Abstract
In this phase I dose-escalation study we evaluated the safety, tolerability, pharmacokinetics, and antitumor activity of ibrutinib, an oral covalent inhibitor of Bruton’s tyrosine kinase (BTK, in Japanese patients with relapsed/refractory B cell malignancies (RRBCM). Fifteen patients aged 42–78 years were enrolled to one of three cohorts. Cohort 1 (n = 3) consisted of two phases, a single-dose (140 and 280 mg) phase and a multiple-dose (420 mg) phase of ibrutinib; cohort 2 (n = 6) included multiple doses of ibrutinib 560 mg; and cohort 3 (n = 6) included only patients with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) dosed at ibrutinib 420 mg. One patient (CLL/SLL cohort) experienced grade 3 pneumonia and sepsis, which were considered dose-limiting toxicities. No deaths were reported. The most common (≥ 20 % patients) adverse events were neutropenia, anemia, nasopharyngitis, increased bilirubin, and rash. Dose-dependent increase in maximum plasma concentration and area under the concentration from 0 to the last quantifiable time was observed, while time to reach maximum plasma concentration and elimination half-life was similar between doses. The overall response rate was 73.3 % (11/15) for all cohorts combined. Overall, ibrutinib (420 and 560 mg) was tolerable with acceptable safety profiles and effective for Japanese patients with RRBCM including CLL/SLL. Clinical trial registration: NCT01704963.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-Hodgkin lymphoma (NHL) is one of the most common malignancies worldwide, estimated with 356,000 new cases and 192,000 deaths (2008) [1]. Mature B cell malignancies account for more than 85 % of NHL worldwide [2]. In Japan, it was reported that 70 % of malignant lymphomas involve B cell, of which more than 90 % were classified as mature B cell malignancies [3]. Current treatment strategy for B cell malignancies involves mostly combination immunochemotherapy, and occasionally radiotherapy. Despite the recent advances in drug development (including rituximab [4], bendamustine [5], cladribine [6], fludarabine [7]), mortality rate remains high for relapsed/refractory B cell malignancies (RRBCM) in Japan.
Bruton’s tyrosine kinase (BTK) is an essential kinase in the B cell receptor (BCR) signaling pathway playing an important role in the pathogenesis of several B cell malignancies, including mantle-cell lymphoma (MCL), chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL), follicular lymphoma (FL) [8–10], and marginal zone lymphoma (MZL) [11] Subsequently, BTK is considered an important potential target in B cell malignancies. Ibrutinib, a novel oral covalent BTK inhibitor, has been approved for the treatment of MCL and CLL in the United States, Europe and several countries for the treatment of patients who have received at least one prior therapy [12]. Ibrutinib binds covalently to Cys-481 in the active-site of BTK with an IC50 of 0.5 nmol/L subsequently inhibiting BCR signaling which prevents proliferation and survival of malignant B cells [13]. The time to reach maximum plasma concentration (T max) of ibrutinib is 1–2 h and elimination half-life (T ½) is 4–8 h [9, 14–16]. Ibrutinib is almost exclusively metabolized by CYP3A4-mediated pathway and primarily excreted via feces [17].
Several clinical studies outside Japan have demonstrated high antitumor activities and acceptable safety profiles of ibrutinib (420–840 mg) in B cell malignancies, including CLL/SLL [9, 10, 14, 18]. In a phase 1, first-in-human study, preliminary antitumor activity and acceptable safety profiles of ibrutinib were observed across multiple B cell malignancies [14]. In another phase 1b/2 study, higher overall response rate (ORR, 71 %) was observed in patients with relapsed/refractory CLL/SLL [9].
This study was designed to confirm the safety profile of ibrutinib in Japanese patients with RRBCM. The primary objective of this phase 1 study was to evaluate the safety and tolerability of ibrutinib in Japanese patients with mature RRBCM who had received at least one prior therapy. Secondary objectives included the evaluation of pharmacokinetic (PK) profile of ibrutinib and its antitumor response.
Patients and methods
Study population
Japanese patients of age ≥ 20 years and body weight ≥ 40 kg with mature RRBCM (according to WHO classification 2008) including CLL/SLL, MCL and FL were eligible. Other key inclusion criteria were: measurable disease (for NHL bi-dimensional disease ≥ 2 cm diameter in at least one dimension and for CLL ≥ 5000 leukemic cells/mm3); failed ≥ 1 previous treatment and no standard therapy available; and an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1. Key exclusion criteria were: plasma cell neoplasm; diffuse large B cell lymphoma (DLBCL) including histologic transformation from low-grade B cell NHL and Richter’s transformation from CLL; received prior allogeneic hematopoietic stem cell transplantation; received immunotherapy, chemotherapy, radiotherapy or experimental therapy within 4 weeks. Major surgery within 4 weeks was also an exclusion criteria.
