Abstract
This study examined physicians’ motivation to engage in work-related learning and its contribution to expertise development beyond work experience. Based on deliberate practice theory, semi-structured interviews were conducted with 17 residents and 28 experienced physicians in internal medicine, focusing on the activities they engaged in during work that might contribute to professional development and the goals underlying this behavior. Learning motivation was also measured using a goal orientation questionnaire. Expertise was measured by a case test derived from the Medical Knowledge Self Assessment Program (MKSAP). The interviews showed that participants’ learning was largely embedded in everyday work; most of their learning activities were inherent to the job rather than motivated by competence improvement goals. The problems encountered in patient care played a key role in prompting learning. Role, work experience and work situation affected the type of activities engaged in, as well as the intensity of practice. Deliberate engagement in work-related learning activities was related neither to goal orientations nor to case test performance, except activities by the experienced physicians to keep up-to-date. Work experience, in contrast, showed a clear positive relationship with the performance of residents. Two main conclusions can be drawn from this study: (1) patient care induced relevant learning activities aimed at performance improvement for the patient’s sake; (2) deliberate investments in learning can be enhanced to promote expertise development. Self-regulated learning by physicians needs to be strengthened and the organization for which they work should facilitate and encourage learning in daily practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Expertise in medicine is based on a large and well-organized knowledge base that is largely developed by learning from experience. Theories on the development of expertise in medicine usually emphasize implicit learning from patients encountered, which implies that knowledge becomes tuned to its practical use (Norman et al. 2006; Schmidt and Rikers 2007; Schmidt et al. 1990). This implies that in routine situations, the right knowledge is automatically activated at the right time through pattern recognition processes (Stolper et al. 2010; Van de Wiel et al. 2000). While research in this domain has focused on knowledge representations that enable this fast and accurate diagnostic reasoning, less attention has been given to the activities undertaken by physicians to learn from their experiences. The theory of deliberate practice (Ericsson 2004, 2006, 2009) has addressed this aspect by arguing that mere practice is not enough to achieve expertise, but that focused efforts are needed. The motivation to improve performance is vital, as it makes one deliberately seek activities and feedback that may help reach this goal. Monitoring performance is regarded as crucial to control automatic behavior and to further refine the knowledge base by reflection, as well as by practicing performance aspects that need improvement. This implies that developing expertise requires physicians to be self-regulated learners who plan, monitor and reflect on their thoughts and actions to learn and improve (Van de Wiel et al. 2004; Zimmerman 2000, 2006). The focus on competence improvement and the deliberate engagement in learning from work experience are considered essential for lifelong learning in the medical profession (Guest et al. 2001). Thus, learning-by-intention must complement learning-by-doing. The present study investigated physicians’ motivation to engage in work-related learning and its contribution to expertise development beyond work experience. We compared two groups with different roles and work experience: residents and experienced physicians.
Motivation for Work-Related Learning
In a review of work motivation, Latham and Pinder (2005) defined the concept as “a set of energetic forces that originate both within as well as beyond an individual’s being, to initiate work-related behavior and to determine its form, direction, intensity, and duration” (p. 486). They described motivation as a psychological process resulting from the interaction between the individual and the environment and discussed a multitude of concepts and theories that are part of the motivational literature. Other reviews of motivation also show the multidimensionality of the concept (Murphy and Alexander 2000; Zimmerman and Schunk 2008). For the purpose of the present study, we focused on self-regulated learning processes, in particular the activities undertaken to learn from and for medical practice, and the goals underlying this behavior.
Self-regulation refers to self-generated thoughts, feelings and actions that are strategically planned and adapted to the attainment of personal goals (Zimmerman 2000, 2006). The process involves three interrelated phases, that occur before, during and after task performance, and relates to domain and personal knowledge. The forethought phase involves setting goals and planning strategies. These may be adjusted in the performance phase, based on careful monitoring of task progress, the self and the context, for example by seeking help where this is necessary to accomplish a task. The reflection phase involves evaluating and reflecting upon the outcomes to generate useful information for subsequent performance. When the explicit goal is to learn from task performance, learning is proactively planned and not merely reactively generated or implicitly gained from practice or experience (Pintrich 2000). Goal-directed learning behavior depends on the interaction between goal orientations and goal setting in the forethought phase. Whereas goal orientations are regarded as relatively stable trait-like goal and outcome preferences in education or training situations (Day et al. 2003; Payne et al. 2007; Seijts et al. 2004; Tuominen-Soini et al. 2010),Footnote 1 goal setting refers to the specific goals that guide effort and persistence in task performance (Seijts et al. 2004; Locke and Latham 2002).
Three main goal orientations have been distinguished, each with different effects on learning and performance in education and training (Brett and VandeWalle 1999; Payne et al. 2007; Pintrich 2000). “Mastery goal orientation” refers to the motivation to master a topic and to improve one’s skills and understanding. “Performance approach goal orientation” describes the tendency to prove and compare competence to others. And “performance avoidance goal orientation” describes the tendency to avoid failure and unfavorable judgments. Mastery goal orientations have generally been shown to be positively related to self-regulated learning and performance, whereas performance avoidance orientations have been shown to be negatively related to these variables (Ford et al. 1998; Payne et al. 2007; Pintrich 2000). Individuals with a mastery goal orientation believe that their ability will be improved by putting in effort, setting challenging but attainable goals, seeking opportunities for practice and feedback, searching for effective strategies, monitoring and evaluating their progress and goal achievement, persisting when facing setbacks, and having adaptive attribution patterns associated with positive feelings and high self-efficacy (Ames 1992; Pintrich 2000; Zimmerman 1998).
Goal setting theory has shown that a specific challenging goal leads to better task performance than a vague goal, such as “do your best” (Locke and Latham 2002). In complex tasks, learning goals specifically focusing on the acquisition of knowledge and skills were found to be more beneficial than goals aimed at reaching a certain performance level, irrespective of goal orientations (Locke and Latham 2006; Seijts et al. 2004). On the other hand, when a vague goal was set, goal orientations predicted performance, with mastery goal orientation resulting in better performance (Seijts et al. 2004). Research on self-set goals in a complex task showed that these goals mediated the relationship between goal orientations and performance, and that only skill improvement goals correlated positively with performance (Brett and VandeWalle 1999). Both for mastery goal orientation and specific learning goals, the relationship with performance is mediated by relevant learning activities (Ford et al. 1998; Seijts et al. 2004; Zimmerman 2008).
Limited research is available on the effect of goal orientations on professional learning in the workplace, except for research into feedback-seeking behavior (Ashford et al. 2003). However, studies on feedback-seeking have predominantly focused on the frequency of this behavior, rather than on the diagnostic and informative value of feedback to foster competence improvement (Janssen and Prins 2007; VandeWalle 2003). In medicine, Teunissen et al. (2009) studied feedback-seeking behavior among obstetrics and gynecology residents during night shifts and found that a mastery goal orientation was positively related to perceived feedback benefits, which were, in turn, related to an increased frequency of feedback seeking. Performance goal orientation was associated with higher perceived image costs of feedback seeking. Janssen and Prins (2007) investigated the relations between goal orientations and the type of information sought by residents. They found that both mastery and performance-avoidance goal orientations were positively related to seeking self-improvement information. This finding had not been hypothesized and suggests that the instrumental value of feedback to improve performance also applies to people with a performance-avoidance orientation.
