Abstract
Bone morphogenetic protein (BMP) 4 plays a crucial role in tumor invasion and metastasis of various human cancers. However, little is known about the correlation of BMP4 expression with clinical aggressiveness and prognosis in hepatocellular carcinoma (HCC). The aim of this study was to investigate the expression of BMP4 in HCC and determine its correlation with tumor progression and prognosis. Immunohistochemistry assay was used to determine the expression of BMP4 in HCC and corresponding paracarcinomatous tissues from 156 patients. The potential prognostic value of BMP4 was investigated by comparing the survival rates between the BMP4-positive and BMP4-negative HCC patients. Immunohistochemically, BMP4 protein expression in the HCC tissues (120/156, 76.9%) was significantly higher than that in the paracarcinomatous tissues (19/156, 12.2%, P < 0.01). The expression of BMP4 in HCC was associated with number of tumor nodules (P = 0.02), Edmondson grade (P = 0.03), TNM stage (P = 0.009), and vascular invasion (P = 0.006). In univariate survival analysis, the significant associations of the BMP4 protein overexpression with shortened patients’ overall and disease-free survival were found (P = 0.001 and 0.006, respectively). Furthermore, its expression was found to be an independent factor for predicting both overall (P = 0.009) and disease-free survival (P = 0.022) of HCC in multivariate analysis. Our data suggest for the first time that BMP4 is overexpressed in HCC tissues and may also act as a novel marker for predicting the recurrence and prognosis of HCC patients after surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is one of the most frequent cause of cancer-related death worldwide, especially in Southeast Asia [1]. It is commonly associated with chronic hepatitis B virus (HBV) or hepatitis C virus (HCV) infections and chronic exposure to the aflatoxin B1. Owing to the advances in surgical techniques and perioperative care, the short-term survival of HCC patients after curative treatment have been improved greatly [2]. However, most HCC patients lose the chance of hepatic resection or liver transplantation because of vascular invasion or metastasis. Even for the patients who have undergone curative treatment, the long-term survival remains unsatisfied due to postoperative recurrence or metastasis. Therefore, HCC remains one of the deadliest cancers with a 5-year survival rate of only 5% [3]. Assessment of the prognosis of HCC remains difficult because of the limited prognostic value of conventional clinicopathological parameters. For example, a-fetoprotein (AFP) levels and des-carboxy prothrombin levels are reported to be indicators of tumor progression associated with patient survival. But they are not sufficient to accurately discriminate the tumor progression of HCC patients. Thus, to identify novel molecular markers for enhancing the accuracy of conventional prognostic factors would be necessary to guide medical treatments.
Bone morphogenetic proteins (BMPs), initially identified in the 1960s, belong to the transforming growth factor-β(TGF-β) superfamily [4]. These proteins are multi-functional growth factors and involved in morphogenesis, cell proliferation and differentiation, apoptosis and general organogenesis by interacting with SMADs [5]. Recent studies have demonstrated that BMPs have growth inhibitory and stimulatory effects on cancer cells [6–8]. BMP4, as a member of BMPs, plays an important role in development because Bmp4 null mice die early during embryogenesis [9]. Besides this function, BMP4 have recently been shown to regulate bone and cartilage formation, morphogenesis, cell proliferation and apoptosis of a wide variety of tissues and cells. Interestingly, emerging body of evidence indicates that BMP4 also plays a role in various types of cancers. For example, BMP4 induced migration and invasion of colon, ovarian, and pancreatic cancer cells [10–12]. BMP4 overexpression has been observed in the high-risk premalignant and malignant lesions of oral epithelium, breast cancer and esophageal squamous cell carcinoma [13–15]. In recent studies, treatment with recombinant BMP4 was found to inhibit the tumorigenic potential of human brain tumor-initiating cells, reduce angiogenesis in malignant melanoma, and induce apoptosis of myeloma cells [16]. Of our interests, Maegdefrau et al. [17] found increased BMP4 mRNA and protein in HCC cell lines and tissue samples compared to primary human hepatocytes and corresponding non-tumorous tissue. They also demonstrated that BMP4 could promote tumor migratory and invasive potential of HCC cell lines. However, little is known about the correlation of BMP4 expression with clinical aggressiveness and prognosis in HCC. This study was designed to evaluate BMP4 expression in a hospital-based cohort of patients with HCC by immunohistochemistry and to elucidate the expression of BMP4 in HCC and its association with clinicopathological characteristics and prognosis.
Materials and Methods
Patients and Tissue Samples
The study was approved by the Research Ethics Committee of 302nd Hospital of PLA, Beijing, China. Informed consent was obtained from all of the patients. All specimens were handled and made anonymous according to the ethical and legal standards.