The study protocol was reviewed and approved by the Institutional Review Board of each participating center. The study was conducted in accordance with the Declaration of Helsinki, the International Conference on Harmonization Guidelines on Good Clinical Practice, and applicable local laws and regulatory requirements. Each patient provided written informed consent prior to study participation.
Study design
This was an open-label, phase 1, dose-escalation study, conducted at four sites in Japan, with 3 cohorts (cohort 1, cohort 2 and CLL/SLL cohort). The study was conducted from September 2012 and is currently ongoing; the data up to cut-off date (5 June 2014) are presented in this paper.
Cohort 1 was divided into two phases: single-dose phase and multiple-dose phase. In the single-dose phase, patients received ibrutinib 140 and 280 mg with a washout period of 72–168 h between dose levels. After a second washout period of 72–168 h, patients then entered the multiple-dose phase to receive 420 mg ibrutinib once-daily for 35 days during cycle 1 and for 28 days in subsequent cycles.
Cohort 2 was designed to enroll recurrent mature B cell neoplasms including CLL/SLL in order to investigate safety and tolerability of ibrutinib 560 mg. Patients received ibrutinib 560 mg once-daily for 35 days during cycle 1 and for 28 days in subsequent cycles. Enrollment in cohort 2 started after the tolerability was confirmed in cohort 1. Based on tolerability of ibrutinib 420 mg in cohort 1, protocol was amended to add a new cohort ‘CLL/SLL’ (cohort 3) which enrolled patients with only CLL/SLL in order to further investigate the safety and tolerability of ibrutinib in Japanese patients with relapsed/refractory CLL/SLL, wherein patients received once-daily ibrutinib 420 mg.
Patients received ibrutinib until disease progression, unacceptable toxicity, or based on investigator’s decision. If no disease progression occurred, a patient was followed for a maximum of 6 months after last study dose. Patients from cohort 1 who continued to receive 420 mg after cycle 1 were allowed to receive 560 mg after tolerability of 560 mg was confirmed in cohort 2. However, no dose escalation was allowed in the CLL/SLL cohort. Cohort 2 and CLL/SLL cohort were opened at the same time and based on investigators discretion patients with CLL/SLL were enrolled to either cohort 2 or CLL/SLL cohort. The doses were administered 30 min before meal or 2 h after meal.
Safety and tolerability
Tolerability was evaluated based on dose-limiting toxicities (DLTs) during single-dose phase and cycle 1 of multiple-dose phases for cohort 1 and cycle 1 for cohort 2 and CLL/SLL cohort. The dose was considered to be tolerable if the DLT occurred in 0 of 3 (<33 %) patients in cohort 1 or in ≤1 of 6 (<33 %) patients in cohort 2 and CLL/SLL cohort. If DLT occurred in ≥33 % but <50 % of patients in a cohort, three additional patients were to be enrolled, and if DLT occurred in ≥50 % of patients, it was considered intolerable. The DLTs were defined as follows: any grade ≥ 3 non-hematologic toxicity persisting despite receipt of a single course of standard outpatient symptomatic therapy, grade ≥ 3 QTc prolongation, grade 4 neutropenia (absolute neutrophil count < 500/μL), grade 4 thrombocytopenia (platelet count < 25,000/μL), or dose delay following toxicity for > 7 consecutive days.
Safety assessments included all patients who received at least one dose of ibrutinib. Safety was assessed based on AEs, laboratory tests, physical examination, vital signs, electrocardiograms (ECGs), performance status (ECOG scale) and corneal eye examination. Severity of AE information was graded using the common terminology criteria for adverse events (CTCAE; version 3.0). All AEs that were reported during the treatment period (including AEs that worsened since baseline) were included in the analysis and evaluated according to MedDRA (version 16.1).
Antitumor activity
All patients except those with CLL were evaluated for response according to the International Working Group Revised Response Criteria for Malignant Lymphoma [19]. CLL patients were evaluated according to the guidelines for the diagnosis and treatment of CLL [20]. The efficacy endpoints to assess antitumor activity were ORR, time to response (TTR), and duration of response (DOR).
