Abstract
The late side-effects of the local therapy of early breast cancer depend on many patient- and therapy-related parameters. We aimed at investigating the factors that influence the cosmetic and functional outcomes among our breast cancer patients after breast-conserving surgery and conformal radiotherapy, with or without adjuvant systemic therapy. A study was made of the association of the cosmetic outcome after a median follow-up time of 2.4 years and the clinical data on 198 patients extracted from a prospectively compiled database. Breast tenderness occurred more frequently among patients ≤50 years old (p < 0.05). Long-term side effects were related to radiotherapy-related factors the most, while no effect of the systemic therapy could be detected. The risk of hyperpigmentation, breast edema and breast fibrosis increased by 18%, 23% and 7%, respectively for every 100 cm3 increase in the irradiated breast volume, while that of breast edema and breast fibrosis increased by 21% and 12%, respectively for every 10 cm3 increase in the boost volume. Patients who received a photon boost were significantly more likely to develop breast edema and fibrosis than those who received electrons (p < 0.005). Dose inhomogeneity was related to the volume of the irradiated breast (p = 0.037). Dyspigmentation developed more often among patients older than 50 years, while smoking favoured both dyspigmentation and teleangiectasia. Breast edema was related to dyspigmentation (p = 0.003), fibrosis (p < 0.001) and breast asymmetry (p = 0.032), whereas none of these abnormalities were associated with teleangiectasia. Body image changes were more frequent at a younger age (p < 0.005), while the need to change clothing habits occurred more often at an older age (p < 0.05). Radiotherapy-related parameters appear to exert the greatest effect on the overall cosmetic outcome after breast-conserving surgery and postoperative radiotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast-conserving surgery, usually followed by whole-breast irradiation, is the most widely used surgical option for early breast cancer [1–5]. Postoperative irradiation and adjuvant systemic therapy improve both local control and survival [2, 6]. The cosmetic and the functional outcome after postoperative breast radiotherapy depend on numerous patient- and therapy-related factors. The age, the menopausal status, the weight and the general health status of the patient, the stage of the tumor and the surgical intervention clearly influence the results [7]. The radiogenic changes of the breast, such as dyspigmentation, teleangiectasia or breast edema, fibrosis causing breast swelling and tenderness, depend on the dose, the irradiated volume and the individual radiosensitivity [7–10]. The overdosing of small volumes in the irradiated breast (i.e. dose inhomogeneity), a phenomenon related to the technique applied, favors breast fibrosis [11–15]. The impact of the systemic therapy on the cosmetic outcome has been the subject of numerous studies [11, 13, 15–17]. Adjuvant chemotherapy [18] and tamoxifen therapy [6, 18] have been suggested to predict a poor cosmetic outcome [17]. We set out a retrospective cohort analysis to study the patient- and therapy related factors that may influence the cosmetic and functional outcomes among our breast cancer patients after breast-conserving surgery and conformal radiotherapy, with or without adjuvant systemic therapy.
Materials and Methods
The clinical data on 198 breast cancer patients who participated in postoperative radiotherapy were extracted from a prospectively compiled database. The mean age of the population was 62.0 ± 10.6 (range 25–89) years. Eligible patients had undergone unilateral breast-conserving surgery, with or without sentinel lymph node biopsy or/and axillary lymph node dissection and conformal radiotherapy 1–5 years before the interview. Patients with prior malignancy or any other significant health problem were excluded, as were those on glucocorticoid therapy. The patients had been operated between May 2004 and December 2008, at either the Department of Surgery, University of Szeged, or at smaller surgical departments.
