Abstract
To investigate the correlation of hypoxia-inducible factor-1α (HIF-1α) expression with clinical prognosis and efficacy of radiochemotherapy in esophageal squamous cell carcinoma (ESCC). Studies assessing the clinical or prognostic significance of HIF-1α expression in ESCC published prior to December 2011 were selected by searching PubMed, EMBASE, Cochrane Library, and (China National Knowledge Infrastructure) CNKI. A meta-analysis was performed to clarify the impact of HIF-1α expression on clinicopathological parameters or survival in ESCC. A total of 16 studies met the inclusion criteria, which included 1261 patients with ESCC. Accordingly, the level of HIF-1α expression in esophageal tissues of patients with ESCC was significantly higher than that in normal patients (odds ratio, OR = 33.111, 95 % confidence interval, CI = 11.912–92.040). The expression of HIF-1α correlated with the depth of invasion (OR = 1.701, 95 % CI = 1.076–4.705), clinical TNM stage (OR = 2.160, 95%CI = 1.516–3.077), as well as lymph node metastasis (OR = 2.393, 95 % CI = 1.319–4.344), regardless of differentiation grading (OR = 1.185, 95 % CI = 0.859–1.635). Furthermore, there was a significant association of increased HIF-1α expression with poorer radiochemotherapy outcomes, 2-year overall survival (OR = 0.219, 95 % CI = 0.104–0.461) and survival (OR = 0.320, 95 % CI = 0.115–0.887, P < 0.05) in patients with ESCC. In addition, HIF-1α expression correlated with VEGF expression in the ESCCs (OR = 4.635, 95%CI = 2.591–8.292). Increased expression of HIF-1α plays an important role in the malignant biology of ESCC resulting in significantly poorer radiochemotherapy outcomes and 2-year overall survival. HIF-1α expression may be a prognostic factor, as well as a potential target for therapy in patients with ESCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer, the leading cause of death all over the world, has become a worldwide public health problem [1]. Esophageal cancer (EC) is one of the most common human cancers, with a 5-year survival rate of ≤10 % in China [1, 2]. There are two main histological types of EC, esophageal squamous cell carcinoma (ESCC) and adenocarcinoma (EAC). ESCC is the predominant histological subtype of EC worldwide [1].
Although the etiology for the carcinogenesis remains to be elucidated, carcinogen exposure, nutritional deficiency and biological virus infection are thought to lead to ESCC [3]. However, only a portion of the population exposed to these risk factors develop ESCC, indicating a variation in individual susceptibility to esophageal cancer [3]. Recent studies have revealed that variations in genes governing carcinoma metabolism, DNA repair, cell proliferation and apoptosis may play a role in individual susceptibility to the occurrence and progression of ESCC [2, 4–6]. Therefore, identification of genes that increase susceptibility may lead to a better understanding of the mechanism underlying ESCC.
Intra-tumoral hypoxia is a hallmark of solid cancer [7]. A hypoxic microenvironment initiates multiple cellular responses, such as proliferation and angiogenesis [7, 8]. Hypoxia-inducible factor-1 (HIF-1) is a key transcription factor that regulates the cellular responses to hypoxia. Recent studies demonstrated that HIF-1 plays an important role in the progression of cancer through the activation of a gene profile that is involved in the crucial aspects of cancer biology [8, 9]. HIF-1 is a heterodimeric transcription factor consisting of α subunit and β subunit. β subunit is constitutively expressed, and α subunit, which determines HIF-1 activity, is regulated by oxygen tension [7–10]. Recent studies have shown that HIF-1α is over-expressed in various human cancers with tumors of advanced grade, implying that HIF-1α may be an independent prognostic factor of cancer [7–9]. Although the majority of studies displayed a significant association of HIF-1α with lymph node involvement in ESCC, some conflicting results were present, thus, the clinical significance of HIF-1α remains unsettled. A meta-analysis was carried out to clarify this issue.
Materials and Methods
Publication Search
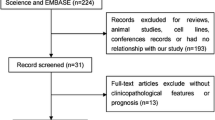
PubMed, the Cochrane database and CNKI were searched using the following terms: (i) esophagus or oesophagus and cancer or neoplasm or carcinoma; (ii) hypoxia-inducible factor-1α or HIF-1α. The references cited in the articles or reviews were also screened. The search included literature published from the initiation of database to December 2011.
