Abstract
Dasatinib, a 2nd-generation tyrosine kinase inhibitor (TKI), can specifically induce large granular lymphocytes (LGL) in some patients with Philadelphia chromosome (Ph)-positive leukemia. To investigate the properties of the induced LGLs, we performed prospective and longitudinal analyses. From Feb 2011 to Jan 2013, a total of 17 patients with Ph-positive leukemia who were previously untreated or refractory to imatinib were enrolled. T cell receptor (TCR)-γ/δ gene rearrangements and phenotypic profiles of lymphocytes were examined before and during administration of dasatinib. LGL lymphocytosis was observed in half of the dasatinib-treated cases (LGL+ group), showing a relation to increased achievement of complete cytogenetic response within 6 months. The phenotypes of the increased lymphocytes were revealed to be mostly natural killer cells. In the LGL+ group, clonal TCR-γ gene rearrangements were frequently detected at diagnosis (six of nine cases) and persisted during therapy, compared with only two of eight in the LGL− group. The proportion of regulatory T cells to CD4+ T cells at diagnosis was lower in the LGL+ compared with the LGL− group (median 4.2 vs. 6.6 %), and this disparity was sustained throughout the therapeutic period. These results demonstrate that immunological condition at diagnosis may affect LGL lymphocytosis in some dasatinib-treated patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tyrosine kinase inhibitors (TKIs) are the standard therapy for chronic myeloid leukemia (CML) and Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL). A first-generation TKI, imatinib was developed and has been clinically used from the beginning of the 21st century, and has shown excellent clinical outcomes for these patients [1]. Dasatinib and nilotinib are called as second-generation TKI, harboring more potent inhibitory effects for target kinase (ABL). Nilotinib exhibits highly selective inhibition for ABL [2], whereas dasatinib exhibits potent inhibition of ABL, as well as inhibition of multiple kinases, i.e., SRC or TEC [3, 4]. These second-generation TKIs have further improved the clinical outcomes for newly diagnosed CML patients in addition to imatinib-resistant/intolerant patients [5–9].
Among CML or Ph+ ALL cases treated with dasatinib, some patients tend to exhibit expansion of large granular lymphocytes (LGLs). While patients with LGL lymphocytosis tend to exhibit preferable clinical effects, adverse effects, such as colitis and pleural effusions, are frequently observed [10–12]. LGLs are phenotypically classified into cytotoxic T cells (CTLs, CD3+ CD8+ CD57+), natural killer (NK) cells (CD3− CD56+), natural killer T (NKT) cells (CD3+ CD56+), and γδ T cells (CD3+ TCR γ/δ+). It was also shown that small numbers of clonal lymphocytes already exist at the diagnosis of these diseases, and that these populations expand during dasatinib treatment, resulting in the characteristic lymphocytosis [13].
Since other TKIs do not exhibit such immunologic effects, the multi-kinase inhibitory effects of dasatinib might be partly responsible for this immunomodulation; however, the detailed mechanism underlying this phenomenon has not been elucidated. To investigate the modulatory influence of dasatinib more precisely, we collected clinical samples from patients with Ph+ leukemia at our institutes and performed a longitudinal analysis. Samples were collected both at diagnosis and after TKI treatment, lymphocyte populations were counted using flow cytometry, and the existence of clonal lymphocytes in each sample was examined by PCR analysis to detect T cell receptor (TCR) γ/δ gene rearrangements. Clinical manifestations, including the effectiveness of treatment and adverse events, were also analyzed in each patient.
Patients and methods
Patients
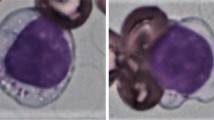
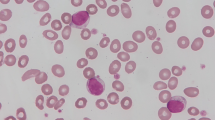
From February 2011 to January 2013, seventeen patients with Ph+ leukemia (14 patients with CML and three with ALL), including 14 previously untreated and 3 that were refractory/intolerant to the initial TKI therapy, were analyzed. Patients with CML received dasatinib and ALL patients were treated with combined chemotherapy including dasatinib and conventional drugs. In addition to routine laboratory tests, TCR gene rearrangements (TCR-γ/δ) and immunophenotypic features using flow cytometer were examined sequentially at diagnosis (before treatment), after treatment within 6 months (2–5 months) and within 1 year (6–12 months). Patients who exhibited apparent emergence of large granular lymphocytes (>20 % of the total white blood cell counts) harboring more than three azurophilic granules in their cytoplasm were defined as LGL positive. This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Ethics Review Board of each institute. Written informed consent was obtained from each patient prior to enrollment.
