Abstract
Background
Health behaviour models typically neglect habitual action. The Self-Report Habit Index (SRHI) permits synthesis of evidence of the influence of habit on behaviour.
Purpose
The purpose of this study is to review evidence around mean habit strength, habit–behaviour correlations, and habit × intention interactions, from applications of the SRHI to dietary, physical activity, and active travel behaviour.
Method
Electronic database searches identified 126 potentially relevant papers. Twenty-two papers (21 datasets) passed eligibility screening. Mean scores and correlations were meta-analysed using fixed, random and mixed effects, and interactions were synthesised via narrative review.
Results
Twenty-three habit–behaviour correlations and nine habit × intention interaction tests were found. Typical habit strength was located around the SRHI midpoint. Weighted habit–behaviour effects were medium-to-strong (fixed: r + = 0.44; random: r + = 0.46). Eight tests found that habit moderated the intention–behaviour relation.
Conclusion
More comprehensive understanding of nutrition and activity behaviours will be achieved by accounting for habitual responses to contextual cues.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Overweight and obesity continues to present a serious global public health risk [1]. Healthful dietary intake and regular physical activity represent key behavioural targets for weight management [2]. Yet, many people fail to meet nutrition and activity guidelines: a recent UK survey, for example, found that only 25% of men and 29% of women reported eating five portions of fruit and vegetables per day, and over 60% of men and 70% of women did not meet minimum physical activity recommendations [3]. Similar patterns are found in US national surveys [4, 5]. There remains a need to design effective behaviour change interventions to promote dietary and activity changes.
Health behaviour change depends on identifying and targeting modifiable determinants of action [6]. Approaches to behaviour change have traditionally been based on reasoned action models [7]. These models portray behaviour as the outcome of conscious deliberation and emphasise concepts such as intentions, attitudes, and self-efficacy. For example, the Theory of Planned Behaviour [8] and the Health Action Process Approach [9] posit that behaviour follows directly from a conscious decision to act, which summarises beliefs around the favourability and controllability of action. However, intention typically predicts only around 25–35% of variance in behaviour [10, 11], and a recent meta-analysis showed that interventions which succeed in changing intentions tend to generate relatively small-sized effects on behaviour [12]. This ‘intention–behaviour gap’ indicates that action is not consistently guided by motivation.
Dual-process theories suggest that behaviour can be initiated through two competing pathways: a deliberative route, which entails prior thought and cognitive effort (as depicted by reasoned action accounts), and an automatic route, which is characterised by environmentally cued responses which proceed in the absence of effort, volitional control, and awareness [13, 14]. Recent work has pointed to habit as a key automaticity-based determinant of action [15–17]. Habits are behavioural patterns learned through context-dependent repetition [17–20]: repeated performance in unvarying settings reinforces context-behaviour associations such that, subsequently, encountering the context is sufficient to automatically cue the habitual response [21].
Habit is hypothesised to have two related functions in determining action. First, assuming the everyday contexts that support habits remain stable and are regularly encountered, habit strength will correlate with behavioural frequency. Second, habits will interact with intentions in determining behaviour: in novel contexts, behaviour will be regulated by intention, but in familiar and unvarying settings, behaviour will be guided by habit, and intention will have little or no impact [22].
Measurement problems have, until recently, constrained progress in documenting the contribution of habit to action. Habit has traditionally been measured as past behavioural frequency [22], but frequency cannot distinguish between reasoned and automatic action because, in unvarying contexts, both repeated deliberation and habit can result in the same pattern of frequent behaviour [23, 24]. Habit has been defined as learned automated cue-contingent action [21], and a multiplicative combination of performance frequency (‘how often do you do behavior X?’) and cue stability (‘when you do behavior X, how often is cue Y present?’) appears to offer a useful habit index, but depends upon prior identification of relevant cues [25, 26]. The measure may thereby fail to detect, for example, habits prompted by temporal cues where only location cue stability is measured, making integration of evidence across behaviours and contexts problematic. Additionally, the measure fails to assess the strength of the automatic response which characterises habitual behaviour. The Self-Report Habit Index (SRHI [27]) overcomes such problems. The SRHI comprises 12 items relating to three characteristics of habitual action with which participants rate their (dis)agreement: automaticity (e.g. ‘[Behavior X is something…] I have no need to think about doing’), frequency (e.g. ‘…I do frequently’), and relevance to self-identity (‘…that's typically “me”’). The SRHI offers a standardised and reliable measure to assess habitual action and so permits evidence synthesis across behaviours and populations [28]. The measure has been found to conform to theoretical predictions by correlating with behavioural frequency, and moderating the intention–behaviour relation [29, 30]. The SRHI is currently the most commonly used measure of habit in health behaviours [28].
Applications of the SRHI have shown dietary behaviours, physical activity, and sedentary behaviours to have a habitual component for many people, with habit predicting behaviour over and above reasoned concepts such as intentions, behavioural control, attitudes, and social norms [29–32]. Additionally, such studies have shown habit to interact with intentions in determining behaviour, such that the intention–behaviour relationship is diminished as habit strength increases [29–31]. Such findings have important implications for behaviour change initiatives. If unwanted habitual health-risk behaviours proceed without forethought, then shifts in motivation may fail to change behaviour [33]. Different techniques are needed to disrupt ‘bad’ habits than are required to change reasoned action [33, 34]. Additionally, forming habits for health-promoting behaviours may prevent relapse and aid maintenance of behaviour change beyond the duration of an intervention [33, 35].
