Abstract
Follicular lymphomas (FL) account for 30% of non-Hodgkin’s lymphomas (NHL). Their evolution is heterogeneous. Some patients present with indolent forms undergoing several relapses while in other patients the disease evolves abruptly toward aggressive NHL. This is why accurate prognostic indices are required so that treatment strategies may be optimized for each patient and so that trials may be conducted in groups of patients that are as homogeneous as possible. The Follicular Lymphoma International Prognostic Index (FLIPI) has been designed to separate patients into 3 groups with significantly different hazard ratios for death. Its accuracy has been confirmed in several studies. The FLIPI2 was designed more recently to separate patients with significantly different hazard ratios for progression/relapse in the era of anti-CD20 monoclonal antibody treatments. Gene profile studies have shown that the prognosis of FL is mainly related to the type, number, and activation of immune cells in the microenvironment of lymphomatous follicles. Immunohistochemical studies suggest that macrophages, CD4+ T cells and among them T-regulatory cells (T-regs) and programed death-1 cells (PD-1 cells) play a major role in the outcome of FLs. However, additional confirmatory studies are required due to discrepancies in results. Up to now, these biological study results are more useful for approaching the pathophysiology of FL rather than to be used as prognostic tools in clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Follicular lymphomas (FL) account for approximately 30% of all non-Hodgkin lymphomas (NHL) in western countries, with a lower incidence in Asian countries. Several retrospective analyses have clearly shown an important improvement in overall survival of FL patients in the last 15 years when compared to historical controls [1, 2]. This improvement is mainly related to the introduction of anti-CD20 monoclonal antibodies (MoAbs) in the treatment arsenal.
Despite these new treatment approaches, there is no consensus concerning the initial treatment FL patients should receive. Patients may be followed without treatment until progression, may be initially treated with rituximab alone, or with a combination of rituximab and various cytotoxic chemotherapies. In some centers, patients with what is considered as advanced disease may even receive high-dose therapy with autologous stem cell transplantation (ASCT). Given the multitude of treatment options, several studies have been conducted in the last 15 years to determine clinical and biological prognostic factors and to propose prognostic indices. The aims of a prognostic index are (1) for a given patient, to help in choosing the treatment the most appropriate for a probable clinical course; (2) to compare the clinical and biological characteristics of the clinical trials reported in the literature; (3) to prospectively design a clinical trial in a subpopulation of FL patients who will most probably follow a homogeneous course.
This review will focus on the analysis of all these prognostic factors and their contribution to the choice of treatment for FL patients.
2 History
The first prognostic classification of FL relied on pathological criteria and was formalized in 1981 in the Working Classification for Clinical Usage [3]. It separated FL into 3 categories, i.e. small-cell, mixed-cell, and large-cell FL. Several reports confirmed the relevance of this classification, especially the poorer prognosis of follicular large-cell lymphomas. However, it rapidly appeared that there was little consensus among pathologists concerning the distinction between these 3 categories, and the clinical accuracy of this classification was thus found to be limited.
Between 1985 and 1990, two groups, the Groupe d’Etude des Lymphomes Folliculaires (GELF) from France and the British National Lymphoma Investigation Group (BNLI) simultaneously determined clinical prognostic criteria with the main goal of identifying a subgroup of patients for whom a ‘no initial treatment policy’ could be proposed [4] (Table 1). Both sets of criteria were found to be very similar. Although the GELF criteria were chosen from the clinical experience of experts, they enabled separation of FL patients into 2 groups, i.e. ‘low’ versus ‘high’ tumor burden, and these two groups showed significantly different overall survival [5].
Since 1993, the International Prognostic Index (IPI) has been confirmed as the ‘gold standard’ of clinical indices for aggressive NHLs [6]. Several groups have tested the IPI in FL patients, and all of them have shown that the IPI could discriminate FL patients into subgroups with significantly different survivals [7–9]. However, when applied to FL or other indolent lymphomas, the IPI has several drawbacks [10] since:
-
the statistical analysis used to build this index was applied only to patients with aggressive lymphomas and parameters which have a prognostic influence in FL but not in aggressive lymphomas could have been missed;
-
conversely, other parameters of the IPI could have no influence on the prognosis of FL. This holds true for performance status (PS) since very few patients with FL initially have a poor PS;
-
the distribution of patients into IPI prognostic subgroups is very heterogeneous, e.g. patients with high-risk IPI represent less than 15% of FL patients at diagnosis.
Since the IPI was found to be poorly differentiating for patients with FL, an international study was initiated with the aim of proposing a specific index for FL patients.