For immunohistochemistry, 156 pairs of formalinfixed and paraffin-embedded blocks of tumor and paracarcinomatous tissues were obtained from 156 patients with HCC who had undergone curative surgical resection between 2001 and 2006 at the 302nd Hospital of PLA, Beijing, China. None of the patients recruited in this study had chemotherapy or radiotherapy before the surgery. One hundred and twenty-eight males and 28 females comprise of the 156 patients, with the mean age of 50.6 years (range, 20–78 years). HCC diagnosis was based on World Health Organization (WHO) criteria [18]. Tumor differentiation was defined according to the Edmondson grading system [19]. Liver function was assessed using the Child-Pugh scoring system [20]. Tumor staging was determined according to the sixth edition of the tumor-node-metastasis (TNM) classification of the International Union against Cancer [21]. The clinicopathological findings of 156 patients are summarized in Table 1.
The complete follow-up data were obtained from all 156 patients. The patients were followed until October 16, 2010. The mean follow-up was of 28.6 months (range, 2–76 months). All patients were prospectively monitored using a-fetoprotein (AFP), abdominal ultrasonography, and chest X-ray every 3–6 months after surgery. Computed tomography and/or magnetic resonance imaging were used if necessary. The overall survival (OS) was defined as the interval between the surgery and the death of patients or the last observation. The data were censored at the last followup for living patients. Disease-free survival (DFS) was measured from the date of resection until the detection of the recurrence tumor or the last follow-up assessment. In the DFS analysis, the data were censored for patients without tumor recurrence.
Immunohistochemistry Analysis
Immunohistochemical staining was carried out following the manufacturer’s instructions. Briefly, the paraffin-embedded tissues were cut at 3 μm and stained following being dried on ProbeOn Plus (Fisher Scientific International, Hampton, NH, USA). Staining was done using avidin- biotin complex with a microprobe manual stainer (Fisher Scientific International). The slide to which a paraffin section was attached went through deparaffinization and hydration, and was then treated with a solution of Peroxidase-blocking reagent (Dako, Glostrup, Denmark) to exhaust endogenous peroxidase activity. The sections were processed with antigen retrieval by being boiled in citrate buffer (pH 6.0) for 20 min and then cooled for an additive 20 min at room temperature. Subsequently, the sections were incubated in a 10% hydrogen peroxide solution for 15 min to eliminate endogenous peroxidase activity. The slides were incubated overnight with the primary antibody against BMP4 (1:100; mouse monoclonal antibody, sc-81000; Santa Cruz Biotechnology, Inc. USA) at 4°C. Secondary antibodies for the detection of primary antibodies were reacted for 10 min using anti-mouse IgG (Sigma, St. Louis, MO, USA) to which biotin was attached, and then washed with buffer solution and reacted with horseradish peroxidase for 10 min. Being washed again, peroxidase activity was visualized with DAB as a chromogen. All sections were rinsed and counterstained lightly with Harris hematoxylin. The negative controls were processed in a similar manner with PBS instead of primary antibody.
Following a hematoxylin counterstaining, immunostaining was scored by two independent experienced pathologists, who were blinded to the clinicopathological parameters and clinical outcomes of the patients. The scores of the two pathologists were compared and any discrepant scores were trained through re-examining the stainings by both pathologists to achieve a consensus score. The number of positive-staining cells showing immunoreactivity in the cytoplasm for BMP4 in ten representative microscopic fields was counted and the percentage of positive cells was calculated. The percentage scoring of immunoreactive tumor cells was as follows: 0 (0%), 1 (1–10%), 2 (11–50%) and 3 (>50%). The staining intensity was visually scored and stratified as follows: 0 (negative), 1 (weak), 2 (moderate) and 3 (strong). A final score was obtained for each case by multiplying the percentage and the intensity score. Therefore, tumors with a multiplied score exceeding 4 (median of total scores for BMP4) were deemed to be positive expressions of BMP4; all other scores were considered to be negative.
Statistical Analysis
The software of SPSS version13.0 for Windows (SPSS Inc, IL, USA) and SAS 9.1 (SAS Institute, Cary, NC) was used for statistical analysis. Fisher’s exact test and the X2 test were performed to assess associations between BMP4 expression and clinicopathological parameters. The Kaplan-Meier method was used for survival analysis, and differences in survival were estimated using the log-rank test. A multivariate survival analysis was performed for all parameters that were significant in the univariate analyses using the Cox regression model. Differences were considered statistically significant when P was less than 0.05.
