Abstract
Background/Purpose
This study examined the relation of age to genitourinary functioning and depressive symptoms over time and examined how age influences the relation between genitourinary functioning and depressive symptoms over time in men treated for localized prostate cancer.
Methods
Participants were 234 men who completed interviews that assessed genitourinary functioning and depressive symptoms at 2, 4, 10 and 16 months after treatment. Analyses were statistically controlled for potential confounds.
Results
Compared with younger men (≤65.5), older men had significantly poorer sexual function and slower improvement. Level of urinary functioning was inversely associated with level of depressive symptoms regardless of age. Level of sexual functioning was inversely associated with level of depressive symptoms but only in younger men.
Conclusion
Interventions may be particularly helpful for all men with urinary dysfunction and for younger men with sexual dysfunction in order to improve symptoms of depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is the most common noncutaneous cancer and the second leading cause of cancer death in men [1]. Prostate cancer was once thought to be a disease of elderly men, but the use of prostate screening tests such as the prostate-specific antigen (PSA) test has increased the detection of early-stage disease [2], resulting in increased diagnosis in younger men [3]. The present study adds to the literature [4–7] on how age might influence trajectories of improvements in functioning following prostate cancer treatments, as well as how older and younger men adjust emotionally to the physical impairments that accompany prostate cancer and its treatments.
Due to early detection, it is estimated that 91% of new cases of prostate cancer are diagnosed at local or regional stages, for which 5-year relative survival approaches 100% [1]. Despite high survival rates, prostate cancer treatments can undermine quality of life in both younger and older men. Treatments for localized prostate cancer can have profound adverse effects on urinary and sexual functioning [3]. Common side effects of treatment include an increased urgency and frequency of urination, difficulty controlling urinary functioning, erectile dysfunction, and loss of sexual pleasure [8, 9]. In addition, some men with localized disease experience problems in domains of general health-related quality of life such as restrictions in role-related activities, decreased energy, and general health changes after treatment [8, 10]. Declines in general health perceptions and self-esteem have been reported just after treatment [10] when physical dysfunction is most evident. Traditionally, quality-of-life measures encompass both physical and psychological domains [11]. In the present study, we examine how functioning in the physical domains (urinary and sexual functioning) relates to functioning in a psychological domain (depression) in older and younger men.
The bodily impairment, life threat, and restrictions in role-related activities that are associated with prostate cancer may cause significant distress in men [12–15]. Specific treatment-related problems (i.e., sexual, urinary, and bowel dysfunction) have been associated with lower levels of mental and social functioning in men with prostate cancer [16]. These treatment-related problems are often thought to be of a personal and private nature, which can induce feelings of embarrassment, changes in body image, self-image, and self-esteem and have an adverse effect on a patient’s sexuality [17, 18].
Although the research is limited, it appears that younger cancer survivors generally have higher physical functioning and health than older survivors [4]. Even as far as 2 years after diagnosis, younger men have reported better urinary and sexual outcomes than older men [5]. These age differences can be attributed in part to normal age-related differences in biology that can make recovery time longer and reduce functioning resilience in older patients. Also, comorbid chronic illnesses and disabilities that are associated with aging can compound the physical impairments due to cancer and its treatment in elderly patients [19–21].
Older prostate cancer survivors do not appear to have worse mental health functioning than relatively younger survivors; if anything, they seem to have fewer mental health problems. Bisson and colleagues [6] found that younger age was predictive of cancer-related distress. In addition, Diefenbach and colleagues [7] found that higher Gleason scores, an indicator of prostate tumor aggressiveness, were associated with higher distress in younger men (≤68 years) but not in older men (>68 years). Studies with other cancer populations also report that older cancer survivors exhibit better psychological adaptation than younger survivors on measures such as depressive and anxious symptoms [22, 23] and cancer-related intrusive thoughts [24].