Use of the following adjuvant medical therapies was permitted: a taxane-based postoperative chemotherapy regimen (involving either docetaxel or paclitaxel at conventional doses) completed ≥4 weeks prior to the radiotherapy (n = 23, 13.1%); adjuvant hormone therapy with either tamoxifen (20 mg/day) or an aromatase inhibitor (anastrozole, 1 mg/day, or letrozole, 2.5 mg/day), started ≥2 weeks before the initiation of radiotherapy (n = 49, 24.7% and n = 48, 24.2%, respectively); patients who did not received any systemic medication during or after the radiotherapy were also eligible for enrolment (n = 75, 37.9%). CT-based three-dimensional treatment planning and conformal radiotherapy were performed in all cases with the patient in a supine position. All relevant technical details have been published previously [19]. Briefly, CT images were acquired at 1 cm intervals throughout the entire planning volume. The target volume and organs at risk (OARs) were contoured on the CT slices in the radiotherapy planning system. The planning target volume (PTV) coverage was analyzed via the dose-volume histograms and isodose visualization. Local or locoregional radiotherapy was chosen according to the local protocol. The tumor bed boost was delivered with either 6 MV photon or 8–15 MeV electron fields. The radiation dose to the remaining breast parenchyma/chest wall and to the lymph nodes, if indicated, was 25x2 Gy (prescribed to the mean of the PTV); a tumor bed boost of 5-8x2 Gy was delivered when necessary. OAR constraints were used as previously described [19].
The following radiotherapy-related data were extracted from our database: the PTV, the volume of the PTV that received more than 47.5 Gy, but less than 53.5 Gy (V95%–107%), the overdosed volume of the PTV (V>107%), the volume and dose of the tumor bed boost, the technique used and the breast separation (BS), i.e. the distance between the points at which the tangential fields entered the body.
The cosmetic outcome was evaluated at a single routine 6-month check-up visit, 1–5 years after the radiotherapy. The patients were examined, and a questionnaire relating to the following items was completed: the overall cosmetic success in the opinions of the patient and the physician (G. K. or Z. K.), the presence of breast fibrosis or edema, teleangiectasia or dyspigmentation, all scored on a 4-point categorical scale according to the modified system of Johansen et al. [15, 18]. Briefly, the following scoring system was used. Breast fibrosis: 0: none, 1: density slightly increased, 2: increased density and firmness, 3: very marked density with retraction; Edema: 0: none, 1: trace thickening of the skin, 2: marked edema, leathery skin texture, 3: severe edema with papillary formation; Teleangiectasia: 0: none, 1: <1 cm, 2: 1–4 cm, 3: >4 cm; Dyspigmentation: 0: none, 1: mild, 2: moderate, 3: severe. Physicians classified the cosmetic result as excellent if no asymmetry or changes of the skin or the breast contour occurred; in the case of slight, moderate or severe manifestation of at least one of these factors, the outcome was considered good, fair or poor, respectively. The patients were asked whether they felt pain or tenderness in the operated breast, and whether they had experienced changes in their body image or in their clothing habits. The length of the excision scar and the difference (regarded as measurable when ≥1.0 cm) in the jugulum-nipple distance (indicative of breast asymmetry) were recorded. Data were additionally collected on smoking habits, with the participants categorized as past or present smokers or non-smokers.
The various patient- and radiotherapy-related characteristics associated with the cosmetic and functional outcomes were analyzed by the means of the chi-square test, analysis of variance and logistic regression. The Kappa test was applied to investigate the connection between the opinions of the physicians and the patients as concerns the cosmetic outcome. Binary univariate logistic regression models were first utilized separately, followed by the multivariate logistic regression model to examine joint effects and interactions. Statistical analysis was performed with SPSS 15.0 for Windows.
Results
A total of 198 patients were enrolled in the study. The mean age of the population was 62.0 ± 10.6 (range 25–89) years. The median follow-up time was 2.4 (range 1.2–5.9) years. Most of the tumors measured ≤2.0 cm and were lymph node-negative (Table 1). Data concerning the radiotherapy are presented in Table 2. One hundred and sixty-seven patients (84.3%) received only breast irradiation, while 31 patients (15.7%) both breast and regional lymph node irradiation. Twenty patients (10.1%) were treated with taxane-based chemotherapy before the radiotherapy. The systemic therapy before the radiotherapy started with an aromatase inhibitor or tamoxifen alone, in 49 (24.7%) and 48 (24.2%) cases, respectively. Four (2.0%) and two (1.0%) patients received a taxane-based chemotherapy and an aromatase inhibitor or tamoxifen thereafter, respectively. Seventy-five patients (37.9%) did not participate in systemic therapy.
