Abstract
Heat shock proteins (HSPs) play an important role in insulin resistance and improve the cellular stress response via HSP induction by exercise to treat type 2 diabetes. In this study, the effects of exercise-induced HSP72 expression levels on whole-body insulin resistance in type 2 diabetic rats were investigated. Male 25-week-old Otsuka Long-Evans Tokushima Fatty rats were divided into three groups: sedentary (Sed), trained in a thermal-neutral environment (NTr: 25 °C), and trained in a cold environment (CTr: 4 °C). Exercise training was conducted 5 days/week for 10 weeks. Rectal temperature was measured following each bout of exercise. An intraperitoneal glucose tolerance test (IPGTT) was performed after the training sessions. The serum, gastrocnemius muscle, and liver were sampled 48 h after the final exercise session. HSP72 and heat shock cognate protein 73 expression levels were analyzed by Western blot, and serum total cholesterol, triglyceride (TG), and free fatty acid (FFA) levels were measured. NTr animals exhibited significantly higher body temperatures following exercise, whereas, CTr animals did not. Exercise training increased HSP72 levels in the gastrocnemius muscle and liver, whereas, HSP72 expression was significantly lower in the CTr group than that in the NTr group (p < 0.05). Glucose tolerance improved equally in both trained animals; however, insulin levels during the IPGTT were higher in CTr animals than those in NTr animals (p < 0.05). In addition, the TG and FFA levels decreased significantly only in NTr animals compared with those in Sed animals. These results suggest that attenuation of exercise-induced HSP72 expression partially blunts improvement in whole-body insulin resistance and lipid metabolism in type 2 diabetic rats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past several decades, the prevalence of lifestyle diseases, including obesity, hyperlipidemia, and type 2 diabetes, has increased dramatically worldwide. The number of people with diabetes is predicted to rise to 300 million worldwide by 2025 (King et al. 1998), and type 2 diabetes, which is a risk factor for premature mortality and morbidity related to cardiovascular disease, blindness, and kidney and nerve diseases, accounts for 90–95% of diabetes cases. Type 2 diabetes is characterized by whole-body and peripheral tissue (i.e., the skeletal muscle, liver, and adipose tissue) insulin resistance. Therefore, a therapeutic strategy for improving insulin resistance is needed.
Recent studies suggest that heat shock proteins (HSPs) play an important role in insulin resistance (Geiger and Gupte 2011). Accordingly, improving the cellular stress response via HSP induction plays an important role in treating type 2 diabetes (Hooper et al. 2014). HSPs serve as a major endogenous defense system against various stressors and are divided into several groups based on their molecular mass (Locke 1997). Among the numerous HSP isoforms, stress-inducible HSP72 is one of the most promising molecules that can be targeted to reduce insulin resistance. Studies in humans and experimental animal models with type 2 diabetes have found a reduced HSP72 expression in insulin-sensitive tissues. Indeed, Kurucz et al. (2002) demonstrated that reduced skeletal muscle HSP72 gene expression correlated with the degree of insulin resistance in patients with type 2 diabetes. In addition, Chung et al. (2008) revealed that HSP72 protein expression decreased in the skeletal muscle from obese insulin-resistant humans. In contrast, they also revealed that HSP72 overexpression in mouse skeletal muscle prevented a high-fat diet-induced insulin resistance and glucose intolerance (Chung et al. 2008). Moreover, Gupte et al. (2009) showed that increased HSP72 induction by heat treatment (41 °C) protected high-fat diet-fed rats against insulin resistance. Therefore, increasing HSP72 expression by extraneous stimuli may offer a mechanism to improve diabetes.