Pharmacokinetic and pharmacodynamic assessments
For PK evaluation, blood samples (2 mL each) were collected before and after single doses of ibrutinib 140 and 280 mg (pre-dose and 30 min, 1, 2, 3, 4, 6, 10, and 24 h post-dose); whereas samples during the multiple-dose phase of cohort 1, cohort 2 and CLL/SLL cohort were collected (pre-dose and 30 min, 1, 2, 3, 4, 6, 10, and 24 h post-dose) on days 1 and 8, and pre-dose on days 15, 22, and 29 and frozen at −70 °C until it was transferred to the bioanalytical facility. Plasma samples were analyzed using the validated liquid chromatography-tandem mass spectroscopy method (lower limit of quantification [LLOQ], 0.5 ng/mL). Non-compartmental PK analysis was performed using Phoenix WinNonlin software version 6.3 (Pharsight Corp. Certara, L.P., St. Louis, MO). The maximum plasma concentration (C max), area under the concentration from 0 to the last quantifiable time (AUClast), AUC from 0 to infinite time (AUCinf), T max, and T ½ were calculated.
For pharmacodynamic analysis, venous blood samples (8.5 mL each) were collected in tubes containing acid citrate dextrose at various time points (cohort 1: 6 samples in single-dose phase, 18 samples during multiple-dose phase on days 1, 8, 15 and 29 during cycle 1 and on days 1 and 15 in cycles 3, 5, 7, 9 and 11; cohort 2 and CLL/SLL cohort: 18 samples on days 1, 8, 15 and 29 during cycle 1, and on days 1 and 15 during cycles 3, 5, 7, 9 and 11). The BTK active site drug occupancy was measured in peripheral blood mononuclear cells (PBMCs), using a Meso Scale Discovery assay at Janssen Research & Development US.
Results
A total of 15 patients, with a median age of 65 years (range 42–78 years), were enrolled. Of these patients, 10 (66.7 %) were men (Table 1); 4 (26.7 %) had an ECOG performance status of one; 10 (66.7 %) had received ≥3 anticancer treatments or regimens. The diagnosis included relapsed or refractory CLL/SLL (n = 11), relapsed MCL (n = 2), relapsed FL (n = 1), and relapsed mucosa-associated lymphoid tissue (MALT) lymphoma (n = 1). One patient with relapsed MCL (560 mg; cohort 2) had autologous peripheral blood stem cell transplantation (auto-PBSCT). No patient received prior radiotherapy. The duration of ibrutinib exposure during single-dose phase of cohort 1 ranged 14–15 days, and during multiple-dose phase the median (range) duration of exposure was—cohort 1: 19.70 (5.9 to 19.7) months; cohort 2: 16.23 (12.5 to 16.9) months; and CLL/SLL cohort: 9.01 (4.8 to 13.5) months. The study is still ongoing and the data obtained on completion of 6 cycles for the last patient from CLL/SLL cohort are presented here (data cut-off date).
Safety and tolerability
No DLTs were reported in either cohort 1 or cohort 2. One patient from CLL/SLL cohort (cohort 3) who received multiple doses of ibrutinib 420 mg/day developed DLTs. This patient experienced grade 2 decreased platelet count on day 2 that improved to grade 1 on day 8, grade 3 pneumonia (day 7) and grade 3 sepsis (day 7), where pneumonia and sepsis were considered as DLTs. Overall, these AEs resulted in dose reduction from 420 to 280 mg of ibrutinib and resolved subsequently.
No deaths were reported during this study. All 15 patients developed at least one AE. Seven serious AEs were reported in 3 of 15 patients (20 %): stomatitis (n = 1), decreased appetite, infection, pneumonia (2 times), and sepsis (n = 1), and lobar pneumonia (n = 1). Seven (46.7 %) patients experienced AEs of grade ≥ 3 severity that resolved subsequently except one, pneumonia (serious AE) (Table S1). The AEs in 5 (33.3 %) patients resulted in dose reduction or dose delay. The most common (≥ 20 % of patients) AEs included neutropenia (n = 8), anemia (n = 7), nasopharyngitis, increased bilirubin, and rash (n = 6 each) (Table 2). Hemorrhagic events were petechiae (n = 4, 26.7 %) and epistaxis (n = 3, 20.0 %), reported in 6 patients (40.0 %). None of these hemorrhagic events were of grade ≥ 3 severity. Additionally, there was no major or intracranial hemorrhage defined in the protocol as special interests.
