Abstract
Previous studies have indicated the antitumoral effect of human melanocytes, human melanoma cell lines expressing CB1 receptor (CB1), and of the peritumoral administration of endocannabinoids. In the present study, we systematically screened several human melanoma cell lines for the expression of CNR1 and demonstrated transcription of the authentic gene. The product of CNR1, the CB1 protein, was found localized to the cell membrane as well as to the cytoskeleton. Further, the studied human melanoma cell lines expressed functional CB1 since physiological and synthetic ligands, anandamide (AEA), Met-F-AEA, ACEA and AM251 showed a wide range of biological effects in vitro, for example anti-proliferative, proapoptotic and anti-migratory. More importantly, our studies revealed that systemic administration of a stable CB1 agonist, ACEA, into SCID mice specifically inhibited liver colonization of human melanoma cells. Since therapeutic options for melanoma patients are still very limited, the endocannabinoid-CB1 receptor system may offer a novel target.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
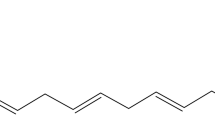
Endocannabinoids (CB) belong to the ever growing bioactive lipid family produced from membrane phospholipids. Among the major intracellular products are the arachidonic acid derivative, anandamide (AEA) produced by Ca2+−dependent N-acyltransferase and N-acylphosphatidylethanolamine-hydrolyzing phospholipase D, and the diacylglycerol derivative, 2-arachidonoylglycerol (2-AG) produced by phospholipase C and diacylglycerol lipase [1]. AEA is metabolized by fatty acid amide hydrolase (FAAH), metabolized further via the activity of lipoxygenases P450s and cyclooxygenase-2 [2].
Receptors for CBs are CB1 and CB2, belonging to the GPCR receptor family. Although initially identified in the central- and peripheral nervous system, the CB1-, and to a smaller extent the CB2 receptor may also be found in various tissues outside the nervous system. The CB1 receptor sends signals through various pathways mediated by G1/0 proteins, characterized by involvement of the RAS-RAF-MAPK pathway, adenyl cyclase and Ca++ [3].
Due to the widespread expression of CB receptors in a variety of tissues, it is not surprising that various cancer types may also express these receptors [4–7]. On the other hand, cancers are also able to produce CB bioactive lipids, setting up the stage for auto-/paracrine lipid signaling loops [8]. In the past decade several studies demonstrated that CBs have direct antitumoral effects in various experimental systems in vitro and in vivo, including antiproliferative, apoptosis-inducing, anti-angiogenic and anti-metastatic effects [9–13].
CB1 and 2 receptors are expressed in various cell types of the skin including the epidermis, appendages, dermal tissues etc. [14]. Studies have indicated that CB1/CB2 receptors are expressed at both mRNA and protein levels in human keratinocytes, in benign and malignant tumors (papillomas, basal cell and squamous carcinomas) [15], in human melanocytes as well as in a human melanoma cell line [16]. The widespread expression of CNR1 (the gene of CB1) in human melanoma, however, was not demonstrated convincingly. Skin melanoma is the most aggressive human cancer type, falling into the category of “orphan tumors” since effective therapy other than surgery does not exist. This is mainly due to the apoptosis resistance of melanocytes and melanomas [17]. Bioactive lipids produced by either COX1/2 [18, 19] or LOX enzymes [20, 21] have been shown to have antitumoral effects in melanoma, but their therapeutic development is still in the early stages. In the present study we provide evidence that various genetically independent human melanoma cell lines, as well as benign and malignant melanocytic tumor tissues express genetically authentic CNR1, and we demonstrate the membrane localization of the receptor. Previous data have suggested antitumoral effects of CB1 agonists following intratumoral application, whereas in our study we confirm the anti-proliferative/proapoptotic and anti-metastatic effects of CB1 modulators in vivo upon systemic therapy.
Materials and Methods
CB1 Modulators
Anandamide (AEA), the physiological CB1 ligand, was purchased from Cayman Chemical (Ann Arbor, MI), its stable analogues, 2-methyl-2-F-anandamide (Met-F-AEA) was obtained from Calbiochem (San Diego, CA) and arachidonyl-2-chloroethylamide (ACEA) from Tocris Bioscience (Bristol, UK). AM251 (N-piperidinyl-iodophenyl-dichlorophenyl-methylpyrazole-carboxamide), a selective inverse CB1 agonist, was also purchased from Tocris. All derivatives were dissolved in ethanol.
Tumor Cell Cultures
The HT168-M1 human melanoma line was derived from the A2058 cell line [22]. The HT199 melanoma line was established by our group. The WM35 melanoma cell line, and the WM983B line that does not express αIIbβ3 on the cell surface were kind gifts of Meenhard Herlyn (The Wistar Institute, Philadelphia, PA). Mock transfected WM983B cells (3.1) as well as αIIb and β3 transfected WM983B cells (19L and 19H) were described earlier [23]. Human melanoma cell lines were grown in RPMI-1640 medium supplemented with 5 % fetal calf serum (FCS) and 1 % penicillin-streptomycin (all produced by Sigma.Aldrich, St. Louis, MO), at 37 °C in a humidified atmosphere containing 5 % CO2.