The patients and the physicians considered the cosmetic outcome to be excellent or good in 76.3% and 47% of the cases, respectively; a weak correlation was observed between the opinions of the physicians and the patients (Table 3). A large majority of the patients (n = 160, 80.8%) underwent their breast surgery at our institute, and 127 (84.1%) of them regarded the cosmetic outcome as excellent or good more often than did those who were operated on in smaller surgical departments (n = 24/38, 63.2%) (p = 0.05). In the view of the physicians, the cosmetic outcome overall was less often excellent or good as the tumor size increased: the mean±SD tumor size was 1.3 ± 0.7 and 1.5 ± 0.7 cm in the excellent and good vs. the fair and poor outcome groups, respectively (p = 0.015). Among those patients who had an axillary block dissection, the physician considered the cosmetic outcome excellent or good in 29 cases (37.7%), and fair or poor in 48 cases (62.3%, p = 0.04). A significant relation or interaction was not detected between these variables in the logistic regression analysis. The incidence and severity of hyperpigmentation, fibrosis, edema and teleangiectasia are presented in Table 4.
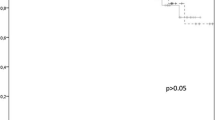
Thirty-one patients (19.7%) complained of pain in the operated breast, while 81 (40.9%) reported tenderness. Breast tenderness occurred significantly more often among premenopausal women or patients ≤50 years old (both p < 0.05). The average age (±SD) of the patients who complained or had no complaint of breast tenderness was 59.8 ± 11.6 and 63.6 ± 9.6 years, respectively (p < 0.05). Breast fibrosis and/or edema occurred in 67 (33.9%) and 23 (11.6%) patients, respectively. Skin hyperpigmentation, found in altogether 71 patients (35.9%) occurred in 59 (83.1%) of the patients >50 years old, and 12 (16.9%) of the women ≤50 years old, respectively (p < 0.05), and its incidence decreased with the median time elapsed after radiotherapy (2.1 and 2.5 years in the presence and the absence of hyperpigmentation, respectively, p = 0.02). Teleangiectasia developed in 22 patients (11.1%).
The mean±SD tumor size was 1.6 ± 0.7 cm if moderate dyspigmentation occurred, and 1.3 ± 0.7 cm in the other cases (p < 0.05). The average ±SD tumor size was 1.9 ± 1.4 cm if breast marked edema occurred, and 1.4 ± 0.7 cm in the other cases (p < 0.05). Breast edema occurred in 15 (65.2%) and 8 (34.8%) among those patients who had or did not have axillary lymph node dissection, respectively (p = 0.01). Breast edema was related to dyspigmentation (p = 0.003), fibrosis (p < 0.001) and breast asymmetry (p = 0.032), whereas none of these abnormalities were associated with teleangiectasia.
Thirty-three (16.7%) patients mentioned changes in their clothing habits and 44 (22.3%) had experienced a variation in their body image. Those patients who noticed body image changes were younger than those who did not (the mean±SD age was 57.6 ± 10.1 vs. 63.3 ± 10.4 years, respectively, p < 0.005). Eighty-six percent of the postmenopausal, and 74% of the ≤50 years old women needed to change their clothing habits (p < 0.05), while this measure was 8.9% and 1.3% according to whether the patient received or did not receive systemic therapy, respectively (p < 0.005).
In most cases, the excisional scar was in the upper quadrants (n = 130, 65.7%). The mean±SD length of the scar was 8.2 ± 3.5 (range, 3.0–28.0) cm. An average (±SD) breast asymmetry (n = 159) of 2.7 ± 1.9 (range, 1.0–15.0) cm was found in 159 of the 194 evaluable patients (nipple excision was performed in 4 patients). The average extent (±SD) of breast asymmetry was 2.4 ± 2.2 cm vs. 1.5 ± 0.9 cm when the tumor was located in the upper vs. the lower quadrants, respectively (p = 0.05), and 2.1 ± 1.7 cm vs. 2.9 ± 2.9 cm when the tumor diameter was ≤2 cm vs. >2 cm, respectively (p < 0.05). The length of the scar did not influence any attribute of the cosmetic outcome.