It is unclear as to why older persons would fare worse on measures of physical functioning but not mental health after having a life-threatening illness like cancer. In general, it appears that older adults cope more effectively with stressful life events than do younger adults [25]. It may be that over the life course, experiences and successes in coping with a variety of stressors build adaptive attitudes and beliefs that generalize to coping with new stressors [26]. Among men with prostate cancer, it is possible that older men have greater experience in dealing with genitourinary dysfunction and lower sexual drive even prior to having prostate cancer, due to other comorbid conditions or normal biological changes associated with aging. It also could be that older men attribute disease-related symptoms to normal aging, which may lessen their emotional distress [27].
In summary, there is some evidence that relative to younger men, older men may have poorer genitourinary functioning [5] but potentially better mental health [6]. However, we could find no studies that examined the relation between posttreatment genitourinary functioning and depressive symptoms in younger versus older prostate cancer survivors. Thus, the present longitudinal study represents a conceptual replication of prior research on age-related differences in the rate and magnitude of improvement of genitourinary functioning and depressive symptoms over time; it also expands upon the literature by examining how age might moderate the relation between genitourinary functioning and depressive symptoms.
Based on the literature, we hypothesized that relative to younger men, older men would have more severe and longer-lasting genitourinary dysfunction including sexual and urinary difficulties. Second, we hypothesized that older men would have fewer symptoms of depression than younger men. Third, we hypothesized that there would be a stronger association between genitourinary dysfunction and depressive symptoms in younger men than in older men.
Methods
Participants
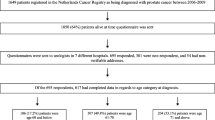
Study participants were recruited through the offices of urologists and radiation oncologists in the greater Pittsburgh area for participation in a clinical trial examining the effects of psychoeducational and support group interventions on men’s adjustment to prostate cancer. For greater detail regarding methodology, please refer to the published clinical trial [28]. Eligibility criteria included: (1) treated for localized prostate cancer within the preceeding 2 months; (2) no history of other cancer; (3) primary residence within 1-h driving distance from Pittsburgh, PA; (4) nonmetastatic disease at time of diagnosis; and (5) completed all follow-up measures. Of the 279 men who completed the first assessment, 234 (84%) completed all follow-up assessments. There were no statistically significant differences on any background variables between the participants who had complete data and those who were lost to follow up.
Procedures
Data were collected using structured face-to-face patient interviews and review of medical records. A male interviewer conducted the in-home, first assessment (Time 1) approximately 2 months after treatment. Follow-up assessments were conducted at approximately 4 months (Time 2), 10 months (Time 3), and 16 months (Time 4) after treatment.
Measures
The following measures were administered at all four interviews with the exception of background variables, which were collected only at Time 1.
Background Variables
Demographic and medical data were collected from each participant at Time 1. Cancer pathology and history were verified through medical chart review.
Genitourinary Functioning
The University of California, Los Angeles (UCLA) Prostate Cancer Index (PCI) was used to measure sexual and urinary functioning [29]. The PCI was selected because it is a disease-specific measure developed for and validated in men with prostate cancer [30, 31]. Sample items include, “How would you rate your ability to have an erection?” and “How often have you leaked urine?” Higher scores on the scale indicate better functioning (range 0–100). In the current study, the urinary functioning scale had good reliability at Time 1 (Cronbach’s α = .88) and the sexual functioning scale at Time 1 had adequate reliability (Cronbach’s α = .72).
Depressive Symptoms
A 15-item, modified version of Radloff’s [32] original 20-item Center for Epidemiological Studies Depression Scale (CES-D) was used to measure depressive symptoms. The 15-item CES-D has been validated with cancer patients [33], and it captures almost all of the information of the original 20-item CES-D, but is free of gender bias [34]. Sample items include, “I felt depressed” and “I felt sad.” Higher scores on the scale indicate greater depressive symptoms (range 0–3). A scale score was created by averaging the 15 items. In addition, since the 15-item measure does not have an established clinical cutoff, to estimate the proportion of men who had probable depression a subset of 10 of the 15 items were summed to calculate the clinical cutoff (≥10) according to Andresen and colleagues [35]. In the current study, at Time 1, reliability of this abbreviated 10-item CES-D, which has been validated against the full 20-item CES-D [35], was good (Cronbach’s α = .83). The reliability of the 15-item scale was also good (Cronbach’s α = .87). The 10-item and 15-item measures were highly correlated at Time 1 (r = .97, p < .01). We maintained the 15-item scale for the inferential analyses because it was slightly more reliable than the 10-item scale.
