Abstract
To investigate whether it is possible to obtain adequate images at uniform image noise levels and reduced radiation exposure with our automatic tube current modulation (ATCM) technique for 64-detector CT. The study population consisted of 64 patients with known or suspected lung or abdominal disease. We used a 64-detector CT scanner (LightSpeed VCT, GE Healthcare, Waukesha, WI, USA) and a combined angular and longitudinal tube current modulation technique (Smart mA, GE Healthcare, Waukesha, WI, USA) to examine 34 patients. The scanning parameters were identical; the minimum and maximum tube current thresholds were 50 and 800 mA, respectively. For study of the constant tube current technique, 30 additional patients were examined at 350 mA. The CT number and image noise (SD of the CT number) were measured in the 64 patients at six levels, i.e., the center of the left ventricle, the liver dome, the porta hepatis, the center of the spleen and the right and left renal pelvis. When we used the ATCM technique, the mean image noise ranged from 8.40 at the center of the left ventricle to 11.31 at the porta hepatis; the mean tube current ranged from 105.9 mAs at the center of the left ventricle to 169.6 mAs at the center of the spleen. The mean dose reduction rate per constant tube current at 175 mAs ranged from 3.1 to 39.5%. By use of the ATCM technique, it is possible to maintain a constant image noise level with a 64-detector CT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Automatic tube current modulation (ATCM) with multidetector CT (MDCT) is analogous to the automatic exposure control and photo-timing techniques that have been used for automatically terminating radiographic exposure in conventional radiography [1–5]. This modulation technique adjusts the tube current from slice to slice depending on the regional body anatomy, thereby maintaining a constant user-specified quantum image noise level and improving the radiation-dose efficiency. It involves angular or x–y modulation, z-axis modulation, and combined or x–y–z-axis modulation. The combined angular and z-axis modulation technique has been introduced on commercially available MDCT scanners and represents the most comprehensive approach to CT dose reduction because the X-ray dose is adjusted to reflect patient-specific attenuation in all three planes [6, 7].
Because of technical improvements, the detector width along the z axis of MDCT scanners continues to increase. The detector width of our first 4-detector CT was 20 mm; the width of the 64-detector CT currently in use at our institute is 40 mm. Furthermore, as the tube rotation time of 0.8 s in 4-detector CT has been reduced to 0.5 s for 64-detector instruments, the volume coverage speed is now as much as 12.8 times faster. On these newer instruments featuring a greater volume coverage speed, automatic dose modulation via angular modulation may not work well in areas with different adjacent attenuation values, for example, at the interface of the lungs and abdomen, because the tube current is determined according to projection data 180° from the X-ray generation angle. Our purpose of this study was to investigate whether the ATCM technique, applied to 64-detector CT, can effectively provide images with uniform image noise at reduced radiation doses.
Materials and methods
Patients
The human research committee of our institutional review board approved our study; prior informed consent was obtained from all patients. Between April 2007 and May 2007, we enrolled 30 patients (15 women and 15 men, mean age 60.6 ± 15.8 years, range 23–85 years) in studies to assess the constant tube current (CTC) technique. Between June and July 2007, we enrolled another 34 patients (15 women and 19 men, mean age 60.4 ± 18.3 years, range 20–84 years) in studies to evaluate the ATCM technique. All patients had known or suspected lung or abdominal disease; all had undergone plain chest and abdominal CT studies. We studied patients with available plain CT scans because image noise (standard deviation of the CT number) for enhancement CT was affected corresponding to the dose rate and the total dose of contrast medium.
Automatic tube current modulation technique
We used a 64-detector CT scanner (LightSpeed VCT, GE Healthcare, Waukesha, WI, USA). The scanning parameters were: tube voltage, 120 kVp; detector collimation, 64 × 0.625 mm; beam pitch, 0.984; table speed, 39.37 mm per gantry rotation (gantry rotation time, 0.5 s); acquisition of 5.0 mm images reconstructed at 5.0 mm intervals; scan field of view (FOV), 50.0 cm; display FOV, 36.0 cm; matrix, 512 × 512; standard reconstruction kernel. In our assessment of the combined angular and longitudinal tube current modulation technique (Smart mA, GE Healthcare, Waukesha, WI, USA), we applied identical scanning parameters to study 34 patients; the minimum and maximum tube current thresholds were 50 (25 mAs) and 800 mA (400 mAs), respectively. The noise index was set at 10 HU according to our routine protocol [8–10].
