Abstract
We conducted a phase I study using midostaurin (25 or 50 mg orally twice daily), all-trans retinoic acid (ATRA) and CLAG chemotherapy to target multiple pathways in relapsed/refractory AML. 10 patients received the combination and no dose-limiting toxicities were observed. Two patients (22 %) achieved complete remission and 1 patient (11 %) achieved complete remission with incomplete count recovery. Pharmacokinetic data showed that the 25 mg dosing of midostaurin achieved therapeutic levels with no significant interaction between midostaurin and ATRA. With evidence of activity of ATRA in NPM1-mutated AML and midostaurin in FLT3-ITD AML, this combination warrants further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with relapsed or refractory acute myeloid leukemia (AML) have poor outcome with conventional salvage chemotherapy. Hence there is a need for better treatment options for these patients. Since multiple signal transduction pathways are simultaneously activated/dysregulated in AML [1], combination of salvage chemotherapy and agents that target survival/signaling pathways may provide a higher disease remission. In this single-institutional phase I study, we investigated the combination of a potent salvage chemotherapy regimen containing cladribine, cytarabine (Ara-C) and granulocyte colony stimulating factor (G-CSF) (CLAG) along with a tyrosine kinase inhibitor (midostaurin) and a differentiation-inducing agent All-trans retinoic acid (ATRA) to assess its tolerability and to identify whether standard dose midostaurin (50 mg BID) could be tolerated in this combination in relapsed/refractory adult AML. Cladribine is known to have a high activity in AML and CLAG has been previously shown to be efficacious in relapsed/refractory AML [2]. In a recent Phase III trial, the addition of cladribine to cytarabine and daunorubicin was found to improve survival [3]. A phase I study using CLAG in combination with G-CSF and imatinib, a tyrosine kinase inhibitor, showed good tolerability for this combination [4]. FLT-3 mutations are seen in about 25–30 % of patients with AML and are associated with poor long-term survival [5]. FLT-3 is also overexpressed and shows high activity in patients without FLT-3 mutations. Constitutively activated FLT-3 signals through pathways that include ras/MAP kinase, STAT5, and PI3 kinase/AKT, contributing to blocks in apoptosis and differentiation and stimulating proliferation making FLT-3 a promising target in AML [6]. Midostaurin is a multi-targeted kinase inhibitor that has been shown to inhibit both wild type and mutated FLT-3. Both directly and indirectly, midostaurin also potently inhibits multiple other molecular targets thought to be important for the pathogenesis of AML like VEGFR-1, a VEGF receptor; c-kit; H-and K-ras; as well as the multidrug resistant gene, MDR [7]. The lack of myelosuppression observed in solid tumor patients treated with midostaurin offers the possibility of increased therapeutic efficacy without prolonged myelosuppression when combined with standard chemotherapy in AML patients [8].
In a recent phase IIb study in patients with AML and high-risk myelodysplastic syndrome (MDS), midostaurin as a single agent showed a response rate [defined as complete response (CR), partial response (PR), hematologic improvement, or reduction in peripheral blood or bone marrow blasts by ≥50 %] of 71 % in FLT3-mutated patients and 42 % in FLT3 wild-type patients [9]. A phase Ib study in newly diagnosed young adult AML using the combination of midostaurin with Ara-C and daunorubicin showed good tolerability with 50 mg twice daily dosing of midostaurin and high CR rate in both FLT3 positive (92 %) and negative patients (74 %) [10]. ATRA is known to have multiple effects in AML cells. In vitro studies have suggested that ATRA induces differentiation not only in AML-M3, but also in other subtypes of AML [11]. In HL-60 cell lines, ATRA induces differentiation and apoptosis by decreasing intracellular Bcl-2 [12]. In AML cell lines ATRA has been shown to increase sensitivity to Ara-C [13]. ATRA is also known to enhance apoptosis that is induced by FLT3 inhibitors in FLT3-ITD-positive AML cells [14]. In addition, ATRA has been shown to differentially modulate several cellular adhesion molecules in APL as well as non-APL cells [15]. These adhesion molecules are known to play a significant role in myeloid differentiation, stem cell mobilization and chemosensitization of the leukemic cells. Interaction of the bone marrow microenvironment with leukemic stem cells plays a crucial role in the pathogenesis of AML [16]. Moreover, addition of ATRA to induction therapy has shown to produce superior results in AML patients over 60 years of age [17]. We hence designed this phase I study combining midostaurin along with ATRA and CLAG chemotherapy to identify the MTD of midostaurin in this combination.
