Abstract
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) is a rare central nervous system (CNS) disorder with distinct radiological features. However, CLIPEERS may mimic CNS lymphoma, and several cases in which CLIPPERS occurred premonitory to CNS lymphoma have been reported. We report a 31-year-old man presenting with progressive gait ataxia and the characteristic MRI features of CLIPPERS. He was diagnosed with stage II Hodgkin’s lymphoma at the age of 15, and we considered the possibility of newly emerged CNS lymphoma occurring in the immunosuppressive condition after the treatment of Hodgkin’s lymphoma. Histological findings showed no evidence of CNS lymphoma and the neurological symptoms were resolved by steroids. Although CLIPPERS developed in the reverse order in this case, CLIPPERS should be considered in different diagnosis for CNS lymphoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain biopsy is an invasive procedure, but is sometimes necessary for making a definite diagnosis of various disorders including central nervous system (CNS) lymphoma. However, the interpretations of brain biopsy specimens are not always conclusive. In 2012, Pittock et al. described the clinically and radiologically distinct pontine-predominant encephalitis that has been called “chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids” (CLIPPERS) [1]. This disease entity is characterized by that a T cell predominant inflammatory pathology in lesions with unique distribution and clinical and radiological responsiveness to immunosuppressive therapies. No underlying diseases or conditions were initially identified in CLIPPERS. However, there have been several case reports in which CLIPPERS was diagnosed by an initial brain biopsy, but the immunosuppressive therapy was ineffective, and CNS lymphoma was finally confirmed by a second brain biopsy [2–5]. These case reports suggest that CLIPPERS could occur as a herald of CNS lymphoma. As opposed to those case reports, we herein report a case of CLIPPERS that developed after treatment for Hodgkin’s lymphoma.
Case report
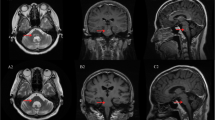
A 31-year-old Japanese man was admitted to our hospital for the evaluation of numbness of hands, dizziness and progressive gait imbalance lasting for 3 months. He was diagnosed with stage II Hodgkin’s lymphoma (mixed cellularity type) at the age of 15 and was treated with C-MOPP (cyclophosphamide, vincristine, procarbazine and prednisone). Complete remission was obtained and he remained free of relapse for 13 years. On admission, neurological examination revealed horizontal nystagmus, dysarthria, and cerebellar ataxia. Limb muscle strengths were normal, but deep tendon reflexes were increased. Position and vibration sensations on both legs were diminished. Laboratory investigation revealed normal blood counts. The levels of liver enzyme, serum creatinine, electrolytes, angiotensin-converting enzyme, vitamin B12, folate and thyroid hormones were all within normal ranges. Serum serological evaluation for syphilis, human immunodeficiency virus and human T cell leukemia virus I was negative. Antinuclear antibodies, rheumatoid factor, antinuclear cytoplasmic antibodies, anti-ganglioside GQ1b IgG antibodies and anti-aquaporin-4 antibodies were negative. Paraneoplastic autoantibodies panels including anti-Hu, anti-CV2, anti-Ma2, anti-Ri, and anti-voltage gated K channels were undetectable. His serum-soluble interleukin-2 receptor level was within a normal range. Head MRI images revealed punctuate gadolinium enhancement in the pons, medulla, cerebellum, cerebral cortex and cervical spinal cord. Contrast-enhancing lesions were associated with high-intensity lesions on T2-weighted MRI and fluid-attenuated inversion recovery sequence (Fig. 1). Cerebrospinal fluid (CSF) showed 5 morphologically normal lymphocytes/mm3 and a total protein level of 96 mg/dL. Oligoclonal bands were not present. No malignant cells were observed, and a microbiological evaluation including bacterial, fungal, and mycobacterial cultures was negative. PCR was negative for Epstein-Barr virus (EBV), cytomegalovirus and JC virus. Brain biopsy from the right frontal cerebral cortex revealed perivascular infiltration of mainly CD4+ mature lymphocytes with parenchymal extension. CD8+ T cells and CD20+ B cells were scarcely detected. Necrotizing vasculitis, demyelination, granulomatous lesions and CNS lymphoma were absent. Hybridization analysis to detect the EBV-RNA was negative (Fig. 2).
Representative brain and spine MRI findings before the immunosuppressive treatment (a–f), at 3 months after treatment (g), at the relapse of disease (h) and after improvement (i). Fluid-attenuated inversion recovery sequence (a, b, i), T2-weighted image (c), T1-weighted with gadolinium enhancement (d–h). Axial and coronal brain MRI shows punctate contrast enhancement affecting the pons and cerebellum on T1-weighted image with gadolinium enhancement with hyper intensity on the fluid-attenuated inversion recovery sequence. Similar foci of gadolinium enhancement are seen in the cervical spinal cord. Chronological change on coronal brain MRI is also indicated
He was diagnosed with CLIPPERS without recurrence of Hodgkin’s lymphoma based upon those findings and was treated with intravenous methylprednisolone at a daily dose of 1 g per body for 5 days, followed by oral prednisolone therapy (1 mg/kg body weight). His neurological deficits and MRI lesions completely disappeared 2 months after commencing steroids. However, when the dose of prednisolone was reduced to 10 mg/day at 22 months after the treatment, he started complaining of difficulty in walking and speaking. A neurological examination showed remarkable ataxia and hypereflexia. Head MRI demonstrated the newly arising enhancing lesions in the middle to upper pons. He was then placed on intravenous methylprednisolone at a dose of 1 g per daily for 5 days. His neurological deficits and radiological findings improved immediately and CLIPPERS remains well controlled with prednisolone 30 months after the diagnosis.