3 Follicular lymphoma international prognostic indices
In 2004, the Follicular Lymphoma International Prognostic Index (FLIPI) was built from a retrospective analysis of more than 4000 patients with FL treated between 1985 and 1992 [11]. After a multivariate analysis, 5 parameters were used to build this index: age >60 versus ≤60 years, serum LDH level >upper limit of normal (UPLN) versus ≤UPLN, number of nodal areas >4 versus ≤4, hemoglobin level <120 versus ≥120 g/L. Three risk groups (low, intermediate, and high) were distinguished. The distribution of patients and the hazard ratios (HR) for overall survival (OS) are given in Table 2. The survival curves of the 3 groups are shown in Fig. 1. Several retrospective analyses of other groups comprising patients treated according to various approaches have confirmed the accuracy of the FLIPI with similar distributions of patients and remarkably similar differences in hazard ratios for death between prognostic subgroups being found [9, 12, 13]. The FLIPI can thus be considered as a standard prognostic index for FLs. Furthermore, the FLIPI has more recently been used as a prognostic index for progression-free survival (PFS) [14, 15]. It should be underlined that the FLIPI was not designed for such analyses since, at the time of data collection, there was no consensus on the definition of PFS. However, despite this, the FLIPI may be used to accurately distinguish 3 groups of patients with significantly different PFS rates. It is especially convenient for patients receiving immunochemotherapy such as rituximab–cyclophosphamide–vincristine–prednisone (R-CVP) [15] or rituximab–cyclophosphamide–doxorubicin–vincristine–prednisone (R-CHOP) [14].
Survival of the 1795 patients according to risk group as defined by the Follicular Lymphoma International Prognostic Index. This research was originally published in Blood 2004 (Solal-Celigny P, Roy P, Colombat P, et al. Follicular lymphoma international prognostic index. Blood. 2004;104:1258–65. ©the American Society of Hematology)
The FLIPI represented a major step forward in the knowledge of clinical prognostic factors in FL. However, some of its limits have recently been outlined:
-
1.
The FLIPI was designed with OS as the endpoint and, because of the recent improvement in survival of FL patients, this endpoint requires a too-long follow-up period to collect a number of events sufficient for statistical analysis. In addition, PFS has become the primary endpoint in all clinical trials as recommended by consensus [16].
-
2.
At the time of the analysis, some important clinical and biological parameters were not routinely collected and therefore were not used to build the FLIPI, i.e. size of the largest tumor mass and serum β2 microglobulin levels.
-
3.
When treated, the patients used to build the FLIPI received conventional chemotherapy, and most of them were never treated, even at the time of relapse(s), with modern immunotherapy, such as rituximab or radioimmunotherapy. The patients included in the initial FLIPI are therefore not representative of FL patients today.
These reasons lead our group to initiate a new prognostic factor study using PFS as the endpoint and integrating all the modern parameters prospectively collected in the univariate and multivariate analyses. The FLIPI2 thus built relies on 5 prognostic parameters: longest diameter of the largest tumor mass >6 versus ≤6 cm, serum β2 microglobulin level >UPLN versus ≤UPLN, bone marrow involved or not, hemoglobin level ≤120 versus >120 g/L, and age >60 versus ≤60 years [17].
The distribution of patients and hazard ratios for progression are provided in Table 3. A recently published retrospective analysis of 280 patients from another group confirmed the accuracy of the FLIPI2 for PFS (as well as that of the FLIPI) and showed notably that the initial median PFS of a group of approximately 20–25% of patients with FL is approximately 2.5 years despite rituximab-based immunochemotherapy which indicates the need for the development of innovative approaches [18].
However, the FLIPI2 still requires confirmation and could be used to complete the FLIPI, with the former being used for PFS, and the latter for OS.
4 Response to treatment
Response to treatment has been shown to be a paramount prognostic factor for OS in many clinical trials before the rituximab era [19, 20]. The advent of immunotherapy has changed this situation since the addition of rituximab to standard chemotherapy improves response rates as well as time to treatment failure, PFS, and OS [15, 21, 22]. In the rituximab era, prospective trials clearly show that patients reaching complete remission enjoy a prolonged duration of response compared to partial responders [15, 23]. As a consequence, response rate—the only prognostic factor that can be influenced—may become a major goal for clinicians in the future. For the time being, response criteria are based on CT scan and/or bone marrow biopsy if initially involved [24]. There are many other ways to explore response to treatment. Positron emission tomography is promising, but its prognostic value remains to be determined in prospective trials [25]. A recent prospective study evaluated the value of Bcl2/IgH genomic PCR in blood and/or bone marrow [26]. A Bcl-2/IgH-positive bone marrow PCR at diagnosis was an adverse prognostic factor for PFS. However, neither pre-treatment nor post-induction Bcl2/IgH levels in peripheral blood could predict a prolonged PFS. Moreover, patients with a positive post-maintenance Bcl-2/IgH peripheral blood or bone marrow PCR relapsed earlier than patients with a negative post-maintenance PCR [26].