More severe dyspigmentation and breast edema occurred in patients with larger PTVs (p < 0.001). The risk of more severe dyspigmentation and breast edema increased by 18% and 23%, respectively, for every 100 cm3 increase in irradiated breast volume (OR = 1.18, 95% CI: 1.07–1.31; OR = 1.23, 95% CI: 1.12–1.36). Breast edema was more frequent with increasing BS (p < 0.005), and was not related to nodal irradiation. The incidence of breast fibrosis was significantly higher with larger PTVs (mean±SD value of PTV, patients with breast fibrosis: 1221.5 ± 571.8 cm3 and patients without fibrosis: 1058.7 ± 416.9 cm3, p < 0.05). The risk of breast fibrosis increased by 7% for every 100 cm3 increase in irradiated breast volume (OR = 1.07, 95% CI: 1.00–1.14). No association was found between any of the attributes of cosmesis and the dose inhomogeneity within the irradiated volume. The dose inhomogeneity was related to the volume of the irradiated breast (p = 0.037). The risk of V>107% ≥ 1% increased by 8% for every 100 cm3 increase in irradiated breast volume (OR = 1.078, 95% CI: 1.003–1.158).
A higher boost volume favored breast fibrosis and edema (p < 0.005 and p < 0.001, respectively). The risk of breast edema and breast fibrosis increased by 21% and 12%, respectively, for every 10 cm3 increase in boost volume (OR = 1.21, 95% CI: 1.09–1.33 and OR = 1.12, 95%, CI: 1.03–1.12). Breast edema and/or fibrosis was more frequent among those patients who received a photon boost than those who received electrons (breast edema: 13/63 vs. 4/98, p = 0.001 and breast fibrosis: 26/63 vs. 26/98, p = 0.038). No association was found between the administration of systemic therapy and cosmetic or functional outcome.
One hundred and twenty-five (63.1%) patients had never smoked, 49 (24.7%) had smoked previously and 24 patients (12.1%) smoked during the radiotherapy. Skin dyspigmentation and teleangiectasia developed significantly less often among the patients who had never smoked (both p < 0.05).
Discussion
We evaluated the cosmetic outcome 1–5 years after breast-conserving surgery, postoperative radiotherapy and systemic therapy. Primarily radiotherapy-related factors such as the irradiated volume, the radiation dose and the beam quality, but also the size of the tumor, the age of the patient, the surgical intervention and the smoking habits influenced the cosmesis. Our analysis provided novel information on the association between late radiation toxicity and the dose-volume attributes of the radiotherapy. With the intent of broad analysis we applied a comprehensive instrument [15, 18], quantitative radiotherapy data, and considered systemic therapy.
More than three-quarters of the patients considered the cosmetic outcome to be excellent or good, which is similar to the observations by other groups [14, 15, 17]. In contrast, in the opinion of the physicians, only about half of the cases belonged in this category. One explanation of the discrepancy might be the strict conditions used for the evaluation of the cosmetic appearance. A further contributing factor could have been the relatively short follow-up time in our study since the consideration of the radiation side-effects by the patient may change in time [16].
The location and stage of the tumor clearly determine the cosmetic outcome [12, 14, 15, 20–22]. In our study, breast edema, fibrosis, teleangiectasia and dyspigmentation were all related to the size of the tumor, and were interrelated. Similarly as in the studies by Johansen et al. and Taylor et al., we found that tumors located in the upper quadrants and those with a larger diameter were predisposed to more severe breast asymmetry [14, 15].