Discussion
CLIPPERS is characterized by typical MRI findings with numerous punctate or nodular enhancing lesions at the pons, medulla or cerebellum. MRI images of our patient initially led us to consider the diagnosis of CLIPPERS. Although recurrence of Hodgkin’s lymphoma in the brain is extremely rare, we did consider the possibility of newly emerged CNS lymphoma occurring in the immunosuppressive condition after treatment for Hodgkin’s lymphoma [6]. Histological findings showed no evidence of CNS lymphoma invasion. Careful follow-up over 2 years found no Hodgkin’s lymphoma relapse, neither in the CNS nor elsewhere.
Characteristics of four patients in the previous reports who presented initially with CLIPPERS features and progressed eventually to CNS lymphoma are summarized in Table 1 [2–5]. They were all male and aged from 33 to 74 years. Their initial presentations include subacute progression of ataxia, diplopia and dysarthria. The first brain biopsy showed reactive T cell lymphocytes similar to those in our patient. Clinical and radiological responses to corticosteroids were initially favorable. However, the disease progressed, and a second biopsy was performed at 3–24 months after the first brain biopsy. Eventually, the diagnosis of B cell lymphoma was made in all four patients.
We believe that the pathogenesis of CLIPPERS is not tightly associated with CNS lymphoma, although there were several patients with CLIPPERS progressed to CNS lymphoma in the literature [2–5]. The underlying pathogenesis of CLIPPERS may also include some autoimmune or hematological disorders. In fact, Ortega et al. reported a 61-year-old woman with multiple sclerosis who developed CLIPPERS shortly after natalizumab withdrawal, and the presentation raised concerns of CNS lymphoma which led to a brain biopsy [7]. Symmonds et al. reported a 36-year-old woman with initial diagnosis of CLIPPERS developed neuromyelitis optica spectrum disorders with brainstem involvement with anti-myelin-oligodendrocyte glycoprotein antibodies [8]. However, CLIPPERS developed after the treatment of CNS lymphoma has not reported. We presented the 31-year-old man of CLIPPERS that developed after treatment for Hodgkin’s lymphoma. We had planned second brain biopsy, when the immunosuppressive therapy was refractory. In fact, we did not perform second biopsy, since the response to treatment in our patient was favorable. In addition, the follow-up brain MRI did not detect any new legions, which were suitable for a biopsy to cause minimum neurological deficits.
Whether CLIPPERS is a process associated with CNS lymphoma remains to be elucidated. However, it is fair to conclude that hematologists should be aware of the possibility of CLIPPERS in differential diagnosis for CNS lymphoma [9]. CLIPPERS might be difficult to determine in the early stage: patients with an initial diagnosis consistent with CLIPPERS should be monitored closely so as not to overlook the coexisting or subsequent development of CNS lymphoma.
References
Pittock SJ, Debruyne J, Krecke KN, Giannini C, van den Ameele J, De Herdt V, et al. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS). Brain. 2010;133:2626–34.
Limousin N, Praline J, Motica O, Cottier JP, Rousselot-Denis C, Mokhtari K, et al. Brain biopsy is required in steroid-resistant patients with chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS). J Neurooncol. 2012;107:223–4.
De Graaff HJ, Wattjes MP, Rozemuller-Kwakkel AJ, Petzold A, Killestein J. Fatal B-cell lymphoma following chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids. JAMA Neurol. 2013;70:915–8.
Taieb G, Uro-Coste E, Clanet M, Lassmann H, Benouaich-Amiel A, Laurent C, et al. A central nervous system B-cell lymphoma arising two years after initial diagnosis of CLIPPERS. J Neurol Sci. 2014;344:224–6.
Lin AW, Das S, Fraser JA, Ang LC, Florendo-Cumbermack A, Jenkins ME, et al. Emergence of primary CNS lymphoma in a patient with findings of CLIPPERS. Can J Neurol Sci. 2014;41:528–9.
Horibe K, Saito AM, Takimoto T, Tsuchida M, Manabe A, Shima M, et al. Incidence and survival rates of hematological malignancies in Japanese children and adolescents (2006–2010): based on registry data from the Japanese Society of Pediatric Hematology. Int J Hematol. 2013;98:74–88.
Ortega MR, Usmani N, Parra-Herran C, Adams DJ, Steingo B, Rammohan KW. CLIPPERS complicating multiple sclerosis causing concerns of CLS lymphoma. Neurology. 2012;79:715–6.
Symmonds M, Waters PJ, Kuker W, Leite MI, Schulz UG. Anti-MOG antibodies with longitudinally extensive transverse myelitis preceded by CLIPPERS. Neurology. 2015;84:1177–9.
Dalia S, Forsyth P, Chavez J, Price S, Shah B, Bello C, et al. Primary B-cell CNS lymphoma clinicopathologic and treatment outcomes in 89 patients from a single tertiary care center. Int J Hematol. 2014;99:450–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
About this article
Cite this article
Mashima, K., Suzuki, S., Mori, T. et al. Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) after treatment for Hodgkin’s lymphoma. Int J Hematol 102, 709–712 (2015). https://doi.org/10.1007/s12185-015-1850-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-015-1850-9