, Horst K (2007) Association of clinical and pathologic variables with lumpectomy surgical margin status after preoperative diagnosis or excisional biopsy of invasive breast cancer. Ann Surg Oncol 14(3):1040–1044
Sanchez C, Brem RF, McSwain AP, Rapelyea JA, Torrente J, Teal CB (2010) Factors associated with re-excision in patients with early-stage breast cancer treated with breast conservation therapy. Am Surg 76(3):331–334
Lovrics PJ, Cornacchi SD, Vora R, Goldsmith CH, Kahnamoui K (2011) Systematic review of radioguided surgery for non-palpable breast cancer. Eur J Surg Oncol 37(5):388–397
Del Turco MR, Ponti A, Bick U, Biganzoli L et al (2010) Quality indicators in breast cancer care. Eur J Cancer 46(13):2344–2356
Ahmed M, Douek M (2013) Radioactive seed localisation (RSL) in the treatment of non-palpable breast cancers: systematic review and meta-analysis. Breast 22(4):383–388
Postma EL, Verkooijen HM, van Esser S et al (2012) Efficacy of ‘radioguided occult lesion localisation’ (ROLL) versus ‘wire-guided localisation’ (WGL) in breast conserving surgery for non-palpable breast cancer: a randomised controlled multicentre trial. Breast Cancer Res Treat 136(2):469–478
Cleffken B, Postelmans J, Olde Damink S, Nap M, Schreutelkamp I, van der Bijl H (2007) Breast-conserving therapy for palpable and nonpalpable breast cancer: can surgical residents do the job irrespective of experience? World J Surg 31(9):1731–1736
Landheer ML, Hoorntje LE, Klinkenbijl JH, Borel Rinkes IH (2004) The surgical treatment of nonpalpable breast carcinoma in a university teaching hospital and a general teaching hospital by residents-in-training and surgeons; comparable results. Ned Tijdschr Geneeskd 148(35):1724–1727
Edge SB, Byrd DR, Compton CC et al (eds) (2010) AJCC cancer staging manual, 7th edn. Springer, New York, pp 347–376
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Tóth, D., Varga, Z., Sebő, É. et al. Predictive Factors for Positive Margin and the Surgical Learning Curve in Non-Palpable Breast Cancer After Wire-Guided Localization – Prospective Study of 214 Consecutive Patients. Pathol. Oncol. Res. 22, 209–215 (2016). https://doi.org/10.1007/s12253-015-9999-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-015-9999-3