A focus on performance improvement and continuous development is required for high-quality performance in medicine, as physicians need to incorporate previous experiences and recent developments in their field to ensure effective patient care. The tasks of physicians in medical practice are complex and require continuous updating of knowledge and skills. Mastery goal orientation and specific learning goals are therefore likely to contribute to high levels of performance. In medicine, these motivational issues were most clearly addressed by Regehr and colleagues (Guest et al. 2001; Mylopoulos and Regehr 2007). In line with deliberate practice theory (Ericsson 2004, 2006, 2009), they argued that acquiring expertise in medicine not only requires an extensive knowledge base, but also a repertoire of behaviors to build knowledge intentionally, and a work approach in which learning from experience is regarded as an ongoing process that needs investment. This would prevent experienced physicians from just routinely applying the knowledge they have accumulated over time, and foster the critical examination of diagnoses, treatments and work practices to improve future performance. Residents, who are trained on the job, need to adopt such an approach to build their professional expertise.
In the professional learning literature, such an approach echoes with Schön’s plea for reflective practitioners (1983). In his typology of non-formal learning, Eraut (2000) pointed to the level of intention to learn as a fundamental factor. On the one hand, there is implicit learning, in which there is no intention to learn and no awareness of the learning process. On the other hand, learning can be deliberative: it is planned and time is specifically set aside for it. A category in between these two types of learning has been described as reactive, meaning that learning takes place in response to specific situations and events that draw one’s attention. This near-spontaneous and unplanned learning can vary in its degree of intentionality.
Previous research on workplace learning in medicine has shown that physicians’ learning is highly dependent on the patients they encounter and the clinical actions they need to undertake (Hoffman and Donaldson 2004; Sargeant et al. 2006; Slotnick 1999; Teunissen et al. 2007). This implies that much of the learning in medical practice is implicit, involving unconscious changes in knowledge based on the clinical cases seen, and that physicians’ learning behavior is usually reactive, i.e. triggered by being confronted with complex patient problems for which they do not have a ready solution (Duffy 2008; Guest et al. 2001; Hoffman and Donaldson 2004; Slotnick 1996, 1999). Two studies also found that gaps experienced in knowledge and skills may trigger goal-setting and planning of learning activities (Sargeant et al. 2006; Slotnick 1999). However, none of these studies specifically addressed physicians’ deliberate engagement in work-related learning activities to improve their performance, nor its relation to the more general goal orientations.
Contribution of Work Experience and Deliberate Practice to Expertise
The role of experience in expertise development has been a basic assumption in studies using the expert-novice paradigm. In these studies, the performance of experienced and/or excellent performers in the domain is compared with the performance of novices and persons with intermediate levels of training for representative tasks. In a wide range of domains, such as chess, physics, medicine and management, experts have distinguished themselves from novices and intermediates by their quick understanding of the problem presented and the quality of their solutions (Arts et al. 2006; Chi et al. 1981; de Groot 1978; Gobet and Charness 2006; Norman et al. 2006; Schmidt and Boshuizen 1993). The experts’ superior performance has been shown to be rooted in the rich and well-organized knowledge they acquired in the course of their career. Their knowledge base allows experts to be efficient in routine situations through automatic processes, and to be flexible and adaptive in more complex situations when they need to consciously think about possible solutions and actions (Elstein and Schwarz 2002; Stolper et al. 2010). According to the “ten-year rule”, at least 10 years of study and practice in a domain are required to achieve expertise (Simon and Chase 1973; Ericsson et al. 1993). Obviously, it is not only the time invested in practice that matters in reaching expert levels of performance, but also the type and quality of the activities engaged in. This has been emphasized by the theory of deliberate practice and supported by empirical results (Ericsson et al. 1993). Expertise is defined as reproducible superior performance on representative tasks. In this expert performance approach, expertise must be measured by presenting standardized situations that capture the essence of superior performance in a domain (Ericsson 2004, 2006, 2009; Ericsson et al. 2007; Ericsson and Smith 1991).
Deliberate practice is the effortful and regular engagement in training activities designed to remediate weak aspects of performance with the aim to improve competence (Ericsson et al. 1993). Research has shown that the more time is spent on deliberate practice, the better the performance. For example, the activity that best predicted expertise in music and chess was the accumulated and current amount of individual practice (Charness et al. 2005; Ericsson et al. 1993). Similar results were found for academic performance: study time only predicted grade point average across college students when previous performance and the quality of study, in particular studying alone in a quiet environment, were taken into account (Plant et al. 2005). In a work context, Sonnentag and Kleine (2000) found that the activities of preparation, mental simulation, asking for feedback, consulting colleagues and concluding and assessing afterwards could most often be interpreted as deliberate practice, as they were regularly carried out with the aim of improving competence. Insurance agents who deliberately spent more of their current time on these activities performed better in terms of sales and the acquisition of new clients. As regards their work experience, it was only the number of cases handled per day that predicted professional performance and not the number of years of experience in the field. So, these studies suggest that the amount of relevant experience, together with activities focusing on competence improvement, determine performance outcomes.
The literature from the field of work and organizational science also regards the specific nature of experience and the way outcomes are measured as important in describing the effects of experience on work performance (Quinones et al. 1995; Tesluk and Jacobs 1998). However, the majority of studies investigated the relationships between the number of years of job experience and measures of general job performance (Quinones et al. 1995). Meta-analyses of this research showed positive correlations between job experience and job performance, with values of r = .32 (McDaniel et al. 1988) and r = .27 (Quinones et al. 1995). Just as in the literature on expertise, the explanation given is that experience enables relevant job knowledge to be acquired (Schmidt et al. 1986). The effects of experience are most pronounced in the early years of a career, as, relatively speaking, more knowledge is gained than in later years (Schmidt et al. 1986). This corresponds to Ericsson’s (2004, 2006, 2009) proposition that without deliberate practice, most professionals increase their performance to an acceptable level in the initial phases of supervised practice and then maintain this level for the rest of their career. However, further research found that there were moderating effects of job complexity and outcome measures. In low complexity jobs, the relationship between work experience and job performance was especially strong during the first years (McDaniel et al. 1988), while in high complexity jobs this relationship became stronger with experience (Sturman 2003). The relationship between work experience and job performance was also stronger when measures of performance were used that were more representative (i.e., work samples) or more objective (i.e., productivity) than overall performance ratings by supervisors (Quinones et al. 1995; Sturman 2003). This stresses the importance of using representative domain tasks to measure expertise (Ericsson 2004, 2006, 2009; Ericsson et al. 2007; Ericsson and Smith 1991).
In medicine, research into the effects of experience on performance has shown mixed results. Results of studies using the expert-novice paradigm, in which students are compared with practicing physicians, show positive effects of experience on clinical reasoning (e.g., Harteis et al. 2012; Norman et al. 2006; Schmidt and Boshuizen 1993; Van de Wiel et al. 2000). However, the relationship between experience and performance becomes more equivocal when studies involve only practicing physicians, and also depends on the type of tasks and outcome measures used. While physician-review programs using knowledge tests have consistently revealed negative correlations between performance and age (Eva 2002), other studies showed that more experienced physicians generated more accurate diagnoses in early stages of a patient encounter (Eva et al. 2010) and on the basis of only brief information on the complaints and context (Hobus et al. 1987). In complex cases, experienced physicians were better able than residents to utilize their knowledge to analyze and diagnose patients’ problems (Lesgold et al. 1988; Norman et al. 1994). A recent review on the relationship between clinical experience and quality of health care, however, reported mostly decreasing performance with increasing years of practice, as assessed by up-to-date knowledge tests, adherence to practice guidelines, and mortality rates (Choudrey et al. 2005). This review was criticized, however, regarding the relevance of the outcome measures used and the weak evidence for the only real healthcare measure, that of mortality (Norman and Eva 2005; Samuels and Ropper 2005). Therefore, Norman and Eva (2005) wondered whether more experienced physicians would gain certain benefits from practical experience that would make up for their failure to keep up with new developments, as shown by their poorer performance on knowledge tests. The question that remains is how work experience, the effort to learn from these experiences, and the effort to keep up with the medical literature contribute to performance on representative tasks in medicine.