The mean body height and weight of the 34 patients were 161.4 ± 10.2 cm and 58.94 ± 13.53 kg, respectively.
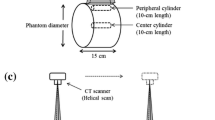
Constant tube current technique
We used the same 64-detector CT scanner to assess the CTC technique in 30 patients. The scans were acquired at 350 mA, 120 kVp (175 mAs); the CTDIvol was 15.21 mGy [11, 12]. Other parameters were the same as in our study of the ATCM technique [6, 7].
Quantitative data
For each patient, we recorded the maximum transverse (mean 30.0 cm at ATCM and 29.1 cm at CTC) and anteroposterior (mean 22.0 cm at ATCM and 21.5 cm at CTC) diameter of the abdomen on transverse images obtained at the liver dome, using a DICOM viewer (Image Vinus Pro, ver. 3.01, Yokogawa, Tokyo, Japan) and a color monitor (Radiforce R22, Eizo, Ishikawa, Japan). The CT number and image noise, represented by the standard deviation of the CT number, were measured in all 64 patients (constant mA, 30 patients; variable mA, 34 patients) at six levels, i.e., the center of the left ventricle, the liver dome, the porta hepatis, the center of the spleen and the right and left renal pelvis, by use of the same DICOM viewer and color monitor. A total of 396 images (66 patients × 6 levels) were measured by use of the region of interest and contrast shape (circular) and size (40 square pixels). Each image was measured at least three times for calculating the mean value. In our study of the ATCM technique, we recorded the tube current at each level of the image; the body mass index (BMI) was calculated with the formula BMI = weight (kg) divided by the square of the height (m) [13]. We categorized the BMI as follows: category 1: BMI ≤ 18.5 kg/m2 (underweight); category 2: BMI between 18.5 and 24.9 kg/ m2 (normal weight); category 3: BMI between 25 and 29.9 kg/ m2 (overweight); category 4: BMI ≥ 30 kg/ m2 (obese). BMI is an index of human constitution based on height and weight and a worldwide method of categorizing human constitution with the BMI is established [14, 15]. Therefore, we used the BMI for a parameter, which evaluates human constitution.
Statistical analysis
The image noise was calculated, and values obtained in the center of the left ventricle, the liver dome, the porta hepatis, the center of the spleen and the right and left renal pelvis with and without the ATCM technique were compared using Student’s t test. The image noise at different BMI values was compared by one-way analysis of variance (ANOVA). When the overall differences were statistically significant, we performed a post-hoc analysis using Dunnett’s method; the image noise at a BMI of 18.5–24.9 kg/m2 (normal weight) was used as control. Differences at P < 0.05 were considered statistically significant. To apply Student’s t test, we used one-way ANOVA and the post-hoc test and a statistical software program (SPSS, version 10.05, SPSS, Chicago, IL, USA).
Results
Table 1 compares the mean CT number, the mean image noise (SD of the CT number), and the mean SD of the image noise obtained at the six examined levels with the ATCM and the CTC technique. At 6.33 HU, the mean image noise with the CTC was lowest at the center of the left ventricle; it was 7.40 HU at the liver dome and 10.16 HU at the porta hepatis on images obtained with the CTC technique at 175 mAs. At the six levels examined, the CTC technique consistently yielded significantly lower image noise values than did the ATCM technique (P < 0.05 or P < 0.001).
With the ATCM technique, the mean image noise ranged from 8.40 HU at the center of the left ventricle to 11.31 at the porta hepatis. Although the mean image noise was lower at the center of the left ventricle and the liver dome than at the other levels examined, these values were close to the 10 HU noise index. At 175 mAs, the mean SD of the image noise was lower with the ATCM than with the CTC technique (1.09–1.39 HU vs. 1.20–2.56 HU).
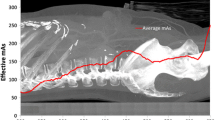
Table 2 shows the tube current reduction rate obtained with the ATCM technique. The mean tube current ranged from 105.9 mAs at the center of the left ventricle to 169.6 mAs at the center of the spleen. The mean reduction rate per constant tube current at 175 mAs ranged from 3.1% (at the center of the spleen) to 39.5% (at the center of the left ventricle). The difference in the range of the tube current was greatest in the right and left renal pelvis [range, 36.0–325.5 mAs; difference, 289.5 mAs vs. 288.0 mAs (the center of the left ventricle, the porta hepatis, the center of the spleen) and 284.0 mAs (liver dome)].
