Abstract
FMS-like tyrosine kinase 3 (FLT3) internal tandem duplication (ITD) mutations in patients with acute myeloid leukemia (AML) are associated with early relapse and poor survival. This multicenter, single-arm, two-stage phase 2 study (NCT02984995) was conducted to evaluate the efficacy and safety of quizartinib hydrochloride (initial dose 20/30 mg/day), an oral, highly potent, selective FLT3 inhibitor in Japanese patients (median age 65 years) with FLT3-ITD positive relapsed/refractory (R/R) AML. The composite complete remission (CRc) rate (primary endpoint) was 53.8% (90% confidence interval 36.2–70.8%) for evaluable patients in the efficacy analysis set. The median duration of CRc and overall survival was 16.1 weeks and 34.1 weeks, respectively. The most frequent treatment-emergent adverse events (TEAEs) were febrile neutropenia (43.2%), platelet count decreased (37.8%), and QT prolonged (35.1%). Two (5.4%) patients experienced TEAEs associated with treatment discontinuation. All serious TEAEs (45.9%), except febrile neutropenia (16.2%), were reported in ≤ 2 patients. The incidence of QTcF 451–480 ms and 481–500 ms was 37.8% and 2.7%, respectively. No QTcF > 500 ms, events of torsade de pointes or arrhythmia with clinical symptoms were reported. Quizartinib monotherapy was well tolerated and resulted in clinically meaningful reductions in blast count in Japanese patients with FLT3-ITD R/R AML.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myeloid leukemia (AML) is the most common type of acute leukemia among adults worldwide [1] and comprises 70% of all cases of leukemia in Japan [2]. Although remission rates have improved over the years, the long-term survival rates are still 40% due to relapse following remission [3].
FMS-like tyrosine kinase 3 (FLT3) is a transmembrane tyrosine kinase in the class III split-kinase domain family of receptor tyrosine kinase [4, 5]. FLT3 mutations are the most common mutations in AML, of which internal tandem duplications (ITD) are predominant and reported in approximately 25% of adult patients newly diagnosed with AML [6, 7]. Patients with FLT3-ITD positive AML are genetically stratified into the risk group in the AML guidelines because of their association with poor prognoses [1, 8].
FLT3-ITD mutation was identified as a strong predictor of relapse rate, poor disease-free survival, event-free survival (EFS), and overall survival (OS) from univariate and multivariate analyses in a large United Kingdom study comprising patients from two AML studies [9]. Similarly, in a Japanese study comprising patients newly diagnosed with de novo AML, the predicted OS rate at 60 months was much lower in those with FLT3-ITD mutations than in those without. Additionally, on multivariate analysis, FLT3-ITD was the most unfavorable predictor for OS in patients < 60 years old [4]. A comparative study in patients with relapsed AML, with and without FLT3-ITD mutations, observed poorer response [complete remission (CR) rate 24% vs 38%] to salvage therapy (including intensive chemotherapy and allogenic transplants) with significantly shorter survival from time of relapse in the 34 patients with FLT3-ITD mutations. The failure of salvage therapy was associated with resistant disease in 65% of the patients in this study [10].
Several therapies targeting FLT3-selective tyrosine kinase inhibitors that have cytotoxicity in leukemic blasts are in development [11]. Gilteritinib, a small molecule inhibitor of the tyrosine kinases FLT3/AXL [12], was approved in Japan in September 2018 for the treatment of patients with relapsed/refractory (R/R) FLT3-mutated AML and was also approved in the United States in November 2018. However, no other FLT3 targeted therapies are currently approved. There remains an unmet need for effective treatment options in patients with R/R FLT3-mutated AML.