Drug-related AEs reported (≥ 20 % of patients) were neutropenia (n = 8), anemia (n = 7), increased bilirubin (n = 6), leukopenia (n = 5), leukocytosis, diarrhea, petechiae, rash, decreased platelet count (n = 4 each), thrombocytopenia, dry skin, nasopharyngitis, fatigue, and stomatitis (n = 3 each). Of these, 7 patients experienced at least 1 drug-related AE of grade ≥ 3 severity (neutropenia, n = 3; stomatitis, increased amylase, pneumonia, infection, lobar pneumonia, and sepsis, n = 1 each).
At the cut-off date of this analysis, 13 patients still continued receiving ibrutinib treatment, whereas two patients had discontinued treatment. One patient from cohort 1 discontinued ibrutinib following progressive disease on day 192, and the other patient from CLL/SLL cohort discontinued ibrutinib due to unacceptable toxicity (stomatitis grade 3; hospitalization) on day 147. Individual immunoglobulin (IgA, IgG and IgM) values did not show a declining trend after ibrutinib administration (data not shown).
Antitumor activity
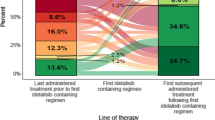
All 15 enrolled patients were evaluable for antitumor activity (Table 3). The overall response rate (complete response [CR] + partial response [PR]) was 73.3 % (95 % confidence interval [CI]: 44.9, 92.2) for all cohorts. Two of the 3 patients from cohort 1 had a PR as best response (CLL, SLL, n = 1 each); in cohort 2, 5 patients had PR as best response (SLL, n = 2; CLL, MCL, MALT lymphoma, n = 1 each). In CLL/SLL cohort, 3 patients each achieved PR (CLL, n = 2; SLL, n = 1) and stable disease. The ORR in patients with relapsed or refractory CLL/SLL who received 420 mg ibrutinib (n = 8) was 62.5 % (95 % CI: 24.5, 91.5) and best overall responses were PR (n = 5). The ORR in patients with relapsed or refractory CLL/SLL receiving 560 mg dose (n = 3) was 100 %. The median (range) TTR was 2.35 (1.9–11.2) months and DOR was 12.03 (5.7–17.7) months. All 14 patients who had the target lesions in the nodal sites at screening, showed ≥50 % reduction in the diameter, except one patient with relapsed/refractory FL (Fig. 1).
Pharmacokinetic and pharmacodynamic assessments
Plasma samples for PK analyses of ibrutinib were collected from all 15 enrolled patients. Ibrutinib was rapidly absorbed after single and multiple oral doses with a median T max of 1–3 h (Fig. 2). The mean T ½ after single- and multiple-dose ibrutinib ranged 4–9 h. The C max and AUClast increased with increasing dose (Table 4). The exposure did not differ by tumor subtype (data not shown).
The pharmacodynamic assessment showed about 90 % occupancy at 4 and 24 h in patients receiving ≥280 mg ibrutinib (Fig. 3). The sustained pharmacodynamic effect despite a relatively rapid elimination of ibrutinib from the circulation is consistent with an inhibition by irreversible binding of BTK in patients’ PBMCs (data not shown).
BTK occupancy following single- and multiple-dose of ibrutinib. BTK Bruton’s tyrosine kinase, CLL chronic lymphocytic leukemia, D day, FL follicular lymphoma, H hour, MALT mucosa associated lymphoid tissue lymphoma, MCL mantle-cell lymphoma, PD pre-dose, SD single-dose, SLL small lymphocytic lymphoma. Lines indicate the median percentage occupancy
Discussion
This phase 1 study with single (140 and 280 mg) and multiple (420 and 560 mg) doses of ibrutinib demonstrated that ibrutinib up to 560 mg was tolerable in Japanese patients with RRBCM. The multiple doses (420 and 560 mg) were chosen based on various approved dose levels in patients with CLL (420 mg) and in patients with MCL (560 mg) [9, 10, 12, 14, 18]. This was the first human study of ibrutinib conducted in Japan, therefore the protocol included evaluation of safety and tolerability of 140 and 280 mg (single doses) ibrutinib before administering higher (≥420 mg/day) or multiple doses.
