Abstract
Background
Metastatic breast cancer patients experience significance distress. Although talking with close others about cancer-related concerns may help to alleviate distress, patients often avoid such discussions, and their partners can engage in social constraints that may limit subsequent patient disclosures and exacerbate distress.
Purpose
We examined how partner constraints unfold, how they influence patient affect, and whether they exacerbate patient avoidance of cancer-related disclosures.
Methods
Fifty-four patients and 48 of their partners completed electronic diary assessments for 14 days.
Results
Partners’ social constraints carried over from one day to the next, but patients’ avoidance of discussing cancer-related concerns did not. When partners engaged in more social constraints one day, patients reported greater negative affect the following day (p < 0.05).
Conclusion
Findings suggest a temporal link between partner constraints and patient momentary affect. Helping partners to become aware of their constraining behaviors and teaching them skills to overcome this may facilitate patient adjustment to metastatic breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Women diagnosed with metastatic breast cancer must learn to cope with the physical, emotional, and social consequences of living with a terminal disease as well as the expectation of a future characterized by additional treatments, progressive physical disability, and death [1, 2]. Given this, it is not surprising that cross-sectional and longitudinal studies show that about one third of these women experience clinically significant levels of depression, anxiety, and/or traumatic stress symptoms [3–6]. For women who are diagnosed with metastatic breast cancer and are either married or in an intimate relationship, the relationship with their partner plays a critical role in their adaptation to their illness [7, 8]. One aspect of the couple relationship that appears to be particularly important is the open discussion of cancer-related concerns [9]. Among breast cancer patients, the ability to express emotions and communicate openly about cancer has been associated with fewer emotional problems and higher levels of perceived control [7, 10, 11]. Conversely, holding back, or the avoidance of discussing cancer-related concerns with a partner, has been linked to poorer emotional well-being [12], increased distress [13], and the experience of cancer-related intrusive thoughts [13]. Despite the potential benefits of disclosure, one study found that 35 % of breast cancer patients did not disclose to anyone (including their partners) their primary cancer-related concern [14]. Thus, whether women with metastatic breast cancer disclose and whether that disclosure facilitates adjustment is likely to depend to a degree on their partners and how they respond.
According to the Social Cognitive Processing Model, talking with others can facilitate cognitive and emotional processing of experiences such as cancer if the social context in which these discussions take place is supportive and positive [15, 16]. From this perspective, talking with a supportive partner should allow patients the opportunity to disclose their emotions, learn to tolerate aversive feelings, receive support for effective coping, and obtain assistance in the process of finding meaning and benefit in their experience [17]. However, research suggests that partners are not always supportive and may instead engage in social constraints [15, 16]. These constraints can take on various forms including the partner being critical, avoidant, unreceptive, or conveying discomfort in discussing a concern that is important to the patient [15, 18, 19]. They are also associated with higher levels of patient distress [20, 21].
Patients coping with metastatic breast cancer may be at greater risk of experiencing social constraints from their partners due to the psychological, practical, and relationship consequences of living with a terminal illness [22, 23]. Indeed, couples coping with advanced cancers report more emotional distress, role restrictions, and physical problems than those coping with early stage cancers [24, 25]. Because support needs may be greater and the detrimental effects of constraints magnified among patients with metastatic breast cancer, developing a clearer understanding of the impact of social constraints on patient adjustment may guide the development of interventions that address the unique needs and challenges faced by this vulnerable and under-researched population.
Some researchers have argued that social constraints can be placed within a dyadic stress and coping framework [22]. Within this framework, it becomes important to consider how the partner’s constraints can influence the patient’s emotions and actions as well as how social constraints unfold in a couple’s relationship over time. In a qualitative study that illustrates the transactional and dynamic qualities of social constraints, Pistrang and Barker [26] used a tape-assisted recall technique that allowed breast cancer patients to reflect on a recently audio-taped conversation with their partner. In one couple, the patient reflected that her husband’s optimism and minimization of her cancer during the discussion prevented her from not only expressing her emotions to him but also fueled her distress. While this is suggestive that social constraints from partners can influence both the patient’s emotional and behavioral responses (e.g., avoidance or holding back cancer-related concerns), studies have yet to quantitatively examine this possibility. Likewise, the few studies that have adopted the Social Cognitive Processing Model to quantitatively examine how couples’ cope with cancer have been cross-sectional [21, 27]. Because relationships are dynamic and ever-changing, and because social constraints occur within the everyday context of relationships, it is plausible that social constraints can also change—perhaps as a function of changes within the illness context, or as couples settle into illness routines [22, 23]. Intensive longitudinal research designs would not only allow researchers to test the Social Cognitive Processing Model by examining the links between partner constraints and patient avoidance within the context of everyday life but would also bolster the directionality of influence from social constraints to patient adjustment in metastatic breast cancer.
On a related note, most of our knowledge of social constraints and their influence on adjustment has come from studies using single-time global retrospective measures. Conclusions from such studies are limited because it is possible that social constraints may vary both within and across days. Indeed, qualitative research suggests that perceptions of social constraints can change in couples over time and that some topics may be more emotionally charged and difficult for couples to discuss than others [23]. Given the possibility that social constraints may wear more on patients when they are consistently experienced, it may be useful to examine the links between daily social constraints and daily affective states.
One reason why fluctuations in daily affect are relevant in the context of cancer is because variations in patient affect have been shown to co-vary with changes in patient real-time reports of physical symptoms such as fatigue and pain [28]. There is also some evidence to suggest that the social environment can influence this link. Namely, studies of experimentally induced affect have shown that people who were made to feel sad reported more physical symptoms [29, 30] and attributed greater discomfort to their symptoms [29] than those made to feel happy. However, it is unclear how such a process might unfold in everyday life. Prospective studies that include both patients and their partners and that consider the role of partner constraints on patient daily affect could be an important first step toward this goal.