Despite growing theoretical and empirical research interest in the relevance of habit to health behaviour [16, 17, 31], no systematic review of applications of the SRHI to dietary and physical activity habits is available. A review of this literature would be of practical benefit. Synthesising the strength of everyday habits across behaviours and samples may point to the typical prevalence of health-related habits. Estimation of typical strength of habits for specific health behaviours would be informative for intervention design, because behaviour change interventions may be most effective when tailored to habit strength of the focal behaviour [33]. Examination of the typical habit–behaviour association, and the robustness of the hypothesised effect of habit on the intention–behaviour relationship, would highlight whether habit disruption or formation is likely to offer a useful route to changing behaviour.
The Present Study
This study reviewed and synthesised evidence on the relevance of habit to nutritional behaviour and physical activity, based on applications of the SRHI. Three research questions were addressed:
-
1.
How habitual have dietary and physical activity behaviours been in previously studied samples?
-
2.
What is the overall association between habit and behaviour in studies of nutrition and physical activity?
-
3.
Does habit consistently moderate the intention–behaviour relationship in studies of nutrition and physical activity?
Method
Search Strategy
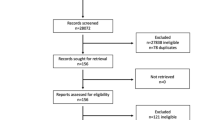
A descendency search was conducted to locate papers which have used Verplanken and Orbell's Self-Report Habit Index [27] (see Figure 1). Five psychology and health databases (PsycInfo, Medline, Embase, Web of Knowledge, Scopus) were searched on 29 January 2011. In each database, Verplanken and Orbell's paper [27] was first located and citing articles were subsequently identified. No date limits were set.
Eligibility Criteria
Papers were accepted only where they were written in English, published in full-text format in peer-reviewed journals, and reported analyses of primary data in which the SRHI was used to operationalise behavioural habit(s) relating to dietary intake (excluding alcohol consumption) or physical activity or inactivity. Studies of active travel habits (e.g. walking, cycling) were included, but inactive travel habits (car or public transport use) were excluded because switching from inactive to active travel may not be feasible for longer journeys.
Studies were retained only where a statistical association between the SRHI and a matched (i.e. habit consistent) or directly opposed (counterhabitual) behaviour was reported (or provided by the author when subsequently contacted), or where the SRHI was investigated as a moderator of the relationship between an intention and a habit consistent or counterhabitual behaviour. For the current purposes, a moderator variable was defined as a ‘variable [i.e. habit] that affects the direction and/or strength of the relation between an independent or predictor variable [intention] and a dependent or criterion variable [behaviour]’ ([36], p. 1174; square brackets added). Explorations of habit as a potential moderator of relationships between motivational variables other than intention (e.g. attitudes [37]) and behaviour were excluded.
Papers which reported secondary data (i.e. reviews) or focused on habitual thought (e.g. [38]) were excluded. We also removed papers which employed an abbreviated (<12-item) SRHI, unless study authors informed us that a 12-item SRHI was measured but not reported in published analyses (e.g. [29]). Intervention evaluations were retained if data could be extracted from pre-intervention baseline or a no-treatment control group.
Screening Procedure
All references were screened in two stages by one reviewer (BG) against eligibility criteria. Initial screening was based on titles, abstracts, and keywords. Remaining studies were subjected to full-text inspection. A second reviewer (PL) independently filtered 20% of papers at both screening stages, and 100% agreement was found between reviewers.
Data Extraction
Up to 36 data segments were coded from each dataset by one coder (BG) using an a priori data extraction form. Data extracted related to: descriptions of sample, setting, measures, and design; SRHI means, standard deviations, ranges, and reliability alphas; bivariate SRHI-behaviour correlations; and, where applicable, details of the hypothesised moderating effect of habit on the intention–behaviour relation, and the predictive utility of intention and behaviour at high, moderate, and low levels of habit [39]. Focal habits and behaviours were coded into one of three prespecified behavioural domains: nutrition (healthful or unhealthful diet), general physical activity, or inactivity, and active travel. Active travel was isolated from general physical activity given growing research interest in travel mode choice as a health-oriented behaviour [40, 41].
Potential between-study sources of bias were assessed by coding for four methodological variables pertaining to study design (whether cross-sectional or prospective), behaviour measure (self-report or objective; actual or typical behaviour), and sample (university-based, school-based or general adult population). Study design may bias effects because the SRHI features items relating to past behaviour frequency, and so cross-sectional designs may inflate true habit–behaviour correlations. Self-reported behaviour measures are prone to memory and self-presentational biases [42]. Actual frequency (behaviour measured in relation to a discrete time period) gives a more specific account of behaviour than does typical frequency (where no timeframe is specified). On these bases, we created a dichotomous indicator of study quality for analysis of correlations, which treated studies as low quality where they were (a) cross-sectional and based on (b) self-reported and (c) typical behaviour, and all other studies as acceptable quality. For comprehensiveness, we also coded for which population was sampled. However, we had no a priori expectation that effects should differ across populations.
Insufficient information in published papers prompted us to seek unpublished material from five authors (including two of the present authors; BG and GJdB) in relation to 12 datasets. Of the three external authors contacted, two responded, though not all requested information was provided.
Where unpublished data provided by authors differed from that reported in published papers (e.g. due to fluctuations in sample size when running bivariate habit–behaviour correlations rather than multi-variable correlation matrices), data received from authors were prioritised.
