Abstract
The outcomes of children with relapsed acute myeloid leukemia (AML) are known to be poor, but remain obscure. We retrospectively analyzed 71 patients who had relapsed following first-line treatment under the AML99 protocol. We investigated the time and site of recurrence, response to re-induction therapy, and performance of hematopoietic stem cell transplantation (HSCT) in relapsed cases, and performed a multivariate analysis to identify prognostic factors. The 5-year overall-survival (OS) rate after relapse was 37 %. Of 71 patients, three died without any anti-leukemic therapy and two underwent allogeneic HSCT. The remaining 66 patients received re-induction chemotherapy, and 33 (50 %) achieved second CR (CR2). Twenty-two of 25 (88 %) late relapse patients and 11 of 41 (27 %) early relapse patients achieved CR2 (P < 0.001). Twenty-nine CR2 cases and 35 non-CR2 cases underwent allogeneic HSCT. The 5-year OS rate was significantly higher in patients who underwent HSCT in CR2 than those in non-CR2 (66 vs. 17 %, P < 0.000001). Multivariate analysis indicated that early relapse (P < 0.05) and the positivity of the FMS-like tyrosine kinase 3—internal tandem duplication (P < 0.05) were adverse prognostic factors for survival. In conclusion, the etiology of relapsed pediatric AML needs to be elucidated and effective chemotherapy should be administered to obtain CR2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of childhood acute myeloid leukemia (AML) in Japan has led to a complete remission (CR) rate of approximately 90 % and 5-year overall-survival rate (OS) of approximately 70 % [1, 2]. Western studies reported a 30–40 % relapse fraction among children with AML and the OS rate for these relapsing children was 24–36 % [3–9]. Relapsed AML in children appears to have some common characteristics in that the median relapse time is approximately 10 months and OS after relapse is less than 40 % in spite of various chemotherapy protocols in different countries [3–9]. Treatment strategies for recurrent AML children in Japan have been left to the discretion of each medical institution, and neither unified treatment guidelines nor nationwide clinical trials have been accomplished until now. To clarify the prognosis of relapsed pediatric AML, we retrospectively analyzed relapsed cases in the AML99 protocol of the Japanese Childhood AML Cooperative Study. In the AML99 protocol, children with newly diagnosed de novo AML were treated with continuous cytarabine-based induction therapy (Induction A, B, or C regimens, details have been described below) and stratified into three risk groups based on the initial treatment response, age, WBC, and cytogenetics [1]. Three or four courses of consolidation chemotherapy included high-dose cytarabine. Allogeneic hematopoietic stem cell transplantation (HSCT) was only indicated for intermediate-risk (IR) patients with a matched related donor and for high-risk (HR) subsets.
Although molecular data were not used for stratifying patients in AML99 protocol, we have analyzed the prognostic factors with several gene alterations such as FMS-like tyrosine kinase 3 (FLT3)—internal tandem duplication (ITD) in addition to the clinical characteristics.
Patients
A total of 240 children younger than 18 years with newly diagnosed de novo AML were registered in the AML99 protocol between January 2000 and December 2002. The Institutional Review Board approved the protocol and written informed consent was obtained from their parents or guardians. Of 209 patients who achieved CR, 73 had relapsed by December 2005. Two patients were excluded from our analysis because of insufficient data. Therefore, the total number of relapsed patients examined in the present study was 71.
Methods
Each medical institution diagnosed recurrence independently. We investigated the time and site of recurrence, response to re-induction therapy, the performance of HSCT after relapse, and cause of death in relapsed cases. Each institution chose treatment procedures for recurrent patients individually. When considering these procedures, we defined “re-induction therapy” as a single course of chemotherapy according to one of the AML99 induction regimens (Induction A, B or C; see below). Other treatment regimens and two or more courses of chemotherapy were classified as “Miscellaneous”.
AML99 Induction A (ECM) regimen: etoposide (VP-16) 150 mg/m2 × 5 days, cytosine arabinoside (Ara-C) 200 mg/m2 × 7 days and mitoxantron (MIT) 5 mg/m2 × 5 days.
AML99 Induction B (sqECI) regimen: VP-16 100 mg/m2 × 3 days, [Ara-C 500 mg/m2 + idarubicin (IDA) 8 mg/m2] × 3 days and [VP-16 200 mg/m2 + Ara-C 500 mg/m2] × 3 days.