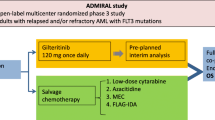
Quizartinib is an oral, potent, highly selective, second-generation FLT3 inhibitor that is active against FLT3-ITD positive AML [13]. The global phase 1, 2, and 3 study results of quizartinib monotherapy in patients with R/R FLT3-ITD positive AML were promising [14,15,16]. In a phase 1, dose-escalation (12–450 mg/day) study, quizartinib demonstrated an acceptable toxicity profile (maximum tolerated dose 200 mg/day) with clinical response in 53% (9 of 17) patients with FLT3-ITD positive AML [14]. In a phase 2 study of quizartinib (90–200 mg/day) with 2 cohorts, the composite CR (CRc) rate was 56% in FLT3-ITD positive AML patients aged ≥ 60 years who had R/R AML within 1 year after first-line therapy and 46% in those aged ≥ 18 years who had R/R AML following salvage chemotherapy or hematopoietic stem cell transplant (HSCT) [15]. A subsequent open-label, randomized, phase 2b study in patients with R/R FLT3-ITD positive AML who had received previous salvage chemotherapy or HSCT that evaluated a quizartinib initial dose of 30 mg/day or 60 mg/day found a similar CRc rate of 47% to the previous phase 2 study [16]. Considering the incidence of QT prolongation in these phase 2 trials, the maximum dose of quizartinib was determined as 60 mg/day. The QuANTUM-R (ClinicalTrials.gov identifier NCT02039726) study was the first phase 3 study to determine whether quizartinib monotherapy prolongs OS compared with standard salvage chemotherapy in patients with R/R FLT3-ITD positive AML. Patients randomized to the quizartinib group received an initial quizartinib dose of 30 mg/day (20 mg/day in patients using concomitant strong CYP3A4 inhibitors) for 15 days, and the dose was escalated to 60 mg/day (30 mg/day in patients using concomitant strong CYP3A4 inhibitors) if QTcF was ≤ 450 ms on day 16. Quizartinib monotherapy demonstrated a significantly prolonged OS (median 6.2 months) compared with standard salvage chemotherapy (median 4.7 months) in patients with R/R FLT3-ITD positive AML [hazard ratio 0.76; 95% confidence interval (CI) 0.58–0.98]. The CRc rate was 48% (95% CI 42–55%) and 27% (19–36%), and median (95% CI) CRc duration was 12.1 (10.4–27.1) weeks and 5.0 (3.3–12.6) weeks in the quizartinib and salvage chemotherapy groups, respectively [17]. However, the QuANTUM-R study was conducted in non-Japanese patients only, and additional data are required to confirm the efficacy of quizartinib in the Japanese population.
In a phase 1 study in Japanese patients (ClinicalTrials.gov identifier NCT02675478) [18] with R/R AML, quizartinib was well tolerated, irrespective of FLT3-ITD mutation, and a 60 mg/day dose was recommended for the phase 2 study in Japanese patients with R/R AML (data unpublished). The current phase 2 study aimed to confirm the efficacy and safety of quizartinib in Japanese patients with FLT3-ITD positive R/R AML, and the population, dosing regimen, and assessment of this study resembled that of the QuANTUM-R study.
Methods
Study design
This was a multicenter, open-label, single-arm, phase 2 study conducted in Japan. A two-stage design [19] was applied and the interim data at the end of stage 1 were evaluated to terminate the study due to efficacy or futility or to continue the study to stage 2. Overall, 25 patients and 16 patients were planned to be registered in stage 1 and stage 2, respectively. The criteria for decision making at the interim analysis and final analysis are described in Sect. 2.6.
Ethics
This study was conducted according to the ethical principles of the Declaration of Helsinki, the International Council for Harmonisation consolidated Guideline E6 for Good Clinical Practice and applicable regulatory requirements including ordinance No. 28 (27 Mar 1997) of the Japanese Ministry of Health, Labour and Welfare, the Act on Securing Quality, Efficacy and Safety of Pharmaceuticals, Medical Devices, Regenerative and Cellular Therapy Products, Gene Therapy Products, and Cosmetics No. 1 (25 Nov 2014) [20], and other applicable Japanese regulations. The genome/gene analysis was performed in accordance with the Ethical Guidelines for Human Genome/Gene Analysis Research [21] and the Ethical Guidelines for Clinical Studies [22], in addition to the above-mentioned regulations. The study protocol, amendments, the informed consent form(s), and information sheets were approved by the Institutional Review Boards of all participating sites. All study participants provided voluntary, written informed consent to take part in the study. The current study is registered at ClinicalTrials.gov (identifier NCT02984995).
Eligibility criteria
Adult patients (≥ 20 years of age) with primary AML or AML with a history of myelodysplastic syndrome, and first relapse within 6 months of achieving first remission with induction therapy/refractory to and no remission with all prior AML therapies with or without HSCT were included in the study. Refractory AML was defined as a less than 50% reduction in bone marrow blasts and failure to achieve CRc after 1 cycle of treatment or failure to achieve CRc after 2 cycles of treatment. First relapse was defined as achievement of first CRc after induction therapy and relapse within 6 months, with or without consolidation or maintenance therapy, and with or without HSCT. The duration of remission was defined as the day of the bone marrow test when CRc was confirmed or the day of HSCT to the day of the bone marrow test when relapse was confirmed or the day of reappearance of leukemic blasts in the peripheral blood. Patients were required to have FLT3-ITD mutation in bone marrow or peripheral blood and Eastern Cooperative Oncology Group performance status (ECOG PS) score of 0–2. The FLT3-ITD mutation status for all patients was finally confirmed by central assessment in this study; the protocol allowed the local FLT3-ITD assessment to evaluate the eligibility. The key exclusion criteria included the following: diagnosis of acute promyelocytic leukemia; AML associated with treatment of malignant tumor except myelodysplastic syndrome; history of malignant tumor within 5 years of registration; persistent, symptomatic grade ≥ 2 non-hematological toxicity; and clinically significant graft-versus-host disease. Patients with prior treatment with quizartinib, prior participation in any clinical study of quizartinib or prior treatment with other FLT3 inhibitors, including sorafenib and those under development except for midostaurin, were also excluded from the study.