5 Prognostic influence of cytogenetic abnormalities in follicular lymphoma
More than 90% of FLs express high levels of Bcl-2 protein, related in most cases, to a t(14;18) translocation. For unknown reasons, this incidence is lower in Asian countries [27]. However, in the Bcl-2-negative variants of FL, alternative molecular pathways and anti-apoptotic routes result in a similar prognosis. An exceptional Bcl-2-negative subtype of FL with a predominant localized involvement of inguinal nodes, 1p deletion, and a good prognosis has been recently described [28].
In one study, initial pre-treatment quantitative evaluation of marrow involvement by t(14;18) positive cells by RT-PCR was predictive of outcome after R-CHOP immunochemotherapy [29]. However, this prognostic evaluation and its usefulness have not been confirmed. Since the initial studies after autologous stem transplantation, molecular remission—as defined by the disappearance of bcl2/IgH-positive cells in the blood and in the bone marrow—was considered as predictive of a good prognosis. However, several drawbacks have considerably decreased the interest of such a ‘molecular remission’: (1) around 30% of patients are negative at initial presentation when using routine PCR techniques and cannot be followed; (2) normal subjects may have a small number of t(14;18) positive cells; (3) several studies have shown that patients—especially when treated only with radiation therapy for localized disease—enjoy remissions of very long duration despite having t(14;18) positive cells in the blood; and (4) when treated with anti-CD20 monoclonal antibodies, a very high number of patients reach ‘molecular remission’, and thus the negative predictive value is low. Quantitative evaluations of the numbers of t(14;18) did not improve significantly the predictive value. Tests for ‘molecular remission’ in FLs have not to be used in routine practice. The persistence of t(14;18) positive cells in the blood or in the marrow after initial treatment does not have to influence the post-induction management.
The majority of FL cells carry karyotypic abnormalities in addition to the t(14;18) translocation. Some abnormalities are recurrent and have a prognostic influence. Among them, −6q, −17p are clearly associated with a poor prognosis and an increased risk of transformation, while +der18q, +7, +8 typically correlate with an indolent course [30, 31]. However, karyotypic analysis of FL lymph nodes is rarely performed since (1) it requires an immediate preparation of a cell suspension after excisional biopsy, (2) karyotypic abnormalities with many different clones are frequently observed in FL, and (3) conventional cytogenetic analysis is cumbersome and rarely yields clinically meaningful results.
6 The prognostic role of the microenvironment in follicular lymphomas
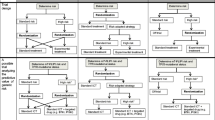
The surrounding population of the non-malignant immune regulatory cells—i.e. the microenvironment—plays a major role in the pathogenesis and the behavior of FL (Fig. 2). The intimate relationship between the tumor microenvironment and neoplastic cells implies a dynamic cross-talk in which tumor cells may give and receive instructions through a complex system. Several lines of investigations have highlighted that FL is an immunologically functional disease in which an active interaction between tumor cells and the functional composition of the microenvironment determines the prognosis and response to treatment.
Intrafollicular and interfollicular microenvironment of follicular lymphomas (FL) cells are present within the follicle and in the interfollicular area. They are surrounded by tissue macrophages (CD68) and T cells which are mostly CD4+ T cells with fewer CD8+ T cells. Among CD4+ T cells T-regulatory cells (T-regs) and programed death-1 T cells (PD-1) play a special role. Most cells (Mast) also influence FL cells (see text for details)
First, gene expression profiling studies have revealed that survival after initial diagnosis of FL can be predicted by biological differences in tumors. However, in contrast with results observed in DLBCL where prognosis is closely related to the gene profile of tumor cells, application of this approach to FL identified two prognostic signatures based on non-malignant tumor-infiltrating cells indicative of the host immune response [32] rather than on the characteristics of the tumor cells as in DLBCL. The ‘immune-response 1’ signature includes genes encoding T-cell markers (e.g. CD7, CD8B1, ITK, LEF1, and STAT4) and genes that are highly expressed in macrophages (e.g. ACTN1 and TNFSF3B). This signature was associated with a good prognosis. In contrast, the ‘immune-response 2’ signature was associated with a poor prognosis. It includes genes expressed in macrophages, dendritic cells or both (e.g. TLR5, FCGR1A, SEPT10, CCR1, LGMN, and C3AR1). Some of these genes appear especially strong predictors such as CD7 for immune-response 1 and CCR1 for immune-response 2 [33]. These immune signatures influenced the prognosis independently of known clinical prognostic factors, but have not been tested with the FLIPI. The median OS of the 4 quartiles of the survival-predictor score according to gene signatures were, respectively, 13.6, 11.1, 10.8, and 3.9 years (p < 0.0001) [32]. These results have been confirmed by other studies [33, 34]. However, measurement of these marker genes in routine practice is cumbersome and costly, and the results are very difficult to interpret on a single patient basis.