Genomic Studies
Construction and use of microarrays were performed according to our earlier descriptions [23, 24]. Briefly, 3200 cDNA inserts from human cDNA libraries (melanoma, benign melanocytic tumor, lymphocytes, heart, and mixed tissue libraries) were amplified, and purified with MultiScreen-PCR plate (Millipore, Billerica, MA), resuspended in 50 % dimethyl sulfoxide/water, and arrayed on FMB cDNA slides (Full Moon BioSystems, Sunnyvale, CA) using MicroGrid Total Array System (BioRobotics, Cambridge, UK) spotter with 16 pins in a 4 × 4 format. DNA elements were deposited in duplicate. The diameter of each spot was approximately 200 μm. After printing, DNA was UV crosslinked to the slides (Stratagene, La Jolla, CA, Stratalinker, 700 mJ). Post-processing and blocking of microarrays were also performed as previously described [23, 24].
Microarray Probe Preparation and Hybridization
RNA isolation from 5 × 106 cells was carried out with the RNA isolation kit of Macherey-Nagel (Macherey-Nagel, Düren, Germany) according to manufacturer instructions. RNA was eluted from the silica membrane and stored at −80 °C in the presence of 30 U of Prime RNAse inhibitor (Fermentas, Vilnius, Lithuania). The quality and quantity of isolated RNA were checked by electrophoresis and spectrophotometry (NanoDrop, Rockland, DE), respectively. For probe preparation, 4 μg of total RNA were reverse transcribed using poly-dT-primed Genisphere Expression Array 350 detection system (Genisphere, Hatfield, PA) in 20 μl total volume using 20 U RNAsin (Fermentas), 1 × first strand buffer and 200 U of RNAse H (−) point mutant M-MLV reverse transcriptase (Fermentas). All other probe preparation steps were performed according to manufacturer instructions (Genisphere). cDNA was hybridized onto human cDNA microarrays in a Ventana hybridization station (Ventana Discovery, Tucson, AR) using the “antibody” protocol. First, hybridization was performed at 42 °C for 6 h in “Chiphyb” hybridization buffer (Ventana), then 2.5 μl each of Cy5 and Cy3 capture reagents were added to the slides in 200 μl “Ribohyb” hybridization buffer (Ventana), followed by incubation at 42 °C for 2 h. After hybridization the slides were washed in 0.2 × SSC twice at room temperature for 10 min, then dried and scanned.
Scanning and Data Analysis
Each array was scanned under a green laser (543 nm for Cy3 labeling) or a red laser (633 nm for Cy5 labeling) using a ScanArray Lite (GSI Lumonics, Billerica, MA) scanning confocal fluorescent scanner with 10 μm resolution (laser power: 85 % for Cy5 and 90 % for Cy3, gain: 80 % for Cy5 and 75 % for Cy3). Scanned output files were analyzed using GenePix Pro3.0 software (Axon Instruments Inc., Foster City, CA). Each spot was defined by automatic positioning of a grid of circles over the image. The average and median pixel intensity ratios calculated from both channels and the local background of each spot were determined. An average expression ratio (MeaR, denoting the average of local background-corrected pixel intensity ratios) was determined for each spot [21, 22]. Normalization was performed by the global Lowess method. Those data were flagged and excluded where the replicate spots from different sites of the same array were significantly different. Those genes were taken into account in the melanoma cell cultures where the average change (increase or decrease) of the four data points were at least 2.0-fold.
CNR1 Expression and Sequencing
Total RNA Isolation
Total RNA was isolated from each tumor suspension sample by the Trizol method (Sigma-Aldrich) according to manufacturer instructions. In brief, cells were lysed in Trizol, after isopropanol precipitation RNA was extracted, washed and precipitated repeatedly with ethanol and solved with DEPC-treated water. Possible DNA contamination was eliminated by means of DNase digestion on NucleoSpin RNA II column: samples were precipitated by ethanol, bound on special column, digested with DNAse I (Macherey-Nagel) for 30 min, washed with serial buffers and eluted with DEPC-treated water.