Study treatment
In this study, treatment administration, assessments, and endpoints were similar to that in the pivotal phase 3 study [17]. Quizartinib was administered orally, once daily every morning in a continuous 28-day treatment cycle at an initial dose of 30 mg/day (as of quizartinib hydrochloride, initial dose of 20 mg/day in patients using concomitant strong CYP3A4 inhibitors). Quizartinib was administered in three doses: 20 mg/day, 30 mg/day, and 60 mg/day. The dose of quizartinib was increased by one dose level at a time, provided the average of triplicate QTcF values, measured by day 15 of cycle 1, was ≤ 450 ms. The dose was increased in patients who did not achieve CR, CR with incomplete platelet recovery (CRp), or incomplete hematologic recovery (CRi) after at least 1 cycle of treatment with quizartinib, if they met the following criteria: absence of grade ≥ 3 treatment-related non-hematological toxicity, increase of ≤ 60 ms in QTcF interval from baseline, and absence of aplastic bone marrow at the time of the decision to increase the dose.
Treatment was continued until any of the following withdrawal criteria were met: overt disease progression, grade 4 QTcF prolongation, left ventricular ejection fraction of less than 45%, treatment interruption for longer than 14 days, any deviation from inclusion/exclusion criteria, pregnancy, or patient’s request for treatment withdrawal. Treatment was also discontinued at the investigator’s discretion. Patients proceeded to the post-observation treatment period after treatment discontinuation.
Dose interruption for 14 days and/or dose reduction by one dose level at a time was stipulated according to the protocol-specified criteria of QTcF prolongation; non-hematological toxicity of grade ≥ 3 persisting for ≥ 48 h; myelosuppression (based on the investigator’s discretion), or concomitant initiation of treatment with strong CYP3A4 inhibitors (for dose reduction only). The dose could be resumed incrementally by 1 dose level (maximum 60 mg/day) to the earlier level, following recovery of non-hematological adverse event (AE), QTcF prolongation from grade 2 to grade 1 or lower, and discontinuation of concomitant strong CYP3A4 inhibitors, with the exception of a dose reduction due to grade 3 QTcF prolongation. Treatment could be resumed with the same dose of quizartinib as that administered at the time of interruption, if myelosuppression improved within 14 days of dose interruption.
Study assessments
Study assessments included central assessment of FLT3-ITD mutation (Navigate BioPharma, Carlsbad, California, USA) using peripheral blood or bone marrow samples. Other assessments included patient baseline characteristics. A 12-lead electrocardiogram (ECG) was performed at baseline and after administration of quizartinib on days 1, 2, 8, and 15 of cycle 1 and on day 1 of cycles 2, 3, 4, and later, and at withdrawal.
Study endpoints
The primary efficacy endpoint of the study was CRc rate (proportion of patients with best response of CR, CRp, or CRi) in FLT3-ITD positive patients with AML. The secondary efficacy endpoints included best response, response rate [proportion of patients whose best response was CR, CRp, CRi, or partial remission (PR)], OS, EFS, leukemia-free survival (LFS), and transplantation rate. Best response was defined as the overall best-measured response [CR, CRp, CRi, PR, or no response (NR)] of response assessments at all time points after the first dose of the study drug to the end of treatment (not including response from any subsequent AML therapy, including transplantation). Efficacy responses were assessed per sponsor-modified International Working Group criteria [23].
The response criteria are defined below.
CR
Achievement of a morphologic leukemia-free state (< 5% blasts in the bone marrow, no blasts with Auer rods, and no persistence of extramedullary disease), an absolute neutrophil count of ≥ 1000/mm3, and a platelet count of ≥ 100,000/mm3, independent of red blood cell (RBC) and platelet transfusions (defined as 4 weeks without RBC transfusion and 1 week without platelet transfusion).
CRp
CR with incomplete platelet recovery (< 100,000/mm3).