AML99 Induction C (CIEC) regimen: [Ara-C 500 mg/m2 + IDA 8 mg/m2] × 3 days and [VP-16 200 mg/m2 + Ara-C 500 mg/m2] × 3 days.
The length of first CR (CR1) was calculated as the time from CR1 to the first relapse. Early relapse was defined as relapse within 1 year of entering CR1, and late relapse was defined as relapse after more than 1 year in CR1. OS after relapse or HSCT was defined as the period from relapse or HSCT to death by any cause. Disease-free survival (DFS) was the time from second CR (CR2) to a second relapse or death by any cause. Surviving patients were censored on the last date when they were known to be alive at each medical institution. Statistical analysis using χ 2 tests was performed in order to assess the relationship between various clinical characteristics and CR2 by chemotherapy. We used the Kaplan–Meier method to estimate survival rates and the Cox proportion hazards model for the multivariate analysis of prognostic factors. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Japan) [10], a graphical user interface for R (The R Foundation for Statistical Computing), or more precisely, a modified version of R commander designed to add statistical functions frequently used in biostatistics.
Genetic alterations and Wilms tumor 1 mutation (WT1) mRNA expression were examined in 40 relapsing individuals from the diagnostic BM samples. Mutation analysis for ITD within the JM domain and D835 mutation (D835Mt) within the TK2 domain of FLT3 were performed as previously described [11, 12]. Mutation analysis of the KIT gene was performed with real-time polymerase chain reaction (RT-PCR) followed by direct sequencing as previously reported [13]. Mixed-lineage leukemia (MLL)—partial tandem duplication (PTD) was examined by simple first round RT-PCR with 35 cycles using the primer pair as previously described [14–16]. Exon 2 and 3 of the N-RAS and K-RAS genes were amplified by RT-PCR and directly sequenced using primer pairs as previously reported [17]. Total RNA extracted from the BM samples was reverse transcribed to cDNA Synthesis Kit (Amersham Bioscience, Tokyo, Japan). WT1 mRNA expression was measured using RT-PCR system (ABI 7700, Applied Biosystems) with primers and controls as previously reported [18].
Results
Relapse occurred in 71 cases 34 to 1,156 days (median 312 days) after achieving CR1. The median follow-up after relapse in all survivors was 9.5 (range 7.5–12.2) years. Table 1 shows the clinical characteristics of the 71 patients examined in the present study. A total of 6 patients underwent allogeneic HSCT in CR1, including 3 IR patients and 3 HR patients. In 45 out of 71 patients (63.4 %), relapse occurred within 1 year after entering CR1 (early relapse), whereas late relapse occurred in 26 patients (36.6 %).
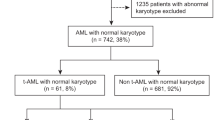
Figure 1 shows the clinical outcomes of all cases. Of 71 patients analyzed in this study, three patients died without any anti-leukemic therapy and two patients proceeded to allogeneic HSCT skipping chemotherapy. The other 66 patients received re-induction chemotherapy and 33 children (50 %) achieved CR2. Twenty-nine cases in CR2 and a total of 35 cases in non-CR2 underwent subsequent allogeneic HSCT. One patient remained in long-term CR after missing HSCT due to a severe infection. Of the 47 cases that died, 42 were in relapse or the refractory phase. Three cases died in CR2 due to multiple organ failure caused by sepsis on day 13 of HSCT, a hemothorax 6 months after HSCT, and sudden death of an unknown cause 9 years after HSCT. Two patients died in third CR (CR3) due to graft-versus-host disease after the second HSCT.
The overall CR2 rate by heterogeneous re-induction regimens was 50 %. As described in detail in Table 2, CR2 rate of late relapse patients was significantly higher than that of early relapse patients (88 vs. 27 %, P < 0.001). Most of late relapse patients received ECM or sqECI regimens as re-induction chemotherapy, which were the same as the initial induction chemotherapy in the AML99 protocol. On the other hand, CR rate of various chemotherapy regimens (miscellaneous) for early relapse patients was 21 %. No patient achieved CR2 by chemotherapy for relapse after allogeneic HSCT in CR1.
As summarized in Table 3, CR2 rate and 5-year OS rate were 69 and 46 % in favorable cytogenetic risk group (n = 13), 39 and 31 % in intermediate-risk group, respectively, and there were no statistically significant differences among three risk groups [19–21]. However, it should be noted that nearly half of the patients having t(8;21) or inv(16), who had been treated without allogeneic HSCT in CR1 following AML99 protocol, were rescued by allogeneic HSCT even after relapse.