A few studies have successfully utilized electronic diary designs to capture the daily within-person experiences of patients dealing with advanced cancer [28, 31, 32]; however, to our knowledge, no studies have taken advantage of such intensive longitudinal methods to evaluate the putative effects of social constraints and avoidance on affect within the context of everyday couple life. Electronic daily diaries (EDs) administered on handheld computers often involve repeated assessments over short durations, have signals to prompt participants, and provide time and date stamps for evaluating compliance [33]. As such, they are uniquely suited for studying not only the within-person daily processes associated with social constraints but also for helping to bolster the directionality of influence from social constraints to affect based on the temporal sequencing of constraint and affect assessments. This is important because assuming that the links among variables within-persons is the same as the link between-persons risks committing an ecological fallacy [34].
With these issues in mind, we conducted a 2-week electronic daily diary study to test the predictions of the Social Cognitive Processing Model in couples where the patient was initiating treatment for metastatic breast cancer. We hypothesized that partner constraints and patient avoidance would co-vary from day to day, such that the effects of constraints or avoidance reported the previous day would carry over and predict partner constraints and patient avoidance the following day (hypothesis 1a). We further hypothesized that the more partners reported constraining patient disclosures on one day, patients would be more likely to report that they avoided cancer-related discussions with their partners that same day (hypothesis 1b) as well as the following day (hypothesis 1c). Finally, because a review of research showed that relative to the positive aspects of life or relationships, the negative aspects are more strongly related to symptoms of distress [35], we examined whether constraints and avoidance predicted changes in the experience of both negative and positive affect. We expected that higher levels of patient avoidance on one day would have lingering adverse effects on patient negative affect, but not necessarily on patient positive affect, the next day (hypothesis 2a). Similarly, we anticipated that higher levels of partner constraints would be associated with lingering adverse effects on patient negative affect, but not necessarily patient positive affect, the following day (hypothesis 2b).
Method
Participants and Procedure
Data for this study were drawn from a larger study of spousal relationships and pain in metastatic breast cancer that was conducted at a comprehensive cancer center in the southwestern United States [8, 36, 37]. Patients were identified through medical chart review and were eligible if they (1) were female patients who were initiating treatment for metastatic breast cancer (any line of therapy); (2) had a physician-rated Eastern Cooperative Oncology Group (ECOG) performance status score ≤2 (ECOG scores range from 0 = fully ambulatory and able to carry on all pre-disease performance without restriction, to 5 = dead—a score of 2 means that the patient is ambulatory and capable of all self-care but is unable to perform any work activities); (3) rated their average pain as ≥1 on the Brief Pain Inventory [38], where 0 = no pain and 10 = worst pain imaginable; (4) could speak and understand English; and (5) had a male partner (spouse or significant other) with whom they had lived for at least 1 year. All consecutive patients who met the eligibility criteria were approached with their partners to participate by study staff during their routine clinic visits. In cases where the partner was not present, consent was obtained from the patient to contact him by phone. Patients and partners who participated in the parent study (N = 191 couples) were asked to separately complete and return written surveys at baseline (within 2 weeks of the patient starting treatment for metastatic breast cancer), and 3 and 6 months later. Couples who participated in the parent study could also participate in an additional optional procedure involving electronic daily diary assessments. Data from the optional procedure are presented here.
Ninety-four consecutive metastatic breast cancer couples who had agreed to participate in the parent study were approached by research staff to participate in the optional procedure. Fifty-nine of these couples (62.8 %) agreed to participate. Reasons for refusal included patient or partner disinterest (57.1 %), perceived burden of completing the optional procedure or conflict with work responsibilities (40 %), and a lack of perceived personal relevance of the study (2.9 %). Due to time and budget constraints, recruitment for the optional procedure was discontinued after 59 couples were enrolled.
Comparisons were made between patients who refused and those who participated based on available data for age, Eastern Cooperative Oncology Group performance status, race, average pain at time of recruitment (assessed by the Brief Pain Inventory), and primary metastatic site. Significant differences were found for age [t(91) = −3.98, p = 0.001] and pain [t(82) = 5.55, p = 0.001]. Specifically, patients who agreed to participate were younger (M = 49.38, SD = 10.76) than those who refused (M = 58.11, SD = 9.30), and patients who agreed to participate had higher ratings of pain (M = 4.41, SD = 3.01) than those who refused (M = 1.12, SD = 0.43). Patients and partners were each provided with their own password-protected electronic diary. The diaries were programmable Palm Tungsten E or E2 computers (32 MB RAM) weighing 4.7 oz. and powered by rechargeable lithium ion batteries. Dimensions were approximately 4.5 × 3.1 × 0.5 in. Participants used a stylus to touch fixed-response options in answer to questions presented in a fixed order on a 2.4-in. transreflective liquid crystal color display (resolution, 320 × 320 pixels). Couples were trained to use the electronic diaries and received follow-up telephone calls within 3 days of taking them home. In 45 cases (76 %), usable data were obtained from both members of the couple; in nine cases, data were recovered from the patient only; in three cases, data were recovered from the spouse only, and in two cases, no usable data could be recovered from either partner because the battery was not recharged. Thus, the final sample comprised 54 patients and 48 partners.