Inclusion Criteria
This meta-analysis investigated the significance of HIF-1α in ESCC. Studies in the meta-analysis met the following criteria: (i) examined the relationship between HIF-1α and clinic-pathological parameters of ESCC, (ii) utilized inmmunohistochemistyr to determine the expression of HIF-1α inparaffin-embedded surgical specimens (IHC), (iii) sufficient data to estimate an odds ratio (OR) with 95 % confidence interval (CI) using multi-variates analysis, (iv) therapeutic response evaluated by RECIST 7.0, (v) ESCC was confirmed histopathologically according to UICC in 1997, (vi) assessed HIF-1α expression in the para-cancerous tissues or normal tissues, (vii) patients had no previous chemotherapy or radiotherapy, (viii) appropriate statistical methodology was used.
Exclusion Criteria
Studies that met the following criteria were excluded: (i) not case–control studies, (ii) case reports, letters, reviews and editorial articles, (iii) studies based on raw data with no usable data, (iv) duplicated data, (v) non-human subjects, (vi) Immunohistochemistry (IHC) was not used to evaluate the HIF-1α expression.
Data Extraction
Two investigators independently extracted data from eligible studies, and disagreements were resolved by discussion amongst the team of pathologists. For each study, the first author, journal, publication year, number of eligible patients, TNM stage, laboratory method, antibody used for IHC, HIF-1α status and survival results were recorded. Quality of data extraction was confirmed by two authors.
Statistical Analysis
The meta-analysis in this study was performed using the statistical software STATA 11.0. With regard to enumerative data, odds ratio (OR) and 95 % confidence interval (95 % CI) were applied to analyze the therapeutic efficacy. The heterogeneity of the data from eligible studies was evaluated by χ 2-test. The meta-analysis was performed using a fixed-effect model to determine the heterogeneous insignificance for the data. Statistical significance was defined as a P-value less than 0.05. The random-effect model was the optimal choice to perform the meta-analysis of the eligible studies, as significant heterogeneity existed among studies, both statistical and clinical. Due to poor-quality studies the sensitivity test was indicated, while depictive analysis was applied for the clinical data that had significant heterogeneity. The funnel chart was created using the Begg’s test, and the logistic model was constructed for the symmetrical test.
Results
Clinico-Pathological Characteristics
A total of 16 of 138 studies addressing HIF-1α expression in ESCC published from 1990 to 2011 met the criteria for this review [11–24]. These 16 studies included 223 controls and 1261 patients with ESCC, including 655 cases of well/moderate-differentiation, 268 of poor-differentiation, 246 of stage I/II, and 404 of stage III/IV. Clinico-pathological characteristics of eligible studies are summarized in Table 1. IHC was the only method used for the evaluation of HIF-1α expression in esophageal cancer specimens. The most commonly used antibody was a Santa Cruz antibody against HIF-1α, SC-13515. A wide range of dilutions were used from 1:200 to 1:1000. The definition of positive HIF-1α staining varied among the studies, and the cut-off values in the studies ranged from 5 % to 30 %.
Association of HIF-1α with Clinico-Pathological Characteristics
Seven studies examined the difference in HIF-1α expression between ESCC and normal tissues. The random-effect model was used for the meta-analysis. A significant difference was detected between ESCC and normal tissues (OR = 33.111, 95%CI: 11.912–92.040, P = 0.000) (Fig. 1 and Table 2).
Eleven studies examined the correlation between HIF-1α expression and histologic differentiation. Since no significant heterogeneity existed (P = 0.215), a fixed-effect model was used for the meta-analysis. As shown in Fig. 2 and Table 2, the combined OR was 1.185 (95 % CI: 0.859–1.635, P = 0.300) for poorly versus well/moderately differentiated tumors. The association between HIF-1α and invasive depth was investigated in 9 studies. The outcomes were significantly heterogeneous (P = 0.000), and a random-effect model was used for the meta-analysis. The combined OR was 2.250 (95 % CI = 1.076–4.705, P = 0.001, Fig. 3 and Table 2) for T3-4 versus T1-2. The association between HIF-1αand metastatic lymph nodes was explored in 13 studies. The heterogeneity in the subgroups was significant (P = 0.000), so a random-effect model was used for the meta-analysis. The combined OR for N(+) versus N(−) was 2.393 (95 % CI = 1.319–4.344, P = 0.000, Fig. 4 and Table 2). Begg’s funnel model was used for the bias analysis, and no bias was detected in the correlation between HIF-1α and lymph node metastasis. Egger’s test consistently supported the fact that no analytical bias appeared in the meta-analysis (Fig. 5, Table 2). The relationship between HIF-1α and tumor stage was evaluated in 8 studies. No significant heterogeneity was detected (P = 0.197), and a fixed-effect model was applied in the meta-analysis. The combined OR for stage III–IV group versus stage I–II group was 2.160 (95 % CI = 1.516–3.077, P = 0.000, Fig. 6 and Table 2).