The 5- and 10-year OS rates were 36.6 % (95 % CI 25.6–47.7) and 32.9 % (95 % CI 22.0–44.2) for 71 cases (Fig. 2a). The 5-year OS rate correlated with the initial risk group: 56.8 % in the LR, 34.8 % in the IR, and 0 % in the HR groups (P < 0.0001, Fig. 2b), respectively. Regarding the 5-year OS rates, significant differences were observed between an age older and younger than 10 years (25.0 vs. 42.6 %, P = 0.023), FAB-M7 and others (16.7 vs. 38.5 %, P = 0.025), initial induction response: M1 and others (41.3 vs. 0 %, P < 0.0001), relapse after allogeneic HSCT in CR1 and others (0 vs. 40.0 %, P < 0.00001), and early and late relapse (22.2 vs. 61.5 %, P < 0.0001).
Based on genomic data in diagnostic BM samples from the AML99 study, we calculated CR2 rate and 5-year OS of 40 relapsed cases with analysis for C-KIT, N-RAS, K-RAS, FLT3-ITD, D838Mt, MLL-PTD and WT1 mutation >10,000 copies (Table 4). CR2 rate of patients with FLT3-ITD and WT1 mutation >10,000 copies were significantly low (P < 0.05). However, only positivity for FLT3-ITD correlated with a significantly poor OS after relapse (P = 3.15e−7).
We selected age at diagnosis (older than 10 years), FAB classification (M7), cytogenetics (core-binding factor; CBF), initial induction response, relapse phase (after allogeneic HSCT), early/late relapse and FLT3-ITD for multivariate analyses for OS in order to identify prognostic factors after the relapse of AML (Table 5). Only an early relapse and positivity of FLT3-ITD were identified as adverse prognostic factors for survival (Cox regression).
The 5- and 10-year OS rates were significantly higher in patients who underwent HSCT in CR2 than those in non-CR2 (65.5 vs. 17.1 %, P < 0.0000001; 65.5 vs. 9.5 %, P < 0.0000001, Fig. 3a). The 5-year DFS rate in CR2 was 65 %. No significant difference was observed in the 5-year OS rate in CR2 and non-CR2 with regard to the stem cell source (Fig. 3b).
a The 5- and 10-year OS after HSCT in patients with CR2 by re-induction chemotherapy (n = 29) and in those with non-CR2 (n = 35) (65.5 vs. 17.1 %, 65.1 vs. 9.5 %, P < 0.000001). b The 5-year OS by the stem cell source after HSCT following (n = 64). No significant difference by stem cell sources in CR2 patients (P = 0.923) and non-CR2 patients (P = 0.801). HSCT hematopoietic stem cell transplantation, OS overall survival, CR2 second complete remission, non-CR2 non-second complete remission, CI confidence interval, BM bone marrow, PB peripheral blood, UCB umbilical cord blood
Discussion
This study showed that the CR2 rate by heterogeneous re-induction regimens was 50 % and 5-year OS was 37 %. Western studies reported that the CR2 rate by chemotherapy was 62–77 % and 5-year OS rate was 23–36 % in childhood AML (Table 6), respectively [3–9]. The percentage of patients that relapsed early (63 %) was consistent with previous findings, whereas the performance rate of HSCT following the first relapse was higher (CR2 cases, 88 %; all cases, 90 %), which may have contributed to the salvage of many cases. Although low-risk (LR) patients having t(8;21) or inv(16) were treated without allogeneic HSCT in CR1, half of the recurrent patients in LR could be rescued by allogeneic HSCT even after relapse (Table 6).
The CR2 rate of early relapse patients was lower than that of late relapse patients, which was in agreement with the findings of non-Japanese studies [3–9]. The combination of fludarabine, Ara-C and granulocyte-colony stimulating factor (FLAG) with or without an anthracycline has induced CR2 rates of 58–78 % [4, 6, 7, 9, 22, 23]; however, we identified only one patient that was treated with FLAG + idarubicin and achieved CR2. Furthermore, no patient in this study received gemtuzumab ozogamicin [24, 25] or clofarabin [26, 27] as re-induction therapy. As many frontline AML chemotherapy protocols include a total anthracycline dose exceeding 350 mg/m2, effective chemotherapy without anthracyclines [28, 29] should be introduced to obtain CR2.