TCR-γ/δ rearrangements
TCR-γ and δ gene rearrangements were examined by polymerase chain reaction (PCR) analysis, according to the EuroClonality/BIOMED-2 standard protocol [14]. PCR was performed in a Veriti Thermal Cycler (Life Technologies, CA, United States). DNA was extracted from each patient’s sample using QIAamp Blood Mini Kit (QIAGEN, Venlo, Netherlands).
Immunophenotypic analyses
Flow cytometric analyses were performed using FACSCalibur™ (BD Biosciences, CA, United States, for measurement of regulatory T cells alone) or FACS CantoII (BD Biosciences). In the analysis of regulatory T cells, about one hundred thousand peripheral blood mononuclear cells (PBMNCs) were stained with the following antibodies; anti-CD4 (labeled with PerCP, BD Biosciences), anti-CD25 (with APC, BD Biosciences), and anti-Foxp3 (with PE, eBioSciences, CA, United States). After cell sorting with CD4, cells that were double immunopositive for CD25 and Foxp3 were counted as regulatory T cells. In other analysis, approximately 104 PBMNCs were examined and gated with anti-CD45 (labeled with PerCP, BD Biosciences), followed by two-color flow cytometry with the following antibodies; anti-CD3 (with FITC or PE), CD4 (with FITC), CD8 (with PE), CD 16 (with FITC), CD56 (with PE), CD57 (with FITC, BD Biosciences) and TCR-γ/δ (wit FITC), TCR-α/β (with PE); all antibodies, except the anti-CD57 antibodies, were purchased from BECKMAN COULTER (CA, United States).
Statistical analysis
All calculations were performed with EZR (modified R software, Saitama Medical Center, Jichi Medical University, Saitama, Japan) [15]. Mann–Whitney U and Student’s T tests were used for comparison of continuous variables between two groups, and Fisher’s exact test was used for comparisons of qualitative variables. All p values were two-sided and p values <0.05 were considered to be statistically significant.
Results
More than half of the dasatinib-treated patients exhibited LGL lymphocytosis
The patient characteristics are summarized in Table 1. The median age was 59 years (range 21–82 years) and 71 % (12 of 17 patients) were male. Fourteen patients were diagnosed with CML and 3 patients with Ph+ ALL. Three patients received dasatinib as salvage therapy after becoming resistant to the first TKI, imatinib. All of the CML patients were in the chronic phase, even the resistant cases.
Nine (eight patients with CML, one with ALL) of 17 patients (53 %) exhibited LGL lymphocytosis, all of which emerged within 6 months after drug administration. The median lymphocyte counts at 2–5 months after dasatinib treatment were 2990/μL (range 1780–4630/μL) and 1340/μL (range 510–2190/μL) in the LGL (+) and LGL (−) groups, respectively (Fig. 1a). Immunophenotypic analyses revealed that activated NK cells (CD16+ CD56+ CD57+) were increased markedly in 6 patients, whereas CTLs (CD3+ CD57+) were increased in one. Two patients showed increase in both NK cells and CTLs. No significant increases were observed in γ/δ T cells or NKT cells.
The emergence of LGL lymphocytosis tends to exhibit better clinical response
From the clinical perspective, patients with CML harboring LGL lymphocytosis tended to exhibit a better clinical response. Among the 14 dasatinib-treated CML patients, eight exhibited LGL lymphocytosis, all of whom achieved a complete cytogenetic response (CCyR) and 2 patients achieved major molecular response (MMR) within 6 months, whereas only 4 of 6 patients exhibited CCyR and no one showed MMR within the same period in the LGL (−) group. Pleural effusions, which correlated with the emergence of LGL in dasatinib-treated patients, were seen in 5, and all of them exhibited LGL lymphocytosis. While some of them were forced to reduce the dosage of dasatinib due to the adverse events, LGL lymphocytosis persisted during the therapy. In the LGL (−) group, only one patient exhibited pleural effusion (Table 1, Pt 2).