The mean tube current at the four different BMI classifications is shown in Table 3. At the center of the spleen, the difference between BMI category 1 (underweight) and category 4 (obese) with respect to the mean tube current was 236.5 mAs (range, 78.3–314.8 mAs); it was 223.0 mAs for the center of the left ventricle (range, 39.8 vs. 262.8 mAs). As shown in Table 4, the difference between BMI category 1 and category 4 with respect to image noise at the porta hepatis was 0 .91 HU (range, 10.68–11.59 HU); it was 4.52 HU (range, 7.29–11.81 HU) at the liver dome. When we evaluated the four BMI categories with one-way ANOVA, the overall difference in the mean image noise at each of the six levels examined was statistically significant (P < 0.001). In the liver dome, the mean image noise in BMI category 1 (7.29 HU) was significantly lower than in category 2 (8.87 HU; P < 0.001). At the center of the left ventricle, the liver dome and the right and left renal pelvis, the mean image noise in obese patients (BMI category 4) was significantly higher than those in patients of normal weight (BMI category 2; P < 0.001).
Discussion
In our CT scanner, the algorithm for ATCM is designed to maintain a constant image noise level as the attenuation values change from one rotation to the next. Our initial hypothesis posited that whereas the ATCM technique would fail to control the tube current at the interface of the lung and abdomen, i.e., at the liver dome, at the six levels studied, the tube current could be controlled and an almost constant image noise level could be maintained, even at the lung–abdomen interface. In the current study, we set the helical pitch at 0.984 because, at helical pitch values below 1.0, redundant projection data can be acquired and aliasing artifacts can be prevented [16]. We think that small pitch values less than 1.0 are effective for the ATCM to function well in even the portion where materials with very different attenuations are adjacent. On the contrary, the ATCM technique may fail to control the tube current if a pitch value larger than 1.0 is adopted. We are now investigating what is the maximum pitch for the effective use of the ATCM technique.
A prototype of a 256-detector CT scanner features a detector width of 128 mm [17]. At that width, techniques other than the current ATCM method must be devised to allow for optimization of the radiation dose.
In general, the image noise is inversely proportional and the radiation dose is proportional to the tube current [18–20]. With the ATCM technique, when the maximum tube current is sufficiently high, the image noise remains constant regardless of the patient BMI or weight. On the other hand, when the value of the maximum tube current is low, the image noise in overweight and obese patients may increase, preventing the acquisition of diagnostic images. We set the maximum tube current at 800 mA (400 mAs) in our assessment of the ATCM technique. We found that the image noise in overweight and obese patients was significantly higher than that in normal weight and underweight patients, although with the ATCM technique it was possible to maintain an almost constant image noise level in these individuals. Thus, when the ATCM technique is used, the maximum tube current should be based on both the image noise (image quality) and the radiation dose. Studies are underway in our laboratory for identifying the optimal maximum tube current.
In further attempts at radiation-dose reduction without degradation of the image quality, we must take into account the body and lesion size and contrast, the section thickness and the window level and width on the display monitor. However, these factors are not considered in the ATCM technique because it is difficult to assess their effects on lesion detection. Because dose modulation based on the contrast–noise ratio (CNR) may allow a further reduction in the radiation dose, we are investigating the relationship between lesion detectability and the CNR at various scan settings.
Our results are encumbered by some limitations. First, in our CTC scans we used 350 mA (175 mAs), which, in our system, is routine for abdominal scanning. Although the use of different tube currents may alter the dose reduction rate, we posit that 175 mAs represents an acceptable value because the mean tube current with the ATCM technique was 152.5 mAs. Second, the distribution of individuals (n = 34) among the four BMI categories was not uniform because the collection of patients with evenly distributed body types is difficult. To acquire a large study population, we are in the process of designing a multicenter study.
In conclusion, with the ATCM technique it is possible to maintain a constant image noise level with 64-detector CT regardless of the patient BMI. For optimizing the radiation dose for the next generation of CT scanners, such as the 256-detector instrument, new methods need to be developed.