CRi
CR with incomplete hematological recovery with residual neutropenia of < 1000/mm3 with or without platelet count < 100,000/mm3. RBC and platelet transfusion independence was not required for CRi. Notably, patients meeting all criteria for CR or CRp, except RBC or platelet transfusion dependence, were still considered to have achieved CRi.
PR
CRi with the exception that only a decrease of ≤ 50% from the baseline bone marrow blast value to a total marrow blast count of 5–25%, inclusive, was required.
EFS
The time from the date of registration until documented failure to achieve CRc, relapse after CRc, or death from any cause, whichever occurred first.
LFS
The time from the first documented response of CRc until documented relapse or death from any cause.
The pharmacokinetics (PK) of quizartinib and its active metabolite (AC886), including maximum plasma concentration (Cmax), area under the plasma concentration–time curve (AUC), and time to reach Cmax (Tmax), were evaluated on days 1 and 15 of cycle 1.
Safety assessments included the incidence of treatment-emergent AEs (TEAEs). A TEAE was defined as an AE that occurred (or worsened) between the first dose of the study drug and the follow-up visit, 30–45 days after the last dose of the study drug. The Medical Dictionary for Regulatory Activities Version 20.1 was used to code all AEs. AEs and clinical laboratory values were graded using the Common Terminology Criteria for Adverse Events Version 4.0 Japanese version [24].
Decision-making criteria for the interim analysis and final analysis
A data monitoring committee (DMC) was established with the persons in charge of medical monitoring, clinical operation, biostatistics, PK analysis, and modeling and simulation, to review the interim analysis results. During the review process, the DMC could consult with external hematology oncology specialists as necessary.
An interim analysis was planned to be performed when 25 patients had been included in the efficacy analysis set in stage 1. The cut-off date for the interim analysis was determined as the day when all the 25 patients met at least one of the following criteria: best response was assessed as CR, CRp, or CRi; quizartinib was discontinued; and assessment of the response on day 1 of cycle 4 was completed. The day when any of the above criteria was met, whichever first, was determined for each patient. The latest day in the 25 patients included in the interim analysis was regarded as the data cut-off date. This procedure was to be applied to the analysis at the end of stage 2.
It was planned that the study would be terminated at the interim analysis due to efficacy [reject the null hypothesis (CRc rate of 23.5%)] if the number of patients with CRc was ≥ 11 of 25 patients; terminated due to futility if CRc ≤ 3; continued to the stage 2 to enroll 41 patients if CRc = 4–10. The results of the final analysis were to be assessed as follows: for the 41 patients included in the efficacy analysis set, if CRc had been achieved in 15 or more patients, the null hypothesis would be rejected.
Statistical analysis
The two-stage design proposed by Mander and Thompson [19] was applied to evaluate the interim data after stage 1 (25 evaluable patients) to terminate the study due to efficacy or futility, or to continue the study to stage 2 (additional 16 evaluable patients). The sample sizes for both the stages and the criteria for the interim and final analyses described in Sect. 2.6 were determined to provide 80% statistical power at a one-sided 5% significance level under the null hypothesis of a CRc rate of 23.5% [10] and the alternative hypothesis of 42%.
All safety analyses were performed using the safety analysis set, defined as all patients who received at least one dose of the study drug, and all efficacy parameters were analyzed using the efficacy analysis set comprising all patients who were FLT3-ITD positive by central assessment and had received at least one dose of the study drug. In addition, the PK data were analyzed using the PK analysis set including all patients who received at least one dose of the study drug, and for whom plasma drug concentration data were available for at least one time point after the start of treatment with the study drug.
The CRc rate of the primary endpoint was estimated based on the maximum likelihood method, and the corresponding 90% and 95% CIs were calculated using Clopper–Pearson’s exact method. The response rate, best response, and transplantation rate were also estimated along with the 95% CIs.
The durations of CRc, OS, EFS, and LFS were analyzed using the Kaplan–Meier method and medians with their corresponding 95% CIs were provided. The analysis for LFS was conditional on the patient having a documented best response of CRc. Patients without a documented best response of CRc were excluded from the analysis.
Safety parameters including TEAEs, clinical laboratory results, and QT prolongation were summarized. Plasma PK parameters were calculated using the actual time of blood collection. Summary statistics for plasma drug concentrations were calculated based on the scheduled time points.
All analyses were performed using SAS® version 9.2 or higher (SAS Institute Inc., Cary, NC, USA).