A lower proportion of Treg to CD4+ T cells at diagnosis possibly correlated with LGL lymphocytosis
To elucidate the mechanism underlying the LGL proliferation, we focused on the immunoprofiles of patients with Ph+ leukemia. NK cells, CTLs, γ/δ T cells, and regulatory T cells in peripheral blood were counted by flow cytometric analysis pre- and post-TKI therapy. As noted above, LGLs in dasatinib-treated patients were mostly composed of NK cells; thus, NK cells were increased significantly post-dasatinib therapy [at 2–5 months from the therapy, median with range, 972 (213–2579) cells/µL in the LGL (+) group, and 270 (37–576) cells/µL in the LGL (−) group, p = 0.003, Fig. 1b]. CTL counts at 2–5 months showed same significant difference [445 (151–807) cells/µL in the LGL (+), 149 (30–471) cells/µL in the LGL (−) group, p = 0.01, Fig. 1c], but the difference was not attributed to the increase of CTLs in LGL (+) group. Rather, sustained lower counts in LGL (−) group from pre-treatment state seemed to be responsible for the difference, as shown in Fig. 1c. By contrast, no difference was observed in NK cell counts between the LGL (+) and LGL (−) groups at the pre-therapy evaluation. The γ/δ T cell counts were generally low, with no significant difference between pre- and post-TKI therapy (Fig. 1d).
Regulatory T cells (Treg) exhibited properties similar to the CTLs. The proportion of Treg to CD4+ T cells was lower in the LGL (+) group (median with range, 4.4 % (3.5–10.4 %) compared with the LGL (−) group [6.6 % (1.2–13.2 %) at diagnosis, and this disparity was maintained during the 2- to 5-month follow-up period [4.0 % in the LGL (+) vs. 5.9 % in the LGL (−) group, p = 0.14]; although this difference was not significant (Fig. 2).
Similar TCR-γ/δ gene rearrangement patterns were consistently maintained before and after TKI therapy in the LGL (+) group
We next checked whether clonal lymphocytes were detected in those patients. TCR γ or δ gene rearrangements were investigated by PCR analysis, and clonality was defined as an area under a single peak, >30 % of the whole area under the curve. At the time of diagnosis, 8 and 4 out of 17 patients exhibited clonal TCR γ gene and TCR δ gene rearrangements, respectively. We previously examined the frequency of clonal TCR gene rearrangements, using the same method, in healthy volunteers and in patients with hematological malignancies, such as multiple myeloma. While approximately half of the myeloma patients (62.5 % for TCR γ gene, 50 % for TCR δ gene) exhibited clonal lymphocyte populations, only one of 7 healthy volunteers exhibited TCR gene clonality (data not shown).
Next, we compared the pattern of clonal TCR gene rearrangements between the LGL (+) and LGL (−) groups. In the LGL (+) group, 66.7 % (6 of 9) of the patients exhibited clonal TCR γ gene rearrangements at diagnosis, and the same clonal peaks were consistently detected during the follow-up, as confirmed by identical direct sequencing findings. On the other hand, only 25 % (2 of 8) patients in the LGL (−) group exhibited TCR γ gene clonality at diagnosis, and a shift of the clonal peak was observed in one patient; thus, only one patient continued to exhibit the same clonal peaks (Fig. 3). At follow-up (at 2–5 months), clonal TCR γ rearrangements were more frequently detected in both LGL (+) and LGL (−) groups, increasing to 77.8 and 50.0 %, respectively (Table 2). With respect to TCR δ gene rearrangements, the number of patients who exhibited a clonal peak increased throughout the course of therapy [11.1 % at diagnosis and 55.6 % at follow-up in the LGL (+), 37.5 % and 50 % in the LGL (−) group]; however, no significant difference was observed between the groups (Table 2).