No relationship was observed between the cytogenetic risk classification at initial diagnosis and CR2 or 5-year OS. FLT3-ITD mutations are known to be a strong prognostic factor, independent of other factors including genetic chromosomal abnormalities [30–34]. However, FLT3-ITD was not available as a stratification factor in the AML99 protocol. We had not only molecular abnormality analysis at diagnosis of all cases, but also cytogenetic data at relapse. In recent protocols using FLT3-ITD as a high-risk factor, allogeneic HSCT in CR1 for AML patients with FLT3-ITD is recommended. On the other hand, high WT1 expression after induction chemotherapy was reported to be a poor prognostic factor [34]. Cytogenetic and molecular studies at relapse as well as diagnosis may be able to more precisely predict the prognosis of patients.
OS after HSCT in CR2 was 68 % for allogeneic BMT and 57 % for UCB transplant; therefore, the stem cell source did not appear to be relevant [35, 36]. UCB transplants for AML patients younger than 16 years have been performed in approximately 289 cases in Japan, and their 5-year OS rates in CR1 and CR2 were 67.3 and 61.4 % [37]. This source for HSCT might facilitate a timely transplant.
There were some limitations in this study. We only analyzed relapses that occurred during the first 3 years from the end of the AML99 study. Another limitation may be that each participating institution diagnosed recurrence independently without a central confirmation. In conclusion, further clinical trials with cytogenetic and molecular data are necessary in order to verify the genetic or molecular background of relapsed pediatric AML, and the swift introduction of new promising drugs [28, 29] is imperative for relapsed AML children to obtain CR [38].
Most of the results of the present study were presented at the 48th Annual Meeting of the Japan Pediatric Society of Hematology (November 2006, Osaka) and the 9th Childhood Leukemia Symposium (April 2014, Prague).
References
Tsukimoto I, Tawa A, Horibe K, Tabuchi K, Kigasawa H, Tsuchida M, et al. Risk-stratified therapy and the intensive use of cytarabine improves the outcome in childhood acute myeloid leukemia: the AML99 trial from the Japanese Childhood AML Cooperative Study Group. J Clin Oncol. 2009;27:4007–13.
Imamura T, Iwamoto S, Kanai R, Shimada A, Terui K, Osugi Y, et al. Outcome in 146 patients with pediatric acute myeloid leukemia treated according to the AML99 protocol in the period 2003–06 from the Japan Association of Childhood Leukemia Study. Br J Haematol. 2012;159:204–10.
Webb DKH, Wheatley K, Harrison G, Stevens RF, Hann IM, et al. Outcome for children with relapsed acute myeloid leukemia following initial therapy in the Medical Research Council (MRC) AML 10 trial. Leukemia. 1999;13:25–31.
Aladjidi N, Auvrigno A, Leblanc T, Perel Y, Berard A, Bordigoni P, et al. Outcome in children with relapsed acute myeloid leukemia after initial treatment with the French Leucemie Aique Myeloide Enfant (LAME) 89/91 protocol of the French Society of Pediatric Hematology and Immunology. J Clin Oncol. 2003;21:4377–85.
Wells RJ, Adams MT, Alonzo TA, Arceci RJ, Buckley J, Buxton AB, et al. Mitoxantrone and cytarabine induction, high-dose cytarabine, and etoposide intensification for pediatric patients with relapsed or refractory acute myeloid leukemia: children’s Cancer Group Study 2951. J Clin Oncol. 2003;21(15):2940–7.
Abrahamsson J, Clausen N, Gustafsson G, Hovi L, Jonmundsson G, Zeller B, et al. Improved outcome after relapse in children with acute myeloid leukemia. Br J Haematol. 2007;136(2):229–36.
Sander A, Zimmermann M, Dworzak M, Fleischhack G, von Neuhoff C, Reinhardt D, et al. Consequent and intensified relapse therapy improved survival in pediatric AML: results of relapse treatment in 379 patients of three consecutive AML-BFM trails. Leukemia. 2010;24:1422–8.
Gorman MF, Ji L, Ko RH, Barnette P, Bostrom B, Hutchinson R, et al. Outcome for children treated for relapsed or refractory acute myelogenous leukemia (rAML): a therapeutic advances in childhood leukemia (TACL) consortium study. Pediatric Blood Cancer. 2010;55(3):421–9.