Immunohistochemical (IHC) studies were therefore developed to better characterize the FL microenvironment and its influence on disease outcome. However, in order to analyze these studies, some technical caveats must be detailed: the immunochemical studies were performed using flow cytometry [35], or immunohistochemistry on conventional paraffin-embedded whole tissue sections [36] or on tissue microarrays (TMA). The former technique allows only a quantitative analysis of cell subpopulations while the two latter methods also study the distribution of cell subpopulations within the lymph nodes. Second, these IHC techniques rely on the counting of cells positive for a marker specific for a subpopulation. This counting may yield very different results according to (1) the choice of the area, either at random or where the number of positive cells seems the highest; (2) the magnification of the selected power field on the microscope; and (3) visual counting by one or several pathologists or quantification using an automated scanning microscope. Third, analyses are usually performed after separation of the results into 2 or 3 categories with each study using different thresholds which makes it very difficult to compare published results. Fourth, involved lymph node infiltration by lymphoma cells and immune cells is heterogeneous, schematised by two compartments, i.e. the follicle itself and the interfollicular area. Cells can locate predominantly in one of these areas or diffusely infiltrate the lymph node. The prognostic significance of follicular, interfollicular, or diffuse infiltration may be very different, adding to the complexity of IHC studies. Despite this, the knowledge of the FL microenvironment—and consequently its influence on the pathogenesis and on the prognosis of the disease—has improved vastly in recent years. Of the various cell types that play a role in the microenvironment of FL, macrophages and T cells are those that have been most extensively studied.
Early studies strongly suggested that a high number of tumor-associated CD68+ macrophages (TAM) in FL lesions were correlated with a poor prognosis [37]. However, this prognostic factor was observed only in some of the studies carried out in patients treated with conventional chemotherapy [37, 38], but not in all [34, 39].
Conversely, in patients treated with rituximab plus chemotherapy, a high number of TAM either had no influence on prognosis [36, 38] or was even associated with a good prognosis [39]. These opposite results on the prognostic role of TAM depending on treatment are most likely related to the critical role of macrophages in B-cell depletion after anti-CD20 therapy through their functions in antibody-dependent cell toxicity (ADCC) [39]. Since nowadays, almost all patients with FL who require an initial treatment are treated with an anti-CD2O MoAb, the prognostic influence of TAM infiltration is at best very limited.
The FL lymph nodes contain numerous T cells with a normal phenotype [40]. Around 75% of these CD3+ cells are helper CD4+ T cells, the remaining being CD8+ cells and a very small percentage CD4+ CD8+ cells. Most of the T cells are located in the interfollicular areas rather than in the follicle (Fig. 2).
Several subpopulations of CD4+ cells play a major role in the pathogenesis and the growth of neoplastic B cells. The overexpression of Bcl-2 protein is not sufficient to allow the growth of FL cells: when incubated in vitro, FL cells rapidly undergo apoptosis. The most important protection of FL cells against apoptosis is based on intimate interaction within the germinal center (GC) between a subpopulation of CD4+ cells carrying the CD40L (CD154) and FL B cells carrying CD40 [41, 42]. Some agents, such as TRAIL, a member of the TNF superfamily, may counteract the antiapoptotic effects of the CD40–CD40L pair, which is just one example of the potential therapeutic effect that may be obtained by acting on the FL cell microenvironment.
A high number of follicular CD4+ cells was associated with long survival in one study [38] while the opposite effect was observed in another trial [43].