Results of TCR γ gene rearrangement. TCR γ gene rearrangement data at diagnosis (left) and during (right) dasatinib therapy (after 2–5 months), respectively. a In patient 13 (LGL+ group), the same pattern and clonal peaks of the TCR repertoire were obtained, whereas b in patient 2 (LGL− group) different peaks were detected before and during dasatinib treatment. Set a or b represents primer sets for amplification within the gene
Since LGL lymphocytosis during dasatinib treatment was reported to have possible relationship to cytomegalovirus (CMV) reactivation [16], we also examined the state of CMV reactivation using PCR amplification for the major immediate-early region of the viral genome [17] in all of our series of patients at the timing of first follow-up period (2–5 months), but none of the patients with LGL lymphocytosis and only one patient without LGL lymphocytosis showed significant increase of CMV-DNA (data not shown).
Discussion
The clinical outcomes of CML have improved dramatically through the development and incorporation of TKI into our therapeutic modality [1, 5, 6]. Second-generation TKIs, especially dasatinib, not only show potent inhibitory effects for the target kinase (ABL), but also possess many off-target effects, which could be responsible for the different properties and adverse event profiles of each TKI [3, 4]. Among these, the immunomodulatory effects of dasatinib have been of principal interest and the subject of vigorous investigation as the effects might directly influence the clinical outcome [13, 18–20].
Mustjoki et al. [10] first reported the incidence of LGL proliferation during dasatinib therapy and the correlation with better clinical outcomes. Furthermore, Kim et al. [11] also reported the characteristic action of this agent. This lymphocytosis did not occur during treatment with other TKIs, imatinib, or nilotinib. To date, while the mechanism and the target(s) responsible for this phenomenon have been investigated, little has yet to be revealed. Resistance and intolerance continue to be serious problems in CML patients treated with TKIs and directly lead to unsatisfactory outcomes. Therefore, understanding the mechanism underlying lymphocytosis and targeting this immunomodulatory effect will be important in the development of a more effective and risk-free therapeutic strategy for Ph+ leukemia. In our data, more than half of the patients with Ph+ leukemia who were treated with dasatinib exhibited LGL lymphocytosis. The incidence of LGL lymphocytosis in dasatinib-treated patients was similar to previous studies, and as previously reported, these patients tended to exhibit better clinical responses. A higher incidence of adverse events, i.e., pleural effusions, was also observed in our series of patients with LGL.
While LGLs are defined by morphological features, immunologically, they are composed of activated CTLs, NK cells, NKT cells, and γδ T cells, and the proportions have been reported to be quite different between studies [10–12, 21, 22]. In our study, almost all of our patients showed NK cell lymphocytosis and activated CTLs were increased in a few patients. The mechanism responsible for LGL lymphocytosis has not been elucidated precisely, but multiple factors including cytokine levels and the regulation of interacting lymphocytes, i.e., regulatory T cells, have been reported [10, 18, 19]. Regulatory T cells are key regulators of the adapted immune system and are closely correlated with tumor immunity, and could therefore be one of the main targets for cancer immunotherapy [23]. Local accumulation of Tregs in malignant tissue or a higher proportion of Tregs in peripheral blood has been reported in a variety of tumors from different tissues and organs, and these higher Treg activities have been associated with poor clinical outcomes [24–26]. Mustjoki et al. [10] revealed that dasatinib-treated patients with LGL lymphocytosis exhibited a lower proportion of Tregs in peripheral blood, and others examined the differences of Treg ratios among TKIs, with conflicting results [18, 20]. In our study, there were no differences in the proportion of Treg cells between dasatinib-treated patients and patients treated with other TKIs. However, in comparison between the LGL (+) and LGL (−) groups, there were different immunological profiles, including the proportion of Tregs. We observed a lower proportion of Tregs among the CD4+ T cells at the diagnosis of disease in those patients subsequently exhibiting LGL lymphocytosis, and the lower proportion was retained for a substantial period of time during dasatinib treatment. The current results indicate that immunological condition prior to treatment might be one of the important factors in the development of LGL lymphocytosis at a later point. Dasatinib may also have additional effects to maintain lower activity of Tregs, although the detailed mechanisms have not been elucidated.