The available data are not completely unequivocal as regards the relation between a young age and the cosmetic and functional outcomes. Most studies report an improved cosmetic outcome among younger women [14, 17, 23, 24] though the opposite to has been suggested [15]. We did not find any age-specific differences in the overall cosmetic outcome. However, the different components of the cosmetic and functional results did depend on the age of the patient. The more frequent breast tenderness or pain among ≤50 years old women might have been related to hormonal effects, and the change in body image in this age group could have been dependent on psychological or mental factors. The higher incidence of dyspigmentation in those over 50 years of age is probably due to the age-dependent response to radiation, with an increased accumulation of melanin and lipofuscin, the pigments related to aging and oxidative stress [25]. It is well known that radiogenic side-effects are more frequent for larger breasts. Nevertheless, to the best of our knowledge, this analysis is the first to report cosmetic results after conformal breast radiotherapy in relation to dose-volume data. Although conformal radiotherapy was applied in the study by Lilla et al., a detailed analysis of the radiotherapy-related data was not reported [24]. In that and other studies, the associations between the side-effects and the irradiated volume were based on approximate data such as the size of the breast or the bra cup [15, 18, 24, 26, 27] and the chest wall separation [26]. Likewise, dose homogeneity in the entire PTV was predicted after visualization of the dose distribution at the central axis [22, 26] or was related to the use or avoidance of tissue compensators or wedges [14, 28, 29]. In one of these studies, the dose homogeneity demonstrated a parallel with the breast size [26], an effect confirmed by our results. In our study, no association was detected between the dose inhomogeneity and poorer cosmesis as a result of restricting the overdosed volume (V>107%) to 1% of the PTV, and the superposition of individually weighted 6 or 15 MV segmental fields to the tangential fields [19]. Our finding that the photon boost was more often related to breast edema and fibrosis is in accordance with the outcome of the robust analysis by Murphy et al. [27]. We consider that this phenomenon is a consequence of the larger volume irradiated when 2 photon fields are applied as compared with the use of one direct electron field. For the best cosmetic result, the use of an electron boost is recommended, or the IMRT technique may be utilized [30–32].
Systemic therapy has been found detrimental to the cosmetic and functional outcome in many studies [13, 14, 18, 22, 27, 33]. Most investigated the effects of chemotherapy with CMF or an antracycline-containing regimen, either concurrently or sequentially with radiotherapy [14, 15, 33]. In the study by Johansen et al., chemotherapy with CMF or with tamoxifen was associated with a 5-fold (CMF) or 10-fold (tamoxifen) higher risk of breast fibrosis, respectively [15]. Taxane-based combinations have become a routine option in adjuvant chemotherapy, but the effects of sequentially applied taxane-based chemotherapy on breast cosmesis have not yet been reported. We did not detect adverse effects of such a regimen, though the number of patients was low. The third-generation aromatase inhibitors currently compromise the standard endocrine therapy of postmenopausal women with hormone-dependent breast cancer. However, tamoxifen is still administered in premenopausal and selected postmenopausal women. Azria et al. demonstrated in their primal work that letrozole does not exert a detrimental effect on early or late radiation skin toxicity [10]. In accordance with these findings, aromatase inhibitor therapy in our analysis did not have any effect on the studied parameters. In contrast, the prospective study by Azria et al. revealed that the concurrent administration of tamoxifen with radiotherapy doubled the risk of subcutaneous fibrosis [8]. Likewise, we found that concomitant tamoxifen increased the risk of lung fibrosis (OR = 2.442) [19]. Due to the limitations of the analyses, other reports have not provided a clear answer as to the effect of simultaneous tamoxifen therapy with radiotherapy on the cosmetic outcome [6, 12, 14, 18]. Our survey suggested that tamoxifen therapy was related to the change in body image, but since no specific radiogenic changes were detected, the frequent weight gain associated with this medication may have played a role in this outcome measure.
Conclusions
The cosmetic outcome after breast-conserving surgery is primarily determined by the stage of the disease and the consequences of radiotherapy. Despite the achievements made regarding the effectiveness and side-effect profile of modern radiotherapy, a careful estimate of its benefits remains necessary in each case and determination of the individual treatment strategy accordingly.