Other CD4+ cells influence FL evolution and risk of transformation. Regulatory CD4+ T cells (T-regs) account for 5–10% of CD4+ T cells. They are characterized mainly by the coexpression of CD25, a marker of activated/memory cells, and of forkhead transcription factor 3 (FOXP3). Most of the T-regs are constitutively produced in the thymus. However, FL cells, as opposed to normal B cells, have the unique capacity to convert effector T cells into T-regs through stimulation of the T-cell receptor [44, 45] (Fig. 3) T-regs regulate T-cell activation and restore immune homeostasis by acting on CD4 and CD8 activated T cells after their response to antigen [46]. T-regs act by intimate contact with T cells and through production and release of Interleukin 10 and Transforming Growth Factor β. Most importantly, T-regs participate in the immune response against tumor cells. In several models of solid tumors, T-regs suppress tumor-specific T-cell immunity, thereby contributing to cancer growth, and a high number of T-regs is correlated with a decreased survival [47]. Conversely, several studies have shown that a high number of T-regs in FL is associated with a good prognosis and a reduced risk of transformation [38, 48]. In a recently published study, the architectural pattern of T-regs infiltration in FL nodes had a crucial role: while a diffuse pattern was associated with a good prognosis, a follicular or perifollicular pattern was correlated with poor prognosis [49]. In other studies, the number of T-regs did not have any prognostic influence per se [34, 50]. T-regs could inhibit FL growth by negatively regulating germinal center (GC) Thelper (Th) cells and GC-Th cell-induced B cell survival [51]. The precise role of T-regs in FL has to be better determined since there are several potential therapeutic approaches to enhance or to reduce T-reg function [46]. The main interest of T-reg infiltration studies in FL relies most probably on determining the reasons of different and possibly opposite effects between solid tumors and FL. Because of the technical caveats previously detailed and the discrepant results of studies, their usefulness as a prognostic tool requires additional confirmatory studies.
T-regulatory cells (T-regs) originate from the thymus (innate T-regs) or from activation by follicular lymphoma (FL) cells (adaptive T-regs). They may act by inhibiting the CD4+ T cells which prohibit FL cells from apoptosis by binding to the CD40 antigen of FL cells through CD40 ligand (CD40L). They may also inhibit germinal center T helper (Th) cells which also promote FL B-cell survival
Programed death-1 cell (PD-1) or CD279 is a member of the CD28 superfamily of membrane receptors that have an important function in the regulation of immune responses and in the tolerance to self-antigens and also to tumor cells. PD-1 is expressed by various lymphoid and non-lymphoid cells, including CD4+ cells. In the germinal center, PD-1 is mainly expressed by CD4+ CD25-FOXP3 cells. PD-1 acts through binding to one of two ligands, i.e. PDL-1 and PDL-2 expressed by a variety of hematopoietic and non-hematopoietic cells including germinal B cells [52]. While PD-L1 expression on renal, gastric, or breast carcinoma cells is correlated with a poor prognosis [53], the opposite has been observed in FL. In a study from Carreras et al. [54], the number of PD-1-positive cells infiltrating the tumor was positively correlated with survival in patients with FL, independently of the FLIPI. Similar results were obtained by another group [43]. It is especially curious that both T-regs and PD-1 cells seem to have opposite effects in solid tumors and in FL, favoring immune surveillance escape and tumor growth in the former and inhibiting proliferation in the latter.
In summary, all these studies of the microenvironment in FL have yielded fascinating results, but have not yet enabled a simple strategy of interaction with FL cells. As mentioned by Wahlin et al. [43], prognosis in FL is affected by several immune cell subsets simultaneously at work rather than being dictated by an individual immune cell subset.
In conclusion, FL is a complex and heterogeneous disease for which important progresses in risk evaluation have recently been reported. From a clinical point of view, the FLIPI or the FLIPI2 are simple and accurate prognostic indices that can be used in the routine management of patients with FL as well as in clinical research. Despite promising results, genetic, molecular, and other biological parameters require confirmatory and further studies before new treatment strategies can be finalized. These studies are in progress and could lead to better understanding of biology of FL and also of other neoplastic diseases in much the same way that the t(14;18) translocation resulted in the discovery of apoptosis, a major characteristic of neoplastic growth and antineoplastic treatments.
References
Swenson WT, Wooldridge JE, Lynch CF, Forman-Hoffman VL, Chrischilles E, Link BK. Improved survival of follicular lymphoma patients in the United States. J Clin Oncol. 2005;23:5019–26.
Liu Q, Fayad L, Cabanillas F, Hagemeister FB, Ayers GD, Hess M, et al. Improvement of overall and failure-free survival in stage IV follicular lymphoma: 25 years of treatment experience at The University of Texas M.D. Anderson Cancer Center. J Clin Oncol. 2006;24:1582–9.
National Cancer Institute sponsored study of classifications of non-Hodgkin’s lymphomas: summary and description of a working formulation for clinical usage. The Non-Hodgkin’s Lymphoma Pathologic Classification Project. Cancer. 1982;49:2112–35.
