Abstract
Neurosurgeons sometimes find it difficult to locate tumors precisely during microsurgery, particularly tumors located in the brain parenchyma because of the absence of boundaries in this region. Image-guided neurosurgical techniques conducted with the help of neuronavigation systems have been developed and have gained importance recently. Accuracy is vital during image-guided neurosurgery. We used a phantom to evaluate the errors introduced during navigation. The three errors evaluated were skin-shift, marker-gap, and table-rotation errors. The skin-shift error occurs if the fiducial markers positioned on the scalp move when the head is fixed to a head holder with head pins. The marker-gap error occurs when the marker ball is positioned incorrectly in the marker socket. The table-rotation error occurs when the operating table is rotated for obtaining an intraoperative MR image and then returned to its original position. Our results indicated that skin shift decreased the navigation accuracy by an error of more than 4 mm, and the gap between the marker ball and the socket resulted in a decrease in navigation accuracy by an error of more than 5 mm. The table-rotation error was found to be negligible. The errors can be avoided by ensuring that the fiducial markers are positioned appropriately on the scalp and the marker ball is fitted well in the marker socket. A phantom is useful for evaluating accuracy, particularly for evaluating errors intrinsic to different operating rooms. Periodic quality assurance by use of a phantom in each operating room might aid in maintaining the accuracy of neuronavigation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The development of image-guided neurosurgery has had a great impact on the practice of neurosurgery, especially with regard to intrinsic brain tumors [1]. Intrinsic brain tumors are often infiltrative in nature, invading the brain parenchyma. Definite boundaries of such tumors cannot be observed under an operative microscope, but magnetic resonance imaging (MRI), computed tomography, and other image modalities facilitate the visualization of these boundaries. Total or near-total image-guided resection of these tumors has been shown to be related to a good prognosis. On the other hand, the boundary zone of the tumor could have certain functions, and excessive resection of this area could lead to severe neurological deficits. Image-guided neurosurgery is, therefore, a robust tool for the appropriate resection of infiltrative tumors.
Accuracy is very important during image-guided neurosurgery. Brain shift and deformation of the brain due to withdrawal of cerebrospinal fluid dramatically decrease the accuracy of the neuronavigation based on preoperative images. Intraoperative MRI and constant improvement of neuronavigation techniques can eliminate the errors introduced by brain shift [2].
Errors related to registration are also important. Registration, which is carried out immediately before the initiation of surgery, involves the synchronization of actual positions on the patient’s scalp with those observed on the images captured by the neuronavigator. In general, fiducial markers are used for the registration of reference points on the patient’s scalp. Errors can be introduced during the alignment of the fiducial markers with the registration points. In clinical practice, marker balls are sometimes inserted inappropriately into the marker base, resulting in a gap between the ball and the marker plate. This gap causes a vertical shift of the registration point. In addition, the skin shift during registration can introduce errors. The patient’s head is usually held in place by a Sugita head holder, which is equipped with four head pins; this is one of the most frequently used head fixation systems in neurosurgery. The application of the head pins to the scalp causes the scalp to move to some extent; the fiducial markers, particularly those near the head pins, also move, causing the registration points to shift horizontally.
Another major error could be introduced by changes in the spatial relationship between the reference antenna and the patient’s head. Our operating room was equipped with an intraoperative MRI unit. It consisted of an operating table that could be rotated by 180° and could be inserted into the MRI scanner for image acquisition during surgery. Errors may be introduced by changes in the spatial relationship between the reference antenna and the patient’s head.
Although accuracy is important during image-guided neurosurgery, there is little information about the factors that could influence accuracy. Using a phantom, we evaluated the errors introduced by skin shift, the gap between the marker ball and marker socket, and changes in the spatial relationship between the patient’s head and the reference antenna as being important clinically.
Materials and methods
Our operating room was equipped with a vertical magnetic field (0.4 Tesla), a permanent magnet, an open MRI scanner (Aperto Inspire; Hitachi Medical Co., Chiba, Japan), and an operating table (Mizuho, Tokyo, Japan). For all examinations, we used a gradient echo pulse sequence (repetition time 21 ms, echo time 9 ms, fractional anisotropy 70°, slice thickness 10 mm, matrix size 256 × 256). A Vector Vision Compact (BrainLAB AG) navigation system was used.