Results
Immunohistochemical Expression of BMP4 in HCC and Paracarcinomatous Liver Tissues
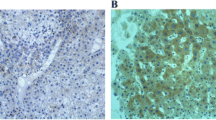
Immunohistochemical analysis revealed that BMP4 staining in HCC tissues was mainly localized in the cytoplasm of cancer cells, some of which stained strongly, while others exhibited little or no staining at all (Fig. 1a). BMP4 expression was absent or sporadic in non-tumorous liver tissues (Fig. 1b). In addition, the positive expression rate of BMP4 protein in the HCC tissues (120/156, 76.9%) was significantly higher than that in the paracarcinomatous tissues (19/156, 12.2%, P ≤ 0.01).
Association of BMP4 Expression with the Clinicopathological Features of the HCCs
We evaluated the association between BMP4 expression and clinicopathological features, including age, gender, tumor size, number of tumor nodules, tumor capsula, HBsAg status, serum AFP level, Edmondson grade, vascular invasion, Child-Pugh class, and TNM stage (Table 1). Whereas no significant differences were noted with respect to age, gender, tumor size, tumor capsula, HBsAg status, serum AFP level and Child-Pugh class, the BMP4-positive tumors had more tumor nodules (P = 0.02) and were higher Edmondson grade (P = 0.03) and TNM stage (P = 0.009), respectively. In addition, the vascular invasion was detected significantly more frequently in the BMP4-positive group (P = 0.006).
Prognostic Values of BMP4 Expression in HCCs
The mean OS rates after resection of the patients of BMP4-positive and BMP4-negative groups were 10.9% and 61.3%, respectively, and the mean DFS rates were 8.2% and 51.8%, respectively. The patients with BMP4-positive expression have significantly poorer OS and DFS after curative resection than those without BMP4 expression (P = 0.001 and 0.006, respectively; Fig. 2). In addition, the survival benefits were also found in those with earlier TNM stage, absence of vascular invasion, single nodule, and lower Edmondson grade, whereas others were not of predictive values (Table 2). Multivariate survival analysis calculated by Cox regression enrolling above-mentioned significant parameters revealed BMP4 expression (P = 0.009 and 0.022, respectively), TNM stage (P = 0.026 and 0.038, respectively), number of tumor nodules (P = 0.013 and 0.032, respectively), and vascular invasion (P = 0.013 and 0.023, respectively) were the independent prognostic factors for both OS and DFS in patients with HCC after curative resection, while Edmondson grade was only the prognosticator for DFS (P = 0.031) (Table 3).
Discussion
To the best of our knowledge, this is the first study to investigate the association between the expression pattern of BMP4 and the aggressive progression, and the prognostic value of BMP4 in HCC. Increased expression of BMP4 was observed in tumor tissues with more tumor nodules, higher Edmondson grade and TNM stage, and present of vascular invasion. In addition, patients with BMP4-positive had significantly poorer survival. On Cox multivariate regression analysis, expression of BMP4 was an independent prognostic factor for both OS and DFS of patients with HCC. Therefore, it is proposed that the presence of BMP4 may be used as a marker for the prediction of HCC recurrence and prognosis.
BMPs, as members of the TGF-β superfamily, have been of interest in cancer because of their versatile functions, such as growth inhibitory and stimulatory effects on cancer cells. It has also been found that the BMP signaling pathway has critical roles in embryogenesis, organogenesis, cell growth, differentiation, cell migration, and cell death [22]. Due to the diversity of these biological functions, it is not surprising that BMPs have been associated with control of proliferation and differentiation in normal and tumor cells. For example, in colorectal cancer, the BMP signaling pathway has been demonstrated to be related with the tumor development by the identification of BMPR-IA mutation in patients with juvenile polyposis syndrome [23]. Using a tissue microarray and immunohistochemistry, researchers also found the inactivation of BMP signaling in sporadic colorectal cancers by demonstrating the loss of BMPR-II, Smad4, and nuclear pSmad1/5/8 expression [24]. In addition, because the BMP signaling pathway promotes differentiation and represses proliferative capacity of prostate epithelial cells, the disregulation of this pathway are often observed in metastatic prostate cancer [25]. Among BMPs, the BMP4 gene has gained more attention because it contains several polymorphic sites and has genetic susceptibility to development of various malignancies. Capasso et al. [26] indicated a role of the predicted functional non-synonymous SNP 6007 C/T of BMP4 in susceptibility to melanoma and its inXuence on BMP4 gene expression. Besides theses, previous studies implicated the functions of BMP4 in both promotion and inhibition of cancer progression. Deng et al. [27] has demonstrated that BMP4 is over-expressed in colonic adenocarcinomas and confers invasive phenotype during progression of colon cancer. Ketolainen et al. [14] have recently shown that BMP4 is commonly expressed in breast cancer and stimulates cell migration and invasion in breast cancer cell lines through the activation of the canonical SMAD signaling pathway. HAMADA et al. [28] also clearly revealed that BMP4 activated ERK and p38 MAPK pathways and that these activations facilitated the induction of MSX2 together with the canonical Smad signaling pathway in pancreatic cancer cells. Furthermore, Piccirillo et al. [29] have suggested BMP4 as a novel, non- cytotoxic therapeutic eVector, which may be used to prevent growth and recurrence of human glioblastomas.