References
Voogd AC, Nielsen M, Peterse JL, Blichert-Toft M, Bartelink H, Overgaard M et al (2001) Differences in risk factors for local and distant recurrence after breast-conserving therapy or mastectomy for stage I and II breast cancer: pooled results of two large European randomized trials. J Clin Oncol 19:1688–1697
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER et al (2002) Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 347:1233–1241
Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A et al (2002) Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 347:1227–1232
Offersen BV, Overgaard M, Kroman N, Overgaard J (2009) Accelerated partial breast irradiation as part of breast conserving therapy of early breast carcinoma: a systematic review. Radiother Oncol 90:1–13
Fyles AW, McCready DR, Manchul LA, Trudeau ME, Merante P, Pintilie M et al (2004) Tamoxifen with or without breast irradiation in women 50 years of age or older with early breast cancer. N Engl J Med 351:963–970
Fowble B, Fein DA, Hanlon AL, Eisenberg BL, Hoffman JP, Sigurdson ER et al (1996) The impact of tamoxifen on breast recurrence, cosmesis, complications, and survival in estrogen receptor-positive early-stage breast cancer. Int J Radiat Oncol Biol Phys 35:669–677
Munshi A, Kakkar S, Bhutani R, Jalali R, Budrukkar A, Dinshaw KA (2009) Factors influencing cosmetic outcome in breast conservation. Clin Oncol (R Coll Radiol) 21:285–293
Azria D, Gourgou S, Sozzi WJ, Zouhair A, Mirimanoff RO, Kramar A et al (2004) Concomitant use of tamoxifen with radiotherapy enhances subcutaneous breast fibrosis in hypersensitive patients. Br J Cancer 91:1251–1260
Azria D, Betz M, Bourgier C, Sozzi WJ, Ozsahin M (2010) Identifying patients at risk for late radiation-induced toxicity. Crit Rev Oncol Hematol, Epub ahead of print
Azria D, Belkacemi Y, Romieu G, Gourgou S, Gutowski M, Zaman K et al (2010) Concurrent or sequential adjuvant letrozole and radiotherapy after conservative surgery for early-stage breast cancer (CO-HO-RT): a phase 2 randomised trial. Lancet Oncol 11:258–265
Bartelink H, Horiot JC, Poortmans PM, Struikmans H, Van den Bogaert W, Fourquet A et al (2007) Impact of a higher radiation dose on local control and survival in breast-conserving therapy of early breast cancer: 10-year results of the randomized boost versus no boost EORTC 22881-10882 trial. J Clin Oncol 25:3259–3265
Wazer DE, Morr J, Erban JK, Schmid CH, Ruthazer R, Schmidt-Ullrich RK (1997) The effects of postradiation treatment with tamoxifen on local control and cosmetic outcome in the conservatively treated breast. Cancer 80:732–740
Collette S, Collette L, Budiharto T, Horiot JC, Poortmans PM, Struikmans H et al (2008) Predictors of the risk of fibrosis at 10 years after breast conserving therapy for early breast cancer: a study based on the EORTC Trial 22881-10882 ‘boost versus no boost’. Eur J Cancer 44:2587–2599
Taylor ME, Perez CA, Halverson KJ, Kuske RR, Philpott GW, Garcia DM et al (1995) Factors influencing cosmetic results after conservation therapy for breast cancer. Int J Radiat Oncol Biol Phys 31:753–764
Johansen J, Overgaard J, Rose C, Engelholm SA, Gadeberg CC, Kjaer M et al (2002) Cosmetic outcome and breast morbidity in breast-conserving treatment—results from the Danish DBCG-82TM national randomized trial in breast cancer. Acta Oncol 41:369–380
Curran D, van Dongen JP, Aaronson NK, Kiebert G, Fentiman IS, Mignolet F et al (1998) Quality of life of early-stage breast cancer patients treated with radical mastectomy or breast-conserving procedures: results of EORTC Trial 10801. The European Organization for Research and Treatment of Cancer (EORTC), Breast Cancer Co-operative Group (BCCG). Eur J Cancer 34:307–314
Cardoso MJ, Cardoso J, Santos AC, Vrieling C, Christie D, Liljegren G et al (2007) Factors determining esthetic outcome after breast cancer conservative treatment. Breast J 13:140–146