In this study, patients reported on their own affect twice daily (evenings and mornings) for 14 consecutive days (28 total assessments). At each evening assessment, patients additionally reported on the degree to which they avoided discussing cancer-related concerns with their partner that day and partners reported on the degree to which they constrained patient disclosures (by avoiding discussing the patient’s cancer-related concerns).
An alarm schedule for the patient’s electronic diary was randomly generated at the time of recruitment. The patients’ morning assessments were randomly scheduled between 9:00 a.m. and 10:00 a.m. and the evening assessments between 8:00 p.m. and 9:00 p.m. The partner’s electronic diary was programmed to generate alarms within a 15-min window around the patient’s scheduled evening assessments to ensure that patients and partners completed assessments at about the same time and on the same phenomena without discussing their responses. Each diary assessment took about 2–5 min to complete. Patients and partners received gift cards (up to $80 each) based on the percentage of assessments they completed. Patients completed 72.2 % of morning assessments. Patients completed 77.7 % and partners completed 71.4 % of the evening assessments. No significant differences were found between patients and partners with regard to the number of evening assessments completed [t(39) = 1.07, p = 0.29].
Measures
Because electronic diary studies often involve intensive assessment schedules, reactivity, reduced adherence, and participant burden are major concerns [39] requiring measures to be as brief and engaging as possible. As a consequence, researchers often truncate existing measures or create single-item measures. This is considered appropriate when the construct being measured is intuitive [39], and reliable when repeated measurements over short time periods are involved [40].
Patient Morning Affect
Patients rated the intensity of their own momentary affect (right now) on a five-point Likert-type scale ranging from 1 (not at all) to 5 (extremely) using eight adjectives: active, happy, peppy, calm, tired, anxious, sad, and angry. The adjectives were taken from the original list of mood adjectives identified by Larsen and Diener’s circumplex model of affect [41], and chosen on the basis of our previous electronic diary research in breast cancer [28].
Because we were interested in examining the effects of evening reports of patient avoidance and partner social constraints on the next morning’s positive and negative affect, within- and between-person correlations of morning affect were examined. The emerging pattern and strength of the within-person correlations suggested a negative affect factor composed of three adjectives (anxious, sad, and angry) as well as a positive affect factor composed of three adjectives (active, happy, and peppy). We sought to construct latent factors of negative and positive affect which can be considered “pure” measures of momentary affect purged of measurement error. Thus, we conducted multilevel confirmatory factor analyses (42) using maximum likelihood estimation on these six patient mood adjectives to determine a plausible factor structure for negative and positive affect. The fit of a correlated two-factor model with separate positive and negative affect factors at both the within-person and between-person levels [χ 2(20) = 138.868, p < 0.001, RMSEA = 0.109, SRMR (within/between) = 0.104/0.084] was compared to that of a one-factor model with all six of the adjectives loading on a single factor at both the within-person and between-person levels [χ 2(23) = 378.363, p < 0.001, RMSEA = 0.176, SRMR (within/between) = 0.167/0.137]. The two-factor model showed significantly better fit than the one-factor model [Δχ 2(3) = 239.495, p < 0.001]. We also examined separate one-factor models of negative affect [χ 2(2) = 1.168, p = 0.4344, RMSEA < 0.001] and positive affect [χ 2(2) = 1.124, p = 0.570, RMSEA < 0.001 respectively] which both indicated excellent fit. Because of our interest in modeling within-person processes, the within-person affect factors from the multilevel CFAs were used to test the study hypotheses. We used a factor analytic-based measure of reliability called omega to assess the ability of the three affect items to capture reliably within-person change in the underlying construct of negative affect [42]. Coefficient omega was 0.71, reflecting acceptable within-person reliability.
Evening Reports of Patient Avoidance and Partner Social Constraints
At the end of each day (i.e., evening assessment), patients reported on the degree to which they avoided discussing their cancer-related concerns with their partners by responding to the question, “Today I avoided talking to my husband about my thoughts and feelings about the cancer.” Partners reported on the degree to which they constrained patients’ cancer-related disclosures by responding to the question, “Today I avoided speaking to my wife about her thoughts and feelings about the cancer.” Patient and partner ratings were made on a Likert-type scale with possible responses ranging from 1 (not at all) to 4 (very much).
Paper-and-Pencil Questionnaire Assessments
After completing the 14 days of electronic diary assessments, patients and partners completed the paper-and-pencil baseline questionnaire from the parent study that included demographic (e.g., age, employment status, and education) and medical questions (e.g., type of treatment, length of time since their initial breast cancer diagnosis, stage at diagnosis, primary metastatic site, and comorbidities) as well as the seven-item short form of the Dyadic Adjustment Scale [43]. Scores can range from 0 to 36 with scores below 21 indicating marital distress. Internal consistency reliability (Cronbach’s alpha) was 0.89 for both patients and partners. These medical, demographic, and relationship variables were used as potential control variables in the analyses.
Data Analysis Strategy
Descriptive statistics (means and within- and between-person variance) were calculated for each of the major study variables (see Table 1). Additionally, intra-class correlations (ICCs) were calculated for the positive and negative affect factors to obtain an understanding of how they varied from day to day. All analyses were conducted using the Mplus 6 statistical software package [44].
Statistical tests of the first set of hypotheses were carried out using multilevel modeling. To test whether there were carryover effects of social constraints and avoidance to the following day (hypothesis 1a), partner reports of constraints in the evening were regressed on their previous evening’s reports of constraints and patient reports of avoidance in the evening were similarly regressed on their previous evening’s reports of avoidance. To determine whether partner reports of constraining disclosure increased the likelihood that the patient avoided engaging in cancer-related discussions that same evening (hypothesis 1b), patient reports of avoidance were regressed on partner reports of constraints. To determine whether spousal reports of constraints at one point in time influenced patient avoidance at a later time (hypothesis 1c), we regressed patient avoidance on one day on the previous day’s reports of partner constraints.
