Abstract
Clinical demand for the prompt assessment of the activity of direct-acting factor Xa inhibitors in the emergency care setting is increasing. In the present study, we examined whether prothrombin time (PT) tests can serve as a clinically useful indicator of anti-factor Xa activity. In the first series, the in vitro effect of edoxaban on PT was evaluated by spiking human plasma with edoxaban and measuring PT using three different commercial PT tests. In the second series, the reversal effect of prothrombin complex concentrates (PCC) and activated PCC (aPCC) in edoxaban-spiked plasma was evaluated. In the third series, PT of plasma samples from patients administered either 15 or 30 mg/day of edoxaban was assessed, and the results were compared with edoxaban concentrations determined by a calibrated anti-factor Xa activity assay. The spike test revealed that all PT reagents positively correlated with edoxaban. The sensitivity to edoxaban varied among the three reagents and Triniclot® Excel S showed the best performance. Prolonged PT by edoxaban was reversed by PCC and aPCC in a dose-dependent manner; however, complete reversal was not achieved. Positive correlation between anti-factor Xa activity and PT was shown in the clinical samples at the edoxaban range from 0 to >300 ng/mL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The direct oral anticoagulants (DOACs) have become popular in the prophylaxis and treatment of venous and arterial thromboembolism. They are usually administered without any monitoring and have proved to be effective and safe [1, 2]. However, accumulating evidence suggests that dose adjustment based on laboratory testing would be helpful in guiding clinicians in the prevention of severe hemorrhage and thrombotic events, especially in patients who are elderly, have low body weight, and in those with chronic renal insufficiency [3]. In those conditions, the plasma concentration of DOACs can be measured by high-performance liquid chromatography [4]; however, it is expensive and time-consuming. Hence, measurement of anticoagulant activity by clotting tests is warranted, and for certain DOACs such as rivaroxaban and apixaban, this may be achieved by the measurement of anti-factor Xa activity or prothrombin time (PT) test [5]. Theoretically, the direct measurement of anti-factor Xa activity is superior to PT [6, 7], but it cannot be done in every local laboratory at any time. Thus, the PT test is preferable if it is permissibly accurate for the practical use.
Edoxaban is a newly developed direct anti-factor Xa inhibitor widely used for venous thromboembolism prevention following total knee and hip arthroplasty, stroke prevention in non-valvular atrial fibrillation, and treatment and recurrence prevention of venous thromboembolism (VTE) [deep vein thrombosis (DVT) and pulmonary thromboembolism (PE)] in Japan. Its efficacy and safety have already been proved in large-scale randomized controlled trials [8, 9], and the incidence of serious bleeding is reported to be 2.75 %/year when administered at 60 mg/day [8]. It has been also reported that proper dosing decreases fatal events [10]. Similar to the other DOACs, edoxaban is readily absorbed from the intestines, and its activity peaks at 1–3 h [11]. Since little information regarding the monitoring of edoxaban is available, the primary objective of this study was to examine whether its anticoagulant activity can be properly evaluated by PT test. In addition, since the suitability of the PT test is different depending on each DOAC, the second aim was to find the most suitable PT test for edoxaban. Furthermore, we also examined whether the PT tests can monitor the effects of reversal agents. Bleeding tends to become more serious with the use of DOACs, and a reversal agent should be applied properly when patients require urgent hemostasis [12]. Thus, a further purpose of this study was to examine whether PT tests reflect the reversal effects of the 4-factor prothrombin complex concentrates (PCC) [13] and activated prothrombin complex concentrates (aPCC) [14].
Materials and methods
Spike test
Pooled citrated normal human plasma was spiked with edoxaban at increasing concentrations to assess its impact in three kinds of PT tests. Edoxaban was kindly donated by Daiichi Sankyo Co., Ltd. (Tokyo, Japan). Working solutions of 0, 50, 100, 300 and 500 ng/mL of edoxaban were obtained from the stock solution at a dose of 1.0 mg/DMSO 1.0 mL by mixing with pooled citrated normal human platelet-poor plasma.
PT test
PT was measured by the following method: 50 μL of plasma samples were incubated at 37 °C up to 60 s and mixed with 100 μL of calcium and thromboplastin. The different thromboplastin reagents used were Triniclot® PT Excel S (trade name in Japan: Shinplastin® Excel S, Kyowa Medex, Tokyo, Japan), Thromborel® S (Dade Behring, Newark, USA.) and Neoplastin® R (Diagnostica Stago, Asnieres, France). Clotting time was measured on Coapresta® 2000 (Sekisui Medical, Tokyo, Japan) for all PT kits.