Reverse Transcription
For reverse transcription the 1 μl of 10 mM dNTP mix (Finnzyme®) was added to 1 μl of random nonamer-oligo dT to reach the final concentration of 2.5 μM and 2 μg of the purified total RNA was used with the mixture. After incubation at 70 °C for 10 min 2 μl of 10 × M-MLV Reverse Transcriptase Buffer (Finnzymes, Finland), 1 μl of M-MLV Reverse Transcriptase (200 units/μl, Finnzyme), 0.5 μl RNase Inhibitor (40 units/μl, Promega, Madison, WI) and 6.5 μl DEPC treated water were added for a final volume of 20 μl, then following incubation at 37 °C for 50 min and 85 °C for 10 min, the β-actin primer pairs (human: βS1: 5′-TCT GGC ACC ACA CCT TCT AC-3′ and βA4: 5′-CTC CTT AAT GTC ACG CAC GAT TTC-3′, murine: MßS1(RefSeq NM_007393):5′-AGA CAA CAT TGG CAT GGC TT-3′, MßA1: 5′-AAT GAA GTA TTA AGG CGG AAG ATT-3′) were used for checking the occurrence of reverse transcription by PCR reaction. RNA of the same sample was used as negative control for detection of DNA contamination, and DEPC-treated water as non-template control. A previously proven RNA sample of K562 was used as positive control for reverse transcription reaction.
PCR Analysis
For detection of both human specific and species-independent CNR1 gene expression at transcriptional level, nested PCR primer pairs were newly designed both on the coding region (homologous human and murine regions) and the non-coding region (present in human and lacking in murine – according to the RefSeq catalogue of NCBI) of CNR1 variant 1. The primer pairs were as follows:
Coding region (NM_016083) – aspecific primers
-
CNR1-outer-sense: 3′-CCAGAAGAGCATCATCATCCAC-5′ (1002–1023)
-
CNR1-outer-antisense: 3′-GTTCAGCAGGCAGAGCATAC-5′ (1230–1211)
-
CNR1-inner-sense: 3′-AAGAGCATCATCATCCACACG-5′ (1006–1026)
-
CNR1-inner-antisense: 3′-CAACACCACCAGGATCAGGA-5′ (1119–1100)
Non-coding region (NM_016083) – “human-specific” primers
-
HCNR1-outer-sense: 3′-TGTCCGTAGTATCAGAGATGTCC-5′ (1848–1870)
-
HCB-outer-antisense: 3′-ATCCACTGCTTGTCCATTGTTC-5′ (2018–1997)
-
HCNR1-inner-sense: 3′-TCCGTAGTATCAGAGATGTCCATT-5′ (1850–1873)
-
HCNR1-inner-antisense: 3′-AGCACATAAACACTGATACACATCT -5′ (1949–1925)
Isolated total RNA of human hippocampus and mouse (BDF1) whole brain were used as positive controls.
The PCR reaction mixture contained 2.5 μl of 10 × PCR buffer+Mg2+ (DyNazyme, Finnzymes), 2 μl of dNTP mix (2.5 mM each), 0.4 μl of DNA polymerase (DyNazyme, 2 U/μl), 2.5 μl each of both primers, 2 μl of cDNA and 13.1 of μl DEPC-treated water for a final volume of 25 μl. The cycling conditions were: 94 °C for 12 min once, followed by 94 °C for 1 min, 55 °C for 1 min, 72 °C for 1 min for 40 cycles and the extension step was 72 °C for 10 min. PCR products were separated on 2 % agarose gel and detected with Gel Doc 2000 (Bio-Rad, Hercules, CA) after ethidium bromide staining. PCR products were reisolated from the agarose gel (High Pure PCR Product Purification Kit, Roche, Mannheim, Germany) in the case of all bands. The DNA sequences were determined by Big Dye Terminator cycle sequencing on Applied Biosystems 3130 Genetic Analyzer (Applied Biosystems, Foster City, CA).
Immunocytochemistry
Melanoma cells were fixed in paraformaldehyde for 10 min and then permeabilized with 0.1 % Triton X-100 (Sigma) in phosphate-buffered saline (PBS) for 1 min. After washing in PBS for 3 × 5 min, slides were blocked with 1 % bovine serum albumine (BSA; Sigma) and goat serum (9:1) for 30 min at room temperature, then incubated with primary rabbit polyclonal antibodies against CB1 protein (1:100 in PBS, Calbiochem). Cells were washed in PBS for 3 × 10 min and then incubated with biotin-conjugated anti-rabbit IgGs (Amersham, Buckinghamshire, UK) for 40 min at 37 °C (dilution 1:100). After washing, CB1 protein was visualized by streptavidin-FITC (dilution 1:100, Vector Laboratories, Burlingame, CA). Negative controls were prepared by replacing the primary antibody with isotype-matched non-immune IgG (Sigma). Cell nuclei were stained with propidium iodide (PI, Sigma). Slides were covered with Vectashield (Vector Laboratories) and cells were examined with a confocal microscope (Eclipse C1 Plus, Nikon Optoteam, Vienna, Austria).