Statistical Methods
Differences in subject characteristics by age group at initial visit were examined using Fisher’s exact tests, chi-square, and Wilcoxon rank sum tests, as appropriate. Generalized estimating equations (GEEs) [36] were used to address primary study hypotheses. GEE is appropriate for longitudinal studies in which individuals are measured at multiple time points and the multiple measures of these individuals are correlated [36]. In all GEE models, four covariates were adjusted for: 1) type of medical treatment (surgery/radiation), 2) received hormonal therapy (yes/no), 3) perform Kegel pelvic floor muscle exercise (yes/no), and 4) experimental condition (intervention/control) from the original clinical trial [28].
To address the hypotheses regarding age-related differences in genitourinary functioning and depressive symptoms, GEE models consisted of age, time, and age by time interaction effects, controlling for the covariates of treatment, hormonal therapy, Kegel, and experimental condition. A significant age group effect indicates a difference in outcome between the two age groups; a significant time effect indicates a marked change in outcome over time; and a significant interaction of age group and time indicates differential rates of change in outcome as a function of age group. Contrasts were estimated within the GEE framework to assess relevant subgroup differences. Separate models were generated for each of the three outcome measures and effects were deemed significant at the 0.05 level. No adjustment was made for multiplicity due to sample size constraints.
To address the hypothesis regarding the association between genitourinary functioning and depressive symptoms by age, GEE models included a three-way age group by functioning by time interaction, controlling for the covariates of treatment, hormonal therapy, Kegel, and experimental condition. Separate models were generated for urinary and sexual functioning.
Results
Sample Characteristics
Of the 234 participants with complete data, most were Caucasian (90%), married and living together, or living with someone in marital-like relationship (86%), and had more than a high school education (63%). The type of treatment most prevalent was radical prostatectomy surgery (57%), followed by radiation therapy (39%) and cryosurgery (4%). Most did not receive hormonal treatments (84%). Tumor stage distribution was: stage 1 (11%), stage 2 (75%), and stage 3 (14%). Less than half (42%) of the participants indicated that they performed Kegel exercises at least once a week or more at Time 1. We used the median age of the sample at Time 1 to divide participants into younger and older age groups (younger: ≤65.5 years vs. older: >65.5 years). The mean ages were of 59.2 (SD 4.84; range 45.0–65.5) for the younger group and 71.1 (SD 3.55, range 65.7–80.3) for the older group. Relative to older men, younger men were more likely to have had their cancer treated by radical prostatectomy than radiation (p < .001), less likely to receive hormone treatments (p < .01), and more likely to perform Kegel exercises (p < .01). Age was unrelated to the intervention condition, but we included it nonetheless as a covariate to be conservative.