Results
Based on the results of the interim analysis in 25 patients who were evaluated from the efficacy analysis set in order of registration, CRc was achieved by 14 patients (data cut-off date: February 26, 2018). Given that the prespecified criterion of CRc in ≥ 11 of 25 patients was achieved with no safety-related concerns, the DMC decided to terminate the study on March 28, 2018, on account of confirmation of efficacy. The registration of patients was discontinued; at that point, 37 patients were registered in the study between January 2017 and February 2018 at 34 sites in Japan, and treatment with the study drug in patients receiving the study drug was continued until the discontinuation criteria were met. From this point forward, we present the results of the final analysis.
Patient disposition
All 37 patients were included in the safety and PK analysis sets, while 32 patients were included in the efficacy analysis set. The five patients excluded from the efficacy analysis set were those who were FLT3-ITD positive in the local assessment at registration but FLT3-ITD negative in the central assessment. Of the 37 patients, 9 patients were on treatment as of the data cut-off date. Overall, 28 patients discontinued the treatment [transplantation (15 patients), progressive disease (12 patients), and AEs (1 patient)], and 14 patients discontinued the study due to death (Fig. 1).
Patient demographics and baseline characteristics
The median age of all registered patients was 65.0 years and 59.5% of patients were women (Table 1). The median body mass index (BMI) was 20.9 kg/m2 and nearly half of the patients had an ECOG PS of 0 (48.6%). Twenty-four (64.9%) were relapsed patients and 13 (35.1%) were refractory patients.
Treatment exposure
Quizartinib was administered for a median (range) duration of 66.0 (11–288) days over a median 3 (1–11) cycles at a mean relative dose intensity of 86.9%. Of the 37 patients, 3 patients had started on 20 mg/day and 34 patients had started on 30 mg/day of quizartinib (Fig. 1). A total of 27 (73.0%) patients received a dose of 60 mg/day as the maximum daily dose. Dose reductions and dose interruptions during the study period were observed in 12 (32.4%) and 11 (29.7%) patients, respectively, the most frequent reason being AEs (Table 2).
Efficacy
The CRc rate, the primary endpoint, was 53.8%, with a 90% CI of 36.2–70.8 for evaluable patients (n = 26) in the efficacy analysis set (Table 3). As the lower limit of the 90% CI was greater than 23.5%, the null hypothesis was rejected and the primary objective of this study was met. The median duration of CRc was 16.1 weeks (95% CI 4.7–24.6). The response rate was 77.8% (95% CI 57.7–91.4). The median OS was 34.1 weeks (95% CI 27.1 to not reached; Fig. 2). The median EFS and LFS were 12.7 weeks (95% CI 0.1–24.7) and 16.1 weeks (95% CI 4.7–24.6), respectively (Supplementary Figs. 1 and 2). Overall, 12 of 32 (37.5%) patients underwent HSCT following quizartinib treatment.
Kaplan–Meier curve for overall survival. Patients without a documented best response of CRc were excluded from the analyses. CIs were calculated based on the method proposed by Brookmeyer and Crowley. CI, confidence interval; CRc, composite complete remission; NE, not evaluated; OS, overall survival
At cycle 1, day 15, geometric mean Cmax was higher in patients receiving an initial dose of 30 mg/day compared to those receiving 20 mg/day, the increase being almost dose-proportional for quizartinib (20 mg/day, 124 ng/mL; 30 mg/day, 170 ng/mL) and more than dose-proportional for AC886 (20 mg/day, 16.2 ng/mL; 30 mg/day, 135 ng/mL) and quizartinib + AC886 (20 mg/day, 145 ng/mL; 30 mg/day, 321 ng/mL). A similar trend was observed for AUC. The median Tmax did not differ notably between the patients with an initial dose of 20 mg/day and 30 mg/day (Table 4).
Safety
All 37 patients experienced at least one TEAE during the study duration (Table 5). The most frequently reported TEAEs were febrile neutropenia in 16 (43.2%), platelet count decreased in 14 (37.8%), ECG QT prolonged in 13 (35.1%), nausea in 11 (29.7%), and anemia in 10 (27.0%) patients. TEAEs of grade ≥ 3 were reported in 34 (91.9%) patients; the most frequently reported were febrile neutropenia in 14 (37.8%), platelet count decreased in 11 (29.7%), anemia in 9 (24.3%), neutrophil count decreased in 8 (21.6%), and white blood cell count decreased in 8 (21.6%) patients. Among them, serious TEAEs were reported in 17 (45.9%) patients, the most frequently reported (≥ 2 patients) were febrile neutropenia [6 (16.2%) patients], followed by bacteremia and sepsis [2 (5.4%) patients each].