Here, we pay more attention to the involvement of BMP4 in the progression of HCC. In the previous study, Maegdefrau et al. [17] found that BMP4 was highly expressed in most HCC tissues compared with normal liver, which was consistent with our data. They also reported that the impairment of BMP4 in HCC cells may inhibit their stimulatory effect on tube formation of human microvascular endothelial cells, suggesting that BMP4 also promotes tumour vasculogenesis. Our data also described that the vascular invasion was detected significantly more frequently in the BMP4-positive group. In addition to these, we found that the expression of BMP4 in HCC was positively associated with number of tumor nodules, Edmondson grade, TNM stage and patients’ survival. Together, these findings indicate a prominent role for BMP4 in tumourigenic processes.
In conclusion, our study suggests that BMP4 is overexpressed in HCC tissues and may also act as a novel marker for predicting the recurrence and prognosis of HCC patients after surgery. Further studies are needed to investigate the precise function of BMP4 in the progression of HCC.
References
Yang H, Lin M, Xiong F, Yang Y, Nie X, McNutt MA, Zhou R (2011) Combined lysosomal protein transmembrane 4 beta-35 and argininosuccinate synthetase expression predicts clinical outcome in hepatocellular carcinoma patients. Surg Today 41:810–817
Farazi PA, DePinho RA (2006) Hepatocellular carcinoma pathogenesis: from genes to environment. Nat Rev Cancer 6:674–687
Thorgeirsson SS, Grisham JW (2002) Molecular pathogenesis of human hepatocellular carcinoma. Nat Genet 31:339–346
Chen D, Zhao M, Mundy GR (2004) Bone morphogenetic proteins. Growth Factors 22:233–241
Simic P, Vukicevic S (2005) Bone morphogenetic proteins in development and homeostasis of kidney. Cytokine Growth Factor Rev 16:299–308
Marki D, Celi T, Grkovi A, Spanjol J, Fukar Z, Grahovac B, Ethorevi G, Bobinac D (2011) mRNA expression of bone morphogenetic proteins and their receptors in human renal cell carcinoma. Urol Int In press
Yuen HF, Chan YP, Cheung WL, Wong YC, Wang X, Chan KW (2008) The prognostic significance of BMP-6 signaling in prostate cancer. Mod Pathol 21:1436–1443
Motoyama K, Tanaka F, Kosaka Y, Mimori K, Uetake H, Inoue H, Sugihara K, Mori M (2008) Clinical significance of BMP7 in human colorectal cancer. Ann Surg Oncol 15:1530–1537
Hogan BL (1996) Bone morphogenetic proteins in development. Curr Opin Genet Dev 6:432–438
Virtanen S, Alarmo EL, Sandström S, Ampuja M, Kallioniemi A (2011) Bone morphogenetic protein −4 and −5 in pancreatic cancer–novel bidirectional players. Exp Cell Res 317:2136–2146
McLean K, Gong Y, Choi Y, Deng N, Yang K, Bai S, Cabrera L, Keller E, McCauley L, Cho KR, Buckanovich RJ (2011) Human ovarian carcinoma–associated mesenchymal stem cells regulate cancer stem cells and tumorigenesis via altered BMP production. J Clin Invest 121:3206–3219
Slattery ML, Lundgreen A, Herrick JS, Kadlubar S, Caan BJ, Potter JD, Wolff RK (2011) Genetic variation in bone morphogenetic protein and colon and rectal cancer. Int J Cancer In press
Qiao B, Johnson NW, Chen X, Li R, Tao Q, Gao J (2011) Disclosure of a stem cell phenotype in an oral squamous cell carcinoma cell line induced by BMP-4 via an epithelial-mesenchymal transition. Oncol Rep 26:455–461
Ketolainen JM, Alarmo EL, Tuominen VJ, Kallioniemi A (2010) Parallel inhibition of cell growth and induction of cell migration and invasion in breast cancer cells by bone morphogenetic protein 4. Breast Cancer Res Treat 124:377–386
Shon SK, Kim A, Kim JY, Kim KI, Yang Y, Lim JS (2009) Bone morphogenetic protein-4 induced by NDRG2 expression inhibits MMP-9 activity in breast cancer cells. Biochem Biophys Res Commun 385:198–203