DLTs were not reported in cohort 1 and 2 but were observed in one patient (grade 3 pneumonia and sepsis) in CLL/SLL cohort who received multiple doses of ibrutinib 420 mg. The most common (≥20 % patients) AEs reported were neutropenia, anemia, nasopharyngitis, increased bilirubin, rash, leukopenia, increased C-reactive protein, diarrhea and pyrexia, which were consistent with AEs reported in previous studies [9, 14, 18]. No deaths were reported during this study.
This exploratory study evaluated the antitumor activity of ibrutinib and demonstrated a positive response with a 73.3 % of ORR, which is consistent with a previous study in CLL [9]. The ORR in patients with relapsed/refractory CLL/SLL receiving 420 mg ibrutinib was 62.5 %, whereas it was 100 % in patients receiving 560 mg dose. Of 15 patients enrolled, 11 patients achieved objective responses (CR [n = 1] + PR [n = 10]) with a DOR of 5.7–17.7 months. In a previous study, ibrutinib when given in patients with MCL for a longer duration showed an increasing CR rate [10]. The median TTR across all cohorts was 2.35 months. Overall, these results indicate that the responses with ibrutinib therapy were rapid and durable, in this small population. Ibrutinib is being further investigated in other indications and subtypes, such as MCL, DLBCL and indolent B cell non-Hodgkin lymphoma.
The PK profile after single and multiple doses of ibrutinib was assessed. Dose-dependent increase was observed in C max and AUClast with considerable overlap between doses which is consistent with a previous study [16]. The T max and T ½ were similar between the dose levels. No difference in PK profile by tumor subtype was observed. The accumulation ratio was <1.6-fold suggesting minimal accumulation of ibrutinib after multiple doses. Overall, these PK results were consistent with the prior studies [14, 16], suggesting no relevant differences in the PK profiles between Japanese and non-Japanese patients with RRBCM. The pharmacodynamic evaluation determined that patients receiving ≥280 mg of ibrutinib achieved 90 % BTK occupancy at 4 and 24 h. However, patients receiving lower doses start losing full occupancy at 24 h, which is consistent with a previous report [14].
We acknowledge the limitation of a small sample size in our study. While the antitumor response of ibrutinib in Japanese patients may not be concluded, these preliminary results support the potential use of ibrutinib in patients with RRBCM. Studies with larger sample size are warranted to confirm these results.
In conclusion, this phase 1, dose-escalation study demonstrated that ibrutinib at 420 and 560 mg per day of ibrutinib was tolerable in Japanese patients with RRBCM who received at least one prior therapy. This preliminary data demonstrate an acceptable safety, PK profile of ibrutinib, with satisfactory ORR in Japanese patients with RRBCM including CLL/SLL. Further investigation is warranted.
References
Boffetta P. Epidemiology of adult non-Hodgkin lymphoma. Ann Oncol. 2011;22:iv27–iv31.
Ravandi F, O’Brien S. Chronic lymphoid leukemias other than chronic lymphocytic leukemia: diagnosis and treatment. Mayo Clin Proc. 2005;80:1660–74.
The World Health Organization classification of malignant lymphomas in Japan: incidence of recently recognized entities. Lymphoma Study Group of Japanese Pathologists. Pathol Int. 2000;50:696–702.
Tobinai K, Kobayashi Y, Narabayashi M, Ogura M, Kagami Y, Morishima Y, et al. Feasibility and pharmacokinetic study of a chimeric anti-CD20 monoclonal antibody (IDEC-C2B8, rituximab) in relapsed B-cell lymphoma. The IDEC-C2B8 Study Group. Ann Oncol. 1998;9:527–34.
Ohmachi K, Ando K, Ogura M, Uchida T, Itoh K, Kubota N, et al. Multicenter phase II study of bendamustine for relapsed or refractory indolent B-cell non-Hodgkin lymphoma and mantle cell lymphoma. Cancer Sci. 2010;101:2059–64.
Ogura M, Morishima Y, Kobayashi Y, Uike N, Sugai S, Chou T, et al. Durable response but prolonged cytopenia after cladribine treatment in relapsed patients with indolent non-Hodgkin’s lymphomas: results of a Japanese phase II study. Int J Hematol. 2004;80:267–77.
Tobinai K, Watanabe T, Ogura M, Morishima Y, Ogawa Y, Ishizawa K, et al. Phase II study of oral fludarabine phosphate in relapsed indolent B-cell non-Hodgkin’s lymphoma. J Clin Oncol. 2006;24:174–80.
Byrd JC, Brown JR, O’Brien S, Barrientos JC, Kay NE, Reddy NM, et al. Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med. 2014;371:213–23.