Decaudin D, Lepage E, Brousse N, Brice P, Harousseau JL, Belhadj K, et al. Low-grade stage III-IV follicular lymphoma: multivariate analysis of prognostic factors in 484 patients—a study of the Groupe d’Etude des Lymphomes de l’Adulte. J Clin Oncol. 1999;17:2499–505.
Brice P, Bastion Y, Lepage E, Brousse N, Haioun C, Moreau P, et al. Comparison in low-tumor-burden follicular lymphomas between an initial no-treatment policy, prednimustine, or interferon alfa: a randomized study from the Groupe d’Etude des Lymphomes Folliculaires. J Clin Oncol. 1997;15:1110–7.
A predictive model for aggressive non-Hodgkin’s lymphoma. The International Non-Hodgkin’s Lymphoma Prognostic Factors Project. N Engl J Med. 1993;329:987–94.
Lopez-Guillermo A, Montserrat E, Bosch F, Terol MJ, Campo E, Rozman C. Applicability of the International Index for Aggressive Lymphomas to patients with low-grade lymphoma. J Clin Oncol. 1994;12:1343–8.
Bastion Y, Coiffier B. Is the International Prognostic Index for Aggressive Lymphoma patients useful for follicular lymphoma patients? J Clin Oncol. 1994;12:1340–2.
Perea G, Altes A, Montoto S, Lopez-Guillermo A, Domingo-Domenech E, Fernandez-Sevilla A, et al. Prognostic indexes in follicular lymphoma: a comparison of different prognostic systems. Ann Oncol. 2005;16:1508–13.
Solal-Celigny P. What is the optimal prognostic tool for the assessment of patients with newly diagnosed follicular lymphoma? Leuk Lymphoma. 2007;48:452–3.
Solal-Celigny P, Roy P, Colombat P, White J, Armitage JO, Arranz-Saez R, et al. Follicular Lymphoma International Prognostic Index. Blood. 2004;104:1258–65.
Formica V, Norman AR, Cunningham D, Wotherspoon A, Oates J, Chong G. Utility of the Follicular Lymphoma International Prognostic Index and the International Prognostic Index in assessing prognosis and predicting first-line treatment efficacy in follicular lymphoma patients. Acta Haematol. 2009;122:193–9.
Arcaini L, Colombo N, Passamonti F, Burcheri S, Orlandi E, Brusamolino E, et al. Correlation of the FLIPI score for follicular lymphoma with period of diagnosis and type of treatment. Leuk Res. 2006;30:277–82.
Buske C, Hoster E, Dreyling M, Hasford J, Unterhalt M, Hiddemann W. The Follicular Lymphoma International Prognostic Index (FLIPI) separates high-risk from intermediate- or low-risk patients with advanced-stage follicular lymphoma treated front-line with rituximab and the combination of cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) with respect to treatment outcome. Blood. 2006;108:1504–8.
Marcus R, Imrie K, Solal-Celigny P, Catalano JV, Dmoszynska A, Raposo JC, et al. Phase III study of R-CVP compared with cyclophosphamide, vincristine, and prednisone alone in patients with previously untreated advanced follicular lymphoma. J Clin Oncol. 2008;26:4579–86.
Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25:579–86.
Federico M, Bellei M, Marcheselli L, Luminari S, Lopez-Guillermo A, Vitolo U, et al. Follicular lymphoma international prognostic index 2: a new prognostic index for follicular lymphoma developed by the international follicular lymphoma prognostic factor project. J Clin Oncol. 2009;27:4555–62.
Arcaini L, Merli M, Passamonti F, Rizzi S, Ferretti V, Rattotti S, et al. Validation of follicular lymphoma international prognostic index 2 (FLIPI2) score in an independent series of follicular lymphoma patients. Br J Haematol. 2010;149(3):455–7.
Buckstein R, Pennell N, Berinstein NL. What is remission in follicular lymphoma and what is its relevance? Best Pract Res Clin Haematol. 2005;18:27–56.
Bachy E, Brice P, Delarue R, Brousse N, Haioun C, Le Gouill S, et al. Long-term follow-up of patients with newly diagnosed follicular lymphoma in the prerituximab era: effect of response quality on survival—a study from the Groupe d’Etude des Lymphomes de l’Adulte. J Clin Oncol. 2010;28:822–9.