TEAEs associated with treatment discontinuation were reported in two patients (5.4%). One patient experienced drug-related lipase increased. Progressive disease (refer to Sect. 3.1 patient disposition) in one patient resulted in death, which was considered as a TEAE associated with treatment discontinuation due to a fatal event (drug-unrelated). TEAEs associated with dose reduction and dose interruption were reported in 7 (18.9%) and 4 (10.8%) patients, respectively.
The incidence of QTcF 450–480 ms and QTcF 481–500 ms was 37.8% and 2.7%, respectively. No QTcF > 500 ms was observed. No events of torsade de pointes or arrhythmia with clinical symptoms were reported. A change in QTcF from baseline to worst post-treatment value > 30 ms was observed in 15 (40.5%) patients, including > 60 ms in one (2.7%). QTcF prolongation was resolved without discontinuation or interruption of quizartinib treatment in all patients except 1 (2.7%), who required a reduction in the quizartinib dose.
Discussion
The results of this phase 2 study demonstrate a favorable efficacy and acceptable safety profile for quizartinib in Japanese patients with FLT3-ITD positive R/R AML. These findings are consistent with the results of the phase 3 global QuANTUM-R study, which applied the same dosing regimen of quizartinib as this study but did not include Japanese patients [17]. Most patients discontinued treatment because of progressive disease or HSCT and only one due to increase in lipase levels that was considered related to the study drug. The exposure levels of quizartinib and its active metabolite were generally similar to those observed in the phase 1 study conducted in Japanese patients (data unpublished, submitted) and the phase 2b study in non-Japanese patients (data unpublished).
Quizartinib was well tolerated in Japanese patients with R/R AML. No grade ≥ 3 QT prolongation was observed in the current study. Moreover, no events of torsade de pointes or arrhythmia with clinical symptoms were reported during this study. QT prolongation associated with dose reduction occurred in only one patient, while no patient reported QT prolongation associated with treatment discontinuation in this study. These results indicate that quizartinib dose escalation was implemented appropriately in this study, and all the cardiac safety findings were manageable.
The CRc rate, the primary endpoint of this study, was 53.8%, and the lower limit of the 90% CI (36.2%) was greater than the threshold of the null hypothesis (23.5% [10]) prespecified in the protocol, indicating that the efficacy of quizartinib is superior to that of other widely used chemotherapies. Although CR was not observed, more than half the patients achieved CRc in the present study, which was comparable to the results in a previous global phase 2 study with 30-, 60-, and 90-/135-mg/day doses (47.4%, 47.4%, and 46.0–56.0%, respectively) and with a 60-mg/day dose (48.0%) in the phase 3 study [15,16,17]. The results of a meta-analysis of AML studies demonstrated that in addition to CR rate, CRi or CRi + CR rates were better predictors of median OS compared with overall response rate in elderly patients with AML [25]. Further, although CR has the greatest impact on OS, the median OS was longer in patients who achieved CRi, PR, or a morphologically leukemia-free response than in all patients that included the remaining patients with no response, in a retrospective analysis of patients receiving salvage therapy for R/R AML. Thus, lesser responses also have a significant impact on survival, but CR still confers the greatest benefit [26]. The duration of CRc in the current study was 16.1 weeks compared with 12.1 weeks in the global QuANTUM-R study [17]. In current study, 38% of patients underwent HSCT following quizartinib treatment and that of the QuANTUM-R study was similar (32%) [17]. The overarching goal of treatment for patients with R/R AML is to induce a second remission and bring as many patients as possible to HSCT, which represents the only established therapeutic option offering a longer survival and possible cure [27]. Therefore, quizartinib treatment appears to be a promising therapy with the potential of bridging patients with R/R AML with FLT3-ITD positive to transplantation. The QuANTUM-R study reported a median OS of 27.0 weeks with quizartinib treatment [17], which was comparable to that in the current study.
Although the majority of CRc was CRi in this study, we believe that treatment with quizartinib monotherapy 60 mg/day resulted in clinically meaningful reductions in blast count in Japanese patients with FLT3-ITD positive R/R AML, irrespective of whether they were eligible for HSCT or were elderly and not eligible for HSCT.
This study was limited by its small sample size and lack of a control arm. Additionally, only short-term data could be collected and long-term safety and efficacy of quizartinib treatment could not be assessed. Moreover, as with other clinical trials, the efficacy and safety of quizartinib was assessed in a controlled patient population (e.g., inclusion and exclusion criteria, concomitant therapy, and performance status), and the results may not be directly extrapolated to the more diverse R/R AML patient population.