Byrd JC, Furman RR, Coutre SE, Flinn IW, Burger JA, Blum KA, et al. Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N Engl J Med. 2013;369:32–42.
Wang ML, Rule S, Martin P, Goy A, Auer R, Kahl BS, et al. Targeting BTK with ibrutinib in relapsed or refractory mantle-cell lymphoma. N Engl J Med. 2013;369:507–16.
Joshi M, Sheikh H, Abbi K, Long S, Sharma K, Tulchinsky M, et al. Marginal zone lymphoma: old, new, targeted, and epigenetic therapies. Ther Adv Hematol. 2012;3:275–90.
US Food and Drug Administration. Hematology/oncology (cancer) approvals & safety notifications. Available from: http://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm279174.htm (Accessed on 11 June 2015).
Honigberg LA, Smith AM, Sirisawad M, Verner E, Loury D, Chang B, et al. The Bruton tyrosine kinase inhibitor PCI-32765 blocks B-cell activation and is efficacious in models of autoimmune disease and B-cell malignancy. Proc Natl Acad Sci USA. 2010;107:13075–80.
Advani RH, Buggy JJ, Sharman JP, Smith SM, Boyd TE, Grant B, et al. Bruton tyrosine kinase inhibitor ibrutinib (PCI-32765) has significant activity in patients with relapsed/refractory B-cell malignancies. J Clin Oncol. 2013;31:88–94.
de Jong J, Sukbuntherng J, Skee D, Murphy J, O’Brien S, Byrd JC, et al. The effect of food on the pharmacokinetics of oral ibrutinib in healthy participants and patients with chronic lymphocytic leukemia. Cancer Chemother Pharmacol. 2015;75:907–16.
Marostica E, Sukbuntherng J, Loury D, de Jong J, de Trixhe XW, Vermeulen A, et al. Population pharmacokinetic model of ibrutinib, a Bruton tyrosine kinase inhibitor, in patients with B cell malignancies. Cancer Chemother Pharmacol. 2015;75:111–21.
McDermott J, Jimeno A. Ibrutinib for the treatment of chronic lymphocytic leukemia and mantle cell lymphoma. Drugs Today (Barc). 2014;50:291–300.
O’Brien S, Furman RR, Coutre SE, Sharman JP, Burger JA, Blum KA, et al. Ibrutinib as initial therapy for elderly patients with chronic lymphocytic leukaemia or small lymphocytic lymphoma: an open-label, multicentre, phase 1b/2 trial. Lancet Oncol. 2014;15:48–58.
Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25:579–86.
Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Döhner H, et al. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood. 2008;111:5446–56.
Acknowledgments
The authors thank the Safety Monitoring Committee members for their participation in this study: Koji Izutsu (Toranomon Hospital, Tokyo), Norio Komatsu (Juntendo University School of Medicine, Tokyo), and Noriko Usui (The Jikei University School of Medicine, Dai-San Hospital, Tokyo). The authors thank all the patients, their families, investigators, review committee members, medical experts, nurses, and clinical research coordinators who participated in this clinical trial. The authors also thank Pravin Bolshete & Rishabh Pandey (SIRO Clinpharm Pvt. Ltd.) for writing assistance and Takamitsu Inami (Janssen Pharmaceutical K.K.) for additional editorial support for the development of this manuscript. This study was funded by Janssen Pharmaceutical K.K. Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Tobinai received research funding from Janssen Pharmaceutical K.K., Chugai Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., Celgene K.K., GSK, Servier, Abbvie; received honoraria from Zenyaku Kogyo, and Spectrum Pharmaceuticals. Dr. Ishizawa received honoraria from Takeda Pharmaceutical Company Ltd., Kyowa Hakko Kirin Co. Ltd., and Sanofi; received research funding from Kyowa Hakko Kirin Co. Ltd. Drs. Suzuki, and Munakata received research funding from Janssen Pharmaceutical K.K. Drs. Ogura, Uchida, Aoki, Morishita, and Ushijima have no conflict of interest to declare. Dr. Takahara is an employee of Janssen Pharmaceutical K.K.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Tobinai, K., Ogura, M., Ishizawa, K. et al. Safety and tolerability of ibrutinib monotherapy in Japanese patients with relapsed/refractory B cell malignancies. Int J Hematol 103, 86–94 (2016). https://doi.org/10.1007/s12185-015-1900-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-015-1900-3