Research Questions
The present study investigated the following two research questions:
-
1)
How motivated are residents and experienced physicians to practice work-related learning, in terms of goal orientations and in terms of their deliberate engagement in work-related learning activities?
We also compared experienced physicians with residents, who are being trained in the workplace to become specialists. We expected that they would value learning activities differently because they are in different phases of their expertise development.
-
2)
What contributions do the motivation for work-related learning and one’s experience make to expertise?
We expected that mastery goal orientation, through its focus on competence improvement, would lead to deliberate engagement in relevant learning activities, and that the latter, together with work experience, would result in higher levels of expertise.
Method
Participants
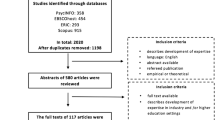
The participants were 45 Dutch physicians working in the field of internal medicine, including 17 residents and 28 experienced specialists in general internal medicine (12 working at a non-university hospital and 16 at a university medical center). Residents attended a 6-year training program in which they practiced internal medicine under supervision and usually specialized further in their final year. Most of the experienced physicians practiced general internal medicine as well as a particular subspecialty, such as clinical pharmacology, endocrinology, geriatrics, hematology, oncology, intensive care, nephrology, rheumatology or vascular medicine. To ensure a clear difference in work experience, we only included residents with a maximum of 7 years of experience, and specialists with at least 10 years of experience in the field of internal medicine. Other indicators of work experience we used were the number of working hours per week, and the number of patients seen per week. Descriptive information on gender distribution, age and the three work experience variables is provided for each group in Table 1 in the results section.
Materials
We conducted semi-structured interviews which focused on the activities that participants engaged in during work and that might contribute to professional development. This method allowed us to examine individual practices in detail, while ensuring comparable data (Emans 2004). The questions were developed based on the theories of deliberate practice (Ericsson 2004, 2006) and self-regulated learning (Zimmerman 2000, 2006), building upon previous studies in work contexts (Sonnentag and Kleine 2000; Van de Wiel et al. 2004), and applied to medical practice in hospitals (Van de Wiel et al. 2011a).
The interview started with questions about work experience, weekly work-related activities, and the goals participants aspired to in their work. It further covered the kind of diagnostic and treatment problems they encountered and how they dealt with them, the situations in which they asked for advice, the extent to which they felt comfortable in doing so, how they handled differences of opinion, and how they were involved in explaining things to others. Subsequently, it focused on receiving, searching for and utilizing feedback, and on the way they evaluated the quality of their decisions and actions. Finally, they were asked what activities they thought contributed most to professional development, including continuing medical education and participation in research. Participants were prompted to reveal the goals underlying their involvement in the activities. For example, in investigating their advice-seeking behaviors and attitudes, we subsequently asked in what situations they asked for advice, how often they did so, why they asked for advice (i.e. “For what purpose do you ask for advice?”) and what considerations played a role in the decision to ask specific colleagues.
The goal orientation questionnaire consisted of 16 items that were rated on a 7-point Likert scale ranging from “strongly disagree” to “strongly agree”. Mastery goal orientation was measured by 8 items validated by Button et al. (1996) for an organizational setting (e.g. “The opportunity to learn new things is important to me”). Items measuring performance-approach goal orientation (e.g. “I try to figure out what it takes to prove my ability to others at work”) and performance-avoidance goal orientation (e.g. “I prefer to avoid situations at work where I might perform poorly”) were taken from VandeWalle (1997) who validated these scales for the work domain. The items were translated into Dutch and presented within the context of participants’ professional development. Cronbach’s alphas were .63, .76, and .79 for the mastery, performance-approach and performance-avoidance goal orientations, respectively.
The case test was developed to measure medical expertise and consisted of 26 items of the Medical Knowledge Self Assessment Program (MKSAP) 2004–2005 (American College of Physicians 2004). The MKSAP is specifically designed to test whether the participant has kept up-to-date with current practice in internal medicine. It requires applying diagnostic and therapeutic knowledge to short case descriptions, and as such can be regarded as a highly representative task in the medical domain. We selected 30 case descriptions, each with a multiple-choice question asking for diagnosis or treatment, in consultation with two internal medicine specialists. After item analysis and review by several internal medicine specialists, four cases were eventually discarded, three cases because they did not correspond to Dutch guidelines and one case because all participants answered it correctly. The 26 remaining cases were divided over the following subspecializations: cardiovascular medicine (3), nephrology and hypertension (3), hematology and oncology (4), infectious disease medicine (2), endocrinology and metabolism (3), gastroenterology and hepatology (4), pulmonary medicine and critical care (2), neurology (2), and rheumatology (3). Performance on the case test was determined by the number of correct answers.
Procedure
Internal medicine physicians in several hospitals in the south of the Netherlands were first approached by the head of the Department of Internal Medicine at Maastricht University Medical Centre and subsequently contacted by the interviewers. The final response rates were 51 %, 20 % and 58 % for the residents (2 hospitals), physicians working at non-university hospitals (6 hospitals) and physicians working at university hospitals (3 hospitals), respectively. The main reason for not participating was being too busy.
Participants were informed that the study was about professional development and would take about 1.5 hours. The interviews and questionnaires were administered individually at the physicians’ offices. In accordance with the Declaration of Helsinki, participants signed an informed consent form and data were treated anonymously.
Analysis
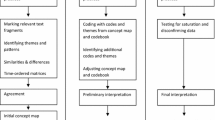
The interviews were transcribed verbatim. Analysis proceeded in two steps. In the first step, we used content analysis to categorize and describe participants’ answers in terms of themes and subthemes, based on the questions asked in the interviews (Van de Wiel et al. 2011a). In the second step, we analyzed, for each of the main themes identified whether the participants’ behavior and attitudes showed elements that were characteristic of deliberate practice. An overview of these themes is presented in Table 2. Most of the themes were directly related to the interview questions, but two themes were rephrased for the purpose of the present analysis. The first was “reflection on diagnoses and treatment”, which is required to learn from previous decisions and their consequences. This theme pervaded the entire interview and was not reported only in answering the question on evaluating the quality of decisions and actions. The second was “planning learning activities”, which referred to the intention to engage in future learning activities and was particularly triggered by questions about the goals underlying professional development activities.
In an iterative process, three raters (CB, PVdB, MvdW) scored a subset of the interviews until they could reliably distinguish three levels of deliberate practice: (0) not engaged in learning activity, (1) learning activities inherent to the job because a practical problem has to be solved, the job has to be done, or requirements for continuing medical education must be fulfilled, and (2) engaged in deliberate practice as indicated by showing greater motivation and effort for learning to improve competence. These levels were defined for each of the themes distinguished throughout the interviews. For example, with regard to the theme of “difference of opinion”, the following scoring options were used: (0) Differences of opinion do not induce the person to take any action and the person stands by his/her own opinion (scored as not engaged in learning activity); (1) When having a difference of opinion, the person is open to arguments from the other party but will not initiate further study about the topic of disagreement (scored as learning activities inherent to the job); (2) When having a difference of opinion, the person is open to arguments from the other party, regarding these as a starting point for efforts to gain more in-depth knowledge on a topic that can be used in the future (scored as engaged in deliberate practice).
One rater (CB) then scored the remainder of the interviews, consulting the other raters in case of doubt. The sum of deliberate practice was computed for each participant by adding up the deliberate practice scores for each main theme. This sum score was used to indicate the overall level of deliberate practice participants engaged in. In addition, we assessed how often participants asked for advice, on a 6-point scale from less than once a month to daily.
Results
Work Experience
The different groups in our sample differed significantly in terms of different aspects of work experience. Table 1 shows that the residents obviously had less work experience than the experienced physicians (F (2, 42) = 33.69, MSE = 36.35, p = .00), that working hours did not differ between groups (F (2, 42) = .93, MSE = 78.31, p = .40), but that experienced physicians working in non-university hospitals saw far more patients than the other two groups (F (2, 42) = 29.45, MSE = 463.34, p = .00). This difference was due to the fact that this group spent more time in the outpatient clinic than the other two groups.