Reversal effect of PCC and a PCC
After edoxaban was incubated at final concentrations of 0, 100, 300 or 500, 700 and 1000 ng/mL with the pooled plasma for 15 min, either PCC (PPSB-HT®, Nihon Pharmaceutical Co. Ltd, Tokyo, Japan) or aPCC (FEIBA®, Baxter, Vienna, Austria) was added at concentrations of 0, 0.5, 1.0, 1.5 or 3.0 U/mL, and these aliquots were incubated at 37 °C. After 15 min of incubation, PT was measured by three PT tests.
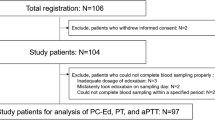
Clinical sample collection
A total of 144 samples were collected from the patients who had been undergone total knee arthroplasty in Juntendo Hospital. All the patients were treated with intermittent pneumatic compression for DVT prophylaxis beginning immediately after the operation. The patients received either 15 or 30 mg of edoxaban (71 cases received 15 mg and 73 cases received 30 mg) once daily for 14 days beginning 24 h after the end of lumbar anesthesia. The blood samples were drawn at various timing after edoxaban intake. Patients with severe renal dysfunction (Ccr <30 mL/min) or bleeding tendency were excluded. The protocol was approved by the Human Ethics Review Committee of the Juntendo University (#26-311) and a signed consent form was obtained from each patient.
Chromogenic anti-factor Xa assay
The plasma levels of edoxaban in the clinical samples were calculated from its anti-factor Xa activity by chromogenic assay. The chromogenic anti-factor Xa assay is based on the inhibitory action of edoxaban on factor Xa, which specifically cleaves para-nitroaniline (p-NA) linked to a chromogenic peptide. Increasing edoxaban concentrations inhibit the activity of factor Xa on the chromogenic peptide, thereby increasing the release of p-NA. The above anti-Xa activity assay was performed using STA-Liquid Anti-Xa (Roche Diagnostics, Japan), S-2222 (Sekisui Medical, Tokyo, Japan) and Coapresta 2000 (CP2000, Sekisui Medical) and the concentration of edoxaban is plotted against the optical density (OD) of released p-NA [15]. A standard curve was made for the lyophilized normal plasma using spiked concentrations of edoxaban.
Statistical analysis
Statistical analysis was performed using the STATVIEW® program (Abacus Concepts, Berkeley, CA, USA). Pearson product-moment correlation coefficient was used to correlate the distribution of PT values between the PT reagents. Overall statistical significance among serial measurements was analyzed by repeated measures ANOVA, followed by an individual comparison by paired t test as appropriate. P < 0.05 was considered statistically significant.
Results
Spike test
The spike test was repeated three times and the similar results were obtained. The summarized result of three independent experiments is depicted in Fig. 1. A concentration-dependent prolongation of PT was found at edoxaban concentrations from 0 to 500 ng/mL. The relationship between PT and edoxaban concentration was almost linear for each PT test at the range of 14.0–35.1 s, r = 0.99 (Triniclot® PT Excel S); 11.7–20.0 s, r = 0.99 (Thromborel® S); and 13.5–29.4 s, r = 0.99 (Neoplastin® R). The slopes of correlations between concentrations of edoxaban and PT were greatest in Triniclot® PT Excel S followed by Neoplastin® R and Thromborel® S (Table 1). PT ratios at a therapeutic plasma edoxaban concentration of 300 ng/mL were 1.9 ± 0.0 (Triniclot® PT Excel S), 1.2 ± 0.0 (Thromborel® S) and 1.4 ± 0.0 (Neoplastin® R), indicating that the magnitude of responses to edoxaban was greatest with Triniclot® PT Excel S (P < 0.01).