Thirty five percent of datasets (including published and unpublished material) were second-coded by an independent coder (PL), with 97% agreement found. Disagreements were resolved through discussion.
Prospective Studies
Where habit or behaviour was measured on multiple occasions, habit data were taken from the earliest timepoint, and behaviour data from the earliest follow-up timepoint, so as to observe the causal sequence of habit–behaviour relationships [22].
Intervention Studies
Where data were obtained from trials of behaviour change interventions, habit and behaviour data were preferably extracted from baseline measures relating to control and intervention groups combined [43], or taken from a no-treatment control group [44], depending on data provided by the study author.
Multiple Behaviour Measures
In one study ([37], study 2, (un)healthy dietary choices were indexed both by a 7-day self-reported sweet (candy) consumption diary, and by observation of participants' choice of either a chocolate or fruit snack as an ostensible reward for participation. The latter behaviour measure was entered into analysis so as to ensure greater compatibility with the habit measure, which related to ‘eating chocolate’.
Analysis Strategy
Habit mean and standard deviations, and observed habit–behaviour correlations were entered into respective meta-analyses.
We adopted a narrative approach to synthesis of the moderating effect of habit on the intention–behaviour relation. Moderation is typically investigated using multiple regression models, with moderation evidenced where the multiplicative product of the hypothesised moderator (habit) and predictor (intention) variables makes a statistically significant contribution, over and above the independent main effects of moderator and predictor variables, to explanation of variance in a dependent variable (behaviour [39]). A ‘moderation effect’ is thus a significant partial correlation between the habit × intention interaction term and behaviour, controlling for other variables in the multiple regression model. Variation across studies in the variables partialled out of the regression model renders partial correlation effects non-comparable, and so meta-analysis is not appropriate in this instance.
Calculating Effect Sizes
Means
Meta-analysis of mean habit scores required that all data be expressed in a standardised form, and so percentage mean and standard deviation (SD) scores were computed using the following formulae. Where raw SRHI scores were obtained on a scale ranging from 1 to X: mean (percent) = ((Y − 1)/(X − 1)) × 100, and SD = (Z/(X − 1)) × 100, where Y is SRHI mean score and Z is SRHI SD. Where SRHI scores ranged from −X to X: mean (percent) = ((Y + X)/(X × 2)) × 100; SD = (Z/X × 2) × 100. Resultant percentage scores indicate the mean extent to which participants agree with 12 statements portraying the focal behaviour as habitual (e.g. ‘[Behavior X] is something: ‘I do automatically’, ‘I do without having to consciously remember’; p. 1329 [27]), where 100% represents complete agreement (i.e. strongest possible habit), 50% represents neither agreement nor disagreement, and 0% indicates complete disagreement (complete absence of habit). While no standard cutoff point has been proposed for the SRHI, for the current purposes we interpreted scores above the midpoint as indicating the presence of habit [17].
The SRHI is frequently operationalised on seven-point scales, and so to permit cross-study comparisons, we also report mean and SDs on 1–7 scales in Tables 1 and 2. Where original studies did not employ 1–7 scales, scores were converted from calculated percentages using the formula: mean (1–7 scale) = (A × 0.06) + 1, and SD (1–7 scale) = B × 0.06, where A is SRHI mean and B is SRHI SD both expressed as percentages.
Habit–Behaviour Correlations
Pearson's product-moment correlation coefficient (r) was used as the effect size for analyses of bivariate habit–behaviour associations. The directionality of (negative) correlations between habit and counterhabitual behaviour was reversed prior to weighting for analysis purposes.
Effects were weighted by observed sample sizes for behavioural domain-specific analyses. A priori power analysis for the estimated weighted mean correlation coefficient was calculated using conservative estimates of model parameters [45]. Assuming the availability of 15 datasets, each with a mean within-study N of 80, and statistical significance set at 0.05, power to detect a small effect (r = 0.10 [46]) using a fixed-effects model was 0.97. Assuming also high between-study heterogeneity, power to detect a small effect using random effects procedures was 0.80.
One dataset ([37], study 2) generated two habit–behaviour effects relevant to the same behavioural domain (nutrition: fruit consumption, chocolate consumption), and based on the same behaviour variable (ratio of chocolate versus fruit snacks chosen by participants at the end of the study sessions). The former effect was excluded from analysis and the latter effect retained due to superior reliability of the habit measure (chocolate α = 0.92; fruit α = 0.86).
Two datasets (marked with asterisks in Table 1) yielded two habit–behaviour correlations relevant to more than one behavioural domain; in both cases, Dutch samples provided data on unhealthful diet habits and behaviour and physical inactivity habits and behaviour [32, 47]. To avoid overrepresentation of each sample, mean within-dataset effects were used to calculate the grand weighted mean habit–behaviour association. Both within-dataset effects were entered independently into subgroup analyses (described below) so as to retain all available data, but to avoid double-counting sample sizes were divided by two (i.e. the number of relevant habit–behaviour correlations) and rounded downwards where this did not produce a whole number (e.g. 383/2 = 191.5 ≈ 191). This treatment does not acknowledge the interdependence of the two effect estimates [48], and so sensitivity analyses were undertaken to explore whether interpretation of meta-analytic coefficients differed according to alternative treatment of the two datasets (i.e. exclusion, or inclusion of higher or lower correlation coefficient only). No differences were found: correlation coefficients varied by a maximum of 0.015 and subgroup analyses yielded stable results across all treatments.