HIF-1α as a Prognostic Factor for ESCC
Four studies in which the correlation between HIF-1α expression and the curative effects of chemo-radiotherapy on ESCC were investigated and did not display significant heterogeneity (P = 0.716). Hence, a fixed-effect model was used for the meta-analysis. HIF-1α was associated with a reduced therapeutic benefit of chemoradiotherapy in patients with ESCC (OR = 0.219, 95 % CI: 0.104–0.461, P = 0.000, Table 2). The function of HIF-1α as a prognostic factor for ESCC was explored in 3 studies. No significantly statistical heterogeneity was detected (P = 0.237), and a fixed-effect model was applied to calculate OR, 1.78 (95 % CI: 0.104–0.461, P = 0.000). These results indicated that HIF-1αcorrelated with poor survival in patients with ESCC (Table 2).
Correlation of HIF-1α Expression with VEGF Expression
Of patients with ESCC, 175 exhibited positive expression of VEGF, while HIF-1α was detected in 276 cases. 95 cases of ESCC presented HIF-1α(−)VEGF(−). The meta-analysis indicated that a substantial correlation between HIF-1α and VEGF existed, in which OR was 4.635 (95 % CI: 2.591–8.292, P = 0.000, Fig. 7, Table 2).
Discussion
Tumor hypoxia negatively regulates tumor cell growth and leads to a malignant phenotype by up-regulating the expression of genes encoding angiogenic, metabolic and metastatic factors [25, 26]. Of clinical importance, insufficient oxygen affects the efficiency of chemotherapy and radiotherapy [9, 27]. HIF-1 is a master transcriptional activator of oxygen-regulated genes, which is constitutively up-regulated in several tumor types [10].
Meta-analysis is a quantitative approach which statistically integrates the findings of individual researchers. Recently, it has been used for the evaluation of cancerous prognosticators [2, 28–30]. In this meta-analysis, 16 studies addressing the expression of HIF-1α in relation to ESCC clinico-pathological parameters and survival were evaluated. Expression of HIF-1α was determined by IHC. HIF-1α was found to be associated with tumor invasion, lymph node metastasis, and advanced pathological stage for ESCC, regardless of tumor differentiation. This was consistent with previous studies in vitro, which demonstrated that HIF-1α expression may enhance tumor cell metastasis by inhibiting cell adhesion and the apoptotic cascade [13, 31]. Although the statistical significance of the correlation between HIF-1α expression and pathological stage may have varied with lymph node metastasis or depth of invasion, the increased expression of HIF-1α in ESCCs with positive lymph node metastasis or T3/T4 invasion still supports the potential role of an HIF-1α inhibitor in the adjuvant therapy of ESCC.
The prognostic value of HIF-1α for survival in patients with ESCC was only evaluated in a few studies included in this meta-analysis. Three eligible studies were evaluated to generate the combined hazard ratio value of 1.78 (95 % CI: 0.104–0.461, P = 0.000), which suggested that HIF-1α is a prognostic factor for patients with ESCC. However, the results of these studies were conflicting; hence, a re-evaluation of these data will be necessary in order to reach a reasonable conclusion.
In the majority of the studies that were included in this analysis, the univariate analysis was applied with the relatively poor convincingness. Pooling the results of these studies may have introduced a bias to the analysis. These findings are important for the clinical application and further prospective studies of HIF-1α in patients with ESCC. Interestingly, the results of this meta-analysis demonstrated that increased HIF-1α expression was correlated with a decreased response to chemoradiation in patients with ESCC. Li et al. found that HIF-1α has the potential to predict the treatment outcome of prostate cancer [32]. Studies in cultured cells or animal models demonstrated that cells overexpressing HIF-1α tend to be resistant to apoptosis [17, 33]. Hence, ESCC with a high level of HIF-1α expression may be less sensitive to radiochemotherapy.