Impact of edoxaban on prothrombin time (PT). Edoxaban prolonged PT concentration-dependently. The relationship was almost linear and the magnitude of responses to edoxaban was depended on the thromboplastin reagent. The response ranged from 0 to 500 ng/mL and Triniclot® PT Excel S showed the greatest response. Solid line, mean; dotted line, 95 % confidence interval. Filled circle: Triniclot® PT Excel S (blue), filled square: Thromborel® S (green), filled upright triangle: Neoplastin® R (yellow)
Reversal effect by PCC
The reversal effect of PCC was examined three times for each PT test and the representative result was shown in Fig. 2. Significant prolongation of PT was observed in the samples pre-incubated with edoxaban from 0 to 1000 ng/mL without PCC. When PCC 0.5 U/mL was added to the 1000 ng/mL of edoxaban-spiked samples, PT decreased most prominently with Triniclot® PT Excel S, and PT reduced to approximately 75 % of that of the original level (0 U/mL). In cases of Thromborel® S and Neoplastin® R, PT decreased in a dose-dependent manner, while the decrease of PT reached plateau when PCC dose was 1.5 U/mL or more in Triniclot® PT Excel S. When edoxaban dose was 300 ng/mL, PT decreased to within the reference value in Thromborel® S (9.8–12.1 s) and Neoplastin® R (13.0–17.0 s) by the administration of 1.5 U/mL of PCC, while PT sustained above the reference value in Triniclot® PT Excel S (12.7–15.2 s).
Impact of prothrombin complex concentrates (PCC) on prothrombin time (PT). Concentration-dependent decrease of PT was recognized after PCC administration. In cases of Thromborel® S and Neoplastin® R, PCC added to the plasma samples that had been spiked with edoxaban showed the decrease of PT in a dose-dependent manner. While in case of Triniclot® PT Excel S, the reached plateau at the PCC concentration of 1.5 U/mL. Data shown is from one experiment, which is representative of the data from three independently performed experiments
Reversal effect by aPCC
The examination for the reversal effect of aPCC was also repeated three times for each PT test and the representative result was shown in Fig. 3. Similar to PCC, PT was prolonged greatest in Triniclot® PT Excel S and 0.63 U/mL of aPCC reduced PT to approximately 64 % of that of the original level. With respect to the reduction rate, the decrease was greatest in Neoplastin® R and 0.63 U/mL of aPCC reduced PT to approximately 54 % of the original level. Regarding the plateau phenomenon, all three PT tests demonstrated similar trends. PT decreased in a dose-dependent manner when aPCC dose was between 0.63 and 2.5, and 5.0 U/mL showed limited additional effects. When edoxaban dose was the therapeutic level (300 ng/mL), 1.25 U/mL of aPCC reduced PT to the normal range in Thromborel® S and Neoplastin® R, while the level was above the reference value in Triniclot® PT Excel S.
Impact of activated prothrombin complex concentrates (aPCC) on prothrombin time (PT). Concentration-dependent decrease of PT was recognized after aPCC administration. When 0.5, 1.0 or 1.5 U/mL of aPCC was added to the plasma samples that had been spiked with edoxaban, each PT test showed the decrease of PT in a dose-dependent manner. However, further addition of aPCC did not result in the complete correction of PT. Data shown is from one experiment, which is representative of the data from three independently performed experiments
Clinical samples
In the clinical samples, edoxaban doses calculated by chromogenic anti-factor Xa assay were distributed between the range of 0 and 366.9 ng/mL. In the same samples, PT was significantly prolonged and distributed in a large range: Triniclot® PT Excel S; 11.6–37.4 s, PT = 0.37 × anti-factor Xa activity + 14.96, r = 0.72: Thromborel® S; 11.8–30.2 s, PT = 0.16 × anti-factor Xa activity + 14.88, r = 0.52: Neoplastin® R; 15.0–49.1 s, PT = 0.33 × anti-factor Xa activity + 18.39, r = 0.60. As is shown in Fig. 4, edoxaban resulted in an increase in PT in a dose-dependent manner and the reactivity was highest with Triniclot® PT Excel S.
Relationship between anti-factor Xa activity and prothrombin time (PT). Anti-factor Xa activity dependent increase of PT was recognized in the patients received edoxaban after the orthopedic surgery (n = 144). Among the PT tests, Triniclot PT Excel S® showed the highest reactivity and good relationship (y = 0.37x + 14.96, r = 0.72). Thromborel S: y = PT = 0.16x + 14.88, r = 0.52. Neoplastin R: y = 0.33x + 18.39, r = 0.60
Discussion
The management of critical bleeding during treatment with DOACs is an urgent matter. Obviously, it would be helpful to have a real-time monitoring method [13]. The development of antidotes that neutralizes the activity of various DOACs is currently underway [16, 17], and the effect of PER977, a synthetic reversal agent, has been reported to be most effective for edoxaban among DOACs [18]. Once the specific reversal agents become available, the importance of monitoring will increase for the appropriate use of these expensive agents. Under these circumstances, we planned to evaluate the suitability of commercially available PT tests to measure the anticoagulant activity of edoxaban. The usefulness of PT tests was examined in the former studies [19], but most of the studies were performed using spiked normal plasma or plasma samples from healthy volunteers and the results are inconsistent [20, 21]. To the best of our knowledge, this is the first report to describe the distribution of PT values in post-surgical patients receiving edoxaban. In addition, since many of the PT reagents have been replaced to the new reagents; for example, Triniclot® PT Excel was replaced to Excel S and Neoplastin® Plus was replaced to Neoplastin® R, we have to update the references. In this study, we compared the performance of three popular PT reagents currently available in Japan.