HSP72 expression increases in various tissues after physical exercise (Atalay et al. 2004; Naito et al. 2001). This increased HSP72 level is caused by many stressors associated with exercise, such as thermal, mechanical, metabolic, and oxidative stresses. In general, the primary factor that stimulates HSP72 induction is elevated cell temperature (Locke et al. 1995). Ogura et al. (2008) let animals exercise in a room at 25 or 4 °C for 60 min and showed that the body temperature during exercise remained the same as that of before exercise (~38.5 °C) at 4 °C, whereas it increased to approximately 40.5 °C at 25 °C. They also reported that suppressing the increase in body temperature during exercise prevents increased HSP72 expression in the liver and skeletal muscle, suggesting that the increase in body temperature is an important factor for exercise-induced HSP72 expression. However, few studies have examined the effects of exercise on improved insulin resistance while considering HSP72 expression; therefore, the role of HSP72 induced by exercise in improving insulin resistance remains unclear. We hypothesized that reducing HSP72 induction during exercise by suppressing the increase in body temperature during exercise would not improve insulin resistance. Herein, we investigated the effects of exercise-induced HSP72 expression levels on whole-body insulin resistance in type 2 diabetic rats.
Methods
Animals and experimental design
All procedures were approved by the Juntendo University Animal Care and Use Committee. Otsuka Long-Evans Tokushima Fatty (OLETF) rats are a well-characterized animal model of human type 2 diabetes. OLETF rats exhibit hyperphagia and obesity beginning early development and develop insulin resistance and type 2 diabetes (Kawano et al. 1992). The animals were obtained from Otsuka Pharmaceutical Co., Ltd. (Tokyo, Japan) and were housed on a 12:12 h light–dark cycle in an environmentally controlled room (23 ± 1 °C and 55 ± 5% relative humidity) and given standard rat chow and water ad libitum. At 25 weeks of age, the OLETF rats were divided into three body-weight-matched groups: sedentary (Sed, n = 9), trained in a thermal-neutral temperature (NTr, n = 9), and trained in a cold temperature (CTr, n = 9).
Training protocol
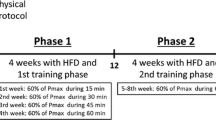
To examine the effects of exercise-induced HSP72 expression levels on whole-body insulin resistance in type 2 diabetic rats, we performed a previously established training protocol by Hamilton et al. (2001) and Ogura et al. (2008). They showed that cold temperature (4 °C) blocks the rise in body temperature during exercise and prevents exercise-induced HSP72 expression in the cardiac and skeletal muscles and in the liver. Animals in the NTr and CTr groups were exercised using a motor-driven animal treadmill (KN-73; Natsume, Tokyo, Japan) 5 days per week for 10 weeks in a climate-controlled room at 25 or 4 °C. Exercise was conducted during the dark (active) period. The first day of training began at a workout intensity of 10–15 m/min without grade for 10 min. The intensity and duration were increased gradually, and 20 m/min was attained for 60 min considering the effects of exercise training. Similar with previous study (Ogura et al. 2008), the training intensity and duration for both exercise groups were the same in the present study. Electric shock was rarely used to motivate the animals to run. Rectal temperature was measured to verify increased body temperature using a calibrated thermistor probe (LT-8; Gram Corp., Saitama, Japan) inserted approximately 6–7 cm past the anal sphincter into the colon before and immediately after each bout of exercise training. The rectal temperatures over the last week of exercise sessions were averaged. The Sed animals were kept sedentary in their living space and were handled in the same manner as the other groups. Additionally, the Sed animals were not allowed to eat during the exercise session to exclude the effects of diet.
Intraperitoneal glucose tolerance test
An intraperitoneal glucose tolerance test (IPGTT) was performed 48 h after the 9-week training period. Overnight-fasted animals were anesthetized with pentobarbital sodium (60 mg/kg) and given a glucose load of 1 g/kg body weight. Blood samples were obtained from a dorsal foot vein 0, 30, 60, and 120 min after injection. The glucose level was determined using a Glutest Neo Super® device (Sanwa Kagaku Kenkyusho Co., Ltd., Aichi, Japan). The blood samples were centrifuged at 3000 rpm for 10 min to obtain serum and stored at −80 °C until insulin analysis. Insulin concentration was measured using a commercially available enzyme-linked immunosorbent (ELISA) assay kit (Morinaga Institute of Biological Science, Inc., Kanagawa, Japan) according to the manufacturer’s instructions. Prior to the training period, IPGTTs were performed to verify the development of type 2 diabetes. All animals were diagnosed with developed diabetes after satisfying the following conditions based on the reference noted: (1) a peak level of blood glucose > 16.8 mM and (2) glucose level > 11.2 mM at 120 min (Kawano et al. 1992).