Materials and methods
This was a single-institutional, open-label, limited dose escalation phase I study designed to evaluate midostaurin administered orally at 2 dose levels (25 and 50 mg twice daily) in combination with ATRA and CLAG chemotherapy in patients with relapsed/refractory AML. We chose 2 doses instead of 3 doses since it has been known that at doses higher than 50 mg twice daily there is auto-induction of metabolism leading to similar systemic levels of the drug. In addition, there were higher gastrointestinal toxicities observed in previous studies at 75 mg twice daily dosing. The study was conducted in compliance with the Declaration of Helsinki, and the applicable local and national regulations.
Objectives
The primary objective was to determine the safety and toxicity of midostaurin in combination with ATRA and CLAG in relapsed refractory AML and identify the MT of midostaurin in this combination. The secondary objectives were to evaluate the response rate and to study the pharmacokinetics of midostaurin and ATRA in this combination.
Eligibility
Patients ≥18 years with relapsed or refractory AML were included. Relapsed AML was defined as any evidence of disease recurrence after achieving CR. Refractory AML was defined as failure to achieve CR after 2 cycles of induction chemotherapy or persistence of >40 % blasts after one cycle of induction chemotherapy. Other eligibility criteria included: (1) aspartate transaminase (AST) and alanine transaminase (ALT) ≤1.5× upper limit of normal (ULN); (2) serum bilirubin ≤1.5× ULN and 3) Serum creatinine ≤1.5× ULN. Patients with APL, central nervous system involvement and patients with significant history of congestive heart failure, cardiac arrhythmias and prolonged QTc interval were excluded from the study.
Treatment plan
The treatment regimen consisted of CLAG induction regimen (cladribine 5 mg/m2 given intravenously on days 2–6, Ara-C 2 g/m2 given intravenously on days 2–6, G-CSF 300 μg given subcutaneously on days 1–6), ATRA 15 mg/m2 given orally in two divided doses daily on days 7–20, midostaurin 25 mg (cohort 1) or 50 mg (cohort 2) orally twice daily on days 7–20 (Fig. 1). Response was assessed by a bone marrow examination done on days 28–45. If no dose-limiting toxicity (DLT) was observed within the first 28 days in any of the patients in cohort 1, enrollment commenced at the next dose level. It was required that 6 patients be enrolled at the MTD. Eligible and suitable patients were allowed to undergo allogeneic stem cell transplantation after the treatment. For ineligible patient or patient with no suitable donors, a second cycle of the same treatment regimen was offered.
Response definition
Treatment response was assessed according to International Working Group criteria [18]. Patients were monitored for safety by assessing all adverse events according to the National Cancer Institute Common Terminology Criteria for Adverse Events version 4.0. Other safety evaluations included complete blood count and serum chemistries, vital signs, physical examination, bone marrow aspirate and biopsy.
Statistical methods
Dose escalations were carried out in standard ‘3+3’ design, but with only 2 dose cohorts (midostaurin 25 mg dose cohort and midostaurin 50 mg dose cohort). Occurrence of DLT in the first cycle in any patient was cause for the addition of at least 3 additional patients at that dose level. All patients who received therapy on study were considered evaluable for toxicity. DLT was defined as non-hematological toxicity ≥3 (NCI common criteria version 4) considered possibly related to study drug. The MTD is defined as the dose combination that caused drug-related grade 3/4 non-hematologic toxicity in one-third or more of the patients treated. All patients provided written informed consent.