In addition to the lower proportion of Tregs, mono/oligo-clonal lymphocytes were also detected in most patients with Ph + leukemia at diagnosis, and a disparate pattern was observed between the LGL (+) and (−) groups. Previous studies have reported the existence of clonal lymphocytes before therapy and those clones were restricted not only to cytotoxic T cells but also to NK cells and γδ T cells [11, 13]. Our results were different from the previous data on a few points. First, we observed clonal TCR γ gene rearrangements more frequently at diagnosis, whereas the previous data mainly showed TCR δ gene rearrangements in the LGL (+) group. Second, we detected identical clones pre- and post- TKI therapy, which were confirmed by PCR and direct sequencing of the clonal bands, compared with the detection of few different clones in the previous studies.
We used PCR analysis of TCR gene rearrangements to identify mono-/oligo-clonal lymphocytes. Clonal lymphocytes with the same TCR gene rearrangements were seldom detected in healthy individuals. However, patients with hematological malignancies often possess such clonal lymphocytes that do not originate from malignant cells. For example, patients with multiple myeloma and Waldenstrom macroglobulinemia exhibited clonal expansion of CTLs at diagnosis. These cells were considered to be associated with tumor-specific antigens, although the clinical influences were not determined [27, 28].
We frequently detected TCR γ gene rearrangements in patients with LGL lymphocytosis, and the LGL populations were mainly composed of NK cells. As TCR γ gene rearrangements were theoretically detected in T cells and not NK cells (in case of the TCR δ gene, NK cells could show positive results) [14], those clonal lymphocytes would not likely be derived from LGL, although sorting of the lymphocyte populations responsible for TCR gene rearrangements was not performed. Senior individuals often exhibit positive results with TCR gene rearrangements, likely due to the previous incidence of infectious disease and a decline in thymic function [29, 30]. Kreutzman et al. [16] posited the association of LGL lymphocytosis with dasatinib treatment and cytomegalovirus (CMV) reactivation; however, our results did not show any correlation with lymphocytosis and CMV.
Considering the various factors together, clonal T lymphocytes that exist before TKI therapy are not considered specific for malignant cells or viruses, and such lymphocytes would occur as a result of several immunological changes induced by tumorigenesis. There is a possibility that the lower ratio of Tregs may be one of the responsible factors for such changes.
TKIs are oral drugs that are generally considered tolerable except for those patients with severe adverse events. However, these drugs are costly and require continuous use for the lifetime. Recently, trials to terminate administration TKIs have been recruiting to explore the possibility of cure with CML. Among the published data, the first-generation TKI, imatinib, was mainly attempted, resulting in a long-term event-free survival for approximately 40 % of CML patients [31]. Dasatinib has more potent efficacy to inhibit the target, tyrosine kinase, and might have some additional effects in enhancing the immune response including tumor immunity. Several studies investigating the effects of interferon-alpha (IFN-α), a standard drug for CML before the era of TKI, revealed that the immunological effects of IFN would induce a durable clinical response with a deeper and longer duration, any longer than imatinib despite the lower response rate [32, 33]. Thus, an improvement in clinical results would be expected when dasatinib was used in TKI stopping trials. Moreover, if we could predict immunological responses to dasatinib, such as higher LGL lymphocytosis, in patients harboring fewer Tregs, we might be able to distinguish patients curable (being able to stop TKIs) or not. In our series of patients, among 5 showing both clonal TCR γ gene rearrangements and lower Treg ratio than median at diagnosis, 4 (80 %) eventually showed LGL lymphocytosis during dasatinib administration, and this frequency was relatively higher than that in other patients (5 of 12 patients, 42 %).
In conclusion, we found that proliferation of LGL was not only caused by dasatinib use, but was also associated with immunological condition at diagnosis, which was modified by leukemia. The lower proportion of Tregs or clonal lymphocytes detected by TCR γ gene rearrangements might be among the predictable factors for LGL lymphocytosis when receiving dasatinib as a treatment. The most important limitation is the scale of this study. It would be too small to obtain significant differences and results. Larger scale studies to ascertain our results must be required to resolve several debatable problems including existence of ethnic differences and the proper immunological target of proliferated lymphocytes.
References
Roy L, Guilhot J, Krahnke T, Guerci-Bresler A, Druker BJ, Larson RA, et al. Survival advantage from imatinib compared with the combination interferon-alpha plus cytarabine in chronic-phase chronic myelogenous leukemia: historical comparison between two phase 3 trials. Blood. 2006;108:1478–84.