References
Kalender WA, Wolf H, Suess C. Dose reduction in CT by anatomically adapted tube current modulation. II. Phantom measurements. Med Phys. 1999;26:2248–53
Greess H, Wolf H, Baum U, Lell M, Pirkl M, Kalender W, et al. Dose reduction in computed tomography by attenuation-based on-line modulation of tube current: evaluation of six anatomical regions. Eur Radiol. 2000;10:391–4
Kalra MK, Maher MM, Toth TL, Hamberg LM, Blake MA, Shepard JA, et al. Strategies for CT radiation dose optimization. Radiology. 2004;230:619–28
Dalal T, Kalra MK, Rizzo SM, Schmidt B, Suess C, Flohr T, et al. Metallic prosthesis: technique to avoid increase in CT radiation dose with automatic tube current modulation in a phantom and patients. Radiology. 2005;236:671–5
McCollough CH, Bruesewitz MR, Kofler JM Jr CT dose reduction and dose management tools: overview of available options. Radiographics. 2006;26:503–12
Kalra MK, Maher MM, Toth TL, Schmidt B, Westerman BL, Morgan HT, et al. Techniques and applications of automatic tube current modulation for CT. Radiology. 2004;233:649–57
Mulkens TH, Bellinck P, Baeyaert M, Ghysen D, Van Dijck X, Mussen E, et al. Use of an automatic exposure control mechanism for dose optimization in multi-detector row CT examinations: clinical evaluation. Radiology. 2005;237:213–23
Kalra MK, Maher MM, Kamath RS, Horiuchi T, Toth TL, Halpern EF, et al. Sixteen-detector row CT of abdomen and pelvis: study for optimization of Z-axis modulation technique performed in 153 patients. Radiology. 2004;233:241–9
Campbell J, Kalra MK, Rizzo S, Maher MM, Shepard JA. Scanning beyond anatomic limits of the thorax in chest CT: findings, radiation dose, and automatic tube current modulation. AJR Am J Roentgenol. 2005;185:1525–30
Rizzo S, Kalra M, Schmidt B, Dalal T, Suess C, Flohr T, et al. Comparison of angular and combined automatic tube current modulation techniques with constant tube current CT of the abdomen and pelvis. AJR Am J Roentgenol. 2006;186:673–9
Tsapaki V, Kottou S, Papadimitriou D. Application of European Commission reference dose levels in CT examinations in Crete, Greece. Br J Radiol. 2001;74:836–40
McNitt-Gray MF. AAPM/RSNA physics tutorial for residents: topics in CT. Radiation dose in CT. Radiographics. 2002;22:1541–53
Geraghty EM, Boone JM. Determination of height, weight, body mass index, and body surface area with a single abdominal CT image. Radiology. 2003;228:857–63
Calculate your BMI—standard BMI calculator. National Heart, Lung and Blood Institute, http://www.nhlbisupport.com/bmi/
d’Agostino AG, Remy-Jardin M, Khalil C, Delannoy-Deken V, Flohr T, Duhamel A, et al. Low-dose ECG-gated 64-slices helical CT angiography of the chest: Evaluation of image quality in 105 patients. Eur Radiol 2006;16:2137–46
Barrett JF, Keat N. Artifacts in CT: recognition and avoidance. Radiographics. 2004;24:1679–91
Mori S, Endo M, Nishizawa K, Murase K, Fujiwara H, Tanada S. Comparison of patient doses in 256-slice CT and 16-slice CT scanners. Br J Radiol. 2006;79:56–61
Siegel MJ, Schmidt B, Bradley D, Suess C, Hildebolt C. Radiation dose and image quality in pediatric CT: effect of technical factors and phantom size and shape. Radiology. 2004;233:515–22
Tack D, De Maertelaer V, Petit W, Scillia P, Muller P, Suess C, et al. Multi-detector row CT pulmonary angiography: comparison of standard-dose and simulated low-dose techniques. Radiology. 2005;236:318–25
Sun Z. Multislice CT angiography in aortic stent grafting: relationship between image noise and body mass index. Eur J Radiol. 2007;61:534–40
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Funama, Y., Awai, K., Hatemura, M. et al. Automatic tube current modulation technique for multidetector CT: is it effective with a 64-detector CT?. Radiol Phys Technol 1, 33–37 (2008). https://doi.org/10.1007/s12194-007-0005-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-007-0005-y