Goal Orientations
The means and standard deviations of participants’ goal orientations are provided in Table 1. All participants showed a high mastery goal orientation, significantly above the midpoint of the scale, t(44) = 20.79, p = .000, whereas their performance-approach goal orientation was just below the midpoint of the scale, t(44) = -2.55, p = .014, and their performance-avoidance goal orientation was far below the midpoint of the scale, t(44) = -11.36, p = .000. There were no significant differences between the three groups in terms of any of the three goal orientations.
Deliberate Practice Level of Learning Behaviors and Attitudes
Table 2 shows the extent to which the residents and experienced physicians were deliberately engaged in work-related learning activities. The results indicate that the participants mostly engaged in such activities because they were inherent to the job of providing high-quality patient care, rather than because they were motivated by competence improvement goals. This was especially true with regard to asking for advice and feedback, dealing with differences of opinion and teaching and explaining. Remarkably, almost half of the participants did not show any sign of reflecting on the way they diagnosed or treated patients. Their motivation to learn was rather prompted by specific problems that needed to be solved. These problems then led to literature search and asking for advice. Overall, the level of deliberate practice was not high, with a mean sum score of 11.36 on a scale of 0–20 (Table 1). Although individual participants differed greatly in their deliberate practice levels (range 7–18), there were no differences between the three groups of physicians.
The groups did differ, however, regarding some specific learning behaviors and attitudes. Comparisons of the three groups using the Kruskall-Wallis test showed significant (or nearly significant) differences regarding the goals they aspired to in their work (H (2) = 9.92, p = .007), teaching and explaining (H (2) = 5.96, p = .051), and contributing to knowledge development (H (2) = 7.28, p = .026). Mann–Whitney tests revealed that these were all due to differences between the residents and the experienced physicians: the residents mentioned more explicit learning goals than the experienced physicians (U = 126.50, z = -3.15, p = .002), while the experienced physicians indicated more engagement in deliberate practice for teaching and explaining (U = 158.50, z = -2.43, p = .015) and for contributions to knowledge development (U = 134.00, z = -2.62, p = .009). Moreover, the experienced physicians expressed more motivation to keep up-to-date than the residents (U = 160.50, z = -2.00, p = .046): half of the experienced physicians engaged in activities to improve their competence, such as reading relevant literature in the evenings and attending non-mandatory lectures. The residents, on the other hand, reported asking for advice more often than the experienced physicians (U = 66.00, z = -4.24, p = .000), and seemed to do this more often with the intention to learn rather than only to solve a problem (U = 190.50, z = -1.88, p = .060). Table 3 provides quotes from the interviews that illustrate engagement in deliberate practice.
Case Test
The case test proved to be rather difficult: the average score of correctly answered items on the 26-item test was 14.67 (SD = 2.60; range 9–20). ANOVA and post-hoc analyses (Tukey HSD) showed that the experienced physicians had higher scores than the residents, F (2, 42) = 28.47, MSE = 4.96, p = .012 (see Table 1).
Relations Between Variables
The above analyses revealed multiple significant differences between residents and experienced physicians, whereas the two groups of experienced physicians only differed in terms of the number of patients they saw per week. Hence, relations between variables were examined separately for residents and experienced physicians, using Pearson correlation and Spearman’s rho.
Engagement in deliberate practice activities as measured by the sum of deliberate practice was not related to the goal orientations for either the residents or the experienced physicians. For the residents, however, mastery goal orientation was negatively related to mentioning explicit learning goals in their work (r = -.52, p = .033) while performance-avoidance goal orientation was negatively related to dealing with differences of opinion (r = -.64, p = .006).
The correlations between the work experience variables and engagement in deliberate practice activities showed some interesting patterns. Residents with more working hours were less likely to ask for advice with the intention to learn (r = -.50, p = .04). Residents who saw more patients had a lower level of deliberate practice in the context of problem solving (r = -.57, p = .016) and reflection (r = -.49, p = .045). Experienced physicians with more working hours, on the other hand, mentioned more explicit learning goals (r = .40, p = .034). With increasing years of work experience, however, they less often asked for advice (r = -.53, p = .004), were less likely to ask for advice with the intention to learn (r = -.34, p = .075), and dealt with differences of opinion on a lower deliberate practice level (r = -.59, p = .001).
Work experience, but not the sum of deliberate practice, proved to be related to case test performance among the residents (r = .55, p = .023; r = .13, p = .62, respectively). Among the experienced physicians, neither work experience nor the sum of deliberate practice were related to case test performance (r = .14, p = .48; r = .08, p = .69, respectively). However, engagement in activities to keep up-to-date seemed to contribute to the performance of the experienced physicians (r = .41, p = .031). The other work experience variables and deliberate practice activities were not correlated with the case test.
The relations between the learning behaviors and attitudes in our deliberate practice analysis showed some consistent patterns for residents (R) and experienced physicians (EP). Work goals were related to problem solving strategies (r R = .36, p = .16; r EP = .44, p = .019). Problem solving strategies were related to planning learning activities (r R = .34, p = .18; r EP = .39, p = .038) and planning learning activities was related to activities to keep up-to-date (r R = .42, p = .092; r EP = .40, p = .034). For the experienced physicians, problem solving strategies were related to feedback seeking (r EP = .46, p = .014), while for the residents, they were related to reflection (r R = .58, p = .015). Feedback seeking and reflection were related for residents (r R = .56, p = .019). Finally, for the experienced physicians, planning learning activities was positively related to contributing to knowledge development (r EP = .51, p = .005), whereas this relation was negative for the residents (r R = -.49, p = .044).
Discussion
Although physicians’ motivation to learn from and for their work is considered vital for professional development and performance improvement, research on this topic has been scarce (Ericsson 2004; Guest et al. 2001). In the present study, we examined the motivation for work-related learning among residents and experienced physicians from a deliberate practice perspective, and investigated whether this motivation contributed to expertise development beyond work experience. With regard to our first research question, we found that although all participants had a high mastery goal orientation, their learning was to a large extent embedded in everyday work; most of their learning activities were inherent to the job rather than motivated by the kind of competence improvement goals that characterize deliberate practice. The problems encountered in patient care played a key role in prompting learning. Role, work experience and work situation affected the type of activities engaged in, as well as the intensity of practice. With regard to our second research question, we found that the deliberate engagement in work-related learning activities was neither related to goal orientations, nor to case test performance, except for the experienced physicians’ activities to keep up-to-date. Work experience, in contrast, showed a clear positive relationship with the residents’ performance. Below, we discuss the results regarding the motivation for work-related learning and the contribution to expertise. We also discuss the limitations of the present study and the implications for future research, and provide educational implications to improve learning in medical practice.
Motivation for Work-Related Learning
The analysis of the interviews showed that the participants’ motivation for work-related learning was inherent to the job of providing high-quality patient care, rather than being characteristic of deliberate practice. Although the residents more explicitly expressed the intention to learn from their work than the experienced physicians, both groups indicated that they were primarily dedicated to achieving the best for patients. The extra effort and motivation required for learning in order to improve competence which characterizes deliberate practice, was found in about half of the participants for solving patients’ problems. The other identified activities, however, were not so much regarded as a learning opportunity. These results underline the value of challenging problems in everyday work for further inquiry and professional development (Duffy 2008; Guest et al. 2001; Hoffman and Donaldson 2004; Slotnick 1996, 1999), but they also show that there is room to increase physicians’ awareness with regard to taking control of their learning and using the available resources. This confirms the contention by Ericsson (2004, 2006, 2009) that the motivation to engage in deliberate practice activities during work is not self-evident.