Chromogenic anti-Xa assay has already been evaluated as more accurate assay for the measurement of DOACs [22–24]; however, it is still not popular as an emergency test. In contrast, the PT test is broadly used for the monitoring of vitamin K antagonist in the local laboratories. However, the validity of PT tests for DOACs monitoring is not consistent. In the current study, edoxaban prolonged PT values in a concentration-dependent manner in both of spike-in and clinical samples. In addition, there was a good linear correlation in PT values between the three reagents (r = 0.99) in spiked-in samples. In the clinical samples, the correlation of PT and anti-Xa activity was not as high as the spiked-in samples probably because PT was affected by the surgery. The phenomenon that the extension of PT was seen in some samples at the time when blood concentrations of edoxaban were considerably low (or zero) further supports this idea. In addition, there are two subjects who showed significantly high prothrombin time comparing their anti-Xa activities. Those cases did not complicate liver dysfunction. They did not intake vitamin K antagonists, and we could not find any other possible reasons for the PT prolongation.
The sufficient reactivity was not achieved in all DOACs. Douxfils et al. [25] reported that PT tests were not sensitive enough to evaluate the activity of apixaban. The same group also recommended not using PT tests for the monitoring of rivaroxaban [26]. To understand these conflicting results, we have to realize that the reactivity of PT tests differ widely between the reagents. Kanemoto et al. [27] reported that Triniclot® PT Excel S showed PT prolongation by 1.1 to 2.0-fold with the use of apixaban 50–500 ng/mL and others [28] reported Triniclot® PT Excel S was one of the most sensitive for rivaroxaban. These results suggested that the matched combination of DOAC and PT test is the key for effective monitoring. In the current study, our data demonstrated that Triniclot® PT Excel S will be most suitable for the monitoring of edoxaban activity in the daily practice.
Although DOACs are rapidly cleared with minimal accumulation [29], strategies for reversing its anticoagulant activity are still required for managing critical bleeding such as intracerebral bleeding in the emergency care setting. Currently, PCC and aPCC are the choices for this situation [30], and PPSB-HT® and FEIBA® are available in Japan. PPSB-HT® contains inactive factor II, IX, X and VIIa and FEIBA® contains activated factors II, VII, IX, and X [14]. American Heart Association guidelines on management of spontaneous intracerebral hemorrhage suggest the use of PCC or aPCC as a potential reversal agent [31]. The study that evaluated the reversal effect of PCC and aPCC by PT was still rare, but Fukuda et al. [32] demonstrated the similar result as ours. However, correlation between the clinical reversal effect and PT is still lacking and no consensus has been reached regarding PCC and aPCC use of dosing [33]. Our results indicated that PCC and aPCC concentration-dependently shortened PT prolonged by edoxaban, but PT never recovered to the normal range if the concentration of edoxaban in plasma is high. It is important for the clinicians to remind this phenomenon to avoid the overdose of PCC and aPCC when they use PT as an indicator.
As for the in vivo study, Herzog et al. [34] revealed that PCC effectively reversed both edoxaban-induced hemorrhaging and the prolongation of PT in a dose-dependent manner by using a rabbit bleeding model; however, the standard method of PCC use has not been clinically established. Our results suggested that the monitoring by PT test might become the guidance for the use of PCC and aPCC. For example, edoxaban 300 ng/mL prolonged PT to 30 s, which is achieved by a single oral dose of edoxaban 60 mg [28], and it was reversed to 20 s by 1.5 U/mL of PCC or 1.25 U/mL of aPCC. At the supra-therapeutic concentrations of edoxaban, similar results were recognized.
In summary, we think the anticoagulant effect of edoxaban can be evaluated at least partially by measuring PT, and the reactivity is different depending on the reagents. The reversal effects of PCC and aPCC can also be evaluated by PT tests. However, the usefulness of monitoring with PT should be clinically evaluated in the future study.