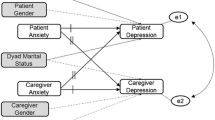
Statistical tests of hypothesis 2 were conducted within a multilevel structural equation modeling (MSEM) frameworkFootnote 1 [45] and the corresponding model is depicted in Fig. 1. MSEM is a method of performing more traditional SEM within a multilevel modeling context which allows for the isolation of within-person (i.e., daily scores within an individual) and between-person (i.e., daily scores across persons) parts of the model. The model consists of simultaneously regressing the patient within-person morning affect latent factor on the previous evening’s partner within-person social constraint rating while controlling for the previous evening’s patient within-person affect latent factor. Between-person variability (i.e., individual means of daily scores differing from person to person) in the partner daily constraint predictor was partitioned out using person-mean centering, such that the remaining within-person variability in constraints (i.e., daily scores on social constraints within an individual varying from their own mean) could be linked to the within-person variability in the patient morning affect factor. The control of evening affect was similarly allowed to explain variability in morning affect only at the within-person level. To insure the equivalent meaning, loadings were set to be equal for morning and evening affect, as well as for within-person and between-person parts of the model. Moreover, between-person random effects for the focal within-person links (i.e., constraints → morning affect) were estimated. Corresponding to Fig. 1, we only depict and interpret the within-person effects in these regressions due to an interest in daily within-person processes, rather than cross-sectional effects.
In order to clearly link the direction of influence as being from social constraints and avoidance to affect rather than vice versa, additional MSEMs were run. First, reports of partner constraints measured in the evening were regressed on same-day patient morning negative affect. Second, patient reports of avoidance in the evening were regressed on same-day patient morning negative affect. Similarly, partner reports of constraints and patient reports of avoidance were regressed on same-day patient morning positive affect.
Pearson correlations between the medical and socio-demographic variables [i.e., age, employment status, education, type of treatment, length of time since the patient’s initial breast cancer diagnosis, stage at diagnosis, primary metastatic site, number of comorbidities, and self-reported pain levels (at the time of recruitment) on the Brief Pain Inventory [38]] with the study predictors and outcomes were examined to determine potential covariates. We also examined correlations with scores on the short form of the Dyadic Adjustment Scale to rule out the possibility that partner constraints and patient avoidance were merely symptomatic of poor relationship quality. Because dyadic adjustment scores were significantly correlated with the study predictors, we considered whether this variable influenced our results in subsequent analyses.
Results
Sample Characteristics
Patients were predominantly white (85 %), well educated (86 % had at least 2 years of college study), and retired or unemployed (61 %). All were married, with wide variation in the length of time married (M = 21.48 years, SD = 13.06; range 1 to 55 years). Average age was 49.38 years (SD = 10.76; range 30 to 73 years). Partners’ average age was 51.32 years (SD = 11.51; range 32 to 78 years). The majority were white (88 %), well educated (86 % had at least 2 years of college study), and employed full time (60 %). In terms of dyadic adjustment, 27 % of patients and 27 % of partners met short-form Dyadic Adjustment Scale criteria for marital distress; however, the percentage of couples where both partners met the criteria for marital distress was much lower (9 %).
Although all patients were beginning treatment for stage 4 (metastatic) breast cancer at the time of study entry, disease stage at initial cancer diagnosis included stage 1 (13.56 %), stage 2 (28.81 %), stage 3 (15.25 %), and stage 4 (42.37 %). The average length of time since initial cancer diagnosis was 4.75 years (SD = 4.5; range 1 month to 19.5 years). Primary metastatic sites were bone (56 %), lung (22 %), liver (19 %), and brain (3 %). With regard to treatment, 83 % of patients were beginning chemotherapy, 15 % hormonal therapy, and 2 % radiation.
Descriptive Results
Table 1 contains the means, standard deviations, and ICCs of morning affect and social constraints items. As can be seen, the ICCs suggest that there are reasonably large proportions of variability in these daily variables both within- and between-person.
Multilevel SEM Results
For hypothesis 1a, we expected that partner constraints and patient avoidance would vary from day to day, such that partner constraints on one evening would predict partner constraints the following evening and that patient avoidance on one evening would predict patient avoidance the following evening. The regression of partner constraints on one evening onto ratings of partner constraints from the previous evening (N = 48 partners) indicated significant carryover effects (B = 0.045, p = 0.011, 95 % CI 0.010, 0.080). Similar analyses were carried out for patient avoidance (N = 54 patients) and indicated that the patient’s reports of avoidance one evening was relatively independent of her reports of avoidance the next evening (B = 0.003, ns). For hypothesis 1b, we expected that the more partners reported constraining patient disclosures on one evening, patients would be more likely to report that they avoided cancer-related discussions with their partners that same evening. Multilevel path modeling was performed to determine the influence of ratings of partner constraints on patient avoidance during the same evening (N = 45 couples). No significant within-person effect of partner constraints on patient avoidance was found (B = 0.073, ns). For hypothesis 1c, we expected that the more partners reported constraining patient disclosures on one evening, patients would be more likely to report that they avoided cancer-related discussions with their partners the following evening. No significant within-person effects were found for partner constraints on one evening leading to patient avoidance the next evening (N = 45 couples; B = 0.007, ns). It should be noted, however, that the between-person link between partner constraints and patient avoidance (i.e., average partner constraints and average patient avoidance) was statistically significant (B = 0.547, p = 0.016, 95 % CI 0.101, 0.994). However, this between-person link does not provide information about the daily process we were interested in.