The results, moreover, suggest that deliberate engagement in learning was determined by role, work experience and work situation. Residents asked more often for advice, while the experienced physicians more often used teaching, research and keeping up-to-date through independent studies and continuing medical education as a means to improve their competence. The more experienced the physician, the less advice they asked and the less they regarded differences of opinion as a learning opportunity. Residents who worked more hours were less likely to consult others for learning purposes and those who saw more patients were less motivated to learn from problem solving and reflection. These findings have important implications for physicians’ workplace learning, in terms of work procedures, time investment, work load and interactions among physicians. It should be noted that these issues go beyond physicians’ individual responsibility for learning and appeal to social structures and organizational practices to create working conditions that afford and support learning (Ashton 2004; Billett 2008; Bleakley 2006; Davis 2009; Hakkarinen et al. 2004; Harteis 2012; Hoffman and Donaldson 2004; Salas and Rosen 2010).
The high mastery goal orientation and the low performance approach goal orientation showed that all participants aimed for competence improvement and did not care so much about others’ opinions of them. However, the goal orientations were not meaningfully related to deliberate engagement in work-related learning activities. Only residents with higher scores on performance avoidance goal orientation were more prone to shun disagreements and to accept the opinions of their supervisors. The results suggest that the more general goal orientations do not capture the specific motivation to engage in learning activities in medical practice. This indicates that it is important in motivation research to look at the more specific content goals underlying behavior and the ways individuals choose to achieve these goals (Brett and VandeWalle 1999; Latham and Pinder 2005; Payne et al. 2007; Seijts et al. 2004).
Contribution of Motivation and Work Experience to Expertise
The number of years of work experience was related to expertise for the residents, but this does not seem to extend beyond the completion of training. The current number of working hours and the number of cases seen per week were not related to expertise as measured by the case test. Nor was case test performance influenced by the motivation to learn in terms of both goal orientations and deliberate engagement in work-related learning activities, except for the motivation of the experienced physicians to improve competence through activities to keep up-to-date. These results show that residents do indeed learn from their everyday experience and that an active attitude in keeping up-to-date matters in terms of acquiring usable knowledge.
In line with studies in work and organizational psychology (McDaniel et al. 1988; Schmidt et al. 1986) and the propositions on professional development by Ericsson (2004, 2006, 2009), our results suggest that performance particularly increases in the initial phases of supervised practice. In terms of deliberate practice, we only found that keeping up with developments in their field made a difference in the performance of the experienced physicians. This finding is consistent with a deliberate practice study among organizational consultants, which showed that top professionals spent twice as much time on activities to keep up-to-date, particularly by reading scientific literature and teaching, than their less successful colleagues with similar years of experience (Van de Wiel et al. 2004). Our results support the notion that keeping up with the medical literature through continuing education and daily practice is important to ensure high-quality healthcare (Choudrey et al. 2005; Eva 2002; Norman and Eva 2005). The fact that we did not find a relationship between the participants’ deliberate engagement in work-related learning and expertise, except for keeping up-to-date, may mean that the case test was not sensitive to the knowledge gained in such activities. However, we think that it is rather a sign that deliberate efforts to learn from and for medical practice were too limited to contribute, as these were very much entangled with everyday patient care. Further research is needed to better understand the interactions between the motivation to learn, the actual time and effort spent on learning activities, and the experience gained from medical practice.
Although medicine can be regarded as a high complexity job in which job knowledge is gained during the years of practice, we did not find, as Sturman (2003) reported, that the relationship between work experience and performance was stronger among the experienced physicians. Neither did we find that work experience reduced the performance on the case test, as has been reported for knowledge tests in medicine (Choudrey et al. 2005; Eva 2002). On the contrary, the experienced physicians performed better on the case test than the residents. According to the expert performance approach (Ericsson 2004, 2006, 2009; Ericsson et al. 2007; Ericsson and Smith 1991) the experienced physicians thus showed a higher level of expertise.
Limitations and Future Research
A limitation of the present study was a possible selection bias due to the low response rate. As our participants were probably those who were more motivated for learning, this may strengthen our conclusion that deliberate investment in learning needs to be increased, but may also have positively influenced the case test performance.
Another limitation is that we only gathered reports from the physicians themselves and did not collect more objective information on their learning behaviors from observations or documents. Thus, our deliberate practice analysis was based on participants’ accounts of how they engaged in work-related learning activities. We did endeavor, however, to create an open, informal atmosphere during the interviews. The questions focusing on specific situations and behaviors in the workplace prompted the participants to explicitly discuss the underlying goals and elicited spontaneous and sincere answers that yielded detailed insights into individual practices. Further research is needed to provide a more comprehensive view of physicians’ learning processes by observing behavior in practice as well as by administering questionnaires in more representative and larger samples. Future studies should also use methods like diaries to better estimate time investment in the different work-related learning activities, and make use of longitudinal designs that examine the learning and performance goals underlying these activities in short and long term.
A final limitation may reside in the way we measured expertise. In the introduction we discussed that the type of outcome measure may influence the experience-performance relationship, and this might also be true for our own results. The case test we used to measure expertise tested the application of diagnostic and therapeutic knowledge to evaluate short case descriptions in the broad domain of internal medicine, and can thus be regarded as a representative task in the medical domain. It proved to be a valid instrument to distinguish residents from experienced physicians and to reflect differences in the number of years of resident training. The relatively low mean score of 14.67 (56 %) showed that the case descriptions posed enough of a challenge and, in addition, may reflect the differences in specific expertise among our participants. As the items were derived from the MKSAP, a program developed to self-assess whether one has up-to-date practical knowledge, it might not be surprising that experienced physicians who put more effort into keeping up with new developments performed better on the test. The fact that the residents’ performance increased over the years suggests that they picked up relevant information about current practice guidelines during their training that could be applied in the case test.
Future research on medical expertise should consider other measures and competences relevant to the medical profession (Davis 2009; Frank 2005). A particularly important skill for high-quality performance in medicine is knowing when to switch from automatic to controlled processing (Ericsson 2004; Van de Wiel et al. 2004). Physicians must be able to act intuitively and fast (Harteis et al. 2012) and to recognize when they can trust their intuitive thoughts and when they need to follow-up and check their ideas by looking things up or asking colleagues for advice (Moulton et al. 2007; Eva and Regehr 2007). They need to monitor their uncertainty and gut feelings, take them seriously, and consider them in deciding upon further action (Mylopoulos and Regehr 2007; Stolper et al. 2010) This requires self-regulation of their thinking and sets the stage for self-regulated learning. Accurate assessments of the situational characteristics (e.g. routine or uncommon situation) and their own knowledge and skills provide the basis for relying on automatic processes or looking for further input to deal with the situation and learn from it to improve future performance. The interaction between automatic and controlled processes also manifests itself in deliberately choosing opportunities for refining one’s knowledge base by selecting experiences that allow practice and implicit learning or by setting challenging goals for deliberate learning. Two recent articles on intuition in decision-making emphasize that skilled intuition is based on learning in conditions that allow expertise development (Hogarth 2010; Kahneman and Klein 2009). Further research into these conditions and the interaction between learning-by-doing and learning-by-intention is required.
Educational Implications
The present study provides several suggestions for improving learning in medical practice. At the individual level, physicians could take more control of their own professional development and enhance their ability to self-regulate their learning. The organizations in which they work, i.e. the specific hospitals and departments, have a responsibility to help them acquire a repertoire of behaviors that enable this and motivate them to invest in building their expertise. This means that learning attitudes and behaviors should be set as norms in the organization, modeled by influential experienced physicians, and integrated in work procedures. Since providing high-quality patient care is already the norm, routine procedures for diagnosing and treating patients could be better exploited for learning purposes. The work-related learning activities investigated in our study could all be practiced at a more conscious level to promote professional development. Table 3 provides examples of the ways in which our participants achieved deliberate practice in their work.