Finally, there are some limitations in this study. First, we examined only a limited numbers of PT tests. Since considerable differences in reactivity between the tests exist, it is important to check the reactivity of each PT test for the target DOAC. Second, edoxaban doses in the clinical samples were limited to 15 and 30 mg. Since the recommended dose for the stroke prevention in non-valvular atrial fibrillation is 60 mg/day [35], the performance of PT tests should be examined in the samples from the patients who take this dose of edoxaban in the next step. Third, the reversal effects were also examined only in spiked-in samples. The evaluation for PT tests on the reversal effects should also be confirmed in the clinical samples.
Conclusion
PT tests are appropriate assays to measure pharmacodynamic effects of edoxaban in the emergency setting. However, a large variability among different PT reagents should be considered. The reversal effects of PCC and aPCC could also be evaluated by PT tests. It is therefore suggested that PCC and aPCC could better be used for emergency reversal of DOACs under the monitoring by PT tests.
References
Lip GY, Lane DA. Stroke prevention in atrial fibrillation: a systematic review. JAMA. 2015;313:1950–62.
Ghanny S, Crowther M. Treatment with novel oral anticoagulants: indications, efficacy and risks. Curr Opin Hematol. 2013;20:430–6.
Pengo V, Crippa L, Falanga A, Finazzi G, Marongiu F, Palareti G, et al. Questions and answers on the use of dabigatran and perspectives on the use of other new oral anticoagulants in patients with atrial fibrillation. A consensus document of the Italian Federation of Thrombosis Centers (FCSA). Thromb Haemost. 2011;106:868–76.
Rohde G. Determination of rivaroxaban–a novel, oral, direct Factor Xa inhibitor–in human plasma by high-performance liquid chromatography-tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci. 2008;872:43–50.
Tripodi A. Which test to use to measure the anticoagulant effect of rivaroxaban: the prothrombin time test. J Thromb Haemost. 2013;11:576–8.
Harenberg J, Krämer R, Giese C, Marx S, Weiss C, Wehling M. Determination of rivaroxaban by different factor Xa specific chromogenic substrate assays: reduction of interassay variability. J Thromb Thrombolysis. 2011;32:267–71.
Samama MM, Amiral J, Guinet C, Le Flem L, Seghatchian J. Monitoring plasma levels of factor Xa inhibitors: how, why and when? Expert Rev Hematol. 2013;6:155–64.
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–104.
Büller HR, Décousus H, Grosso MA, Mercuri M, Middeldorp S, Prins MH, et al. Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med. 2013;369:1406–15.
Ruff CT, Giugliano RP, Braunwald E, Morrow DA, Murphy SA, Kuder JF, et al. Association between edoxaban dose, concentration, anti-Factor Xa activity, and outcomes: an analysis of data from the randomised, double-blind ENGAGE AF-TIMI 48 trial. Lancet. 2015;385:2288–95.
Yin OQ, Miller R. Population pharmacokinetics and dose-exposure proportionality of edoxaban in healthy volunteers. Clin Drug Investig. 2014;34:743–52.
Bauer KA. Targeted anti-anticoagulants. N Engl J Med. 2015;373:569–71.
Pernod G, Albaladejo P, Godier A, Samama CM, Susen S, Gruel Y, et al. Management of major bleeding complications and emergency surgery in patients on long-term treatment with direct oral anticoagulants, thrombin or factor-Xa inhibitors: proposals of the working group on perioperative haemostasis (GIHP)—March 2013. Arch Cardiovasc Dis. 2013;106:382–93.
Turecek PL, Va´radi K, Gritsch H, Schwarz HP. FEIBA: mode of action. Haemophilia. 2004;10(Suppl 2):3–9.
Harenberg J, Krämer R, Giese C, Marx S, Weiss C, Wehling M. Determination of rivaroxaban by different factor Xa specific chromogenic substrate assays: reduction of interassay variability. J Thromb Thrombolysis. 2011;32:267–71.
Crowther M, Crowther MA. Antidotes for novel oral anticoagulants: current status and future potential. Arterioscler Thromb Vasc Biol. 2015;35:1736–45.
Siegal DM, Curnutte JT, Connolly SJ, Lu G, Conley PB, Wiens BL, et al. Andexanet alfa for the reversal of factor Xa inhibitor activity. N Engl J Med. 2015;373:2413–24.