Kaspers GJL, Zimmermann M, Reinhardt D, Gibson BES, Tamminga RYJ, Aleinikova O, et al. Improved outcome in pediatric acute myeloid leukemia: results of randomized trial on Liposomal Daunorubicin by the International BFM Study Group. J Clin Oncol. 2013;31(5):599–607.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” (Easy R) for medical statics. Bone Marrow Transplant. 2013;48:452–8.
Taketani T, Taki T, Sugita K, et al. FLT3 mutations in the activation loop of tyrosine kinase domain are frequently found in infant ALL with MLL rearrangements and pediatric ALL with hyperdiploidy. Blood. 2004;103:1085–8.
Yamamoto Y, Kiyoi H, Nakano Y, et al. Activating mutation of D835 within the activation loop of FLT3 in human hematologic malignancies. Blood. 2001;31:187–90.
Shimada A, Taki T, Tabuchi K, Tawa A, Horibe K, Tsuchida M, et al. KIT mutations, and not FLT3 internal tandem duplication, are strongly associated with a poor prognosis in pediatric acute myeloid leukemia with t(8;21): a study of the Japanese Childhood AML Cooperative Study Group. Blood. 2006;107:1806–9.
Shimada A, Taki T, Tabuchi K, Taketani T, Hanada R, Tawa A, et al. Tandem duplication of MLL and FLT3 are correlated with poor prognoses in pediatric acute myeloid leukemia: a study of the Japanese childhood AML cooperative Study Group. Pediatr Blood Cancer. 2008;50(2):264–9.
Jamal R, Taketani T, Taki T, et al. Coduplication of the MLL and FLT3 genes in patients with acute myeloid leukemia. Genes Chromosomes Cancer. 2001;31:187–90.
Schnittger S, Wormann B, Hiddemann W, et al. Partial tandem duplications of the MLL gene are detectable in peripheral blood and bone marrow of nearly all healthy donors. Blood. 1998;92:1728–34.
Shimada A, Taki T, Koga D, Tabuchi K, Tawa A, Hanada R, et al. Low frequency of KIT mutations in pediatric acute myeloid leukemia with inv(16)(p13q22): a study of the Japanese Childhood AML Cooperative Study Group. Int J Hematol. 2007;86:289–90.
Sano H, Shimada A, Tabuchi K, Taki T, Murata C, Park MJ, et al. WT1 mutation in pediatric patients with acute myeloid leukemia: a report from the Japanese Childhood AML Cooperative Study Group. Int J Hematol. 2013;98:437–45.
Harrison CJ, Hills RK, Moorman AV, Grimwade DJ, Hann I, Webb DK, et al. Cytogenetics of childhood acute myeloid leukemia: United Kingdom Medical Research Council Treatment trials AML 10 and 12. J Clin Oncol. 2010;28(16):2674–81.
Von Neuhoff C, Reinhardt D, Sander A, Zimmermann M, Bradtke J, Betts DR, et al. Prognostic impact of specific chromosomal aberrations in a large group of pediatric patients with acute myeloid leukemia treated uniformly according to trial AML-BFM 98. J Clin Oncol. 2010;28(16):2682–9.
Creutzig U, van den Heuvel-Eibrink MM, Gibson B, Dworzak MN, Adachi S, de Bont E, et al. Diagnosis and management of acute myeloid leukemia in children and adolescents: recommendations from international expert panel. Blood. 2012;120(16):3187–205.
Fleischhack G, Hassan C, Graf N, Mann G, Bode U. IDA-FLAG (idarubicin, fludarabine, cytarabine, G-CSF), an effective remission-induction therapy for poor-prognosis AML of childhood prior to allogeneic or autologous bone marrow transplantation: experiences of a phase II trial. Br J Haematol. 1998;102(3):647–55.
Yalman N, Sarper N, Devecioğlu O, Anak S, Eryilmaz E, Can M, et al. Fludarabine, cytarabine, G-CSF and idarubicin (FLAG-IDA) for the treatment of relapsed or poor risk childhood acute leukemia. Turk J Pediatr. 2000;42(3):198–204.
Aplenc R, Alonzo TA, Gerbing RB, Lange BJ, Hurwitz CA, Wells RJ, et al. Safety and efficacy of gemtuzumab ozogamicin in combination with chemotherapy for pediatric acute myeloid leukemia: a report from the Children’s Oncology Group. J Clin Oncol. 2008;26:2390–5.