For hypothesis 2a, we expected that the more patients reported avoiding discussing cancer-related concerns with their partners on one evening, the more they would report higher levels of negative, but not necessarily lower positive affect the following morning. To test this hypothesis, we ran a multilevel SEM regressing the patient morning affect factor (positive vs. negative) on patient avoidance, controlling for the patient’s previous evening affect factor, time, and the patient’s dyadic adjustment (N = 54 patients). Effects from this model can be interpreted as representing within-person residualized change in patient affect. Results indicated that at the within-person level, the typical patient reported marginally higher levels of negative affect on mornings after which she reported greater avoidance (B = 0.109, p = 0.064, 95 % CI −0.006, 0.225). Patient dyadic adjustment did not have an influence on this within-person association. No significant effects were found for the regression of patient morning positive affect on patient avoidance (B = −0.037, ns). For hypothesis 2b, we expected that the more partners reported constraining the patient’s disclosure on one evening, the more patients would report higher levels of negative, but not necessarily lower positive, affect the following morning. Multilevel analyses similar to those conducted for hypothesis 2a were carried out (N = 45 couples). Consistent with the hypothesis, results showed that the typical patient reported significantly higher levels of negative affect, independent of time, the previous evening’s affect, and dyadic adjustment, on the mornings after her partner reported engaging in higher levels of constraints (B = 0.126, p = 0.017, 95 % CI 0.023, 0.229). Patient dyadic adjustment did not have an influence on this within-person association. No significant effects were found for the regression of patient positive affect on partner constraints (B = −0.025, ns). Findings focusing on the within-person effects are detailed in Table 2. It should be noted that we estimated random effects for intercepts and for the constraint and avoidance slopes in these models.
Finally, to rule out the possibility of reverse causality, we re-ran the models for hypotheses 2a and 2b reversing the directionality of effects (e.g., patient morning affect as a cause of evening spousal constraints). Patient morning negative affect was not related to either spousal reports of constraints or patient reports of avoidance measured later on in the day (B = 0.17, ns and B = 0.20, ns, respectively). Similarly, patient morning positive affect was not related to either partner constraints or patient avoidance that evening (B = −0.063, ns and B = −0.062, ns, respectively).
Discussion
This study sought to address gaps in the social constraints literature by using electronic daily diaries to prospectively examine how patient avoidance and partner constraints unfold in the everyday lives of couples coping with metastatic breast cancer. Toward this end, we examined how patient avoidance on one day affected subsequent interactions with the partner the following day. We also examined how partner reports of social constraints on one day affected subsequent interactions with the patient the following day. Finally, we examined how patient avoidance and partner constraints on one day affected patient momentary affect the following day.
We found that when patients avoided discussing their cancer-related concerns with their partners on one day, this did not increase the likelihood that patients would avoid discussing cancer-related concerns the following day. Overall, patients reported relatively low levels of avoidance (M = 1.574 out of 4); however, this varied significantly across patients and from day to day, suggesting that some patients may have been more selective than others in what they chose to discuss with their partners. This selectivity was apparently not without cost as those who reported higher levels of avoidance experienced marginal increases in negative affect the following day. Although it is possible that patients’ behaviors were influenced by their assessments of what their partners could handle, do to help, or wanted to hear, we did not ask about what influenced their decisions to avoid disclosing their cancer concerns to their partners on some days but not others. Developing a better understanding of the evaluation process that patients go through and what factors influence their decisions about whether, how much, and how to disclose cancer-related concerns to their partners would help researchers to design interventions to facilitate adaptive spousal communication in metastatic breast cancer.
We also found that partner constraints carried over from one day to the next. At first glance, our finding that partner constraints are relatively stable seems contrary to the Social Cognitive Processing Model which posits that constraints are dynamic and can change over time. However, it is possible that the length of the current study (14 days) may not have been sufficient to detect changes in partner constraints. Because metastatic breast cancer is a degenerative disease, as it progresses, patient functional disability increases and couples’ relationships and interactions are likely to become increasingly clouded by the cancer experience. Under such circumstances, there is a real possibility that partner constraints may continue to persist or even become worse. It is also possible that constraints might decrease as the couple realizes that their time together is short or that the partner no longer feels the need to avoid discussion in order to be encouraging to the patient. Helping partners to become aware of constraints and teaching them skills to overcome them during the initial treatment period for metastatic breast cancer may thus be beneficial as cancer progresses and the patient moves toward the end of life.
Contrary to our expectations, partner constraints did not have an influence on patient avoidance of disclosing cancer-related concerns. One possibility that may also explain the low within-person correlation between partner constraints and patient avoidance (r = 0.10) is that multiple motives can underlie these behaviors. For example, partners and patients may wish to protect themselves and each other from difficult emotions, or may not know what would be helpful to say or how best to act. Research is needed to determine whether such distinct motives have distinct consequences for one or both partners and their relationship.
Finally, consistent with our hypothesis, we found that when partners reported engaging in more constraints one day, patients reported greater negative affect the following day and that this association was significant even after controlling for time, the patient’s affect the previous day, and the patient’s overall dyadic adjustment. In contrast, partner constraints the previous day were not associated with next-day changes in patient positive affect. Such a pattern of results, where avoiding talking about cancer makes negative affect worse but does not necessarily decrease positive affect, is consistent with findings showing that positive and negative affect are relatively independent of each other [46] such that they can have differing relations to other variables [47].