Cell Proliferation Assay
Cell suspensions containing 5 × 103 viable cells/well were plated in 96-well tissue culture plates and allowed to attach for 24 h at 37 °C in RPMI-1640 medium supplemented with 5 % FCS. After attachment the medium was changed (5 % or 0 % FCS) and the cells were exposed to different CB1 agonists for 48 h. At the end of incubation, 20 μl of 5 mg/ml thiazolyl blue tetrazolium bromide (MTT, Sigma) were added to the cell medium for 4 h at 37 °C, then the medium was removed and tetrazolium crystals were dissolved in 100 μl DMSO (Sigma). Absorbance was measured at 570 nm using ELISA Microplate Reader (Bio-Rad). The 50 % inhibitory concentrations (IC50) were calculated by Dose-Effect Analysis using Microcomputers software (Elsevier-Biosoft, Cambridge, UK).
Flow Cytometric Measurement of Apoptosis
Cells previously treated for 48 h with different concentrations of CB1 agonists were detached with 0.02 % EDTA, washed with PBS, and fixed with 70 % ethanol. After 4 h of incubation with PI and RNAse (CyStain PI Absolute T, Partec, Germany) the DNA in cells was quantified by flow cytometry [24]. The percentage of apoptotic cells was determined as the amount of cells in the sub-G1 fraction analyzed by FlowMax software.
Modified Boyden Chamber Migration Assay
Chemotaxis assay was performed in Boyden chambers using 48-well micro chemotaxis chamber (Neuroprobe Inc., Cabin John, MD) and polyvinylpyrrolidone-free polycarbonate membrane filter with 8 μm pore size (Whatman, Kent, UK) without coating. Cultured cells were harvested with 0.02 % EDTA, washed twice with serum-free medium and resuspended at 4 × 105 cells/ml in medium containing 0.1 % BSA. The cell suspension (50 μl) was placed onto the membrane in the presence or absence of CB1 agonists, and the lower compartment was filled with 27 μl of fibronectin (100 μg/ml, Sigma). Cells were allowed to migrate for 6 h at 37 °C, then cells on the upper surface of the filter were removed mechanically, the membranes were stained with toluidine blue and the cells counted under light microscope.
Animal Experiments for Liver Colonization
SCID mice were bred and maintained in our specific pathogen-free mouse colony, housed 8 per cage. Previously cultured human melanoma HT168-M1 cells were detached with 0.02 % EDTA (Sigma), washed twice with serum-free medium, and one-cell suspension was inoculated into the spleen of SCID mice with the number of 5 × 104 cells/animal. CB1 agonists AEA and ACEA were suspended in physiologic saline with 0.5 % ethanol. Seven days following intrasplenic injection of the tumor cells, animals were treated intraperitoneally with two concentrations of AEA, ACEA or solvent control daily for 21 days (8 animals per group). At the endpoint (35 days following intrasplenic injection), weights of primary tumors were measured and the number of liver colonies counted under stereomicroscope. All animal experiments were conducted following standards and procedures approved by the Animal Care and Use Committee of the National Institute of Oncology, Budapest, Hungary
Statistics
To determine the statistical significance of differences between the groups, ANOVA was used, with post hoc Scheffé test where parametric methods were available. Evaluation of the differences in the animal experiments was performed by the non-parametric Kruskal-Wallis test using post hoc analysis. P values under 0.05 were considered statistically significant. Analyses were performed by Statistica 7.0 (StatSoft, Tulsa, OK).
Results
Human Melanoma Cell lines and Tissues Express Authentic CNR1
In our previous studies we looked for novel human melanoma-specific genes in cell lines using microarray technology which identified a set of Ca-signaling related genes [24]. We used human nevus tissue-derived mRNA as reference. During these studies we noted that from the list of expressed genes analyzed, CNR1 could be found in 4 human melanoma cell lines (non-metastatic: WM35 or metastatic: HT168, A2068, HT168-M1), though the expression level did not significantly differ from benign melanocytic tumor tissue (relative range: 1.02–1.44). Furthermore, the CNR1 expression was maintained in primary or metastatic tumor tissues when WM983B clones (3.1, 1919H) [23] were implanted subcutaneously into newborn mice (relative range in metastasis compared with primary was 0.57–1.19). This observation prompted us to systematically test CNR1 gene expression in human melanoma cell lines currently available in our laboratory using PCR primers designed for a coding and a non-coding region of the human CNR1 gene, with human and mouse whole brain used as controls. The data obtained indicated that all seven human melanoma cell lines, the majority of which are genetically unrelated, expressed CNR1 (Fig. 1) and sequencing of the PCR products in 4 cell lines revealed 98–100 % similarity to the human CNR1 sequence (Table 1), providing unquestionable evidence for the expression of authentic CNR1 gene in human melanoma. Furthermore, our study did not detect significant genetic alterations of CNR1 in human melanoma.