Sampling
The rats were anesthetized with pentobarbital sodium (60 mg/kg) 48 h after the final exercise session of the 10-week training period. After reaching a surgical plane of anesthesia, blood samples were collected from an abdominal vein. The gastrocnemius muscle, liver, and epididymal fat were removed quickly, weighed, frozen in liquid nitrogen, and stored at −80 °C until Western blot analysis. The blood samples were centrifuged at 3000 rpm for 10 min to obtain serum and stored at −80 °C until triglyceride (TG), free fatty acid (FFA), and total cholesterol (T-Cho) measurements, which were performed at a commercial laboratory (SRL, Tokyo, Japan).
Sodium dodecyl sulfate polyacrylamide gel electrophoresis and immunoblot analyses
Muscle and liver tissues were powdered in liquid nitrogen and homogenized in a 5-fold volume of ice-cold homogenization buffer (20 mM HEPES, pH 7.4, 4 mM EGTA, 0.1 mM EDTA, 10 mM MgCl2, and 0.1% Triton X-100) containing Halt™ protease inhibitor cocktail (Thermo Scientific, Rockford, IL, USA) and PhosSTOP™ (Roche, Penzberg, Germany). The homogenates were centrifuged at 900×g for 5 min at 4 °C. Then, the supernatants were centrifuged at 12,000×g for 15 min at 4 °C. Protein concentrations in the samples were determined using the bicinchoninic acid (BCA) protein assay (Thermo Scientific).
The protein samples were prepared for electrophoresis by adjusting the protein concentration with sample buffer (99% glycerol, 1 M Tris-HCl, pH 6.8, 10% SDS, and β-mercaptoethanol) to 2 μg/μL and boiled for 5 min at 95 °C. An equal amount of protein (10–20 μg) was loaded into each well and separated by sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) at 150 V for 50 min. The proteins were then transferred to polyvinylidene difluoride (PVDF) membranes at 100 V for 1 h. After transfer, the membranes were blocked for 1 h using 5% non-fat skim milk/Tris-buffered saline with Tween-20 (T-TBS) or PVDF-blocking reagent (Toyobo Co. Ltd., Osaka, Japan) and incubated for 1 h at room temperature with the following primary antibodies: HSP72 (SPA-810AP; 1:5000; Stressgen, Victoria, BC, Canada), HSC73 (SPA-815AP; 1:5000; Stressgen), and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (1:10,000, Cell Signaling Technology, Beverly, MA, USA, #8884) in dilution buffer. The membranes were washed in T-TBS and reacted with alkaline phosphatase substrate (Bio-Rad, Hercules, CA, USA) to analyze the expression levels of HSP72 and HSC73. The membranes were incubated with anti-rabbit horseradish peroxidase-conjugated secondary antibody (1:20,000) in 5% non-fat skim milk/T-TBS for 1 h at room temperature and then reacted with ECL™ prime reagents (GE Healthcare, Piscataway, NJ, USA). Signals were recorded using an ATTO light capture system (Tokyo, Japan). GAPDH was used as a loading control to confirm the standardized protein loading and transfer. Analyses were performed using CS analyzer 3.0 software (ATTO).
Statistical analysis
Values are expressed as the mean ± standard error. Changes in body temperature before and immediately after exercise, body weight, and food intake were analyzed using a two-way factorial analysis of variance (ANOVA; group × time) and Bonferroni post hoc tests. Other parameters were analyzed using a one-way ANOVA with Bonferroni’s multiple comparisons test. A p value <0.05 was considered significant. All statistical analyses were performed using Prism software ver. 6.0. (GraphPad Software, La Jolla, CA, USA).