Rate and Magnitude of Improvement in Genitourinary Functioning and Mental Health Over Time in Younger Versus Older Men
Estimated marginal means (EMM) and standard errors (SE) for the study variables at all measurement waves as well as the longitudinal analyses are presented in Table 1. Longitudinal analyses, which included the four covariates, revealed that overall, level of sexual functioning was much poorer than level of urinary functioning. Level of genitourinary functioning varied by time and age, with significant improvements seen in sexual functioning (χ 2 = 38.67, p < .001) and urinary functioning (χ 2 = 186.50, p < .001) over time (see Fig. 1). Averaging across time, sexual functioning was significantly poorer in older men (EMM = 14.89, SE = 1.89) than in younger men (EMM = 29.38, SE = 2.61) [χ 2 = 25.78, p < .001]. Contrasts revealed that at each measurement wave, including Time 1, older men had poorer sexual functioning than younger men (all p values < .01) (see Table 1). Longitudinal analysis also revealed a significant two-way interaction of time by age on level of sexual functioning (χ 2 = 16.13, p < .01), indicating that the rate of improvement in sexual functioning varied by age, with younger men improving steadily and significantly at each time wave (from Time 1 to Time 2, p < .05, from Time 2 to Time 3, p < .001, and from Time 3 to Time 4, p < .01), but older men showing no significant improvement at any time wave (see Table 1). Averaging across time, urinary functioning was poorer in older men (EMM = 71.74, SE = 1.97) than in younger men (EMM = 76.01, SE = 2.04) [χ 2 = 3.82, p = .05]. Initially, older and younger men did not differ in their level of urinary functioning, but older men had poorer urinary functioning by Time 3 (p < .05) and Time 4 (p < .01). There was not a significant two-way interaction of time by age on level of urinary functioning.
With respect to depressive symptoms, overall, 17.5% reported symptoms above the clinical cutoff score (≥10) at Time 1, with no significant difference in rates of probable depression between older and younger men. The longitudinal analysis revealed a significant effect of time (χ 2 = 16.62, p < .01): the mean level of depressive symptoms dropped significantly from Time 1 to Time 2 (p < .001) (see Fig. 2). Despite the lower level of genitourinary functioning among older men, there were no significant overall age differences in depressive symptoms. However, contrast analyses revealed that level of depressive symptoms in younger men declined significantly from Time 1 to Time 2 (p < .01), whereas there was no significant decline in older men from Time 1 levels (see Table 1).
Examining Age as Moderating the Relation Between Genitourinary Functioning and Mental Health
We used data on participants’ genitourinary functioning at Time 1 to identify high- and low- sexual functioning and urinary functioning groups. For sexual functioning, the median cut-point was 9.38. The mean in the low sexual functioning group at Time 1 was 2.58 (SD 3.39; range .00–9.38) and in the high sexual functioning group was 35.84 (SD 24.29; range 9.39–100.00). For the urinary functioning, the median cut-point was 63.40. The mean in the low urinary functioning group was 35.45 (SD 17.02, range .00–63.40) and in the high urinary functioning group was 83.90 (SD 12.63, range 63.41–100.00).
The longitudinal analysis of age by sexual functioning by time on depressive symptoms revealed no significant main effects of age or sexual functioning, but there was a significant effect of time (χ 2 = 15.11, p < .01). The mean level of depressive symptoms dropped significantly from Time 1 (EMM = .55, SE = .04) to Time 2 (EMM = .47, SE = .04; p < .01) and then remained fairly steady (Time 3 EMM = .45, SE = .05; Time 4 EMM = .45, SE = .04). There also was a significant two-way interaction of age by sexual functioning on level of depressive symptoms (χ 2 = 5.25; p < .05). As shown in Fig. 3, younger men with low sexual functioning had a higher level of depressive symptoms than older men with low sexual functioning (p < .05) and a higher level of depressive symptoms than younger men with high sexual functioning (p < .05). The three-way interaction of age by sexual functioning by time on depressive symptoms was not significant.