Subcellular Localization of CB1 in Human Melanoma Cells
Next we determined the subcellular localization of CB1 protein in human melanoma cells cultured in vitro using confocal laser microscopy. We used paraformaldehyde- and ethanol fixation to define cell surface or subcellular localization, respectively. Our data indicated that CB1 protein is present on the cell surface of human melanoma cells occasionally concentrated to defined large membrane areas (Fig. 2a). This membrane-associated localization of CB1 could also be demonstrated in permeabilized cells (Fig. 2b), where cytoskeleton-associated (Fig. 2b) and cytoplasmic labelings (Fig. 2c) were further identified.
Immunofluorescence detection of CB1 in in vitro cultured HT16-M1 melanoma cells using confocal laser scanning microscopy. a Paraformaldehyde fixation. Note the clear membrane localization of the green signal (CB1). Red: nuclear staining (propidium iodine). b-d Ethanol fixation. b Note the membrane and cytoskeletal localization of the green signal (CB1). c Frequently, the green signal (CB1) was present in the cytoplasm (red signal: nuclear staining). d Negative control, no primary antibody. Bar: 20 μm
Effect of CB1 Modulators on Human Melanoma Cells In Vitro
To prove the functional expression of CB1 in human melanoma cells, we used the physiological agonist ligand, AEA, its stable, more selective analogues, ACEA and Met-F-AEA, as well as a highly selective inverse agonist, AM251, administered in vitro for 48 h to tumor cells, then the proliferation was measured using MTT assay. The modulator classes (agonists AEA, ACEA, Met-F-AEA, inhibitor AM251) inhibited melanoma cell proliferation with an IC50 range of 3.5–10.64 μM (Table 2). Interestingly, a combination of low dose (5 μM) agonist (Met-F-AEA) with increasing concentrations of inverse agonist had an additive effect (Fig. 3). Looking for the mechanism of the antitumoral effect, we analyzed the in vitro apoptosis-induction potential of the CB1 modulators by means of DNA-staining and flow cytometry (Fig. 4a). These studies revealed that the main effect of CB1 agonists in HT168-M1 and WM983B (data not shown) human melanoma cells is a significant induction of apoptosis (as determined by the appearance of sub-G0 population, Fig. 4b), and the inverse agonist, AM251, was proved to be even more potent (Fig. 4c). Parallel supravital labelings also tested CB1 modulator effects on cell viability and revealed that besides apoptosis induction, cell necrosis was also induced parallel to apoptosis, although at higher concentrations (data not shown). Furthermore, a relative increase of G2 fraction cells upon AM251 treatment was also observed in WM983B cells, suggesting a G2/M block as well (data not shown).
Effect of CB1 ligands on the proliferation of HT-168-M1 human cells in vitro (MTT assay). Met-F-AEA and AM251 were applied in a concentration range of 1–10 μM in serum-containing medium. M5 + A = melanoma cells were treated with 5 μM Met-F-AEA together with increasing concentrations of AM251. Data are means ± SD of four parallel samples, expressed as % of control (untreated cells). */**p < 0.05 according to untreated control and 5 μM Met-F-AEA alone, respectively
Effect of CB1 ligands on the apoptosis of human melanoma cells in vitro. a Tumor cells were exposed to CB1 ligands for 48 h in medium-serum and nuclei were isolated, labeled and the subG1 fraction (arrow) measured by flow cytometry. b Effect of AEA and ACEA on HT168-M1 cells. c Effect of AM251 on human melanoma cell lines. Data are expressed in mean % ± SD of nuclei (n=3). * = p < 0.05
Effect of Systemic CB1 Modulation on Migration and Liver Colonization of Human Melanoma Cells
Next we tested CB1 agonists in a spleen liver metastasis model of SCID mice using metastatic human melanoma cells, HT168-M1. Tumor cells were inoculated into the spleen and unstable and stable agonists, AEA and ACEA, respectively, were applied intraperitoneally for 3 weeks followed by a drug-free period of another week. Administration of the CB1 ligands did not affect primary spleen tumor growth in vivo (data not shown). On the other hand, the stable analogue ACEA, unlike the unstable one AEA (data not shown), exhibited a significant inhibitory activity on liver colonization in doses of 0.24 and 1.2 mg/kg, respectively (Fig. 5a). These results suggest a specific antimetastatic effect of CB1 agonist in this human melanoma model. There are data available on the antimigratory potential of CB1 modulators – a key component of antimetastatic activity – in certain tumor cell types [25, 26], we therefore tested the CB1 agonist AEA in a modified Boyden chamber migration assay. Our data indicated that the administration of the CB1 agonist AEA has a significant antimigratory effect in vitro on HT168-M1 cells (Fig. 5b).