Meta-analysis of Means and Correlations
Meta-analyses were undertaken using Comprehensive Meta Analysis (CMA) software (Version 2.2.057 [49]). Both fixed and random effects models were employed to permit inferences both about effects specific to the observed studies (fixed effects) and the likely distribution of effects in the population from which these studies have been sampled (random effects [50]). Weighted average effect sizes (r + ) were calculated using Fisher's Z transformations [51]. 95% confidence intervals (CIs) were calculated for each r + value. Following Cohen's guidelines [46], correlation coefficients of 0.10, 0.30, and 0.50 were interpreted to be small, medium, and large in size, respectively.
Statistical heterogeneity was assessed using Q and I 2 statistics. Q assesses the presence versus absence of heterogeneity, by testing the hypothesis that observed variance in effects is no greater than would be generated by sampling error. Statistically significant Q values indicate heterogeneity. I 2 quantifies heterogeneity as the ‘percentage of total variation across studies that is due to heterogeneity rather than chance’ ([52] p. 558). Heterogeneity was interpreted as high where I 2 was over 75%, moderate if over 50%, and low at 25% [52].
Subgroup analyses were undertaken to explore whether habit mean scores or habit–behaviour effects systematically differed across behavioural domain, and whether between-study methodological characteristics biassed effects. Effects of study quality were assessed for habit–behaviour correlations (a table of these data is available as Electronic Supplementary Material). Mixed effects analysis was used. Q statistics were generated to assess between-study variability (Q B ) attributable to potential moderators, and to evaluate heterogeneity within each of the subgroups (Q W ). Moderating variables were denoted by significant Q values. Where variables generated three subgroups, dummy variables were also used to investigate between-subgroup differences. Behaviour measures, and so study quality, were not expected to influence habit mean scores and hence were assessed as potential moderators of habit–behaviour correlations only.
Publication bias was assessed by calculating Rosenthal's failsafe N, which estimates the number of studies needed to reduce weighted habit–behaviour correlations to statistical non-significance (p > 0.05 [53]). Larger failsafe N values denote a more robust r + .
Results
A total of 126 potentially relevant papers were identified, including 125 unique citations generated by the database search, and Verplanken and Orbell's paper [27]. Title, keyword, and abstract screening against eligibility criteria removed five papers, and subsequent full-text screening removed a further 99 papers. The 22 eligible papers were based on 21 unique datasets.
Study Characteristics
The 21 datasets reported 23 relevant and unique bivariate habit–behaviour correlations and nine tests of the moderating effect of habit on the intention–behaviour relation (see Table 1). Mean within-dataset sample size (N) was 294.
Of 13 diet and nutrition habit–behaviour correlations, four related to healthful and nine to unhealthful dietary habits. Five correlations focused on general physical activity, two on inactivity, and three on active travel. Four moderation tests related to activity or inactivity, three to nutrition, and two to active travel.
Habit measures showed satisfactory alphas within all datasets (minimum α = 0.84).
Fourteen datasets used prospective designs, and seven were cross-sectional. Behaviour was measured via self-report in 19 datasets, of which 13 focused on actual behaviour over a given period and eight on typical behavioural patterns. Two datasets used objective behaviour measures (observed food choice in a lab setting [37, study 2; 56]). Most samples were university-based (14 datasets).
Habit Mean Scores
As Table 2 shows, the grand weighted mean SRHI score across behaviours, expressed as a percentage, was ~50%. Scores were below the midpoint for healthy and unhealthy eating (both ~43%), but above the midpoint for studies of physical activity or inactivity (both ~60%) and active travel (~55%). Nutrition mean scores were significantly lower than those for general physical (in)activity (Q B = 52.59, p < 0.001), but active travel scores did not differ from nutrition or activity. There was strong heterogeneity within each sub-domain (minimum I 2 = 80.98, p = 0.02), and, across all studies and behaviours, raw within-study standard deviation scores ranged from 16 to 30 percentage points (see Table 1), suggesting considerable variation around weighted mean scores.
Neither study design (Q B = 0.18, p = 0.68) nor sample (Q B = 0.82, p = 0.66) explained variation in mean scores.
Habit–Behaviour Correlations
The average weighted correlation between habit and behaviour across all studies was estimated at r + = 0.44 using a fixed model (p < 0.001), and r + = 0.46 using a random effects model (p < 0.001), indicating a moderate to strong effect (see Table 2). This effect was robust (failsafe N = 7,011), but strong heterogeneity was observed around the mean (Q = 223.01, p < 0.001; I 2 = 91.03). All habit–behaviour correlations reported below were significant at p < 0.001.
The weighted habit–behaviour correlation effect estimate for nutritional habits was moderate to strong in size (fixed: r + = 0.43; random: r + = 0.41), and effects were of equal magnitude across healthful (fixed: r + = 0.43; random: r + = 0.42) and unhealthful (fixed: r + = 0.42; random: r + = 0.41) dietary habits. General physical activity habits correlated with behaviour at r + = 0.43 (fixed; random: r + = 0.44). This effect was underpinned by correlations of r + ≈ 0.42 (fixed: r + = 0.43; random: r + = 0.44) for activity habits, and r + = 0.47 (both fixed and random) for inactivity habits. Habit–behaviour correlations in the domain of active travel were significantly stronger (fixed: r + = 0.65; random: r + = 0.70) than those observed for general physical activity or nutrition (Q B = 12.79, p < .001), but this effect may be an artefact of the lack of active travel studies (k = 3) relative to activity or nutrition (k = 20). Nutrition and activity correlations did not differ.