Results
Rectal temperature during exercise
Figure 1 shows the average rectal temperatures of the animals before and immediately after exercise during the final week of exercise sessions. The rectal temperature was significantly higher in NTr animals after exercise (p < 0.05) than that of the basal level (basal 37.97 ± 0.48 °C; after exercise 40.55 ± 0.48 °C) and that of CTr animals (p < 0.05). In contrast, no significant difference in rectal temperature was observed between the basal levels and after exercise in CTr animals (basal 38.26 ± 0.30 °C; after exercise 38.01 ± 0.35 °C).
Changes in rectal temperature in rats trained in ordinary (25 °C; NTr) or cold temperatures (4 °C; CTr). The rectal temperatures over the last week of exercise sessions were averaged. NTr, n = 8 (gray plot); CTr, n = 9 (black plot). Values are mean ± standard error. #p < 0.05 vs. CTr after exercise, §p < 0.05 vs. basal NTr
70-kDa HSP expression levels in the skeletal muscle and liver
To assess the HSP72 induction following exercise, we next analyzed the expression of HSP72 in the skeletal muscle and in the liver (Fig. 2). Although, not only NTr but also CTr animals exhibited higher HSP72 expression levels in both the skeletal muscle and liver than those of Sed animals, and HSP72 levels were significantly lower in CTr animals than those in NTr animals (p < 0.05; Fig. 2b, e). No differences in HSC73 levels in the skeletal muscle or liver were found among the groups (Fig. 2c, f).
Heat shock protein 72 (HSP72) (B, E) and heat shock cognate protein 73 (HSC73) expression levels (C, F) in the gastrocnemius muscle (upper) and liver (lower). GAPDH was used as a loading control. Sedentary (Sed), n = 7 (white bar); NTr (25 °C), n = 7 (gray bar); and CTr (4 °C), n = 8 (black bar). Values are mean ± standard error. *p < 0.05 vs. Sed, #p < 0.05 vs. NTr
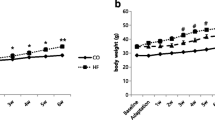
Changes in body weight and food intake during training
The body weights of NTr and CTr animals decreased gradually throughout the training period, and a significant decrease appeared approximately 2 weeks after training began in the NTr and CTr groups compared with that in the Sed group (Fig. 3a). However, no differences were observed between the training conditions.
Food intake by NTr and CTr animals decreased significantly during the early training period compared to that in the Sed group but increased gradually to the level observed in the Sed group. No differences were observed between the training conditions (Fig. 3b).
Glucose tolerance and insulin secretion during the IPGTT
To evaluate whole-body insulin resistance, we performed the IPGTT after the training periods and the glucose and insulin area under curve (AUC) values were calculated using the trapezoidal rule. The glucose AUC values decreased significantly in NTr and CTr animals compared with those in Sed animals; however, no differences were observed among the training conditions (p < 0.05; Fig. 4a). In addition, the insulin AUC decreased significantly in NTr and CTr animals compared with that in Sed animals (p < 0.05); the insulin AUC in CTr animals was significantly higher than that in NTr animals (p < 0.05; Fig. 4b).
The area under the curve (AUC) values for glucose (a) and insulin (b) as determined by the intraperitoneal glucose tolerance test (IPGTT) performed after exercise training. Sed, n = 6 (white bar); NTr (25 °C), n = 6 (gray bar); and CTr (4 °C), n = 6 (black bar). Values represent the mean ± standard error. *p < 0.05 vs. Sed, #p < 0.05 vs. NTr
Epididymal fat weight and serum lipid profile
Relative epididymal fat weight decreased significantly in NTr animals compared with that in Sed animals (p < 0.05; Fig. 5a). The serum TG and FFA levels also decreased significantly in NTr animals compared with those in Sed animals (p < 0.05; Fig. 5b, c). The T-Cho levels decreased significantly in NTr and CTr animals compared with those in Sed animals (p < 0.05; Fig. 5d).