Effect of CB1 agonists on liver colonization and migration of HT168-M1 human melanoma cells. a Three weeks administration of 0.24 or 1.2 mg/kg ACEA intraperitoneally into SCID mice inoculated with melanoma cells into the spleen. Data are the mean number of liver metastasis ± SD (n = 8). CTR = solvent control. *p < 0.05. b Effect of AEA in vitro on cell migration (6 h). Data are expressed as mean number of migrated cells/field (±SD, n = 5). *p < 0.05
Discussion
Human melanoma is a chemo- and radiation therapy resistant cancer, due partly to the genetic constitution of the melanocytic lineage and partly to acquired genetic alterations during carcinogenesis [27–29]. Accordingly, modulation of the apoptotic sensitivity has clinical significance, since these modulations may allow re-introduction of conventional chemotherapeutics to which these tumors are resistant.
Endocannabinoids and their receptors have been extensively studied in the past decades as novel anticancer strategies. Beside hematological malignancies, modulators of the CB system have demonstrated striking activities in a variety of human solid cancer types (prostate, breast, colon, etc.) in experimental models and in a few early clinical trials [9–13]. Only one such study made an attempt to test cannabinoid analogues on an animal and a human melanoma cell line, revealing interesting antitumoral activity upon peritumoral administration in vivo [16]. These data, however, have not been confirmed or extended in case of human melanoma, therefore we have revisited this issue in our current paper.
We used several genetically independent groups of human melanoma cell lines to confirm the expression of CNR1 using microarray and PCR approaches. Further, we sequenced CNR1 from melanoma, demonstrating authentic receptor expression and no genetic defects. In summary, based on our presented data and an earlier report [16] it can be stated that the human melanoma expresses authentic CNR1.
The previous study on melanoma indicated expression of CB1 protein in melanoma, but the subcellular localization was not known [16]. In normal neuronal or glial cells CB1 was found to localize to lipid rafts at the cell membrane [30], to caveoli [31] and to endosomes [32] in the cytoplasm. In the present report we have confirmed the cell membrane-associated localization of CB1 in human melanoma cells and in addition, have found cytoplasmic accumulation of CB1 associated with cytoskeletal filaments.
We tested CB1 agonists on human melanoma in vitro with the use of several cell lines. As agonist, we used the natural ligand, AEA, its stable analogues Met-F-AEA, ACEA and an inverse agonist AM251, where the analogues are highly selective for CB1 compared with CB2. We confirmed the antiproliferative effect of CB1 agonists on human melanoma cells with an IC50 range of 3–10 μM. Further, we showed that the effect of CB1 modulators is primarily due to potent induction of apoptosis, similarly to previous data on various cancer types [16]. However, the significant antiproliferative effect of CB1 modulators may also be due to induction of cell necrosis as well as to G2/M arrest in cell cycle in certain sensitive melanoma cell lines, therefore having complex pathomechanism. Our studies have also indicated that the combination of various CB1 agonists resulted in an additive antiproliferative effect in human melanoma cells.
Cannabinoids have been shown to have anti-migratory effect in certain tumor cell types [25, 26] and here we provide evidence that they may have similar effect in human melanoma cells as well, suggesting a complex antitumoral mechanism of action. Previously, a stable CB1 agonist was tested in a mouse melanoma metastasis model where the drug was administered peritumorally and a significant antiproliferative effect was detected on the primary tumor [16]. Although the reported data suggested that parallel to the effect on the primary tumor, CB1 modulation may have antimetastatic effect [16], the specificity of this cannot be proved due to the inhibitory effect on the primary tumor. We used a human melanoma spleen-liver metastasis model and the CB1 modulator was administered systematically. In this model we did not find significant antiproliferative effect of ACEA on the primary tumor, but we were able to confirm the previous data regarding mouse melanoma [16] that CB1 agonist(s) have a specific antimetastatic effect in vivo. The metastatic cascade is a complex process involving growth at the primary site, vascularization, intravasation, organ colonization and establishment of secondary tumor in the metastatic organ, where the migratory potential of disseminating tumor cells is a rate limiting step. Our observation that CB1 modulation has an antimigratory effect besides apoptosis induction in human melanoma, similar to other cancer types [25, 26], suggests that this activity may significantly contribute to its antimetastatic effect observed in vivo.
The molecular mechanism of melanoma cell apoptosis induced by CB1 modulation was reported to involve inhibition of AKT and dephosphorylation of Rb [16]. AKT has emerged as a novel molecular target in cancer [33, 34], including melanoma [35]. In clear-cell renal cell cancer, mTOR inhibition was proved to be highly effective clinically in therapy-resistant tumors [36, 37]. Since human melanoma is highly similar to clear-cell renal cell cancer in its resistance to chemotherapy and relative sensitivity to cytokines (IFNα, IL-2), it seems probable that they may share a common molecular target, the PI3K/AKT/mTOR pathway, which controls their apoptotic sensitivity. Accordingly, further testing of CB1 modulators in human melanoma is warranted. We raise the issue that various CB1 agonists may have similar pro-apoptotic effect in human melanoma, therefore selection of the right modulator can be based on the potential side effects [38].