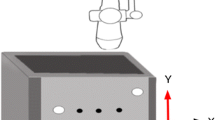
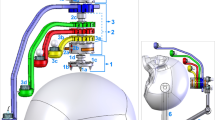
This system facilitates the positioning of more than five fiducial markers on the surface of the scalp (it is recommended that six fiducial markers be used). A fiducial marker consists of a marker plate, a marker socket, and a marker ball. The essential steps for registration and neuronavigation are the following: (1) The marker ball is inserted into the marker socket (Fig. 1). (2) The six fiducial markers are positioned on the patient’s scalp in the ward. (3) Usually, on the day before the surgery, MR images of the patient’s head bearing the fiducial markers are obtained (preoperative images). (4) On the day of the surgery, the patient is anesthetized in the operating room, and the patient’s head is fixed to the head holder with the four head pins. (5) The reference antenna is fixed to the operating table. (6) The marker sockets bearing the marker balls are replaced with registration sockets, but the marker plates are retained in the same position; the pointer in the operating room precisely locates the center of the registration sockets (Fig. 1). This procedure synchronizes the actual positions of the marker ball with the position of the marker ball depicted on the image. The neuronavigator emits infrared rays by which it can detect the three spheres of the reference antenna and the two spheres on the pointer, thereby determining the position of the tip of the pointer on the image. (7) After registration, surgery is performed under the guidance of the neuronavigator. If an intraoperative MRI is required during the surgery because of brain shift or for any other reason, the surgery is interrupted. The operating table is made horizontal near the opening of the scanner, rotated by 180°, and inserted into the scanner. After the imaging, the table is returned to the original position (Fig. 2), and the surgery is continued with the guidance of the updated neuronavigation information based on the initial registration (restoration of the initial registration information). If the spatial relationship between the patient’s head and the reference antenna changes, the accuracy of neuronavigation decreases.
Registration workflow for neuronavigation. a The marker plate is inserted into the patient’s head. b A fiducial marker consists of a marker plate, marker socket, and a marker ball. c The six fiducial markers are positioned on the marker plate. d, e After preoperative images are obtained, the marker sockets bearing the marker balls are replaced with registration sockets, but the marker plates are retained in the same position. f The center of registration sockets are pointed by the pointer precisely in the operating room
We examined three possible factors that introduce errors. First, the center of the marker ball must precisely correspond to the center of the registration socket; thus, the presence of a vertical gap between the marker ball and the bottom of the marker socket might introduce an error (Fig. 2). It is recommended that the marker ball be inserted deeply into the socket, but variations in the techniques of different operators can lead to errors.
The second possible error could be introduced by movement of the scalp when the patient’s head is fixed in the head fixation frame; this is termed skin-shift error. A surgical coil system integrated with a head fixation frame (head holder) allows imaging to be performed during surgery. However, when a head pin is screwed in place, the surrounding skin tightens and moves, resulting in a skin-shift error. When the surgeon performs the registration, the position of the marker, as determined from the preoperative MR images, changes from its original position (Fig. 3).
In the left image, the skin is tightened when the coil is fitted, and this causes a slight movement of the skin. In the right image, skin shift was produced intentionally during registration by moving of two points out of six fiducial markers 5 mm backward. Navigation accuracy was measured at 40 points under each condition
The spatial relationship between the head and the antenna is also important for navigational accuracy. The third error is the table-rotation error, which is caused by changes in the spatial relation between the antenna and the head; this occurs when the operating table is rotated by 180° and then returned to its original position after intraoperative MRI images are obtained (Fig. 4).
Our primary aim was to evaluate the marker-gap, skin-shift, and table-rotation errors. An acrylic phantom 25 cm × 15 cm × 15 cm in size was filled with water and used for evaluation of the navigation process. Four 1-cm acrylic blocks bearing small holes (φ = 0.86 mm) in the center were placed 1 cm apart against each wall of the phantom. The holes in the center of the blocks were filled with water and were represented by more intense signals in T1-weighted images (T1WI) than those for the acrylic blocks, allowing easy identification of the center of the blocks in T1WI. Six fiducial markers were positioned on the outer wall of the phantom (Fig. 5).