Conclusions
Treatment with quizartinib monotherapy 60 mg/day was well tolerated and resulted in clinically meaningful reductions in blast count in Japanese patients with FLT3-ITD positive R/R AML.
References
O’Donnell MR, Tallman MS, Abboud CN, Altman JK, Appelbaum FR, Arber DA, et al. Acute myeloid leukemia, version 3.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2017;15:926–57.
Niino M, Matsuda T. Type distribution of myeloid leukemia from Cancer Incidence in Five Continents vol. X. Jpn J Clin Oncol. 2016;46:394.
Ohtake S, Miyawaki S, Kiyoi H, Miyazaki Y, Okumura H, Matsuda S, et al. Randomized trial of response-oriented individualized versus fixed-schedule induction chemotherapy with idarubicin and cytarabine in adult acute myeloid leukemia: the JALSG AML95 study. Int J Hematol. 2010;91:276–83.
Kiyoi H, Naoe T, Nakano Y, Yokota S, Minami S, Miyawaki S, et al. Prognostic implication of FLT3 and N-RAS gene mutations in acute myeloid leukemia. Blood. 1999;93:3074–80.
Gilliland DG, Griffin JD. The roles of FLT3 in hematopoiesis and leukemia. Blood. 2002;100:1532–42.
Kihara R, Nagata Y, Kiyoi H, Kato T, Yamamoto E, Suzuki K, et al. Comprehensive analysis of genetic alterations and their prognostic impacts in adult acute myeloid leukemia patients. Leukemia. 2014;28:1586–95.
Levis M. FLT3 mutations in acute myeloid leukemia: what is the best approach in 2013? Hematol Am Soc Hematol Educ Program. 2013;2013:220–6.
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–47.
Kottaridis PD, Gale RE, Frew ME, Harrison G, Langabeer SE, Belton AA, et al. The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood. 2001;98:1752–9.
Ravandi F, Kantarjian H, Faderl S, Garcia-Manero G, O’Brien S, Koller C, et al. Outcome of patients with FLT3-mutated acute myeloid leukemia in first relapse. Leuk Res. 2010;34:752–6.
Tallman MS. New strategies for the treatment of acute myeloid leukemia including antibodies and other novel agents. Hematology Am Soc Hematol Educ Program. 2005;2005:143–50.
Mori M, Kaneko N, Ueno Y, Yamada M, Tanaka R, Saito R, et al. Gilteritinib, a FLT3/AXL inhibitor, shows antileukemic activity in mouse models of FLT3 mutated acute myeloid leukemia. Invest New Drugs. 2017;35:556–65.
Zarrinkar PP, Gunawardane RN, Cramer MD, Gardner MF, Brigham D, Belli B, et al. AC220 is a uniquely potent and selective inhibitor of FLT3 for the treatment of acute myeloid leukemia (AML). Blood. 2009;114:2984–92.
Cortes JE, Kantarjian H, Foran JM, Ghirdaladze D, Zodelava M, Borthakur G, et al. Phase I study of quizartinib administered daily to patients with relapsed or refractory acute myeloid leukemia irrespective of FMS-like tyrosine kinase 3-internal tandem duplication status. J Clin Oncol. 2013;31:3681–7.
Cortes J, Perl AE, Döhner H, Kantarjian H, Martinelli G, Kovacsovics T, et al. Quizartinib, an FLT3 inhibitor, as monotherapy in patients with relapsed or refractory acute myeloid leukaemia: an open-label, multicentre, single-arm, phase 2 trial. Lancet Oncol. 2018;19:889–903.
Cortes JE, Tallman MS, Schiller GJ, Trone D, Gammon G, Goldberg SL, et al. Phase 2b study of 2 dosing regimens of quizartinib monotherapy in FLT3-ITD-mutated, relapsed or refractory AML. Blood. 2018;132:598–607.
Cortes J, Khaled S, Martinelli G, Perl A, Ganguly S, Russell N, et al. Quizartinib versus salvage chemotherapy in relapsed or refractory FLT3-ITD acute myeloid leukaemia (QuANTUM-R): a multicentre, randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2019;20:984–97.
Phase 1 Study of Quizartinib [Available at:https://www.clinicaltrials.gov/ct2/show/NCT02675478] Accessed August 21, 2018.
Mander AP, Thompson SG. Two-stage designs optimal under the alternative hypothesis for phase II cancer clinical trials. Contemp Clin Trials. 2010;31:572–8.
Act on Securing Quality, Efficacy and Safety of Pharmaceuticals, Medical Devices, Regenerative and Cellular Therapy Products, Gene Therapy Products, and Cosmetics No. 1. Ordinance No. 28 (27 Mar 1997) Ministry of Health, Labour and Welfare, Japan; 1997 [Available at: https://www.pmda.go.jp/files/000152996.pdf] Accessed November 8, 2018.