Abbreviations
- 2-AG:
-
2-arachidonoylglycerol
- A:
-
Adenosine
- ACEA:
-
Arachidonyl-2-chloroethylamide
- AEA:
-
Anandamide
- AKT:
-
Protein kinase B
- AM251:
-
N-piperidinyl-iodophenyl-dichlorophenyl-methylpyrazole-carboxamide
- BSA:
-
Bovine serum albumin
- C:
-
Cytosine
- Ca:
-
Calcium
- CB:
-
Cannabinoid
- CB1:
-
Cannabinoid receptor 1
- CB2:
-
Cannabinoid receptor 2
- CNR1:
-
Gene of cannabinoid receptor 1
- cDNA:
-
Complementary deoxyribonucleic acid
- DEPC:
-
Diethylpyrocarbonate
- DMSO:
-
Dimethyl sulfoxide
- DNA:
-
Deoxyribonucleic acid
- COX:
-
Cyclooxygenase
- EDTA:
-
Ethylenediaminetetraacetic acid
- FAAH:
-
Fatty acid amide hydrolase
- FCS:
-
Fetal calf serum
- FITC:
-
Fluorescein isothiocyanate
- G:
-
Guanine
- GPCR:
-
G protein-coupled receptor
- IC50:
-
Half maximal inhibitory concentration
- IFN:
-
Interferon
- IL:
-
Interleukin
- LOX:
-
Lipooxygenase
- MAGL:
-
Monoacylglycerol lipase
- MAPK:
-
Mitogen-activated protein kinase
- Met-F-AEA:
-
2-methyl-2-fluoro-anandamide
- mTOR:
-
Mammalian target of rapamycin
- MTT:
-
Thiazolyl blue tetrazolium bromide
- P:
-
Probability
- PBS:
-
Phosphate-buffered saline
- PCR:
-
Polymerase chain reaction
- PI:
-
Propidium iodide
- PI3K:
-
Phosphatidylinositol-3 kinase
- RAF:
-
RAF oncogene
- RAS:
-
RAS oncogene
- Rb:
-
Retinoblastoma
- RNA:
-
Ribonucleic acid
- SCID:
-
Severe combined immunodeficiency
- T:
-
Thymine
References
Wang J, Ueda N (2009) Biology of endocannabinoid synthesis system. Prostaglandins Other Lipid Mediat 89:112–119
Flygare J, Sander B (2008) The endocannabinoid system in cancer-potential therapeutic target? Semin Cancer Biol 18:176–189
Mouslech Z, Valla V (2009) Endocannabinoid system: an overview of its potential in current medical practice. Neuro Endocrinol Lett 30:153–179
Bifulco M, Di Marzo V (2002) Targeting the endocannabinoid system in cancer therapy: a call for further research. Nat Med 8:547–550
Alexander A, Smith PF, Rosengren RJ (2009) Cannabinoids in the treatment of cancer. Cancer Lett 285:6–12
Alpini G, Demorrow S (2009) Changes in the endocannabinoid system may give insight into new and effective treatments for cancer. Vitam Horm 81:469–485
Fowler CJ, Gustafsson SB, Chung SC et al (2010) Targeting the endocannabinoid system for the treatment of cancer–a practical view. Curr Top Med Chem 10:814–827
Bifulco M, Malfitano AM, Pisanti S et al (2008) Endocannabinoids in endocrine and related tumours. Endocr Relat Cancer 15:391–408
Portella G, Laezza C, Laccetti P et al (2003) Inhibitory effects of cannabinoid CB1 receptor stimulation on tumor growth and metastatic spreading: actions on signals involved in angiogenesis and metastasis. FASEB J 17:1771–1773
Pisanti S, Bifulco M (2009) Endocannabinoid system modulation in cancer biology and therapy. Pharmacol Res 60:107–116
Bifulco M, Laezza C, Gazzerro P et al (2007) Endocannabinoids as emerging suppressors of angiogenesis and tumor invasion (review). Oncol Rep 17:813–816
Sarfaraz S, Afaq F, Adhami VM et al (2005) Cannabinoid receptor as a novel target for the treatment of prostate cancer. Cancer Res 65:1635–1641
Gazzerro P, Malfitano AM, Proto MC et al (2010) Synergistic inhibition of human colon cancer cell growth by the cannabinoid CB1 receptor antagonist rimonabant and oxaliplatin. Oncol Rep 23:171–175
Biro T, Toth BI, Hasko G et al (2009) The endocannabinoid system of the skin in health and disease: novel perspectives and therapeutic opportunities. Trends Pharmacol Sci 30:411–420
Casanova ML, Blazquez C, Martinez-Palacio J et al (2003) Inhibition of skin tumor growth and angiogenesis in vivo by activation of cannabinoid receptors. J Clin Invest 111:43–50
Blazquez C, Carracedo A, Barrado L et al (2006) Cannabinoid receptors as novel targets for the treatment of melanoma. FASEB J 20:2633–2635
Sosman JA, Puzanov I (2006) Molecular targets in melanoma from angiogenesis to apoptosis. Clin Cancer Res 12:2376s–2383s
Denkert C, Kobel M, Berger S et al (2001) Expression of cyclooxygenase 2 in human malignant melanoma. Cancer Res 61:303–308