While this study had a number of strengths including digital momentary assessment, use of a late-stage disease sample, the ability to detect temporal associations between partner constraints and patient avoidance, and a strong theoretical and empirical grounding, there were some limitations. First, we focused on only one type of social constraint—partner avoidance, even though social constraints also include behaviors such as criticism, or unsupportive responses [22]. Our focus stemmed from an interest in examining not just how the patient’s avoidance influenced the patient but also how the partner’s avoidance of discussions about the patient’s cancer-related concerns (social constraint) affected the patient; however, future studies should identify and examine the effects of the full range of partner constraints to determine their relative importance and impact on patient adjustment.
A second limitation is that we used self-report measures of partner constraints. Indeed, partners may have under-reported their level of constraint because saying that one avoided discussions with a loved one about her metastatic disease could sound callous or uncaring. From a statistical perspective, this possibility would likely not have adversely affected our findings and provides an even more conservative test of our hypotheses. However, we still do not know whether the partner’s report of his own constraint or the patient’s report of the partner’s constraint better reflects actual behavior.
A related issue is that we do not know whether actual or perceived partner behavior is most important in terms of patient adjustment and well-being. One advantage of focusing on social constraints reported by the partner, as we did here, is the ability to link “actual” partner behaviors onto patient outcomes. Although most studies that have investigated the role of social constraints have focused on the perceptions of the person whose disclosure is being constrained [22], the social support literature defines perceived support as a person’s report of the support that they receive from their partner and actual support as the partner’s report of the support that they provided [48]. Using data from a daily diary study of support provision and receipt in couples, one study found that many transactions reported by supporters were not reported by recipients and that these “invisible support” transactions promoted adjustment to a major stressor [48]. Although our findings provide partial support for the idea that a similar process may occur with regard to social constraints, future studies should include measures of actual patient and partner constraints as well patients’ and partners’ perceptions of each other’s constraints in an effort to develop a model of couples’ communication that is fully reciprocal. Another direction for future research that would support the validity of the measures of patient avoidance and partner constraints would be to compare scores on these measures to recordings of actual couple conversations coded for avoidance and constraint.
A third set of limitations concern the study sample. Participants were relatively young (M = 49.38 years) given that the median age for a breast cancer diagnosis is 61 years [49]. Older patients may have declined participation because they were not as comfortable with the computerized assessments. Our sample was also relatively homogeneous in terms of race and we had insufficient power to examine socio-cultural differences. Differences in culture, family structure, and class can all affect the ways in which couples adapt to stressful circumstances, such as metastatic breast cancer. Finally, despite collecting 14 days of repeated measures, our sample size was relatively modest. This may have contributed to not being able to detect a significant within-person link between partner constraints and patient avoidance, as well as our finding a trend for the effect of patient avoidance on next-day patient negative affect. However, this is the first study to use electronic diaries to identify within-day processes linking both patient avoidance and social constraints to patient negative affect; since the trend for patient avoidance was in the same direction as the significant effect for partner constraints, it can serve as a tenable hypothesis for future work.
A final set of limitations concern the use of electronic diary methods and the conclusions that can be drawn from this type of data. Indeed, researchers who use electronic diaries outside the oncology setting typically report adherence rates of 80 % or more [50]. Decreased rates of adherence in this study may be due to the fact that patients were initiating treatment for metastatic breast cancer, had increased demands on their time, and were experiencing pain and cancer-related symptom burden. Diary alarms were also generated between 9:00 a.m. and 9:00 p.m. This may have affected compliance because participants sometimes went to bed early or woke up late and missed assessments.
While no theory currently exists to explain when diary completion has an impact and when it does not, it is possible that participants’ understanding of a particular construct may become more complex or reliable with repeated monitoring and that the repeated exposure to diary questions may enhance encoding or retrieval of relevant information [51]. The converse is also possible. In fact, one study found that reports of support provision increased over the course of a 28-day daily diary study [52]. To address whether increased monitoring altered participant behavior in this study, we controlled for time in all of our analyses. We also examined whether ratings of constraints and avoidance increased during the duration of our study by regressing patient avoidance and partner constraints on time (day). Results indicated the absence of a linear effect of time on patient avoidance or partner constraints.
Another common critique is that diary designs produce correlational data and thus cannot be used to make causal arguments. Relative to a cross-sectional survey studies, diary studies allow effects to be ordered in time, and this structured data often can be used to test and reject various causal explanations. However, the same data cannot be used to establish other causal explanations unless assurances can be made that the analytic model is an exact representation of the causal process, including the time lags of causal effects [53]. Thus, diary studies have some limitations relative to randomized experiments but offer clear benefits and can be used to further causal thinking relative to cross-sectional designs [51].
In conclusion, our findings provide partial support for the Social Cognitive Processing Model in metastatic breast cancer and extend previous research by identifying a temporal link between patient avoidance and partner constraints on patient momentary affect. They also suggest that in spite of the numerous physical symptoms that women with metastatic breast cancer struggle with (e.g., progressive pain, fatigue, and weight loss) they continue to be reactive to the effects of communication problems with their partners such that the daily experience of social constraints impacts their affect negatively the following day. Indeed, in the context of metastatic breast cancer, social support needs and communication challenges may be greater and the detrimental effects of withholding and restraint between patients and partners may be magnified as the patient experiences greater functional disability and approaches the end of life. This is therefore a population where psychosocial interventions that teach communication skills and target the daily support transactions between patients and their partners are sorely needed. With an eye toward developing such interventions, future work should clarify the mechanisms by which social constraints hinder patient adjustment. Studies have shown that expressing cancer-related thoughts and feelings to a supportive partner can facilitate therapeutic insights [54], the processing of cancer-related intrusive thoughts [55], and the solicitation and provision of social support [56]. Future work should thus investigate whether the converse is true for social constraints or whether social constraints operate via different pathways to affect patient well-being and adjustment.