Hiddemann W, Kneba M, Dreyling M, Schmitz N, Lengfelder E, Schmits R, et al. Frontline therapy with rituximab added to the combination of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) significantly improves the outcome for patients with advanced-stage follicular lymphoma compared with therapy with CHOP alone: results of a prospective randomized study of the German Low-Grade Lymphoma Study Group. Blood. 2005;106:3725–32.
Herold M, Haas A, Srock S, Neser S, Al-Ali KH, Neubauer A, et al. Rituximab added to first-line mitoxantrone, chlorambucil, and prednisolone chemotherapy followed by interferon maintenance prolongs survival in patients with advanced follicular lymphoma: an East German Study Group Hematology and Oncology Study. J Clin Oncol. 2007;25:1986–92.
Czuczman MS, Weaver R, Alkuzweny B, Berlfein J, Grillo-Lopez AJ. Prolonged clinical and molecular remission in patients with low-grade or follicular non-Hodgkin’s lymphoma treated with rituximab plus CHOP chemotherapy: 9-year follow-up. J Clin Oncol. 2004;22:4711–6.
Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25:579–86.
Janikova A, Bolcak K, Pavlik T, Mayer J, Kral Z. Value of [18F]fluorodeoxyglucose positron emission tomography in the management of follicular lymphoma: the end of a dilemma? Clin Lymphoma Myeloma. 2008;8:287–93.
van Oers MH, Tonnissen E, Van Glabbeke M, Giurgea L, Jansen JH, Klasa R, et al. BCL-2/IgH polymerase chain reaction status at the end of induction treatment is not predictive for progression-free survival in relapsed/resistant follicular lymphoma: results of a prospective randomized EORTC 20981 phase III intergroup study. J Clin Oncol. 2010;28:2246–52.
Biagi JJ, Seymour JF. Insights into the molecular pathogenesis of follicular lymphoma arising from analysis of geographic variation. Blood. 2002;99:4265–75.
Katzenberger T, Kalla J, Leich E, Stocklein H, Hartmann E, Barnickel S, et al. A distinctive subtype of t(14;18)-negative nodal follicular non-Hodgkin lymphoma characterized by a predominantly diffuse growth pattern and deletions in the chromosomal region 1p36. Blood. 2009;113:1053–61.
Rambaldi A, Carlotti E, Oldani E, Della Starza I, Baccarani M, Cortelazzo S, et al. Quantitative PCR of bone marrow BCL2/IgH+ cells at diagnosis predicts treatment response and long-term outcome in follicular non-Hodgkin lymphoma. Blood. 2005;105:3428–33.
Tilly H, Rossi A, Stamatoullas A, Lenormand B, Bigorgne C, Kunlin A, Monconduit M, et al. Prognostic value of chromosomal abnormalities in follicular lymphoma. Blood. 1994;84:1043–9.
Hoglund M, Sehn L, Connors JM, Gascoyne RD, Siebert R, Sall T, et al. Identification of cytogenetic subgroups and karyotypic pathways of clonal evolution in follicular lymphomas. Genes Chromosomes Cancer. 2004;39:195–204.
Dave SS, Wright G, Tan B, Rosenwald A, Gascoyne RD, Chan WC, et al. Prediction of survival in follicular lymphoma based on molecular features of tumor-infiltrating immune cells. N Engl J Med. 2004;351:2159–69.
Byers RJ, Sakhinia E, Joseph P, Glennie C, Hoyland JA, Menasce LP, et al. Clinical quantitation of immune signature in follicular lymphoma by RT-PCR-based gene expression profiling. Blood. 2008;111:4764–70.
Glas AM, Knoops L, Delahaye L, Kersten MJ, Kibbelaar RE, Wessels LA, et al. Gene-expression and immunohistochemical study of specific T-cell subsets and accessory cell types in the transformation and prognosis of follicular lymphoma. J Clin Oncol. 2007;25:390–8.
Wahlin BE, Sander B, Christensson B, Kimby E. CD8+ T-cell content in diagnostic lymph nodes measured by flow cytometry is a predictor of survival in follicular lymphoma. Clin Cancer Res. 2007;13:388–97.
Canioni D, Salles G, Mounier N, Brousse N, Keuppens M, Morchhauser F, et al. High numbers of tumor-associated macrophages have an adverse prognostic value that can be circumvented by rituximab in patients with follicular lymphoma enrolled onto the GELA-GOELAMS FL-2000 trial. J Clin Oncol. 2008;26:440–6.
Farinha P, Masoudi H, Skinnider BF, Shumansky K, Spinelli JJ, Gill K, et al. Analysis of multiple biomarkers shows that lymphoma-associated macrophage (LAM) content is an independent predictor of survival in follicular lymphoma (FL). Blood. 2005;106:2169–74.