Results
Patient characteristics
Eleven patients were enrolled in the study (4 in cohort 1 and 7 in cohort 2) (Table 1). The median age was 52 years (range 32–71, SD 10.9) and 5 (45 %) were male. Nine (82 %) had relapsed AML and 2 (18 %) were refractory to initial induction chemotherapy (first relapse, 7; second relapse, 2; refractory after first induction, 2). FLT-3 mutation was positive in 6 patients (5 ITD and 1 D835 mutations), negative in 4 and unknown in 1. 2 patients had complex karyotype cytogenetics. The ECOG performance score was 0 for all enrolled patients.
Treatment
Of the 11 patients enrolled in the study, 1 withdrew consent prior to starting the treatment. The remaining 10 patients (4 in cohort 1 and 6 in cohort 2) were evaluable for toxicity. One patient in cohort 1 died on day 14 of treatment due to pulmonary hemorrhage, which was unrelated to the study drug, and hence only the remaining 9 (3 in cohort 1 and 6 in cohort 2) were evaluable for response (Table 2).
Safety and adverse events
There was no DLT observed in any of the cohorts and hence MTD was not reached. Grade 3/4 hematological toxicity was seen in 100 % of patients as expected. 8 patients had grade 3/4 non-hematological toxicity not related to midostaurin or ATRA (hyperglycemia, 3 patients; pneumonia, 2 patients; sepsis, 2 patients; sinusitis, 1 patient; hypokalemia, 1 patient; hyperkalemia, 1 patient; hyponatremia, 1 patient; and hypertriglyceridemia, 1 patient). One patient had grade 5 pulmonary hemorrhage attributed to thrombocytopenia that resulted in death on day 14 and was considered not attributed to the study drugs. Significant hepatotoxicity (grade 3/4) was not observed in our two dosing cohorts, which is likely due to avoiding the concomitant use of azoles with midostaurin and ATRA in this study.
Pharmacokinetics
We performed pharmacokinetic studies to study the potential drug–drug interaction between midostaurin and ATRA. We measured ATRA and midostaurin levels on day 7 of Cycle 1 at baseline and 4, 8 and 12 h post administration in cohorts 1 and 2 (midostaurin level 25 and 50 mg, respectively) as presented on Fig. 1. The bioanalytical analysis using LC–MS/MS method formidostaurin, its metabolites and ATRA performed at SGS Life Science Service (St Benoit, France). The LLOQs were 10 and 1.00 ng/ml for midostaurin CGP62221, CGP52421 and for ATRA, respectively. Midostaurin concentrations were similar to those already reported at the same dose levels. No drug–drug interaction between midostaurin and ATRA was observed as shown on Fig. 2.
Pharmacokinetic studies of midostaurin and ATRA. a Mean concentration (±standard deviation) of midostaurin and midostaurin metabolite (CGP52421 and CGP62221) at base line and 2, 4, 6 and 12 h post-ingestion after a single dose (Cycle 1, day 7). b Mean concentration (±standard deviation) of ATRA levels at on day 7 Cycle 1 at base line and 2, 4, 6 and 12 h post-ingestion when administrated with midostaurin at 25 mg (closed circle) and at 50 mg (closed triangle)
Response
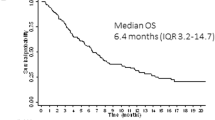
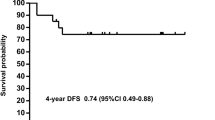
Overall 2 patients (22 %) achieved CR and 1 patient (11 %) achieved CR with partial count recovery. 5 patients died and the causes of death were progressive disease in 4 and respiratory failure secondary to pulmonary hemorrhage in 1. Median overall survival was 106 days (range 26–338). 8 patients died after day 50 due to progressive disease. There was one long-term survivor. Interestingly, in one of the patients the relapsed AML blasts converted from FLT3 ITD positive to negative suggesting the possibility of FLT3-negative clone emerging after therapy.