Notes
The methods for handling missing data in multilevel SEM are the same as multilevel modeling and SEM more generally. Essentially, all data from cases (in this case, days) with missing outcomes are retained and maximum likelihood is used to estimate parameters in the presence of missing data under the assumption that the data are missing at random. Cases with missing data on predictors are deleted.
References
Cella D, Tross S. Psychological adjustment to survival from Hodgkin’s disease. J Consult Clin Psychol. 1986; 54: 616-662.
Butler L, Koopman C, Cordova M, et al. Psychological distress and pain significantly increase before death in metastatic breast cancer patients. Psychosom Med. 2003; 65: 416-426.
Cella D, Mahon S, Donovan M. Cancer recurrence as a traumatic event. Behav Med. 1990; 16: 15-22.
Butler L, Koopman C, Classen C, Spiegel D. Traumatic stress, life events, and emotional support in women with metastatic breast cancer: Cancer-related traumatic stress symptoms associated with past and current stressors. Heal Psychol. 1999; 18: 555-560.
Baider L, Perez T, DeNour A. Gender and adjustment to chronic disease. Gen Hosp Psychiatry. 1989; 11: 1-8.
Carter CA, Carter RE. Some observations on individual and marital therapy with breast cancer patients and spouses. J Psychosoc Oncol. 1994; 12: 65-81.
Giese-Davis J, Hermanson K, Koopman C, Weibel D, Spiegel D. Quality of couples’ relationship and adjustment to metastatic breast cancer. J Fam Psychol. 2000; 14: 251-266.
Milbury K, Badr H. Sexual problems, communication patterns, and depressive symptoms in couples coping with metastatic breast cancer. Psycho-Oncology. 2012 [Epub ahead of print].
Manne S, Badr H. Intimacy and relationship processes in couples’ psychosocial adaptation to cancer. Cancer. 2008; 112: 2541-2555.
Dunkel-Schetter C. Social support and cancer: Findings based on patients interviews and their implications. J Soc Issues. 1984; 40: 77-98.
Mesters I, van der Borne H, McCormick L, et al. Openness to discuss cancer in the nuclear family: Scale development, and validation. Psychosom Med. 1997;59:269-279.
Figueiredo M, Fries E, Ingram K. The role of disclosure patterns and unsupportive social interactions in the well-being of breast cancer patients. Psycho-Oncology. 2004; 13: 96-105.
Porter L, Keefe F, Hurwitz H, Faber M. Disclosure between patients with gastrointestinal cancer and their spouses. Psycho-Oncology. 2005; 14: 1030-1042.
Kornblith A, Regan M, Kim Y, et al. Cancer-related communication between female patients and male partners scale: A pilot study. Psycho-Oncology. 2006; 15: 780-794.
Manne S. Intrusive thoughts and psychological distress among cancer patients: The role of spouse avoidance and criticism. J Consult Clin Psychol. 1999; 67: 539-546.
Lepore SJ, Helgeson V. Social constraints, intrusive thoughts, and mental health in prostate cancer survivors. J Soc Clin Psychol. 1998; 17: 89-106.
Tait R, Silver RC. Coming to terms with major negative life events. In: Uleman JS, Bargh JA, eds. Unintended Though. New York: Guilford; 1989: 351-382.
Manne S, Glassman M. Perceived control, coping efficacy, and avoidance coping as mediators between spouses’ unsupportive behaviors and cancer patients’ psychological distress. Heal Psychol. 2000; 19: 155-164.
Manne S, Taylor KL, Dougherty J, Kerneny N. Supportive and negative responses in close relationships: Their association with psychological adjustment among individuals with cancer. J Behav Med. 1997; 20: 101-126.
Zakowski S, Harris C, Kreueger N, et al. Social barriers to emotional expression and their relations to distress in male and female cancer patients. Br J Heal Psychol. 2003; 8: 271-286.
Manne SL, Winkel G, Grana G, et al. Couple-focused group intervention for women with early stage breast cancer. J Consult Clin Psychol. 2005; 73(4): 634-646.
Lepore SJ, Revenson TA. Social constraints on disclosure and adjustment to cancer. Soc Personal Psychol Compass. 2007; 1: 313-333.
Badr H, Carmack Taylor C. Social constraints and spousal communication in lung cancer. Psycho-Oncology. 2006; 15: 673-683.
Lewis F, Deal L. Balancing our lives: A study of the married couple’s experience with breast cancer recurrence. Oncol Nurs Forum. 1995; 22: 943-953.
Weitzner MA, McMillan SC, Jacobsen PB. Family caregiver quality of life: Differences between curative and palliative cancer treatment settings. J Pain Symptom Manag. 1999; 17: 418-428.
Pistrang N, Barker C. How partners talk in times of stress: A process analysis approach. In: Revenson T, Kayser K, Bodenmann G, eds. Couples Coping with Stress: Emerging Perspectives on Dyadic Coping. Washington, DC: American Psychological Association; 2005: 97-119.
Coyne JC, Smith DAF. Couples coping with a myocardial infarction—a contextual perspective on wives distress. J Personal Soc Psychol. 1991; 61: 404-412.
Badr H, Basen-Engquist K, Carmack Taylor C, de Moor C. Mood states associated with transitory physical symptoms among breast and ovarian cancer survivors. J Behav Med. 2006; 29: 461-475.
Salovey P, Birnbaum D. Influence of mood on health-relevant cognitions. J Personal Soc Psychol. 1989; 57: 539-551.