Hypoxic microenvironments are frequently found in solid tumors as a result of morphologically and functionally inappropriate vascularization, irregular bloodflow, anemia and the high oxygen consumption of rapidly proliferating malignant cells [31]. Hypoxic tumor cells undergo oxygen-regulated transcriptional activation of a specific set of genes [34, 35]. HIF-1α is a transcription factor that regulates the transcription of genes associated with cell proliferation and angiogenesis [36–38]. Our results showed a correlation between HIF-1α and VEGF in ESCC tissues, which is in agreement with HIF-1α’s function as a transcriptional factor for these angiogenic factors.
The lack of reliability of IHC as a technique to assess the expression of HIF-1α may have introduced some heterogeneity issues into the meta-analysis. IHC is the method most commonly used technique to assess the expression of HIF-1α due to the fact that it is readily available and inexpensive, as well as able to detect variations in a relatively low proportion of tumor cells and formation-fixed tissues for retrospective studies. Furthermore, additional variations exist among these studies in regard to IHC, including the wide range of primary antibodies used with varying dilutions, protocols, and cut-off points, which were selected arbitrarily by investigators.
There are limitations to this meta-analysis. Among the studies included in the meta-analysis there was also variability in the length of follow-up and the inconsistency in the inclusion of clinico-pathological parameters. Only studies published in English or Chinese were included, which may have led to a bias in publication inclusion. Due to the fact that most of the studies analyzing survival analysis were not performed by multivariate analysis, the meta-analysis could only be performed by univariate analysis.
Conclusions
In conclusion, this meta-analysis demonstrates that HIF-1α is associated with tumor invasion, lymph node metastasis, pathological stage, chemo/radiotherapy sensitivity, and survival of patients with ESCC. These results warrant the prospective validation of HIF-1α expression as a prognostic marker for patients with ESCC.
References
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62:10–29
Zhang GH, Mai RQ, Huang B (2010) Meta-analysis of ADH1B and ALDH2 polymorphisms and esophageal cancer risk in China. WJG 16:6020–6025
Enzinger PC, Mayer RJ (2003) Esophageal cancer. N Engl J Med 349:2241–2252
Yang SJ, Yokoyama A, Yokoyama T, Huang YC, Wu SY, Shao Y, Niu J, Wang J, Liu Y, Zhou XQ, Yang CX (2010) Relationship between genetic polymorphisms of ALDH2 and ADH1B and esophageal cancer risk: a meta-analysis. World J Gastroenterol 16:4210–4220
Liang Y, Liu JL, Wu Y, Zhang ZY, Wu R (2011) Cyclooxygenase-2 polymorphisms and susceptibility to esophageal cancer: a meta-analysis. Tohoku J Exp Med 223:137–144
Knechtel G, Szkandera J, Stotz M, Hofmann G, Langsenlehner U, Krippl P, Samonigg H, Renner W, Langner C, Dehchamani D, Gerger A (2010) Single nucleotide polymorphisms in the hypoxia-inducible factor-1 gene and colorectal cancer risk. Mol Carcinog 49:805–809
Unruh A, Ressel A, Mohamed HG, Johnson RS, Nadrowitz R, Richter E, Katschinski DM, Wenger RH (2003) The hypoxia-inducible factor-1 alpha is a negative factor for tumor therapy. Oncogene 22:3213–3220
Adams JM, Difazio LT, Rolandelli RH, Luján JJ, Haskó G, Csóka B, Selmeczy Z, Németh ZH (2009) HIF-1 a key mediator in hypoxia. Acta Physiol Hung 96:19–28
Smith TG, Robbins PA, Ratcliffe PJ (2008) The human side of hypoxia-inducible factor. Br J Haematol 141:325–334