Lee AM, Clear AJ, Calaminici M, Davies AJ, Jordan S, MacDougall F, et al. Number of CD4+ cells and location of forkhead box protein P3-positive cells in diagnostic follicular lymphoma tissue microarrays correlates with outcome. J Clin Oncol. 2006;24:5052–9.
Taskinen M, Karjalainen-Lindsberg ML, Nyman H, Eerola LM, Leppa S. A high tumor-associated macrophage content predicts favorable outcome in follicular lymphoma patients treated with rituximab and cyclophosphamide-doxorubicin-vincristine-prednisone. Clin Cancer Res. 2007;13:5784–9.
Jacob MC, Piccinni MP, Bonnefoix T, Sotto MF, Couderc P, Bensa JC, et al. T lymphocytes from invaded lymph nodes in patients with B-cell-derived non-Hodgkin’s lymphoma: reactivity toward the malignant clone. Blood. 1990;75:1154–62.
Dallman C, Johnson PW, Packham G. Differential regulation of cell survival by CD40. Apoptosis. 2003;8:45–53.
Carbone A, Gloghini A, Cabras A, Elia G. The Germinal centre-derived lymphomas seen through their cellular microenvironment. Br J Haematol. 2009;145:468–80.
Wahlin BE, Aggarwal M, Montes-Moreno S, Gonzalez LF, Roncador G, Sanchez-Verde L, et al. A unifying microenvironment model in follicular lymphoma: outcome is predicted by programmed death-1—positive, regulatory, cytotoxic, and helper T cells and macrophages. Clin Cancer Res. 2009;16:637–50.
Ai WZ, Hou JZ, Zeiser R, Czerwinski D, Negrin RS, Levy R. Follicular lymphoma B cells induce the conversion of conventional CD4+ T cells to T-regulatory cells. Int J Cancer. 2009;124:239–44.
Yang ZZ, Novak AJ, Ziesmer SC, Witzig TE, Ansell SM. Malignant B cells skew the balance of regulatory T cells and TH17 cells in B-cell non-Hodgkin’s lymphoma. Cancer Res. 2009;69:5522–30.
Fehervari Z, Sakaguchi S. CD4+ T-regs and immune control. J Clin Invest. 2004;114:1209–17.
Liyanage UK, Moore TT, Joo HG, Tanaka Y, Herrmann V, Doherty G, et al. Prevalence of regulatory T cells is increased in peripheral blood and tumor microenvironment of patients with pancreas or breast adenocarcinoma. J Immunol. 2002;169:2756–61.
Carreras J, Lopez-Guillermo A, Fox BC, Colomo L, Martinez A, Roncador G, et al. High numbers of tumor-infiltrating FOXP3-positive regulatory T cells are associated with improved overall survival in follicular lymphoma. Blood. 2006;108:2957–64.
Farinha P, Al-Tourah A, Gill K, Klasa R, Connors JM, Gascoyne RD. The architectural pattern of FOXP3-positive T cells in follicular lymphoma is an independent predictor of survival and histologic transformation. Blood. 2010;115:289–95.
Sweetenham JW, Goldman B, Leblanc ML, Cook JR, Tubbs RR, Press OW, et al. Prognostic value of regulatory T cells, lymphoma-associated macrophages, and MUM-1 expression in follicular lymphoma treated before and after the introduction of monoclonal antibody therapy: a Southwest Oncology Group Study. Ann Oncol. 2010;21(6):1196–202.
Lim HW, Hillsamer P, Kim CH. Regulatory T cells can migrate to follicles upon T cell activation and suppress GC-Th cells and GC-Th cell-driven B cell responses. J Clin Invest. 2004;114:1640–9.
Keir ME, Butte MJ, Freeman GJ, Sharpe AH. PD-1 and its ligands in tolerance and immunity. Annu Rev Immunol. 2008;26:677–704.
Keir ME, Francisco LM, Sharpe AH. PD-1 and its ligands in T-cell immunity. Curr Opin Immunol. 2007;19:309–14.
Carreras J, Lopez-Guillermo A, Roncador G, Villamor N, Colomo L, Martinez A, et al. High numbers of tumor-infiltrating programmed cell death 1-positive regulatory lymphocytes are associated with improved overall survival in follicular lymphoma. J Clin Oncol. 2009;27:1470–6.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Solal-Céligny, P., Cahu, X. & Cartron, G. Follicular lymphoma prognostic factors in the modern era: what is clinically meaningful?. Int J Hematol 92, 246–254 (2010). https://doi.org/10.1007/s12185-010-0674-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-010-0674-x