Hjertner O, Hjorth-Hansen H, Borset M, Seidel C, Waage A, Sundan A (2001) Bone morphogenetic protein-4 inhibits proliferation and induces apoptosis of multiple myeloma cells. Blood 97:516–522
Maegdefrau U, Arndt S, Kivorski G, Hellerbrand C, Bosserhoff AK (2011) Downregulation of hemojuvelin prevents inhibitory effects of bone morphogenetic proteins on iron metabolism in hepatocellular carcinoma. Lab Invest In press
Ishak KG, Anthony PP, Sobin LH (1994) Nonepithelial tumors. In: Ishak KG (ed) Histological typing of tumors of the liver. World Health Organization International Classification of Tumors. Springer, Berlin, pp 22–27
Wittekind C (2006) Pitfalls in the classification of liver tumors. Pathologe 27:289–293
Gao Q, Qiu SJ, Fan J, Zhou J, Wang XY, Xiao YS (2007) Intratumoral balance of regulatory and cytotoxic T cells is associated with prognosis of hepatocellular carcinoma after resection. J Clin Oncol 25:2586–2593
Zhu XD, Zhang JB, Zhuang PY, Zhu HG, Zhang W, Xiong YQ (2008) High expression of macrophage colony-stimulating factor in peritumoral liver tissue is associated with poor survival after curative resection of hepatocellular carcinoma. J Clin Oncol 26:2707–2716
Shen H, Huang GJ, Gong YW (2003) Effect of transforming growth factor beta and bone morphogenetic proteins on rat hepatic stellate cell proliferation and trans-differentiation. World J Gastroenterol 9:784–787
Slattery ML, Lundgreen A, Herrick JS, Wolff RK, Caan BJ (2011) Genetic variation in the transforming growth factor-β signaling pathway and survival after diagnosis with colon and rectal cancer. Cancer 117:4175–4183
Lombardo Y, Scopelliti A, Cammareri P, Todaro M, Iovino F, Ricci-Vitiani L, Gulotta G, Dieli F, de Maria R, Stassi G (2011) Bone morphogenetic protein 4 induces differentiation of colorectal cancer stem cells and increases their response to chemotherapy in mice. Gastroenterology 140:297–309
Lee YC, Cheng CJ, Bilen MA, Lu JF, Satcher RL, Yu-Lee LY, Gallick GE, Maity SN, Lin SH (2011) BMP4 promotes prostate tumor growth in bone through osteogenesis. Cancer Res 71:5194–5203
Capasso M, Ayala F, Russo R, Avvisati RA, Asci R, Iolascon A (2009) A predicted functional single-nucleotide polymorphism of bone morphogenetic protein-4 gene affects mRNA expression and shows a significant association with cutaneous melanoma in Southern Italian population. J Cancer Res Clin Oncol 135:1799–1807
Deng H, Ravikumar TS, Yang WL (2007) Bone morphogenetic protein-4 inhibits heat-induced apoptosis by modulating MAPK pathways in human colon cancer HCT116 cells. Cancer Lett 256:207–217
Hamada S, Satoh K, Hirota M, Fujibuchi W, Kanno A, Umino J, Ito H, Satoh A, Kikuta K, Kume K, Masamune A, Shimosegawa T (2009) Expression of the calcium-binding protein S100P is regulated by bone morphogenetic protein in pancreatic duct epithelial cell lines. Cancer Sci 100:103–110
Piccirillo SG, Reynolds BA, Zanetti N, Lamorte G, Binda E, Broggi G, Brem H, Olivi A, Dimeco F, Vescovi AL (2006) Bone morphogenetic proteins inhibit the tumorigenic potential of human brain tumour-initiating cells. Nature 444:761–765
Author information
Authors and Affiliations
Corresponding author
Additional information
Xiaodong Guo and Lu Xiong contributed equally to this study.
Rights and permissions
About this article
Cite this article
Guo, X., Xiong, L., Zou, L. et al. Upregulation of Bone Morphogenetic Protein 4 is Associated with Poor Prognosis in Patients with Hepatocellular Carcinoma. Pathol. Oncol. Res. 18, 635–640 (2012). https://doi.org/10.1007/s12253-011-9488-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-011-9488-2