Kuphal S, Winklmeier A, Warnecke C, Bosserhoff AK (2010) Constitutive HIF-1 activity in malignant melanoma. Eur J Cancer 46:1159–1169
Liu JL, Zhou BJ, Zhang Y (2007) Expression and biological significance of HPA and HIF-1alpha in human esophageal squamous cell carcinoma. Zhonghua Zhong Liu Za Zhi[Chin J Oncol] 29:689–692
Yu ZT, Zhao HF, Shang XB (2008) Expression of hypoxia-inducible factor-1alpha and vessel endothelial growth factor in esophageal squamous cell carcinoma and clinico-pathological significance thereof. Zhonghua Yi Xue Za Zhi 88:2465–2469
Matsuyama T, Nakanishi K, Hayashi T, Yoshizumi Y, Aiko S, Sugiura Y, Tanimoto T, Uenoyama M, Ozeki Y, Maehara T (2005) Expression of hypoxia-inducible factor-1alpha in esophageal squamous cell carcinoma. Cancer Sci 96:176–182
Kurokawa T, Miyamoto M, Kato K, Cho Y, Kawarada Y, Hida Y, Shinohara T, Itoh T, Okushiba S, Kondo S, Katoh H (2003) Overexpression of hypoxia-inducible-factor 1alpha(HIF-1alpha) in oesophageal squamous cell carcinoma correlates with lymph node metastasis and pathologic stage. Br J Cancer 89:1042–1047
Sohda M, Ishikawa H, Masuda N, Kato H, Miyazaki T, Nakajima M, Fukuchi M, Manda R, Fukai Y, Sakurai H, Kuwano H (2004) Pretreatment evaluation of combined HIF-1alpha, p53 and p21 expression is a useful and sensitive indicator of response to radiation and chemotherapy in esophageal cancer. Int J Cancer 110:838–844
Tzao C, Lee SC, Tung HJ, Hsu HS, Hsu WH, Sun GH, Yu CP, Jin JS, Cheng YL (2008) Expression of hypoxia-inducible factor (HIF)-1alpha and vascular endothelial growth factor (VEGF)-D as outcome predictors in resected esophageal squamous cell carcinoma. Dis Markers 25:141–148
Ogawa K, Chiba I, Morioka T, Shimoji H, Tamaki W, Takamatsu R, Nishimaki T, Yoshimi N, Murayama S (2011) Clinical significance of HIF-1alpha expression in patients with esophageal cancer treated with concurrent chemoradiotherapy. Anticancer Res 31:2351–2359
Kimura S, Kitadai Y, Tanaka S, Kuwai T, Hihara J, Yoshida K, Toge T, Chayama K (2004) Expression of hypoxia-inducible factor (HIF)-1alpha is associated with vascular endothelial growth factor expression and tumour angiogenesis in human oesophageal squamous cell carcinoma. Eur J Cancer 40:1904–1912
Talks KL, Turley H, Gatter KC, Maxwell PH, Pugh CW, Ratcliffe PJ, Harris AL (2000) The expression and distribution of the hypoxia-inducible factors HIF-1alpha and HIF-2alp:a in normal human tissues, cancers, and tumor-associated macrophages. Am J Pathol 157:411–421
Wu XA, Sun Y, Fan QX, Wang LX, Wang RL (2007) Relationship between the expression of hypoxia-inducible factor-1α and chemotherapy response in esophageal squamous cell carcinoma. Chinese Med J Peking 87:1783–1786
Zhang HZ, Wang YZ, Xu N, Zhu SC, Liu B (2007) Expression and clinical significance of HIF-1α, VEGF and Survivin in esophageal squamous cell carcinoma. Chin-Ger J Clin Oncol 6:339–344
Guo LJ, Chen ZJ, Chen CZ, Hong CQ, Wu X (2009) Expressions of HIF-1α and COX-2 in esophageal squamous cell carcinoma and their correlation with intratumoral MVD. Chin J Radiol Med Prot 29:502–505
Wu XA, Fan QX, Wang LX, Sun Y, Zhao PR (2006) ReIationship between HIF-lα expression and angiogenesis in esophageal sguamous cell carcinoma tissue. J Zhengzhou Univ 41:1111–1114
Hu JL, Chen P, Liu W, Li ZY, Chen YS, Wu G (2010) Expression of VEGF16sb and HIF-1α in esophageal squamous carcinoma tissues and their significance. Cancer Res Prev Treat 1:9–11
Carmeliet P, Jain RK (2011) Molecular mechanisms and clinical applications of angiogenesis. Nature 473:298–307