The epididymal fat weight (a), serum triglyceride (TG) (b), free fatty acid (FFA) (c), and total cholesterol (T-Cho) (d) levels after exercise training. Sed, n = 6 (white bar); NTr (25 °C), n = 6 (gray bar); and CTr (4 °C), n = 6 (black bar). Values represent the mean ± standard error. *p < 0.05 vs. Sed, #p < 0.05 vs. NTr
Discussion
In the present study, we report the first evidence demonstrating that attenuation of exercise-induced HSP72 expression in the skeletal muscle and liver partially blunts the improvement in whole-body insulin resistance and lipid metabolism in type 2 diabetic rats. We suggest that higher expression of exercise-induced HSP72 may be necessary to obtain sufficiently the beneficial effects of exercise on whole-body glucose insulin resistance and lipid metabolism.
It has been reported that exercise protects against or ameliorates insulin resistance; however, few studies have examined the effects of exercise on improved insulin resistance while considering HSP72 expression. We used a previously reported exercise protocol (Hamilton et al. 2001; Ogura et al. 2008) to examine the effects of attenuated exercise-induced HSP72 expression on whole-body insulin resistance. In agreement with these previous studies, the increase in body temperature by exercise was completely blocked in a cold environment. Conversely, exercise training in both environments increased HSP72 levels; i.e., HSP72 expression was not suppressed completely in a cold environment, although exercise-induced HSP72 expression in a cold environment was lower than that in a thermal-neutral environment. It is likely that the increase in exercise-induced HSP72 levels in a cold environment was due to other stressors associated with exercise, such as prolonged mechanical and metabolic stresses, excluding thermal stress (Skidmore et al. 1995). HSP72 is a potential therapeutic target for type 2 diabetes (Hooper and Hooper 2009; Soti et al. 2005). Inducing HSP72 expression either genetically or pharmacologically can prevent insulin resistance in the skeletal muscle in the context of genetic obesity or high-fat feeding (Chung et al. 2008; Henstridge et al. 2014). In addition, Gupte et al. (2009) reported that heat treatment induced HSP72 expression in the skeletal muscle and improved insulin resistance in rats fed a high-fat diet. In the present study, the insulin AUC during IPGTT was higher in animals trained in a cold environment than in those trained in a thermal-neutral environment, thus blunting the improvement in whole-body insulin resistance by exercise in a cold environment. Our results suggest that the difference in exercise-induced HSP72 expression levels between training conditions may contribute to improve whole-body insulin resistance. Since the precise mechanism by which HSP72 affects insulin resistance remains to be elucidated, further studies are needed to examine the underlying mechanisms by which exercise-induced HSP72 contributes to improve insulin resistance.
Interestingly, exercise markedly induced HSP72 expression in the liver as well as in skeletal muscle in a thermal-neutral environment. Conversely, exercise without an increase in body temperature partially attenuated HSP72 induction, and may result in blunted improvement in insulin resistance. To date, the beneficial effects of exercise on improved insulin resistance have been mostly examined in the skeletal muscle, not in the liver. However, the liver is a key organ for whole-body blood glucose and lipid homeostasis. As hepatic insulin resistance plays a crucial role in hyperglycemia, the liver is an important therapeutic target organ. Previous studies reported that pharmacological up-regulation of hepatic HSP72 expression is associated with improved insulin resistance and glucose homeostasis in high-fat-fed mice (Adachi et al. 2010; Zeng et al. 2015). Therefore, inducing HSP72 in the liver also likely contributes to improve insulin resistance similar to that observed in the skeletal muscle.