Ansell JE, Bakhru SH, Laulicht BE, Steiner SS, Grosso M, Brown K, et al. Use of PER977 to reverse the anticoagulant effect of edoxaban. N Engl J Med. 2014;371:2141–2.
Cuker A, Husseinzadeh H. Laboratory measurement of the anticoagulant activity of edoxaban: a systematic review. J Thromb Thrombolysis. 2015;39:288–94.
Morishima Y, Kamisato C. Laboratory measurements of the oral direct factor Xa inhibitor edoxaban: comparison of prothrombin time, activated partial thromboplastin time, and thrombin generation assay. Am J Clin Pathol. 2015;143:241–7.
Samama MM, Mendell J, Guinet C, Le Flem L, Kunitada S. In vitro study of the anticoagulant effects of edoxaban and its effect on thrombin generation in comparison to fondaparinux. Thromb Res. 2012;129:e77–82.
Becker RC, Yang H, Barrett Y, Mohan P, Wang J, Wallentin L, Alexander JH. Chromogenic laboratory assays to measure the factor Xa-inhibiting properties of apixaban–an oral, direct and selective factor Xa inhibitor. J Thromb Thrombolysis. 2011;32:183–7.
Barrett YC, Wang Z, Frost C, Shenker A. Clinical laboratory measurement of direct factor Xa inhibitors: anti-Xa assay is preferable to prothrombin time assay. Thromb Haemost. 2010;104:1263–71.
Yuri M, Tabe M, Tsuchiya K, Sadatsuki R, Aoki J, Horii T, et al. Evaluation of factor Xa-specific chromogenic substrate assays and the determination of pharmacokinetics of fondaparinux. Clin Appl Thromb Hemost. 2015;pii:1076029615595878.
Douxfils J, Chatelain C, Chatelain B, Dogné JM, Mullier F. Impact of apixaban on routine and specific coagulation assays: a practical laboratory guide. Thromb Haemost. 2013;110:283–94.
Douxfils J, Tamigniau A, Chatelain B, Chatelain C, Wallemacq P, Dogné JM, Mullier F. Comparison of calibrated chromogenic anti-Xa assay and PT tests with LC-MS/MS for the therapeutic monitoring of patients treated with rivaroxaban. Thromb Haemost. 2013;110:723–31.
Kanemoto M, Kuhara H, Ueda T, Shinohara T, Oda T, Nakao F, et al. Association of apixaban therapy and prothrombin time in patients with atrial fibrillation. Circ J. 2014;78:2651–6.
Douxfils J, Mullier F, Loosen C, Chatelain C, Chatelain B, Dogné JM. Assessment of the impact of rivaroxaban on coagulation assays: laboratory recommendations for the monitoring of rivaroxaban and review of the literature. Thromb Res. 2012;130:956–66.
Ogata K, Mendell-Harary J, Tachibana M, Masumoto H, Oguma T, Kojima M, et al. Clinical safety, tolerability, pharmacokinetics, and pharmacodynamics of the novel factor Xa inhibitor edoxaban in healthy volunteers. J Clin Pharmacol. 2010;50:743–53.
Majeed A, Schulman S. Bleeding and antidotes in new oral anticoagulants. Best Pract Res Clin Haematol. 2013;26:191–202.
Hemphill JC III, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:2032–60.
Fukuda T, Honda Y, Kamisato C, Morishima Y, Shibano T. Reversal of anticoagulant effects of edoxaban, an oral, direct factor Xa inhibitor, with haemostatic agents. Thromb Haemost. 2012;107:253–9.
Silvain J, Hauguel M, Kerneis M, Collet JP, Montalescot G. Measuring and reversing the effect of non-vitamin K antagonist oral anticoagulants (NOACs). Circ J. 2015;79:289–91.
Herzog E, Kaspereit F, Krege W, Doerr B, Mueller-Cohrs J, Pragst I, et al. Effective reversal of edoxaban-associated bleeding with four-factor prothrombin complex concentrate in a rabbit model of acute hemorrhage. Anesthesiology. 2015;122:387–98.
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–104.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Emmi M. works for Kyowa Medex Co. Ltd. The other authors state that they have no conflict of interests.
About this article
Cite this article
Iba, T., Emmi, M., Hiki, M. et al. Comparison of prothrombin time tests used in the monitoring of edoxaban and their evaluation as indicators of the reversal effect. Int J Hematol 103, 665–672 (2016). https://doi.org/10.1007/s12185-016-1975-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-016-1975-5