Ethical Guidelines for Human Genome/Gene Analysis Research (established on 29 Mar 2001, fully rev. on 28 Dec 2004, partially rev. on 29 Jun 2005, partially rev. on 1 Dec 2008, fully rev. on 8 Feb 2013). Ministry of Education, Culture, Sports, Science and Technology; Ministry of Health, Labour and Welfare; Ministry of Economy, Trade and Industry; Japan; 2001 [Available at: http://www.lifescience.mext.go.jp/files/pdf/n796_00.pdf] Accessed November 8, 2018.
Ethical Guidelines for Clinical Studies (established on 30 Jul 2003, fully rev. on 28 Dec 2004, fully rev. on 31 Jul 2008): Ministry of Health, Labour and Welfare, Japan; 2003 [Available at: https://www.mhlw.go.jp/general/seido/kousei/i-kenkyu/rinsyo/dl/shishin.pdf] Accessed November 8, 2018 [In Japanese].
Cheson BD, Bennett JM, Kopecky KJ, Buchner T, Willman CL, Estey EH, et al. Revised recommendations of the International Working Group for diagnosis, standardization of response criteria, treatment outcomes, and reporting standards for therapeutic trials in acute myeloid leukemia. J Clin Oncol. 2003;21:4642–9.
Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0: Japan Clinical Tumor Research Group; 2009 [Available at: http://www.jcog.jp/doctor/tool/CTCAEv4J_20130409.pdf] Accessed November 8, 2018.
Agarwal SK, Mangal N, Menon RM, Freise KJ, Salem AH. Response rates as predictors of overall survival: a meta-analysis of acute myeloid leukemia trials. J Cancer. 2017;8:1562–7.
Shah SS, Kantarjian HM, Ravandi F, O’Brien S, Garcia-Manero G, Andreeff M, et al. Survival outcomes in relapsed/refractory acute myeloid leukemia patients who achieve less-than-complete response after salvage therapy. Blood. 2013;122:2654.
Forman SJ, Rowe JM. The myth of the second remission of acute leukemia in the adult. Blood. 2013;121:1077–82.
Acknowledgements
The main data of this manuscript were previously presented at the 80th Annual Meeting of the Japanese Society of Hematology (October 12–14, 2018, Osaka, Japan). This study was sponsored by Daiichi Sankyo Co., Ltd. Medical writing and editorial assistance was provided by Dr. Deepali Garg, MBBS, PGDHA, of Cactus Communications and was funded by Daiichi Sankyo Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KU has received honoraria and lecture fees from Novartis and research funding from Fujimoto, Astellas, Otsuka, Sumitomo Dainippon, Kyowa Hakko Kirin, GlaxoSmithKline, Sanofi, Shire, SymBio, Celgene, Daiichi Sankyo, Boehringer Ingelheim, Pfizer, and Janssen, and speakers bureau from Novartis, Ono, Takeda, Chugai, Nippon Shinyaku, Mochida, MSD, Celgene, Sumitomo Dainippon, and Pfizer. MM, SO, and TTg are employees of Daiichi Sankyo. SS was an employee of Daiichi Sankyo at the time of this study. TT, KM, HO, TS, and RI have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12185_2019_2727_MOESM1_ESM.tif
Supplementary Fig. 1 Kaplan–Meier curve for event-free survival (efficacy analysis set). Patients without a documented best response of CRc were excluded from the analyses. CIs were calculated based on the method proposed by Brookmeyer and Crowley. CI, confidence interval; CRc, composite complete remission; EFS, event-free survival (TIFF 695 kb)
12185_2019_2727_MOESM2_ESM.tif
Supplementary Fig. 2 Kaplan–Meier curve for leukemia-free survival (efficacy analysis set). The analyses for LFS were conditional on the patients having a documented best response of CRc. Patients without a documented best response of CRc were excluded from the analyses. CIs were calculated based on the method proposed by Brookmeyer and Crowley. CI, confidence interval; CRc, composite complete remission; NE, not evaluated; LFS, leukemia-free survival (TIFF 662 kb)
About this article
Cite this article
Takahashi, T., Usuki, K., Matsue, K. et al. Efficacy and safety of quizartinib in Japanese patients with FLT3-ITD positive relapsed or refractory acute myeloid leukemia in an open-label, phase 2 study. Int J Hematol 110, 665–674 (2019). https://doi.org/10.1007/s12185-019-02727-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-019-02727-6