With the exception of physical inactivity, all weighted correlations were robust (minimum failsafe N = 308) and highly heterogeneous (minimum Q = 23.21, p = 0.001; minimum I 2 = 74.15). While physical inactivity correlations appeared homogeneous (Q = 1.01, p = 0.31; I 2 = 1.23), the small number of available studies (k = 2) is likely to have underpowered heterogeneity analyses [56], and precluded calculation of failsafe Ns.
Correlations did not differ by study quality, sample, design, whether actual or typical behaviour was measured, or whether behaviour was self-reported or objective (maximum Q B = 2.31, p = 0.13).
Tests of Habit as Moderator of Intention–Behaviour Relationship
Four of the nine studies investigating the effect of habit on the intention–behaviour relation used cross-sectional, and five prospective, designs. Eight studies found moderation (Table 3). With the exception of one study, which examined intention–behaviour correlation coefficients at three levels of habit but did not compute an overall interaction effect [15], all studies used moderated multiple regression, whereby a significant partial correlation for the habit × intention interaction term (controlling for intention and habit as independent predictors) denotes moderation. Effects were subsequently investigated using ‘simple slopes analysis’, whereby regression coefficients (beta weights) are examined at three levels of habit (typically at one standard deviation below the mean [weak or no habit], at the mean [moderate habit], and at one standard deviation above the mean [strong habit] [39]).
In six studies, habit, intention, and other variables derived from the Theory of Planned Behaviour (attitudes [subdivided into instrumental attitude and affective attitude in two studies], subjective norms, perceived behavioural control) were partialled out of the moderated multiple regression models. Two studies controlled for intention and habit only.
Nutrition
All three studies of the habit × intention interaction in nutrition behaviour pointed to moderation [15, 31, 57]. In two studies which used moderated multiple regression [31, 57], a graded reduction was observed in beta weights for intention as habit strength increased. De Bruijn [31] showed that intentions remained significantly predictive of fruit consumption, albeit less strongly so, at higher levels of habit.
De Bruijn et al. [15] observed that fruit consumption intentions correlated most strongly with behaviour where habit was weakest (r = 0.32), but remained significantly correlated at moderate and strong levels of habit (both rs = 0.23).
General Physical (In)Activity
One study of leisure-time activity found no moderation effect when controlling for habit, TPB variables, intention stability, and an interaction between intention and intention stability (p = 0.12 [58]). Beta coefficients for intention at each level of habit were not reported.
Chatzisarantis and Hagger ([59] studies 1 and 2) showed that intentions to engage in vigorous physical activity or active sports became less associated with behaviour as habit strength increased, but beta weights were not provided to illustrate this effect. Kremers and Brug ([30] study 2) reported a significant interaction between screen-viewing habits and intentions. Given non-reporting of beta weights, inspection of p values demonstrated that intention predicted behaviour only where habit was weak or moderate.
Active Travel
Both active travel studies in which moderation was investigated related to bicycle use, and found significant summary effects. In both studies, beta weights for intentions decreased as habit strength increased ([29] (study 2); [40]), though Gardner ([29] study 2) found that intention to commute by bicycle did not predict behaviour at any level of habit. De Bruijn et al. [40] reported that intentions had no relationship with behaviour where habit was strong.
Discussion
We systematically reviewed the literature around the influence of habit on dietary and (in)activity behaviours, based on applications of the Self-Report Habit Index (SRHI). Meta-analysis of habit scores revealed that strongest habits were reported in relation to physical (in)activity and active travel. Weighted mean habit–behaviour correlations were typically medium to large in size, and active travel correlations were strongest. In eight of nine tests, habits moderated the intention–behaviour relationship, such that the impact of intention on behaviour diminished as habit strength increased. These results highlight the importance of integrating habit into behaviour change theory and practice.
In the absence of intervention, mean habit scores may point to the extent to which habituation of a given behaviour is likely to naturally occur. Using the scale midpoint as a crude operational boundary to determine the presence or absence of habit [17], and assuming normal within-study habit score distributions, the location of the grand weighted mean standardised habit score at the midpoint suggests that around half of each sample reportedly perform the focal behaviour habitually. The medium-to-large grand weighted mean habit–behaviour correlation (r + ≈ 0.45) suggests that habit alone can explain around 20% of variation in nutrition and physical activity-related behaviours (i.e. R 2 ≈ 0.20). Meta-analyses have pointed to similar-sized correlations with behaviour for intention (0.47 [10]), control (0.37 [10]), and affect (0.42 [60]), and so habit may be as important a proximal determinant of action as these constructs.