Johansen J, Overgaard J, Overgaard M (2007) Effect of adjuvant systemic treatment on cosmetic outcome and late normal-tissue reactions after breast conservation. Acta Oncol 46:525–533
Kahan Z, Csenki M, Varga Z, Szil E, Cserhati A, Balogh A et al (2007) The risk of early and late lung sequelae after conformal radiotherapy in breast cancer patients. Int J Radiat Oncol Biol Phys 68:673–681
Van Limbergen E, Rijnders A, van der Schueren E, Lerut T, Christiaens R (1989) Cosmetic evaluation of breast conserving treatment for mammary cancer. 2. A quantitative analysis of the influence of radiation dose, fractionation schedules and surgical treatment techniques on cosmetic results. Radiother Oncol 16:253–267
Borger JH, Kemperman H, Smitt HS, Hart A, van Dongen J, Lebesque J et al (1994) Dose and volume effects on fibrosis after breast conservation therapy. Int J Radiat Oncol Biol Phys 30:1073–1081
Wazer DE, DiPetrillo T, Schmidt-Ullrich R, Weld L, Smith TJ, Marchant DJ et al (1992) Factors influencing cosmetic outcome and complication risk after conservative surgery and radiotherapy for early-stage breast carcinoma. J Clin Oncol 10:356–363
Pezner RD, Patterson MP, Hill LR, Vora NL, Desai KR, Lipsett JA (1985) Breast retraction assessment. Multiple variable analysis of factors responsible for cosmetic retraction in patients treated conservatively for stage I or II breast carcinoma. Acta Radiol Oncol 24:327–330
Lilla C, Ambrosone CB, Kropp S, Helmbold I, Schmezer P, von Fournier D et al (2007) Predictive factors for late normal tissue complications following radiotherapy for breast cancer. Breast Cancer Res Treat 106:143–150
Porta EA (2002) Pigments in aging: an overview. Ann N Y Acad Sci 959:57–65
Moody AM, Mayles WP, Bliss JM, A’Hern RP, Owen JR, Regan J et al (1994) The influence of breast size on late radiation effects and association with radiotherapy dose inhomogeneity. Radiother Oncol 33:106–112
Murphy C, Anderson PR, Li T, Bleicher RJ, Sigurdson ER, Goldstein LJ et al (2010) Impact of the radiation boost on outcomes after breast-conserving surgery and radiation. Int J Radiat Oncol Biol Phys Epub ahead of print
Ellenbogen R, Jankauskas S, Collini FJ (1990) Achieving standardized photographs in aesthetic surgery. Plast Reconstr Surg 86:955–961
Sarin R, Dinshaw KA, Shrivastava SK, Sharma V, Deore SM (1993) Therapeutic factors influencing the cosmetic outcome and late complications in the conservative management of early breast cancer. Int J Radiat Oncol Biol Phys 27:285–292
Hill-Kayser CE, Chacko D, Hwang WT, Vapiwala N, Solin LJ (2010) Long-term clinical and cosmetic outcomes after breast conservation treatment for women with early-stage breast carcinoma according to the type of breast boost. Int J Radiat Oncol Biol Phys, Epub ahead of print
Harsolia A, Kestin L, Grills I, Wallace M, Jolly S, Jones C et al (2007) Intensity-modulated radiotherapy results in significant decrease in clinical toxicities compared with conventional wedge-based breast radiotherapy. Int J Radiat Oncol Biol Phys 68:1375–1380
McDonald MW, Godette KD, Whitaker DJ, Davis LW, Johnstone PA (2010) Three-year outcomes of breast intensity-modulated radiation therapy with simultaneous integrated boost. Int J Radiat Oncol Biol Phys 77:523–530
Abner AL, Recht A, Vicini FA, Silver B, Hayes D, Come S et al (1991) Cosmetic results after surgery, chemotherapy, and radiation therapy for early breast cancer. Int J Radiat Oncol Biol Phys 21:331–338
Conflict of Interest Statement
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kelemen, G., Varga, Z., Lázár, G. et al. Cosmetic Outcome 1–5 Years After Breast Conservative Surgery, Irradiation and Systemic Therapy. Pathol. Oncol. Res. 18, 421–427 (2012). https://doi.org/10.1007/s12253-011-9462-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-011-9462-z