We also found that exercise training improved serum TG and FFA levels; these beneficial effects were blunted in animals trained in a cold environment. The increase in circulating TG and FFA, as well as the accumulation of intramuscular and intrahepatic TG and FFA, is associated with whole-body and peripheral insulin resistance (Boden 1997; Bonen et al. 2004). Thus, decreasing these lipid parameters may improve insulin resistance. In this regard, inducing HSP72 is also likely to be important for improving lipid metabolism. Whole-body energy utilization and fatty acid oxidation were increased in mice overexpressing HSP72 in the skeletal muscle, thereby preventing intramuscular lipid accumulation (Henstridge et al. 2014). On the other hand, fatty acid oxidation decreased in the muscle of HSP72 knock-out mice, resulting in intramuscular accumulation of diacylglycerol and triacylglycerol (Drew et al. 2014). Although we did not measure the intramuscular and intrahepatic lipid accumulation, it is believed that attenuation of exercise-induced HSP72 in animals trained in a cold environment likely reduces lipid accumulation, thereby blunting the beneficial effects of exercise on whole-body insulin resistance. Additionally, Gupte et al. (2009) reported that heat treatment (41 °C) increased fatty acid oxidation and mitochondrial oxygen consumption. Moreover, Liu and Brooks (2011) reported that heat stress (41 °C) induced mitochondrial biogenesis via the AMP-activated protein kinase-sirtuin 1-peroxisome proliferator-activated receptor gamma coactivator-1α pathway in C2C12 myotubes. These previous studies suggest that increasing tissue temperature may improve lipid metabolism. Therefore, the increase in tissue/body temperature that occurs during exercise and the increased expression of exercise-induced HSP72 are important factors in realizing the beneficial effect of exercise on lipid metabolism.
In summary, we demonstrated that attenuation of exercise-induced HSP72 expression in the skeletal muscle and liver partially blunted the improvement in whole-body insulin resistance and lipid metabolism. Although further studies are required to clarify the mechanism (s) underlying by which exercise-induced HSP72 expression contributes to improve insulin resistance and lipid metabolism, sufficient HSP72 induction contributes to propose an effective exercise program for individuals with type 2 diabetes.
References
Adachi H et al (2010) An acylic polyisoprenoid derivative, geranylgeranylacetone protects against visceral adiposity and insulin resistance in high-fat-fed mice. Am J Phys Endocrinol Metab 299:E764–E771. doi:10.1152/ajpendo.00075.2010
Atalay M et al (2004) Exercise training modulates heat shock protein response in diabetic rats. J Appl Physiol 97:605–611. doi:10.1152/japplphysiol.01183.2003
Boden G (1997) Role of fatty acids in the pathogenesis of insulin resistance and NIDDM. Diabetes 46:3–10
Bonen A, Parolin ML, Steinberg GR, Calles-Escandon J, Tandon NN, Glatz JF, Luiken JJ, Heigenhauser GJ, Dyck DJ (2004) Triacylglycerol accumulation in human obesity and type 2 diabetes is associated with increased rates of skeletal muscle fatty acid transport and increased sarcolemmal FAT/CD36. FASEB J 18(10):1144–1146. doi:10.1096/fj.03-1065fje
Chung J et al. (2008) HSP72 protects against obesity-induced insulin resistance Proceedings of the National Academy of Sciences of the United States of America 105:1739–1744 doi:10.1073/pnas.0705799105
Drew BG et al (2014) HSP72 is a mitochondrial stress sensor critical for Parkin action, oxidative metabolism, and insulin sensitivity in skeletal muscle. Diabetes 63:1488–1505. doi:10.2337/db13-0665
Geiger PC, Gupte AA (2011) Heat shock proteins are important mediators of skeletal muscle insulin sensitivity. Exerc Sport Sci Rev 39:34–42. doi:10.1097/JES.0b013e318201f236