The fiducial markers were positioned at six points on the phantom such that they represented the actual positions of the markers on a human head. We used a pointer with two spheres to evaluate the errors. The steps undertaken for calculating the navigation accuracy were as follows: (1) The pointer was directed at the center of the block. (2) The screen of the Vector Vision Compact navigation system displayed the corresponding positions on axial, coronal, and sagittal images. The errors were determined with the help of these captured images. From the axial, sagittal, and coronal images, the distance between the pointer and the center of the block on the phantom was calculated (Fig. 6). The navigation error in each direction was calculated by a vector sum [3, 4]. Twenty points on the phantom were evaluated during a single registration procedure. In order to improve the accuracy of the error measurements, we performed another registration so that a total of 40 points were evaluated. The maximum error, average error, and standard deviation (SD) of the errors were calculated and used for statistical analysis.
Marker-gap error
Marker-gap error refers to the error caused by the vertical gap between the marker ball and the bottom of the marker socket, which often occurs because the marker ball is not fitted well into the socket. We evaluated the navigation error introduced when the gap distance between the marker ball and the socket was 0 mm (recommended gap distance), 1 mm (appeared to be fitted well), 2 mm (loosely fitted), and 3 mm (very loosely fitted).
Gap distances greater than 3 mm were not evaluated because a gap distance greater than 3 mm implied that the marker ball could not be fitted in the socket.
Skin-shift error
Errors introduced by skin shift were also evaluated. In our experience, we observed that two points positioned on either side of a marker moved by more than 5 mm in the area surrounding the head pin. Taking this into consideration, the two marker points in this study were positioned 5 mm behind their original position, and the navigation error was evaluated.
Table-rotation error
Errors could be introduced when the operating table is rotated by 180° and then returned to its original position. To investigate this, we fixed the phantom to the head holder and investigated whether errors occurred after the table was rotated.
Results
Marker-gap error
The results for navigational accuracy with regard to the gap between the marker ball and the bottom of the marker socket are shown in Table 1. No significant navigation errors occurred when the gap was 1 mm; however, the average error, SD, and maximum error were found to increase dramatically when the gap distance was greater than 2 mm; thus, a gap distance greater than 2 mm resulted in statistically significant navigation errors.
Skin-shift error
Student’s t test was performed. Errors introduced by skin shift were found to have a statistically significant effect on navigation accuracy (P < 0.001; Table 2).
Table-rotation error
Errors introduced before and after rotation of the operating table are shown in Table 3. Student’s t test was performed. The error was significantly greater after the rotation (P < 0.01), although the error was less than 3 mm, which is acceptable in a clinical situation.
Discussion
Despite the remarkable advances in brain tumor surgery, including the introduction of operative microscopes, precise removal of infiltrative brain tumors such as gliomas remains difficult. In many cases, the boundaries of such tumors cannot be distinguished even when viewed under the microscope. It has been reported that total or near-total resection of a tumor is associated with a better prognosis than is a subtotal or lesser resection. However, the problems faced by surgeons are that if larger portions of a tumor are excised, the risk of the patient developing postoperative neurologic complications is greater. Thus, advances in image-guided neurosurgery are expected to play an important role in the precise resection of intrinsic and infiltrative brain tumors. However, the accuracy and reliability of image-guided neurosurgery should be evaluated in light of errors that could potentially affect the accuracy of neuronavigation.