Tabolacci C, Lentini A, Provenzano B et al (2010) Similar antineoplastic effects of nimesulide, a selective COX-2 inhibitor, and prostaglandin E1 on B16-F10 murine melanoma cells. Melanoma Res 20:273–279
Liu B, Khan WA, Hannun YA et al (1995) 12(S)-hydroxyeicosatetraenoic acid and 13(S)-hydroxyoctadecadienoic acid regulation of protein kinase C-alpha in melanoma cells: role of receptor-mediated hydrolysis of inositol phospholipids. Proc Natl Acad Sci U S A 92:9323–9327
Raso E, Dome B, Somlai B et al (2004) Molecular identification, localization and function of platelet-type 12-lipoxygenase in human melanoma progression, under experimental and clinical conditions. Melanoma Res 14:245–250
Ladanyi A, Timar J, Paku S et al (1990) Selection and characterization of human melanoma lines with different liver-colonizing capacity. Int J Cancer 46:456–461
Dome B, Raso E, Dobos J et al (2005) Parallel expression of alphaIIbbeta3 and alphavbeta3 integrins in human melanoma cells upregulates bFGF expression and promotes their angiogenic phenotype. Int J Cancer 116:27–35
Deli T, Varga N, Adam A et al (2007) Functional genomics of calcium channels in human melanoma cells. Int J Cancer 121:55–65
Grimaldi C, Pisanti S, Laezza C et al (2006) Anandamide inhibits adhesion and migration of breast cancer cells. Exp Cell Res 312:363–373
Ramer R, Hinz B (2008) Inhibition of cancer cell invasion by cannabinoids via increased expression of tissue inhibitor of matrix metalloproteinases-1. J Natl Cancer Inst 100:59–69
Hersey P, Zhuang L, Zhang XD (2006) Current strategies in overcoming resistance of cancer cells to apoptosis melanoma as a model. Int Rev Cytol 251:131–158
Eberle J, Fecker LF, Hossini AM et al (2008) Apoptosis pathways and oncolytic adenoviral vectors: promising targets and tools to overcome therapy resistance of malignant melanoma. Exp Dermatol 17:1–11
La Porta CA (2009) Mechanism of drug sensitivity and resistance in melanoma. Curr Cancer Drug Targets 9:391–397
Sarnataro D, Grimaldi C, Pisanti S et al (2005) Plasma membrane and lysosomal localization of CB1 cannabinoid receptor are dependent on lipid rafts and regulated by anandamide in human breast cancer cells. FEBS Lett 579:6343–6349
Osborne KD, Lee W, Malarkey EB, et al (2009) Dynamic imaging of cannabinoid receptor 1 vesicular trafficking in cultured astrocytes. ASN Neuro 1.
Bari M, Oddi S, De Simone C et al (2008) Type-1 cannabinoid receptors colocalize with caveolin-1 in neuronal cells. Neuropharmacology 54:45–50
Engelman JA (2009) Targeting PI3K signalling in cancer: opportunities, challenges and limitations. Nat Rev Cancer 9:550–562
Liu P, Cheng H, Roberts TM et al (2009) Targeting the phosphoinositide 3-kinase pathway in cancer. Nat Rev Drug Discov 8:627–644
Madhunapantula SV, Robertson GP (2009) The PTEN-AKT3 signaling cascade as a therapeutic target in melanoma. Pigment Cell Melanoma Res 22:400–419
Hudes GR, Berkenblit A, Feingold J et al (2009) Clinical trial experience with temsirolimus in patients with advanced renal cell carcinoma. Semin Oncol 36(Suppl 3):S26–S36
Porta C, Figlin RA (2009) Phosphatidylinositol-3-kinase/Akt signaling pathway and kidney cancer, and the therapeutic potential of phosphatidylinositol-3-kinase/Akt inhibitors. J Urol 182:2569–2577
European public assessment report. Acomplia. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/000666/WC500021282.pdf.
Acknowledgments
This work was supported by TAMOP 4.2.1b, OTKA-NK72595 (JTi) and OTKA-K84173 (JTó).
Author information
Authors and Affiliations
Corresponding author
Additional information
István Kenessey and Balázs Bánki equal contribution.
Rights and permissions
About this article
Cite this article
Kenessey, I., Bánki, B., Márk, Á. et al. Revisiting CB1 Receptor as Drug Target in Human Melanoma. Pathol. Oncol. Res. 18, 857–866 (2012). https://doi.org/10.1007/s12253-012-9515-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-012-9515-y