Weisberg E, Manley P, Mestan J, Cowan-Jacob S, Ray A, Griffin JD. AMN107 (nilotinib): a novel and selective inhibitor of BCR-ABL. Br J Cancer 2006;94:1765–9.
Rix U, Hantschel O, Dürnberger G, Remsing Rix LL, Planyavsky M, Fernbach NV, et al. Chemical proteomic profiles of the BCR-ABL inhibitors imatinib, nilotinib, and dasatinib reveal novel kinase and nonkinase targets. Blood. 2007;110:4055–63.
Hantschel O, Rix U, Schmidt U, Bürckstümmer T, Kneidinger M, Schütze G, et al. The Btk tyrosine kinase is a major target of the Bcr-Abl inhibitor dasatinib. Proc Natl Acad Sci USA. 2007;104:13283–8.
Kantarjian HM, Shah NP, Cortes JE, Baccarani M, Agarwal MB, Undurraga MS, et al. Dasatinib or imatinib in newly diagnosed chronic-phase chronic myeloid leukemia: 2-year follow-up from a randomized phase 3 trial (DASISION). Blood. 2012;119:1123–9.
Kantarjian HM, Hochhaus A, Saglio G, De Souza C, Flinn IW, Stenke L, et al. Nilotinib versus imatinib for the treatment of patients with newly diagnosed chronic phase, Philadelphia chromosome-positive, chronic myeloid leukaemia: 24-month minimum follow-up of the phase 3 randomised ENESTnd trial. Lancet Oncol. 2011;12:841–51.
Giles FJ, le Coutre PD, Pinilla-Ibarz J, Larson RA, Gattermann N, Ottmann OG, et al. Nilotinib in imatinib-resistant or imatinib-intolerant patients with chronic myeloid leukemia in chronic phase: 48-month follow-up results of a phase II study. Leukemia. 2013;27:107–12.
Hochhaus A, Baccarani M, Deininger M, Apperley JF, Lipton JH, Goldberg SL, et al. Dasatinib induces durable cytogenetic responses in patients with chronic myelogenous leukemia in chronic phase with resistance or intolerance to imatinib. Leukemia. 2008;22:1200–6.
Fujisawa S, Nakamae H, Ogura M, Ishizawa K-I, Taniwaki M, Utsunomiya A, et al. Efficacy and safety of dasatinib versus imatinib in Japanese patients with newly diagnosed chronic-phase chronic myeloid leukemia (CML-CP): subset analysis of the DASISION trial with 2-year follow-up. Int J Hematol. 2014;99:141–53.
Mustjoki S, Ekblom M, Arstila TP, Dybedal I, Epling-Burnette PK, Guilhot F, et al. Clonal expansion of T/NK-cells during tyrosine kinase inhibitor dasatinib therapy. Leukemia. 2009;23:1398–405.
Kim DH, Kamel-Reid S, Chang H, Sutherland R, Jung CW, Kim HJ, et al. Natural killer or natural killer/T cell lineage large granular lymphocytosis associated with dasatinib therapy for Philadelphia chromosome positive leukemia. Haematologica. 2009;94:135–9.
Nagata Y, Ohashi K, Fukuda S, Kamata N, Akiyama H, Sakamaki H. Clinical features of dasatinib-induced large granular lymphocytosis and pleural effusion. Int J Hematol. 2010;91:799–807.
Kreutzman A, Juvonen V, Kairisto V, Ekblom M, Stenke L, Seggewiss R, et al. Mono/oligoclonal T and NK cells are common in chronic myeloid leukemia patients at diagnosis and expand during dasatinib therapy. Blood. 2010;116:772–82.
van Dongen JJM, Langerak AW, Bruggemann M, Evans PAS, Hummel M, Lavender FL, et al. Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: report of the BIOMED-2 Concerted Action BMH4-CT98-3936. Leukemia. 2003;17:2257–317.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Kreutzman A, Ladell K, Koechel C, Gostick E, Ekblom M, Stenke L, et al. Expansion of highly differentiated CD8 + T-cells or NK-cells in patients treated with dasatinib is associated with cytomegalovirus reactivation. Leukemia. 2011;25:1587–97.