Valastyan S, Weinberg RA (2011) Tumor metastasis: molecular insights and evolving paradigms. Cell 147:275–292
Gebski V, Burmeister B, Smithers BM, Foo K, Zalcberg J, Simes J (2007) Survival benefits from neoadjuvant chemoradiotherapy or chemotherapy in oesophageal carcinoma: a meta-analysis. Lancet Oncol 8:226–234
Zhao J, Li L, Wei S, Gao Y, Chen Y, Wang G, Wu Z (2011) Clinicopathological and prognostic role of cyclin D1 in esophageal squamous cell carcinoma: a meta-analysis. Dis Esophagus 25:520–526
Yu WW, Guo YM, Zhu M, Cai XW, Zhu ZF, Zhao WX, Fu XL (2011) Clinicopathological and prognostic significance of EGFR over-expression in esophageal squamous cell carcinoma: a meta-analysis. Hepatogastroenterology 58:426–431
Fang P, Jiao S, Zhang X, Liu Z, Wang H, Gao Y, Luo H, Chen T, Shi L (2011) Meta-analysis of ALDH2 variants and esophageal cancer in Asians. Asian Pac J Cancer Prev 12:2623–2627
Miyazawa M, Yasuda M, Fujita M, Kajiwara H, Hirabayashi K, Takekoshi S, Hirasawa T, Murakami M, Ogane N, Kiguchi K, Ishiwata I, Mikami M, Osamura RY (2009) Therapeutic strategy targeting the mTOR-HIF-1alpha-VEGF pathway in ovarian clear cell adenocarcinoma. Pathol Int 59:19–27
Grebhardt S, Veltkamp C, Strobel P, Mayer D (2012) Hypoxia and HIF-1 increase S100A8 and S100A9 expression in prostate cancer. Int J Cancer
Natsuizaka M, Naganuma S, Kagawa S, Ohashi S, Ahmadi A, Subramanian H, Chang S, Nakagawa KJ, Ji X, Liebhaber SA, Klein-Szanto AJ, Nakagawa H (2012) Hypoxia induces IGFBP3 in esophageal squamous cancer cells through HIF-1alpha-mediated mRNA transcription and continuous protein synthesis. FASEB J 26:2620–2630
Tang N, Wang L, Esko J, Giordano FJ, Huang Y, Gerber HP, Ferrara N, Johnson RS (2004) Loss of HIF-1alpha in endothelial cells disrupts a hypoxia-driven VEGF autocrine loop necessary for tumorigenesis. Cancer Cell 6:485–495
Arany Z, Foo SY, Ma Y, Ruas JL, Bommi-Reddy A, Girnun G, Cooper M, Laznik D, Chinsomboon J, Rangwala SM, Baek KH, Rosenzweig A, Spiegelman BM (2008) HIF-independent regulation of VEGF and angiogenesis by the transcriptional coactivator PGC-1alpha. Nature 451:1008–1012
Buchler P, Reber HA, Buchler MW, Friess H, Lavey RS, Hines OJ (2004) Antiangiogenic activity of genistein in pancreatic carcinoma cells is mediated by the inhibition of hypoxia-inducible factor-1 and the down-regulation of VEGF gene expression. Cancer-Am Cancer Soc 100:201–210
Pore N, Jiang Z, Gupta A, Cerniglia G, Kao GD, Maity A (2006) EGFR tyrosine kinase inhibitors decrease VEGF expression by both hypoxia-inducible factor (HIF)-1-independent and HIF-1-dependent mechanisms. Cancer Res 66:3197–3204
Pore N, Gupta AK, Cerniglia GJ, Maity A (2006) HIV protease inhibitors decrease VEGF/HIF-1alpha expression and angiogenesis in glioblastoma cells. Neoplasia 8:889–895
Acknowledgments
This study was supported by the Ministry of education of the People’s Republic of China for the higher level education foundation (20091323110011).
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
GS and WH conceived the study and drafted the manuscript. GS and WH collected and analyzed the data, GS and YW also secured funding. YL and YW contributed to the quality control of study inclusion and discussion. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sun, G., Hu, W., Lu, Y. et al. A Meta-Analysis of HIF-1α and Esophageal Squamous Cell Carcinoma (ESCC) Risk. Pathol. Oncol. Res. 19, 685–693 (2013). https://doi.org/10.1007/s12253-013-9631-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-013-9631-3