Croyle R, Uretsky M. Effects of mood on self-appraisal of health status. Heal Psychol. 1987; 6: 239-253.
Badr H, Laurenceau J, Schart L, Basen-Engquist K, Turk D. The daily impact of pain from metastatic breast cancer on spousal relationships: A dyadic electronic diary study. Pain. 2010; 151: 644–654.
Sherliker L, Steptoe A. Coping with new treatments for cancer: A feasibility study of daily diary measures. Patient Educ Couns. 2000; 40: 11-19.
Stone A, Shiffman S, Schwartz J, Broderick J, Hufford M. Patient compliance with paper and electronic diaries. Control Clin Trials. 2003; 24: 182-199.
Robinson W. Ecological correlations and the behavior of individuals. Am Sociol Rev. 1950; 15: 351-357.
Baumeister RF, Bratslavsky E, Finkenauer C, Vohs KD. Bad is stronger than good. Rev Gen Psychol. 2001; 5: 323-370.
Badr H, Carmack C, Kashy D, Cristofanilli M, Revenson T. Dyadic coping in metastatic breast cancer. Heal Psychol. 2010; 29: 169-180.
Badr H, Milbury K. Associations between depression, pain behaviors, and partner responses to pain in metastatic breast cancer. Pain. 2011; 152: 2592-2604.
Cleeland C, Syrjala K. How to assess cancer pain. In: Turk D, Melzack R, eds. Handbook of Pain Assessment. New York: Guilford; 1992: 362-387.
Cranford J, Shrout P, Iida M, et al. A procedure for evaluating sensitivity to within-person change: Can mood measures in diary studies detect change reliably? Personal Soc Psychol Bull. 2006; 32: 917.
Shiffman S, Stone A, Hufford M. Ecological momentary assessment. Annu Rev Clin Psychol. 2008; 4: 1–32
Larsen R, Diener E. Promises and problems with the circumplex model of emotion. Rev Personality Soc Psychol. 1992; 13: 25-59.
Shrout P, Lane S. Psychometrics. In: Mehl M, Conner T, eds. Handbook of Research Methods for Studying Daily Life. New York: Guilford; 2012: 302-320.
G. S. Dyadic Adjustment Scale. In C. M.-h. S. Inc (ed), 1986.
Muthén LK, Muthén BO. Mplus user’s guide. 6th ed. Los Angeles: Muthén & Muthén; 2010.
Muthén B, Asparouhov T. Beyond multilevel regression modeling: Multilevel analysis in a general latent variable framework. In: Hox J, Roberts JK, eds. Handbook of Advanced Multilevel Analysis. New York: Taylor and Francis; 2011: 15-40.
Diener E, Emmons RA. The independence of positive and negative affect. J Personal Soc Psychol. 1984; 47: 1105-1117.
Costa PT, McCrae RR. Influence of extraversion and neuroticism on subjective well-being: Happy and unhappy people. J Personal Soc Psychol. 1980; 38: 668-678.
Bolger N, Zuckerman A, Kessler RC. Invisible support and adjustment to stress. J Personal Soc Psychol. 2000; 79: 953-961.
Horner M, Ries L, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2006. Bethesda, MD: National Cancer Institute, http://seer.cancer.gov/csr/1975_2004/, posted to the SEER web site, 2006.
Stone A, Broderick J, Schwartz J, et al. Intensive momentary reporting of pain with an electronic diary: Reactivity, compliance, and patient satisfaction. Pain. 2003; 104: 343-351.
Iida M, Shrout P, Laurenceau JP, Bolger N. Using diary methods in psychological research. In H. Cooper (ed), APA Handbook of Research Methods in Psychology: Vol 1. Foundations, Planning, Measures, and Psychometrics. Washington DC: American Psychological Association, 2012: 277–305.
Lida M, Seidman G, Shrout PE, Fujita K, Bolger N. Modeling support provision in intimate relationships. J Personal Soc Psychol. 2008; 94: 460-478.
Cole DA, Maxwell SE. Testing mediational models with longitudinal data. J Abnorm Psychol. 2003; 112: 558-577.
Watson JC, Rennie DL. Qualitative analysis of clients’ subjective experience of significant moments during the exploration of problematic reactions. J Couns Psychol. 1994; 41: 500-509.
Cordova MJ, Cunningham LLC, Carlson CR, Andrykowski MA. Social constraints, cognitive processing, and adjustment to breast cancer. J Consult Clin Psychol. 2001; 69: 706-711.
Kennedy-Moore E, Watson JC. How and when does emotional expression help? Rev Gen Psychol. 2001; 5: 187-212.
Acknowledgments
This research was supported by a multi-disciplinary award from the U.S. Army Medical Research and Materiel Command W81XWH-0401-0425 (Hoda Badr, PhD, Principal Investigator). The authors thank Leslie Schart and Krystal Davis who assisted with data collection. We would also like to acknowledge the assistance of Drs. Massimo Cristofanilli, Daniel Booser, Aman Buzdar, Francisco Esteva, Ana Gonzalez-Angulo, Marjorie Greene, Nuhad Ibrahim, Lajos Pusztai, Edgardo Rivera, Vicente Valero, and Ronald Walters for allowing access to their patients for this study.
Conflict of Interest Statement
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Badr, H., Pasipanodya, E.C. & Laurenceau, JP. An Electronic Diary Study of the Effects of Patient Avoidance and Partner Social Constraints on Patient Momentary Affect in Metastatic Breast Cancer. ann. behav. med. 45, 192–202 (2013). https://doi.org/10.1007/s12160-012-9436-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-012-9436-8