Discussion
Our study suggests that the combination of CLAG with midostaurin and ATRA regimen appears to have an acceptable toxicity profile for relapsed/refractory AML. The dose of midostaurin in this combination is identified to be 50 mg orally twice daily. Of note is the significant paucity of liver toxicity, which is likely due to avoiding concurrent administration of azoles with ATRA and midostaurin. Our pharmacokinetic data suggest that there is no major interaction between midostaurin and ATRA in this combination.
The less than expected response rate in this patient population is likely due to poor risk patients having had multiple prior treatments and also from the possible lack of anthracyclines in the regimen. The dose and schedule of ATRA in this study was modified based on the dosing schedule by Schlenk et al. [17]. It is possible that a higher dose and a longer duration of treatment with ATRA and/or midostaurin may yield better outcomes.
It is increasingly clear that AML is a multiclonal disease with possibly different clones harboring alterations in different pathogenic pathways. Hence, it is imperative that we develop therapeutic strategies to target multiple pathways to achieve cure in AML. Our study shows the feasibility of adding a multi-kinase inhibitor to salvage chemotherapy in AML. A phase 2 study to assess the effectiveness of this regimen in relapsed refractory AML is warranted.
The trial was registered under clinicaltrials.gov number: NCT01161550.
Abbreviations
- AML:
-
Acute myelogenous leukemia
- CLAG:
-
Cladribine 5 mg/m2 given intravenously on days 2–6, Ara-C 2 g/m2 given intravenously on days 2–6, G-CSF 300 μg given subcutaneously on days 1–6
- ATRA:
-
All-trans retinoic acid
- ICTS:
-
Institute for Clinical and Translational Science
- Ara-C:
-
Cytarabine
- G-CSF:
-
Granulocyte colony stimulating factor
- MDS:
-
Myelodysplastic syndrome
- CR:
-
Complete remission
- PR:
-
Partial remission
- CRi:
-
Complete remission with incomplete count recovery
- MTD:
-
Maximum tolerated dose
- DLT:
-
Dose-limiting toxicity
References
Kornblau SM, Womble M, Qiu YH, Jackson CE, Chen W, Konopleva M, et al. Simultaneous activation of multiple signal transduction pathways confers poor prognosis in acute myelogenous leukemia. Blood. 2006;108(7):2358–65.
Price SL, Lancet JE, George TJ, Wetzstein GA, List AF, Ho VQ, et al. Salvage chemotherapy regimens for acute myeloid leukemia: is one better? Efficacy comparison between CLAG and MEC regimens. Leuk Res. 2011;35(3):301–4.
Holowiecki J, Grosicki S, Giebel S, Robak T, Kyrcz-Krzemien S, Kuliczkowski K, et al. Cladribine, but not fludarabine, added to daunorubicin and cytarabine during induction prolongs survival of patients with acute myeloid leukemia: a multicenter, randomized phase III study. J Clin Oncol. 2012;30(20):2441–8.
Walker AR, Komrokji RS, Ifthikharuddin J, Messina P, Mulford D, Becker M, et al. Phase I study of cladribine, cytarabine (Ara-C), granulocyte colony stimulating factor (G-CSF) (CLAG Regimen) and simultaneous escalating doses of imatinibmesylate (Gleevec) in relapsed/refractory AML. Leuk Res. 2008;32(12):1830–6.
Santos FP, Jones D, Qiao W, Cortes JE, Ravandi F, Estey EE, et al. Prognostic value of FLT3 mutations among different cytogenetic subgroups in acute myeloid leukemia. Cancer. 2011;117(10):2145–55.
Kindler T, Lipka DB, Fischer T. FLT3 as a therapeutic target in AML: still challenging after all these years. Blood. 2010;116(24):5089–102.
Fabbro D, Ruetz S, Bodis S, Pruschy M, Csermak K, Man A, et al. PKC412—a protein kinase inhibitor with a broad therapeutic potential. Anticancer Drug Des. 2000;15(1):17–28.