Gupte AA, Bomhoff GL, Swerdlow RH, Geiger PC (2009) Heat treatment improves glucose tolerance and prevents skeletal muscle insulin resistance in rats fed a high-fat diet. Diabetes 58:567–578. doi:10.2337/db08-1070
Hamilton KL, Powers SK, Sugiura T, Kim S, Lennon S, Tumer N, Mehta JL (2001) Short-term exercise training can improve myocardial tolerance to I/R without elevation in heat shock proteins. Am J Physiol Heart Circ Physiol 281:H1346–H1352
Henstridge DC et al (2014) Activating HSP72 in rodent skeletal muscle increases mitochondrial number and oxidative capacity and decreases insulin resistance. Diabetes 63:1881–1894. doi:10.2337/db13-0967
Hooper PL, Balogh G, Rivas E (2014) The importance of the cellular stress response in the pathogenesis and treatment of type 2 diabetes. Cell Stress Chaperones 19(4):447–464. doi:10.1007/s12192-014-0493-8
Hooper PL, Hooper PL (2009) Inflammation, heat shock proteins, and type 2 diabetes. Cell Stress Chaperones 14:113–115. doi:10.1007/s12192-008-0073-x
Kawano K, Hirashima T, Mori S, Saitoh Y, Kurosumi M, Natori T (1992) Spontaneous long-term hyperglycemic rat with diabetic complications: Otsuka Long-Evans Tokushima Fatty (OLETF) strain. Diabetes 41:1422–1428
King H, Aubert RE, Herman WH (1998) Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care 21:1414–1431
Kurucz I, Morva A, Vaag A, Eriksson KF, Huang X, Groop L, Koranyi L (2002) Decreased expression of heat shock protein 72 in skeletal muscle of patients with type 2 diabetes correlates with insulin resistance. Diabetes 51:1102–1109
Liu CT, Brooks GA (2011) Mild heat stress induces mitochondrial biogenesis in C2C12 myotubes. J Appl Physiol. doi:10.1152/japplphysiol.00989.2011
Locke M (1997) The cellular stress response to exercise: role of stress proteins. Exerc Sport Sci Rev 25:105–136
Locke M, Noble EG, Tanguay RM, Feild MR, Ianuzzo SE, Ianuzzo CD (1995) Activation of heat-shock transcription factor in rat heart after heat shock and exercise. Am J Phys 268:C1387–C1394
Naito H, Powers SK, Demirel HA, Aoki J (2001) Exercise training increases heat shock protein in skeletal muscles of old rats. Med Sci Sports Exerc 33:729–734
Ogura Y et al (2008) Elevation of body temperature is an essential factor for exercise-increased extracellular heat shock protein 72 level in rat plasma. American journal of physiology Regulatory, integrative and comparative physiology 294:R1600–R1607. doi:10.1152/ajpregu.00581.2007
Skidmore R, Guitierrez JA, Guerriero V, Kregel KC (1995) HSP70 induction during exercise and heat stress in rats: role of internal temperature. Am J Phys 268:R92–R97
Soti C, Nagy E, Giricz Z, Vigh L, Csermely P, Ferdinandy P (2005) Heat shock proteins as emerging therapeutic targets. Br J Pharmacol 146:769–780. doi:10.1038/sj.bjp.0706396
Zeng XY et al (2015) Identification of matrine as a promising novel drug for hepatic steatosis and glucose intolerance with HSP72 as an upstream target. Br J Pharmacol 172:4303–4318. doi:10.1111/bph.13209
Acknowledgements
This study was supported in part by the MEXT-supported program for Juntendo University and a grant-in-aid for JSPS fellows (13J10819, to T.T.). The Juntendo University Institute of Health and Sports Science & Medicine also supported this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Statement
All procedures were approved by the Juntendo University Animal Care and Use Committee (H24-01).
Rights and permissions
About this article
Cite this article
Tsuzuki, T., Kobayashi, H., Yoshihara, T. et al. Attenuation of exercise-induced heat shock protein 72 expression blunts improvements in whole-body insulin resistance in rats with type 2 diabetes. Cell Stress and Chaperones 22, 263–269 (2017). https://doi.org/10.1007/s12192-017-0767-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12192-017-0767-z