Based on the social-cognitive theory of self-regulation (Zimmerman 2000, 2006), development might be further improved by setting challenging but attainable learning goals (see also Locke and Latham 2006; Zimmerman 2008), setting clear reference standards for patient care that could be used in monitoring and evaluating performance and providing feedback (see also Davis 2009; Ericsson 2004), and thinking aloud while choosing between alternatives in patient care, using mental simulations of outcome scenarios. Direct instruction can make students and physicians aware of these self-regulated learning behaviors, while modeling and practice are needed to incorporate them in regular work habits (Boekaerts 1997; Van de Wiel et al. 2004; Zimmerman 2000). In addition, the clinical teaching literature emphasizes that an open atmosphere that fosters positive relationships, encourages participation, activates critical thinking and shows enthusiasm for the profession supports learning (Sutkin et al. 2008). Clinical teachers are regarded as important role models in conveying the values and attributes of the profession, besides supervising the procedural and content aspects of health care.
Investments in learning and teaching activities obviously require resources that might be scarce in clinical practice, time being the most obvious example (Hoffman and Donaldson 2004; Wyatt and Sullivan 2005). Thus, if hospitals, and organizations in general, take continuous development seriously, they should invest in the life-long learning habits of professionals in routine work procedures. Our study showed that residents, who are trained on the job, should not be fully absorbed by patient care, but should be given enough time to follow up and assimilate their experiences. The experienced physicians, on the other hand, could be more intensively involved in supervision and discussions with colleagues. Efforts to organize the sharing of information, considerations and research findings in dealing with the more complex patient problems in everyday routines may play a key role in involving everyone in learning. Furthermore, work procedures need to be critically reviewed to see whether they produce maximal benefit from exchanging feedback, knowledge and experience among specialists with different expertise and roles. In addition, reflecting on the course of disease over longer periods of time and among different attending physicians could also be exploited to generate useful feedback. Finally, sharing clinical uncertainty as a means to improve on current practices may encourage those residents who are impeded by performance-avoidance goal orientations to set these aside and openly discuss what they do not know or are unsure of.
Although our study and its implications apply to the medical domain, we think that the recommendations provided to promote professional development can be used in other professions as well. Building expertise in the workplace is a multi-faceted learning process that, like the trajectory toward expertise in other domains, involves interactions between characteristics of the learner, the tasks engaged in, the context in which it takes place, and the time invested (Alexander et al. 2009).
Conclusion
Although patient care was found to induce relevant learning activities that contributed to expertise development among residents, life-long learning in medical practice could be enhanced by more deliberate investments. This includes investments on the part of individual physicians to plan, monitor and evaluate their own learning, as well as investments on the part of the organization they are working for to promote education and facilitate work procedures that capitalize on the learning potential of the workplace. In this way, the interaction between learning-by-doing and learning-by-intention can be reinforced, helping physicians to adapt to the requirements of their dynamic working environment (Mylopoulos and Regehr 2007). It can be argued that these implications are not restricted to medicine, but could be used to promote expertise in the workplace in other professions as well. The theory of deliberate practice proved to be a valuable framework for investigating how people learn in the workplace. It also provides principles to guide the analysis of professional learning and the design of working environments that promote the development of expertise (Van de Wiel et al. 2011b). Future research may test the specific interventions suggested in the educational implications section above, as well as examine specific learning activities that highly impact on workplace learning, such as problem-solving and knowledge-sharing, and should further disentangle the complex three-way interaction between work experience, deliberate practice and expertise to fully benefit from the merits of both implicit and intentional learning.
Notes
Other authors have emphasized that goal orientations are domain- and situation-specific and can be formed by classroom structures, instruction and strong situational cues, such as specific task goals (Ames 1992; Dweck and Master 2008; Latham and Pinder 2005). In their meta-analysis, Payne et al. (2007) distinguished between trait and state goal orientation. Trait goal orientation is dispositional, whereas state goal orientation is specific to a certain task and context and can be experimentally induced.
References
Alexander, P. A., Murphy, P. K., Kulikowich, J. M., Smith, M. C., & DeFrates-Densch, N. (2009). Expertise and the adult learner: A historical, psychological, and methodological exploration. In Handbook of research on adult learning and development (pp. 484-523). New York, NY US: Routledge/Taylor & Francis Group.
American College of Physicians. (2004). Medical knowledge self assessment program (13th ed.). Philadelphia, PA: American College of Physicians.
Ames, C. (1992). Classrooms: Goals, structures, and student motivation. Journal of Educational Psychology, 84(3), 261–271.
Arts, J. A. R., Gijselaers, W. H., & Boshuizen, H. P. A. (2006). Understanding managerial problem-solving, knowledge use and information processing: Investigating stages from school to the workplace. Contemporary Educational Psychology, 31(4), 387–410.
Ashford, S. J., Blatt, R., & VandeWalle, D. (2003). Reflections on the looking glass: A review of research on feedback-seeking behavior in organizations. Journal of Management, 29(6), 773–799.
Ashton, D. N. (2004). The impact of organisational structure and practices on learning in the workplace. International Journal of Training and Development, 8(1), 43–53.
Billett, S. (2008). Emerging perspectives on workplace learning. In S. Billett, C. Harteis, & A. Eteläpelto (Eds.), Emerging perspectives of workplace learning (pp. 1–15). Rotterdam: Sense Publishers.
Bleakley, A. (2006). Broadening conceptions of learning in medical education: the message from teamworking. Medical Education, 40(2), 150–157.
Boekaerts, M. (1997). Self-regulated learning: A new concept embraced by researchers, policy makers, educators, teachers, and students. Learning and Instruction, 7(2), 161–186.
Brett, J. F., & VandeWalle, D. (1999). Goal orientation and goal content as predictors of performance in a training program. Journal of Applied Psychology, 84(6), 863–873.
Button, S. B., Mathieu, J. E., & Zajac, D. M. (1996). Goal orientation in organizational research: A conceptual and empirical foundation. Organizational Behavior and Human Decision Processes, 67(1), 26–48.
Charness, N., Tuffiash, M., Krampe, R., Reingold, E., & Vasyukova, E. (2005). The role of deliberate practice in chess expertise. Applied Cognitive Psychology, 19(2), 151–165.
Chi, M. T. H., Feltovich, P. J., & Glaser, R. (1981). Categorization and representation of physics problems by experts and novices. Cognitive Science, 5, 121–152.
Choudrey, N. K., Fletcher, R. H., & Soumerai, S. B. (2005). Systematic review: The relationship between clinical experience and quality of health care. Annals of Internal Medicine, 142(4), 260–273.
Davis, D. (2009). How to help professionals maintain and improve their knowledge and skills: Triangulating best practices in medicine. In K. A. Ericsson (Ed.), Development of professional expertise: Toward measurement of expert performance and design of optimal learning environments (pp. 180–202). New York, NY: Cambridge University Press.
Day, E. A., Radosevich, D. J., & Chasteen, C. S. (2003). Construct- and criterion-related validity of four commonly used goal orientation instruments. Contemporary Educational Psychology, 28(4), 434–464.
De Groot, A. D. (1978). Thought and choice in chess (2nd ed.). Oxford England: Mouton.
Duffy, F. D. (2008). Commentary: Training internists for practice focused on meeting patient needs. Academic Medicine, 83(10), 893–896.
Dweck, C. S., & Master, A. (2008). Self-theories motivate self-regulated learning. In D. H. Schunk & B. J. Zimmerman (Eds.), Motivation and self-regulated learning: Theory, research, and applications (pp. 31–51). Mahwah, NJ US: Lawrence Erlbaum Associates Publishers.
Elstein, A. S., & Schwarz, A. (2002). Clinical problem solving and diagnostic decision making: Selective review of the cognitive literature. Britisch Medical Journal, 324, 729–732.