Millward MJ, House C, Bowtell D, Webster L, Olver IN, Gore M, et al. The multikinase inhibitor midostaurin (PKC412A) lacks activity in metastatic melanoma: a phase IIA clinical and biologic study. Br J Cancer. 2006;95(7):829–34.
Fischer T, Stone RM, Deangelo DJ, Galinsky I, Estey E, Lanza C, et al. Phase IIB trial of oral midostaurin (PKC412), the FMS-like tyrosine kinase 3 receptor (FLT3) and multi-targeted kinase inhibitor, in patients with acute myeloid leukemia and high-risk myelodysplastic syndrome with either wild-type or mutated FLT3. J Clin Oncol Off J Am Soc Clin Oncol. 2010;28(28):4339–45.
Stone RM, Fischer T, Paquette R, Schiller G, Schiffer CA, Ehninger G, et al. Phase IB study of the FLT3 kinase inhibitor midostaurin with chemotherapy in younger newly diagnosed adult patients with acute myeloid leukemia. Leukemia Off J Leuk Soc Am Leuk Res Fund UK. 2012;26(9):2061–8.
Manfredini R, Trevisan F, Grande A, Tagliafico E, Montanari M, Lemoli R, et al. Induction of a functional vitamin D receptor in all-trans-retinoic acid-induced monocytic differentiation of M2-type leukemic blast cells. Cancer Res. 1999;59(15):3803–11.
Delia D, Aiello A, Soligo D, Fontanella E, Melani C, Pezzella F, et al. bcl-2 proto-oncogene expression in normal and neoplastic human myeloid cells. Blood. 1992;79(5):1291–8.
Freund A, Rossig C, Lanvers C, Gescher A, Hohenlochter B, Jurgens H, et al. All-trans-retinoic acid increases cytosine arabinoside cytotoxicity in HL-60 human leukemia cells in spite of decreased cellular ara-CTP accumulation. Ann Oncol Off J Eur Soc Med Oncol ESMO. 1999;10(3):335–8.
Scholl S, Muller R, Clement JH, Loncarevic IF, Bohmer FD, Hoffken K. ATRA can enhance apoptosis that is induced by Flt3 tyrosine kinase inhibition in Flt3-ITD positive cells. Leuk Res. 2006;30(5):633–42.
Di Noto R, Schiavone EM, Lo Pardo C, Ferrara F, Manzo C, Vacca C, et al. Differential regulation of GPI-linked molecules on leukaemic promyelocytes treated in vitro with all-trans retinoic acid. Br J Haematol. 1996;93(2):392–3.
Nwajei F, Konopleva M. The bone marrow microenvironment as niche retreats for hematopoietic and leukemic stem cells. Adv Hematol. 2013;2013:953–82.
Schlenk RF, Frohling S, Hartmann F, Fischer JT, Glasmacher A, del Valle F, et al. Phase III study of all-trans retinoic acid in previously untreated patients 61 years or older with acute myeloid leukemia. Leukemia Off J Leuk Soc Am Leuk Res Fund UK. 2004;18(11):1798–803.
Cheson BD, Bennett JM, Kopecky KJ, Buchner T, Willman CL, Estey EH, et al. Revised recommendations of the International Working Group for diagnosis, standardization of response criteria, treatment outcomes, and reporting standards for therapeutic trials in acute myeloid leukemia. J Clin Oncol. 2003;21(24):4642–9.
Conflict of interest
C.N.A. obtained research support for this study from Novartis and serves in the advisory board for Novartis.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ramsingh, G., Westervelt, P., McBride, A. et al. Phase I study of cladribine, cytarabine, granulocyte colony stimulating factor (CLAG regimen) and midostaurin and all-trans retinoic acid in relapsed/refractory AML. Int J Hematol 99, 272–278 (2014). https://doi.org/10.1007/s12185-014-1503-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-014-1503-4