Olive DM, Simsek M, Al-Mufti S. Polymerase chain reaction assay for detection of human cytomegalovirus. J Clin Microbiol. 1989;27:1238–42.
Rohon P, Porkka K, Mustjoki S. Immunoprofiling of patients with chronic myeloid leukemia at diagnosis and during tyrosine kinase inhibitor therapy. Eur J Haematol. 2010;85:387–98.
Powers JJ, Dubovsky JA, Epling-Burnette PK, Moscinski L, Zhang L, Mustjoki S, et al. A molecular and functional analysis of large granular lymphocyte expansions in patients with chronic myelogenous leukemia treated with tyrosine kinase inhibitors. Leuk Lymphoma. 2011;52:668–79.
Hayashi Y, Nakamae H, Katayama T, Nakane T, Koh H, Nakamae M, et al. Different immunoprofiles in patients with chronic myeloid leukemia treated with imatinib, nilotinib or dasatinib. Leuk Lymphoma. 2012;53:1084–9.
Kumagai T, Matsuki E, Inokuchi K, Ohashi K, Shinagawa A, Takeuchi J, et al. Relative increase in lymphocytes from as early as 1 month predicts improved response to dasatinib in chronic-phase chronic myelogenous leukemia. Int J Hematol. 2014;99:41–52.
Tanaka H, Nakashima S, Usuda M. Rapid and sustained increase of large granular lymphocytes and rare cytomegalovirus reactivation during dasatinib treatment in chronic myelogenous leukemia patients. Int J Hematol. 2012;96:308–19.
Nishikawa H, Sakaguchi S. Regulatory T cells in tumor immunity. Int J Cancer. 2010;127:759–67.
Sasada T, Kimura M, Yoshida Y, Kanai M, Takabayashi A. CD4+ CD25+ regulatory T cells in patients with gastrointestinal malignancies: possible involvement of regulatory T cells in disease progression. Cancer. 2003;98:1089–99.
Curiel TJ, Coukos G, Zou L, Alvarez X, Cheng P, Mottram P, et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med. 2004;10:942–9.
Bates GJ, Fox SB, Han C, Leek RD, Garcia JF, Harris AL, et al. Quantification of regulatory T cells enables the identification of high-risk breast cancer patients and those at risk of late relapse. J Clin Oncol. 2006;24:5373–80.
Sze DM-Y. Clonality detection of expanded T-cell populations in patients with multiple myeloma. Methods Mol Med. 2005;113:257–67.
Li J, Sze DMY, Brown RD, Cowley MJ, Kaplan W, Mo SL, et al. Clonal expansions of cytotoxic T cells exist in the blood of patients with Waldenstrom macroglobulinemia but exhibit anergic properties and are eliminated by nucleoside analogue therapy. Blood. 2010;115:3580–8.
Posnett DN, Sinha R, Kabak S, Russo C. Clonal populations of T cells in normal elderly humans: the T cell equivalent to “benign monoclonal gammapathy”. J Exp Med. 1994;179:609–18.
Naylor K, Li G, Vallejo AN, Lee W-W, Koetz K, Bryl E, et al. The influence of age on T cell generation and TCR diversity. J. Immunol. 2005;174:7446–52.
Mahon F-X, Réa D, Guilhot J, Guilhot F, Huguet F, Nicolini F, et al. Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol. 2010;11:1029–35.
Kreutzman A, Rohon P, Faber E, Indrak K, Juvonen V, Kairisto V, et al. Chronic myeloid leukemia patients in prolonged remission following interferon-α monotherapy have distinct cytokine and oligoclonal lymphocyte profile. PLoS One. 2011;6:e23022.
Talpaz M, Hehlmann R, Quintás-Cardama A, Mercer J, Cortes J. Re-emergence of interferon-α in the treatment of chronic myeloid leukemia. Leukemia. 2013;27:803–12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Masafumi Taniwaki have received grant from Bristol-Myers Squibb.
About this article
Cite this article
Shimura, Y., Horiike, S., Tsutsumi, Y. et al. The longitudinal analysis of large granular lymphocytosis in patients with Philadelphia chromosome-positive leukemia treated with dasatinib. Int J Hematol 102, 426–433 (2015). https://doi.org/10.1007/s12185-015-1848-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-015-1848-3