There are many factors that influence the accuracy of neuronavigation. The neuronavigation system has its intrinsic accuracy and limitations defined as less than 3 mm [5], and these limitations cannot be overcome by users. The registration procedure can introduce marker-gap errors, skin-shift errors, and errors due to table rotation. Before registration, the registration points are defined on the planning workstation. The center of the marker ball must be registered as the registration point to prevent an error from occurring. MRI conducted under high magnetic fields can result in distortion and fusion of the images, contributing to inaccuracies in the process. Once surgery has commenced, the spatial relationship between the head and the reference antenna ideally should not change. Application of force may cause the antenna to move unexpectedly, which usually results in a catastrophic decrease in navigation accuracy. Our operating room has an intraoperative MRI equipped with a rotating operating table. The operating table can be inclined, allowing the head to be suitably positioned during neurosurgery. The rotational and flexible characteristics of the table might influence the accuracy of neuronavigation. Of the errors introduced by these factors, some were considered negligible, whereas others were found to be large enough to warrant their evaluation; however, some errors occurred irrespective of the operator’s technique. The pointing error was evaluated before the start of this study, and it was found to be small (0–0.2 mm) (data not shown). We therefore evaluated the marker-gap, skin-shift, and table-rotation errors.
Our data indicate that accurate assembly of the fiducial markers is crucial. The gap distance between the marker ball and the bottom of the marker socket must be less than 1 mm. Skin shift also has a large influence on the accuracy; therefore, the fiducial markers must be positioned as far away from the head pins as possible. Table-rotation errors are also possible; however, these are negligible (<3 mm) and can be ignored in a clinical situation. In a clinical setting, the arm of the head holder may bend to some extent under the weight of the patient’s head and body, and this may result in a subtle shearing movement of the head despite it being fixed by the head pins. Therefore, one should be careful about drawing a conclusion from our data on the table-rotation error. Instead, we should pay attention to the accuracy after the table is returned to its original position. An ideal situation for overcoming all of the errors evaluated in this study would be intraoperative registration using intraoperative MRI. These errors are introduced when preoperative images are used for neuronavigation. With intraoperative MRI, the images obtained can be used for performing registration again, which would take into account changes caused by skin shift, brain shift, changes between the position of the head and reference antenna, and movement after the table has been returned to its original position. Marker-gap error can be corrected with the use of an intraoperative MRI machine; however, in many hospitals worldwide, operating rooms are not equipped with intraoperative MRI.
Conclusion
We evaluated three errors in neuronavigation by using a phantom model. We observed that the skin shift resulted in a more than 4-mm error in accuracy and that the gap between the marker ball and the marker socket resulted in a more than 5-mm error; therefore, it is crucial that fiducial markers are assembled precisely.
With the advances in image-guided neurosurgery, the importance of accuracy in neuronavigation procedures also increases. More attention must be paid to this accuracy, and the concept of quality assurance (QA) should be introduced into image-guided neurosurgery. The equipment and settings for image-guided neurosurgery differ among operating rooms. The use of a phantom for evaluating accuracy is effective, particularly in determining errors intrinsic to each operating room. Conducting periodic QA with use of phantoms might contribute to the maintenance of accuracy in neuronavigation for each operating room.
References
Nagashima Y, Hirose S, Suzukawa H, Naemura K, Takanobu H, Muragaki Y, et al. Improvement of a navigation system for the neurosurgery in the intraoperative MRI-equipped operating theater. J Jpn Soc Comput Aided Surg. 2003;5:331–2.
Iseki H, Muragaki Y, Nakamura R, Ozawa N, Taniguchi H, Hori T, et al. Intelligent operating theater using intraoperative open MRI. Magn Reson Med Sci. 2005;4:129–35.
Muto S, Ando H, Nagashima Y, Uematsu M, Suzukawa H, Nakamura R, et al. Clinical application of the navigation system for the neurosurgery in the intraoperative MRI-equipped operating theater using reflective ball markers. J Jpn Soc Comput Aided Surg. 2004;6:367–8.
Nagashima Y, Hirose S, Suzukawa K, Naemura K, Takanobu H, Muragaki Y, et al. Accuracy evaluation of navigation system during neurosurgery at open MRI theater and improvement of its maneuverability. J Jpn Soc Comput Aided Surg. 2004;6:5–13.
Brain Lab AG. Clinical user guide rev. 1.0. Vector vision cranial ver. 7.5J. Feldkirchen: Brain Lab AG; 2005.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Watanabe, Y., Fujii, M., Hayashi, Y. et al. Evaluation of errors influencing accuracy in image-guided neurosurgery. Radiol Phys Technol 2, 120–125 (2009). https://doi.org/10.1007/s12194-009-0053-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-009-0053-6