Emans, B. (2004). Interviewing: Theory, techniques and training. Groningen, The Netherlands: Wolters-Noordhoff.
Eraut, M. (2000). Non-formal learning and tacit knowledge in professional work. British Journal of Educational Psychology, 70, 113–136.
Ericsson, K. A. (2004). Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Academic Medicine, 79(10 Suppl), S70–S81.
Ericsson, K. A. (2006). The Influence of experience and deliberate practice on the development of superior expert performance. In K. A. Ericsson, N. Charness, P. J. Feltovich, & R. R. Hoffman (Eds.), The Cambridge handbook of expertise and expert performance (pp. 683–704). New York, NY: Cambridge University Press.
Ericsson, K. A. (2009). Enhancing the development of professional performance: Implications from the study of deliberate practice. In K. A. Ericsson (Ed.), Development of professional expertise: Toward measurement of expert performance and design of optimal learning environments (pp. 405–431). New York, NY: Cambridge University Press.
Ericsson, K. A., & Smith, J. (1991). Prospects and limits of the empirical study of expertise: An introduction. In K. A. Ericsson & J. Smith (Eds.), Toward a general theory of expertise: Prospects and limits (pp. 1–38). Cambridge: Cambridge University Press.
Ericsson, K. A., Krampe, R. T., & Tesch-Römer, C. (1993). The role of deliberate practice in the acquisition of expert performance. Psychological Review, 100(3), 363–406.
Ericsson, K. A., Roring, R. W., & Nandagopal, K. (2007). Giftedness and evidence for reproducibly superior performance: An account based on the expert performance framework. High Ability Studies, 18(1), 3–56.
Eva, K. W. (2002). The aging physician: Changes in cognitive processing and their impact on medical practice. Academic Medicine, 77(10), S1–S5.
Eva, K. W., & Regehr, G. (2007). Knowing when to look it up: A new conception of self-assessment ability. Academic Medicine, 82(10), S81–S84.
Eva, K. W., Link, C. L., Lutfey, K. E., & McKinlay, J. B. (2010). Swapping horses midstream: Factors related to physicians' changing their minds about a diagnosis. Academic Medicine, 85(7), 1112–1117.
Ford, J. K., Smith, E. M., Weissbein, D. A., Gully, S. M., & Salas, E. (1998). Relationships of goal orientation, metacognitive activity, and practice strategies with learning outcomes and transfer. Journal of Applied Psychology, 83(2), 218–233.
Frank, J. R. (2005). The CanMEDS 2005 Physician Competency Framework. Ottawa, Ontario: The Royal College of Physicians and Surgeons of Canada.
Gobet, F., & Charness, N. (2006). Expertise in chess. In K. A. Ericsson, N. Charness, P. J. Feltovich & R. R. Hoffman (Eds.), The Cambridge handbook of expertise and expert performance (pp. 523–538). New York, NY: Cambridge University Press.
Guest, C. B., Regehr, G., & Tiberius, R. G. (2001). The life long challenge of expertise. Medical Education, 35(1), 78–81.
Hakkarinen, K., Palonen, T., Paavola, S., & Lehtinen, E. (2004). Communities of networked expertise: Educational and professional perspectives. Amsterdam: Elsevier.
Harteis, C. (2012). When workplace learning fails: individual and organisational limitations - exemplarily demonstrated by the issue of responsibility in work life. International Journal of Human Resources Development and Management, 12, 92–107.
Harteis, C., Morgenthaler, B., Kugler, C., Ittner, K. P., Roth, G., & Graf, B. (2012). Professional competence and intuitive decision making: A simulation study in the domain of emergency medicine. Vocations and Learning, 5, 119–136.
Hobus, P. P., Schmidt, H. G., Boshuizen, H. P., & Patel, V. L. (1987). Contextual factors in the activation of first diagnostic hypotheses: Expert-novice differences. Medical Education, 21(6), 471–476.
Hoffman, K. G., & Donaldson, J. F. (2004). Contextual tensions of the clinical environment and their influence on teaching and learning. Medical Education, 38(4), 448–454.
Hogarth, R. M. (2010). Intuition: A challenge for psychological research on decision making. Psychological Inquiry, 21(4), 338–353.
Janssen, O., & Prins, J. (2007). Goal orientations and the seeking of different types of feedback information. Journal of Occupational and Organizational Psychology, 80(2), 235–249.
Kahneman, D., & Klein, G. (2009). Conditions for intuitive expertise: A failure to disagree. American Psychologist, 64(6), 515–526.
Latham, G. P., & Pinder, C. C. (2005). Work motivation theory and research at the dawn of the twenty-first century. Annual Review of Psychology, 56, 485–516.
Lesgold, A., Rubinson, H., Feltovich, P., Glaser, R., Klopfer, D., Wang, Y., et al. (1988). Expertise in a complex skill: Diagnosing x-ray pictures. In M. T. H. Chi, R. Glaser, & M. J. Farr (Eds.), The nature of expertise (pp. 311–342). Hillsdale, NJ England: Lawrence Erlbaum.
Locke, E. A., & Latham, G. P. (2002). Building a practically useful theory of goal setting and task motivation: A 35-year odyssey. American Psychologist, 57(9), 705–717.
Locke, E. A., & Latham, G. P. (2006). New directions in goal-setting theory. Current Directions in Psychological Science, 15(5), 265–268.
McDaniel, M. A., Schmidt, F. L., & Hunter, J. E. (1988). Job experience correlates of job performance. Journal of Applied Psychology, 73(2), 327–330.
Moulton, C. E., Regehr, G., Mylopoulos, M., & MacRae, H. M. (2007). Slowing down when you should: A new model of expert judgment. Academic Medicine, 82(10 Suppl), S109–S116.
Murphy, P. K., & Alexander, P. A. (2000). A motivated exploration of motivation terminology. Contemporary Educational Psychology, 25(1), 3–53.
Mylopoulos, M., & Regehr, G. (2007). Cognitive metaphors of expertise and knowledge: prospects and limitations for medical education. Medical Education, 41(12), 1159–1165.
Norman, G. R., & Eva, K. W. (2005). Does clinical experience make up for failure to keep up to date? Evidence-Based Medicine, 10, 66–68.
Norman, G. R., Trott, A. D., Brooks, L. R., & Smith, E. K. M. (1994). Cognitive differences in clinical reasoning related to postgraduate training. Teaching and Learning in Medicine, 6(2), 114–120.
Norman, G. R., Eva, K., Brooks, L., & Hamstra, S. (2006). Expertise in medicine and surgery. In K. A. Ericsson, N. Charness, P. J. Feltovich, & R. R. Hoffman (Eds.), The Cambridge handbook of expertise and expert performance (pp. 339–354). New York, NY: Cambridge University Press.
Payne, S. C., Youngcourt, S. S., & Beaubien, J. M. (2007). A meta-analytic examination of the goal orientation nomological net. Journal of Applied Psychology, 92(1), 128–150.
Pintrich, P. R. (2000). The role of goal orientation in self-regulated learning. In M. Boekaerts & P. R. Pintrich (Eds.), Handbook of self regulation (pp. 451–502). San Diego, CA, US: Academic.
Plant, E. A., Ericsson, K. A., Hill, L., & Asberg, K. (2005). Why study time does not predict grade point average across college students: Implications of deliberate practice for academic performance. Contemporary Educational Psychology, 30(1), 96–116.
Quinones, M. A., Ford, J. K., & Teachout, M. S. (1995). The relationship between work experience and job performance: A conceptual and meta-analytic review. Personnel Psychology, 48(4), 887–910.
Salas, E., & Rosen, M. A. (2010). Experts at work: Principles for developing expertise at work. In S. W. J. Kozlowski & E. Salas (Eds.), Learning, training, and development in organizations (pp. 99–134). New York, NY: Routledge.