Zwaan CM, Reinhardt D, Zimmerman M, Hasle H, Stary J, Stark B, et al. Salvage treatment for children with refractory first or second relapse of acute myeloid leukemia with gemtuzumab ozogamicin: results of a phase II study. Br J Haematol. 2010;148(5):768–76.
Jeha S, Razzouk B, Rytting M, Rheingold S, Albano E, Kadota R, et al. Phase II study of clofarabine in pediatric patients with refractory or relapsed acute myeloid leukemia. J Clin Oncol. 2009;27(26):4392–7.
Becker PS, Kantarjian HM, Appelbaum FR, Petersdorf SH, Storer B, Pierce S, et al. Clofarabine with high dose cytarabine and granulocyte colony-stimulating factor (G-CSF) priming for relapsed and refractory acute myeloid leukemia. Br J Haematol. 2011;155(2):182–9.
Miano M, Pistorio A, Putti MC, Dufour C, Messina C, Barisone E, et al. Clofarabine, cyclophosphamide and etoposide for the treatment of relapsed or resistant acute leukemia in pediatric patients. Leuk Lymphoma. 2012;53(9):1693–8.
Davila J, Slotkin E, Renaud T. Relapsed and refractory pediatric acute myeloid leukemia: current and emerging treatments. Pediatr Drugs. 2014;16:151–68.
Kiyoi H, Naoe T, Nakano Y, Yokota S, Minami S, Miyawaki S, et al. Prognostic implication of Flt3 and N-ras gene mutations in acute myeloid leukemia. Blood. 1999;93:3074–80.
Kottaridis PD, Gale RE, Frew ME, Harrison G, Langabeer SE, Belton AA, et al. The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood. 2001;98:1752–9.
Meshinchi S, Woods WG, Stirewalt DL, Sweetser DA, Buckley JD, Tjoa TK, et al. Prevalence and prognostic significance of Flt3 internal tandem duplication in pediatric acute myeloid leukemia. Blood. 2001;97:89–94.
Zwaan CM, Meshinchi S, Radich JP, Veerman AJ, Huismans DR, Munske L, et al. FLT3 internal tandem duplication in 234 children with acute myeloid leukemia: prognostic significance and relation to cellular drug resistance. Blood. 2003;102:2387–94.
Shimada A, Taki T, Koga D, Tabuchi K, Tawa A, Hanada R, et al. High WT1 mRNA expression after induction chemotherapy and FLT3-ITD have prognostic impact in pediatric acute myeloid leukemia: a study of the Japanese Childhood AML Cooperative Study Group. Int J Hematol. 2012;96(4):469–76.
Fagioli F, Zecca M, Locatelli F, Lanino E, Uderzo C, Di Bartolomeo P, et al. Allogeneic stem cell transplantation for children with acute myeloid leukemia in second complete remission. J Pediatr Hematol Oncol. 2008;30:575–83.
Isoyama K, Oda M, Kato K, Nagamura-Inoue T, Kai S, Kigasawa H, et al. Long-term outcome of cord blood transplantation from unrelated donors as an initial transplantation procedure for children with AML in Japan. Bone Marrow Transplant. 2010;45:69–77.
The Japan Society for Hematopoietic Cell Transplantation Annual Report of Nationwide Survey 2012, JSHCT monograph, vol. 38, p. 97–127 (in Japanese), ISSN 1344-5898.
Rubnitz JE, Razzouk BI, Lensing S, Pounds S, Pui CH, Ribeiro RC. Prognostic factors and outcome of recurrence in childhood acute myeloid leukemia. Cancer. 2007;109:157–63.
Acknowledgments
The authors deeply appreciate the invaluable cooperation by the large number of physicians working at institutions affiliated to The Japanese Childhood AML Cooperative Study Group and The Japanese Pediatric Leukemia/Lymphoma Study Group. Research was supported by Grant-in-Aid for Cancer Research from the Ministry of Health, Labor, and Welfare of Japan.
Conflict of interest
The authors declare no conflict of financial interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Nakayama, H., Tabuchi, K., Tawa, A. et al. Outcome of children with relapsed acute myeloid leukemia following initial therapy under the AML99 protocol. Int J Hematol 100, 171–179 (2014). https://doi.org/10.1007/s12185-014-1616-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-014-1616-9