While it was not possible to meta-analyse interaction effects, in almost all studies, habit moderated the relationship between intention and behaviour, such that intentions had reduced impact on behaviour where habit was strong. This finding must however be interpreted cautiously, as it may reflect a bias towards publication of studies which find significant interaction, and so an overestimation of the robustness of this effect. Additionally, all studies in which habit interacted with intention focused on intention-concordant habits and many reported strong habit–intention correlations (e.g. [29]). This compromises the external validity of statistically modelled effects of strong intentions where habit is weak, and vice versa, because habit–intention conflicts were rarely observed within the sample. Explorations of the role of counterintentional habits on the intention–behaviour relationship, such as the capacity for habitual snacking to obstruct intentions to eat a healthful diet [61], are needed. Notwithstanding these limitations, our results suggest that models which portray intention as the key antecedent of action may overemphasise the role of forethought in behaviour [29]. The predictive and explanatory utility of these models may be increased by incorporating habit as a determinant of action situated on a parallel, cue-driven pathway to behaviour and a variable which can bypass deliberation and obstruct the translation of intention into action [14, 62]. A more comprehensive model of nutrition and activity behaviour may also require a temporal element, so as to acknowledge that frequent performance of reasoned action leads to habit formation [17, 20].
Our results have important implications for behaviour change practice. The failure of intention to translate into action where habit is strong suggests that motivation change, while likely to be necessary for behaviour change, will not change unhealthful (‘bad’) habits, and so the cue–response association underpinning habitual action must be disrupted [33]. Purposive discontinuation of exposure to the everyday cues that support habits [26, 63] may be an unrealistic intervention strategy, but using volitional strategies such as vigilant monitoring (i.e. heightening attention to behaviour so as to detect habit initiation) can inhibit performance of ‘bad’ habits [64]. We showed that healthful behaviours can habituate. The formation of healthful (‘good’) habits, so as to aid maintenance of behaviour change, thus represents a realistic goal for health promotion campaigns [35]. Such campaigns should focus on promoting consistent repetition of behaviour in unvarying contexts [17, 20].
We found considerable between-study variation in mean habit scores and in habit–behaviour correlations, but subgroup analyses could not reliably attribute heterogeneity to methodological characteristics. Habit scores varied by around twenty percentage points between behaviours, with significantly higher scores observed for physical activity than nutritional behaviour. These discrepancies may perhaps point to differences in the extent to which these behaviours are liable to become habitual, based on intrinsic properties of the behaviours or stability of the contexts in which they are performed. Alternatively, between-study variation in habit strength may be attributable to covariates pertaining to the populations studied. Active travel habits, for example, were predominantly documented in the Netherlands, where bicycling is the main mode of transport for short journeys [65], which may make bicycle habit formation more likely. Further work in more diverse samples is needed to explore potential sources of variation in habit formation.
There are several important limitations to this work. Many of the studies used cross-sectional designs, and so modelled habit as a predictor of past behaviour. This fails to acknowledge the expected temporal sequence between habit and behaviour [62], and is also conceptually problematic given that, at least in early stages of habit formation, repeated action strengthens habit [17]. We also documented a reliance on self-reports of behaviour, which are prone to inaccuracy. Two studies which used objective measures posted lower habit–behaviour correlations, suggesting that self-reports of action may inflate true effects. More methodologically rigorous research is required to provide more conceptually coherent and less biassed observations of the influence of habit on action.
Concerns have been raised around the validity of the SRHI for modelling habit–behaviour correlations [31]. Some SRHI items relate to behavioural frequency (e.g. ‘[Behaviour X…] is something I do frequently’, ‘is something I have been doing for a long time’), and so are likely to inflate the habit–behaviour correlation. Some researchers have removed frequency items when applying the SRHI, with no apparent losses in reliability [17, 29]. Indeed, a study that removed two frequency items from the SRHI was re-analysed using the full 12-item SRHI for our meta-analysis [29]. The SRHI-behaviour correlation (r = 0.86) was attenuated using the abbreviated index (r = 0.80), and marginally lower mean scores were observed (expressed as percentages of maximum scores, M = 69.67 vs 67.50, respectively), but reliability and habit × intention interaction coefficients were identical. Various subscales have been proposed, and we synthesised evidence using the 12-item SRHI for the purpose of between-study consistency. Future reviews of this literature would however be aided by the use of a SRHI subscale which removes frequency and so may permit a truer estimate of the relationship between cue–response association strength and behavioural performance [23].
We have shown that considerable proportions of the samples studied in observational studies to date have reported dietary or exercise habits. Habits were shown to not only consistently correlate with behaviour but also typically reduce the predictive utility of reasoned intentions for predicting behaviour. Effects were consistent and highly robust between and within studies of (un)healthful dietary behaviour, physical (in)activity, and active travel. Traditional models may have overstated the importance of deliberation in determining health action. A more comprehensive understanding of nutrition and activity behaviours, and how they might be changed, will be achieved by integrating habitual responses to contextual cues into theoretical accounts of behaviour.
References
References marked with an asterisk are at least partly based on a dataset included in the meta-analysis
Organisation for Economic Co-operation and Development. OECD Health Data 2010. Paris: Organisation for Economic Co-operation and Development; 2010.
World Health Organisation. WHO Mega Country Health Promotion Network: Behavioural Risk Factor Surveillance Guide. Genera: World Health Organisation; 2002.
Craig R, Mindell J, Harani V. Health Survey for England 2008. London: NHS Information Centre; 2009.
Centers for Disease Control and Prevention. U.S. Physical Activity Statistics. 2010. Available at http://apps.nccd.cdc.gov/PASurveillance/StateSumResultV.asp?CI=&Year=2007&State=0#data. Accessed August 17 2010.
Kimmons J, Gillespie C, Seymour J, Serdula M, Blanck HM. Fruit and vegetable intake among adolescents and adults in the United States: Percentage meeting individualized recommendations. Medscape Journal of Medicine. 2009; 11: 26.