Samuels, M. A., & Ropper, A. H. (2005). The relationship between clinical experience and quality of health care. Annals of Internal Medicine, 143(1), 84.
Sargeant, J., Mann, K., Sinclair, D., Ferrier, S., Muirhead, P., van der Vleuten, C., et al. (2006). Learning in practice: Experiences and perceptions of high-scoring physicians. Academic Medicine, 81(7), 655–660.
Schmidt, H. G., & Boshuizen, H. P. (1993). On the origin of intermediate effects in clinical case recall. Memory and Cognition, 21(3), 338–351.
Schmidt, H. G., & Rikers, R. M. J. P. (2007). How expertise develops in medicine: Knowledge encapsulation and illness script formation. Medical Education, 41(12), 1133–1139.
Schmidt, F. L., Hunter, J. E., & Outerbridge, A. N. (1986). Impact of job experience and ability on job knowledge, work sample performance, and supervisory ratings of job performance. Journal of Applied Psychology, 71(3), 432–439.
Schmidt, H. G., Norman, G. R., & Boshuizen, H. P. (1990). A cognitive perspective on medical expertise: Theory and implications. Academic Medicine, 65(10), 611–621.
Schön, D. A. (1983). The reflective practioner: How professionals think in action. New York: Basic Books.
Seijts, G. H., Latham, G. P., Tasa, K., & Latham, B. W. (2004). Goal setting and goal orientation: An integration of two different yet related literatures. Academy of Management Journal, 47(2), 227–239.
Simon, H. A., & Chase, W. G. (1973). Skill in chess. American Scientist, 61(4), 394–403.
Slotnick, H. B. (1996). How doctors learn: The role of clinical problems across the medical school-to-practice continuum. Academic Medicine, 71(1), 28–34.
Slotnick, H. B. (1999). How doctors learn: Physicians' self-directed learning episodes. Acadamic Medicine, 74(10), 1106–1117.
Sonnentag, S., & Kleine, B. M. (2000). Deliberate practice at work: A study with insurance agents. Journal of Occupational and Organizational Psychology, 73(1), 87–102.
Stolper, E., Van de Wiel, M., Van Royen, P., Van Bokhoven, M., Van der Weijden, T., & Dinant, G. J. (2010). Gut feelings as a third track in general practitioners' diagnostic reasoning. Journal of General Internal Medicine, 26(2), 197–203.
Sturman, M. C. (2003). Searching for the inverted U-shaped relationship between time and performance: Meta-analyses of the experience/performance, tenure/performance, and age/performance relationships. Journal of Management, 29(5), 609–640.
Sutkin, G., Wagner, E., Harris, I., & Schiffer, R. (2008). What makes a good clinical teacher in medicine? A review of the literature. Academic Medicine, 83(5), 452–466.
Tesluk, P. E., & Jacobs, R. R. (1998). Toward an integrated model of work experience. Personnel Psychology, 51(2), 321–355.
Teunissen, P. W., Scheele, F., Scherpbier, A. J. J. A., van der Vleuten, C. P. M., Boor, K., van Luijk, S. J., et al. (2007). How residents learn: Qualitative evidence for the pivotal role of clinical activities. Medical Education, 41(8), 763–770.
Teunissen, P. W., Stapel, D. A., van der Vleuten, C., Scherpbier, A., Boor, K., & Scheele, F. (2009). Who wants feedback? An investigation of the variables influencing residents' feedback-seeking behavior in relation to night shifts. Academic Medicine, 84(7), 910–917.
Tuominen-Soini, H., Salmela-Aro, K., & Niemivirta, M. (2010). Stability and change in achievement goal orientations: A person-centred approach. Contemporary Educational Psychology. doi:10.1016/j.cedpsych.2010.08.002.
Van de Wiel, M. W. J., Boshuizen, H. P. A., & Schmidt, H. G. (2000). Knowledge restructuring in expertise development: Evidence from pathophysiological representations of clinical cases by students and physicians. European Journal of Cognitive Psychology, 12(3), 323–355.
Van de Wiel, M. W. J., Szegedi, K. H. P., & Weggeman, M. C. D. P. (2004). Professional learning: Deliberate attempts at developing expertise. In H. P. A. Boshuizen, R. Bromme, & H. Gruber (Eds.), Professional learning: Gaps and transitions on the way from novice to expert (pp. 181–206). Dordrecht: Kluwer.
Van de Wiel, M. W. J., Van den Bossche, P., Janssen, S., & Jossberger, H. (2011). Exploring deliberate practice in medicine: How do physicians learn in the workplace? Advances in Health Sciences Education, 16, 81–95. doi:10.1007/s10459-010-9246-3.
Van de Wiel, M. W. J., Van den Bossche, P., & Koopmans, R. P. (2011). Deliberate practice, the high road to expertise: K.A. Ericsson. In F. Dochy, D. Gijbels, M. Segers, & P. Van den Bossche (Eds.), Theories of learning for the workplace: Building blocks for training and professional development programs (pp. 1–16). London: Routledge.
VandeWalle, D. (1997). Development and validation of a work domain goal orientation instrument. Educational and Psychological Measurement, 57(6), 995–1015.
VandeWalle, D. (2003). A goal orientation model of feedback-seeking behavior. Human Resource Management Review, 13(4), 581–604.
Wyatt, J. C., & Sullivan, F. (2005). Keeping up: Learning in the workplace. British Medical Journal, 331(7525), 1129–1132.
Zimmerman, B. J. (1998). Developing self-fulfilling cycles of academic regulation: An analysis of exemplary instructional models. In D. H. Schunk (Ed.), Self regulated learning: From teaching to self reflective practice (pp. 1–19). New York, NY: Guilford Publications, Inc.
Zimmerman, B. J. (2000). Attaining self-regulation: A social cognitive perspective. In M. Boekaerts & P. R. Pintrich (Eds.), Handbook of self regulation (pp. 13–39). San Diego, CA: Academic.
Zimmerman, B. J. (2006). Development and adaptation of expertise: The role of self-regulatory processes and beliefs. In K. A. Ericsson, N. Charness, P. J. Feltovich, & R. R. Hoffman (Eds.), The Cambridge handbook of expertise and expert performance (pp. 705–722). New York, NY: Cambridge University Press.
Zimmerman, B. J. (2008). Goal setting: A key proactive source of academic self-regulation. In D. H. Schunk & B. J. Zimmerman (Eds.), Motivation and self-regulated learning: Theory, research, and applications (pp. 267–295). Mahwah, NJ: Lawrence Erlbaum Associates Publishers.
Zimmerman, B. J., & Schunk, D. H. (2008). Motivation: An essential dimension of self-regulated learning. In D. H. Schunk & B. J. Zimmerman (Eds.), Motivation and self-regulated learning: Theory, research, and applications (pp. 1–30). Mahwah, NJ: Lawrence Erlbaum Associates Publishers.
Acknowledgements
The authors wish to thank Richard Koopmans, Jeroen Kooman, Walther van Mook, Roger Rennenberg, Nicolaas Schaper, and Coen Stehouwer of the Department of Internal Medicine at Maastricht University Medical Center for their support in developing the materials for this study and reflecting on the outcomes. Furthermore, they would like to thank Sandra Janssen and Helen Jossberger for administering the interviews and questionnaires and for their contribution to the first analysis. Chantal Bemelmans’ assistance in developing the second analysis and scoring the data as the main rater is greatly appreciated. Finally, the authors wish to thank the physicians who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van de Wiel, M.W.J., Van den Bossche, P. Deliberate Practice in Medicine: The Motivation to Engage in Work-Related Learning and Its Contribution to Expertise. Vocations and Learning 6, 135–158 (2013). https://doi.org/10.1007/s12186-012-9085-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12186-012-9085-x