Bartholomew LK, Parcel GS, Kok G, Gottlieb NH. Intervention mapping: Designing theory and evidence-based health promotion programs. San Francisco: Jossey-Bass; 2006.
Conner M, Norman P. Predicting health behaviour: A social cognition approach. In: Conner M & Norman P, eds. Predicting health behaviour: Research and practice with social cognition models. 2nd ed. Buckingham: Open University Press; 2005: 1–27.
Ajzen I. The theory of planned behavior. Organ Behav Hum Dec. 1991; 50: 179–211.
Schwarzer R. Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Appl Psychol—Int Rev. 2008; 57: 1–29.
Armitage CJ, Conner M. Efficacy of the Theory of Planned Behaviour: A meta-analytic review. Brit J Soc Psychol. 2001; 40: 471–99.
Godin G, Kok G. The theory of planned behavior: A review of its applications to health-related behaviors. Am J Health Promot. 1996; 11: 87–98.
Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? An analysis of the experimental evidence. Psychol Bull. 2006; 132: 249–68.
Bargh JA. The four horsemen of automaticity: Awareness, intention, efficiency, and control in social cognition. In: Wyer RS, Srull TK, eds. Handbook of social cognition. Vol. 1. Hillsdale, NJ: Lawrence Erlbaum; 1996: 1–40.
Strack F, Deutsch R. Reflective and impulsive determinants of social behaviour. Pers Soc Psychol Rev. 2004; 8: 220–47.
* De Bruijn GJ, Kremers SPJ, De Vet E, De Nooijer J, Van Mechelen W, Brug J. Does habit strength moderate the intention-behaviour relationship in the Theory of Planned Behaviour? The case of fruit consumption. Psychol Health. 2007; 22: 899–916.
Kremers SPJ, De Bruijn GJ, Visscher TLS, van Mechelen W, de Vries NK, Brug J. Environmental influences on energy balance-related behaviors: A dual-process view. Int J Behav Nutr Phys Act. 2006; 3: 9.
Lally P, van Jaarsveld E, Potts HWW, Wardle J. How are habits formed? Modelling habit formation in the real world. Eur J of Soc Psychol. 2010; 40: 998–1009.
Aarts H, Paulussen T, Schaalma H. Physical exercise habit: on the conceptualization and formation of habitual health behaviours. Health Educ Res. 1997; 12: 363–74.
Danner UN, Aarts H, de Vries NK. Habit formation and multiple means to goal attainment: Repeated retrieval of target means causes inhibited access to competitors. Pers Soc Psychol Bull. 2007; 33: 1367–79.
Lally P, Wardle J, Gardner B. Experiences of habit formation: A qualitative study. Psychol Health Med (in press)
Orbell S, Verplanken B. The automatic component of habit in health behavior: Habit as cue-contingent automaticity. Health Psychol. 2010; 29: 374–83.
Triandis H. Interpersonal behavior. Monterey, CA: Brooks-Cole; 1977.
Ajzen I. Residual effects of past on later behavior: Habituation and reasoned action perspectives. Pers Soc Psychol Rev. 2002; 6: 107–22.
* Verplanken B. Beyond frequency: Habit as mental construct. Brit J Soc Psychol. 2006; 45: 639–56.
Ouellette JA, Wood W. Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychol Bull. 1998; 124: 54–74.
Wood W, Tam L, Witt MG. Changing circumstances, disrupting habits. J Pers Soc Psychol. 2005: 88, 918–33.
* Verplanken B, Orbell S. Reflections on past behavior: A self-report index of habit strength. J Appl Soc Psychol. 2003; 33: 1313–1330.
Verplanken B, Myrbakk V, Rudi E. The measurement of habit. In: Betsch T, Haberstroh S, eds. The routines of decision making. Mahwah, NJ: Lawrence Erlbaum; 2005: 231–47.
* Gardner B. Modelling motivation and habit in stable travel mode contexts. Transport Res F – Traf. 2009; 12: 68–76.
* Kremers SPJ, Brug J. Habit strength of physical activity and sedentary behavior among children and adolescents. Pediatr Exerc Sci. 2008; 20: 5–17.
* De Bruijn GJ. Understanding college students' fruit consumption. Integrating habit strength in the theory of planned behaviour. Appetite. 2010; 54: 16–22.
* Kremers SPJ, van der Horst K, Brug J. Adolescent screen-viewing behaviour is associated with consumption of sugar-sweetened beverages: The role of habit strength and perceived parental norms. Appetite. 2007; 48: 345–50.
Verplanken B, Wood W. Interventions to break and create consumer habits. J Public Policy Mark. 2006; 25: 90–103.
Aarts H, Verplanken B, Van Knippenberg A. Habit and information use in travel mode choices. Acta Psychol. 1997; 96: 1–14.
Rothman AJ, Sheeran P, Wood W. Reflective and automatic processes in the initiation and maintenance of dietary change. Ann Behav Med. 2009; 38 (S1):S4–S17
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986; 51: 1173–82.
* Conner M, Perugini M, O'Gorman R, Ayres K, Prestwich A. Relations between implicit and explicit measures of attitudes and measures of behaviour: Evidence of moderation by individual difference variables. Pers Soc Psychol Bull. 2007: 33; 1727–40.
Verplanken B, Velsvik R. Habitual negative body image thinking as psychological risk factor in adolescents. Body Image. 2008; 5: 133–40.
Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. London: Sage; 1991.
* De Bruijn GJ, Kremers SPJ, Singh A, Van Den Putte B, Van Mechelen W. Adult active transportation: Adding habit strength to the theory of planned behaviour. Am J Prev Med. 2009; 36: 189–94.
* Lemieux M, Godin G. How well do cognitive and environmental variables predict active commuting? Int J Behav Nutr Phys Act. 2009; 6: 12.
Paulhus DL. Self-deception and impression management in test responses. In: Angleitner A, Wiggins JS, eds. Personality assessment via questionnaire: Current issues in theory and measurement. New York: Springer; 1986: 143–65.
* Jurg ME, Kremers SPJ, Candel MJJM, Van Der Wal MF, De Meij JSB. A controlled trial of a school-based environmental intervention to improve physical activity in Dutch children: JUMP-in, kids in motion. Health Promot Int. 2006; 21; 320–30.
* Tam L, Bagozzi RP, Spanjol J. When planning is not enough: The self-regulatory effect of implementation intentions on changing snacking habits. Health Psychol. 2010: 29; 284–92.
Hedges LV, Pigott TD. The power of statistical tests in meta-analysis. Psychol Methods. 2001; 3: 203–217.
Cohen J. A power primer. Psychol Bull. 1992; 112: 155–159.
* De Bruijn GJ, Van Den Putte B. Adolescent soft drink consumption, television viewing and habit strength. Investigating clustering effects in the Theory of Planned Behaviour. Appetite. 2009; 53: 66–75.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Chichester: Wiley; 2009.
Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive meta analysis version 2.2.057. [Computer software]. Englewood, NJ: Biostat; 2010.
Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychol Methods. 1998; 3: 486–504.
Hedges LV, Olkin I. Statistical methods for meta-analysis. Orlando: Academic Press; 1985.
Higgins JPT, Thompson SG, Deeks JJ, Altman, DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327: 557–60.
Rosenthal R. Meta-analytic procedures for social research. London: Sage; 1984.
* Weijzen PLG, de Graaf C, Dijksterhuis GB. Predictors of the consistency between healthy snack choice intentions and actual behaviour. Food Qual Prefer. 2009; 20: 110–119.
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006; 11: 193–206.
* Brug J, de Vet E, de Nooijer J, Verplanken B. Predicting fruit consumption: Cognitions, intention, and habits. J Nutr Educ Behav. 2006; 38: 73–81.
* De Bruijn GJ, Kroeze W, Oenema A, Brug J. Saturated fat consumption and the theory of planned behaviour: Exploring additive and interactive effects of habit strength. Appetite. 2008; 51: 318–23.
* Rhodes R, De Bruijn GJ, Matheson DH. Habit in the physical activity domain: Integration with intention temporal stability and action control. J Sport Exerc Psychol. 2010; 32: 84–98.
* Chatzisarantis NLD, Hagger MS. Mindfulness and the intention-behavior relationship within the Theory of Planned Behavior. Pers Soc Psychol Bull. 2007; 33: 663–76.
Rhodes RE, Fiala B, Conner M. A review and meta-analysis of affective judgments of physical activity in adult populations. Ann Behav Med. 2010; 38: 180–204.
Verplanken B, Faes S. Good intentions, bad habits, and effects of forming implementation intentions on healthy eating. Eur J Soc Psychol. 1999; 29: 591–604.
Verplanken B, Aarts H, van Knippenberg A. Habit, information acquisition and the process of making travel mode choices. Eur J of Soc Psychol. 1997; 27: 539–560.
Verplanken B, Walker I, David A, Jurasek M. Context change and travel mode choice: Combining the habit discontinuity and self-activation hypothesis. J Environ Psychol. 2008; 28: 121–7.
Quinn JM, Pascoe A, Wood W, Neal DT. Can't control yourself? Monitor those bad habits. Pers Soc Psychol Bull. 2010; 36: 499–511.
Statistics Netherlands. Kernresultaten mobiliteit [Main Results Mobility]. 7th ed. Statistics Netherlands: Voorburg; 2002, pp12-13.
* Adriaanse MA, de Ridder DTD, Evers C. Emotional eating: Eating when emotional or emotional about eating? Psychol Health. 2011; 26: 23–39.
* Van Der Horst K, Kremers S, Ferreira I, Singh A, Oenema A, Brug J. (2007) Perceived parenting style and practices and the consumption of sugar-sweetened beverages by adolescents. Health Educ Res. 2007; 22: 295–304.
* Kremers SPJ, Dijkman MAM, De Meij JSB, Jurg ME, Brug J. Awareness and habit: important factors in physical activity in children. Health Educ. 2008; 108: 475–88.
* Verplanken B, Melkevik O. Predicting habit: The case of physical exercise. Psychol Sport Exerc. 2008; 9: 15–26.
Conflict of Interest Statement
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
12160_2011_9282_MOESM1_ESM.doc
Supplementary table. Mixed effect meta-analysis: methodological characteristics as potential moderators of habit–behaviour effects (N = 6173†; k = 23) (DOC 62 kb)
About this article
Cite this article
Gardner, B., de Bruijn, GJ. & Lally, P. A Systematic Review and Meta-analysis of Applications of the Self-Report Habit Index to Nutrition and Physical Activity Behaviours. ann. behav. med. 42, 174–187 (2011). https://doi.org/10.1007/s12160-011-9282-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-011-9282-0