Estimated marginal mean level of depressive symptoms as measured by the Center for Epidemiological Studies Depression Scale (CES-D) averaged across time by age and level of sexual functioning at time 1 (n = 234). Notes: Time 1 corresponds to approximately 2 months after treatment. Low and high sexual functioning was determined using the median cut-point of 9.38 on the sexual functioning scale: scores ranged from 0.00 to 9.38 (mean = 2.58) for men in the low sexual functioning group and from 9.39 to 100.00 (mean = 35.84) for men in the high sexual functioning group. Ages of younger men ranged from 45.0 to 65.5 (mean = 59.2 years) and of older men ranged from 65.7 to 80.3 (mean = 71.1 years)
The longitudinal analysis of age by urinary functioning by time on depressive symptoms revealed a significant main effect of urinary functioning (χ 2 = 9.47, p < .01) and time (χ 2 = 17.64, p < .01), but no main effect of age. The mean level of depressive symptoms dropped significantly from Time 1 (EMM = .55, SE = .04) to Time 2 (EMM = .47, SE = .04) (p < .001) and then remained fairly steady (Time 3 EMM = .45, SE = .05; Time 4 EMM = .45, SE = .04). Averaged across time, level of depressive symptoms was higher among men with a low level of urinary functioning (EMM = .57, SE = .05) than among men with a relatively high level of urinary functioning (EMM = .39, SE = .04) (p < .01). However, the two-way interaction of age by urinary functioning on depressive symptoms was not significant, nor was the three-way interaction of age by urinary functioning by time on depressive symptoms.
Discussion
In general, relative to urinary functioning, sexual functioning was more impaired, took longer to improve, and did not improve very much over time. Depressive symptoms were relatively low, although 17.5% of the men had probable depression at Time 1. This rate is within the range reported in other studies in men treated for prostate cancer [37]. There were no age-related differences in overall level of depressive symptoms; however, whereas younger men reported significant improvements at the first (4 month) follow-up wave, older men did not report significant improvements at any follow-up wave. Overall, older men had significantly lower levels of sexual functioning. In terms of urinary functioning, older and younger men initially had comparable levels of difficulties and both showed marked improvements from Time 1 to 4-month follow-up. However, by 10- and 16-month follow-ups the younger men improved more and had significantly fewer urinary problems than the older men at these time points. The relation of age to sexual functioning was most dramatic. Older men started out 7.85 points lower in sexual functioning than younger men and this gap more than doubled to a 20.26 point difference by the 16-month follow-up, owing to the slower and smaller increments in improvements in older compared to younger men. Finally, level of urinary dysfunction was positively associated with greater depressive symptoms in older and younger men, but level of sexual dysfunction was associated with depressive symptoms only among younger men.
The observation that genitourinary functioning and depressive symptoms can improve over time posttreatment is consistent with prior research [5, 38], as is the finding that in the long run problems in sexual functioning are more prevalent than problems in urinary functioning [39]. The present study further showed that the rate and magnitude of improvements in genitourinary functioning and depressive symptoms are related to age. Urinary functioning was moderately impaired in both age groups shortly after treatment but improved steadily over time. However, the younger age group had higher levels of urinary functioning by the long-term follow-ups. It is possible that improvements in urinary functioning peaked sooner in older men because older men tend to experience some degree of urinary problems even in the absence of prostate cancer [40]. With respect to sexual functioning younger men showed significant improvements approximately 4 months after treatment whereas older men did not show any significant improvements even by 16 months after treatment. This age advantage in improvements in sexual functioning has been observed in other studies [41].
As expected, poorer sexual functioning was more strongly related to distress in younger than in older men. This finding is particularly striking given the overall better sexual functioning and faster rate of improvement in sexual functioning among younger men. One explanation of this finding is that older men are likely to have had a higher level of sexual problems prior to their prostate cancer treatments and may have become accustomed to those problems. Bacon et al. [42] found that the prevalence of sexual dysfunction strongly increased with age, regardless of health status, with a clear, linear, age-related decline in overall ability to function sexually, sexual desire, orgasm, and quality of erections. In addition younger men tend to have greater sexual desire than older men [43], possibly due to less age-related hormonal alterations [44], and this greater desire might exacerbate distress caused by sexual dysfunction. Indeed, Dahn and colleagues [45] found that in men with sexual dysfunction, sexual desire was inversely related to quality of life. Also, younger men may have had more frequent sexual activity prior to treatment and therefore place a higher value on sexual functioning. Sommers and colleagues [46] found that men who engaged in more frequent sexual activity reported significantly lower utilities for living with dysfunction than did men who had sex infrequently.
The psychological theory that older persons cope better with life stresses and illnesses [25], or have more adaptive attitudes than younger persons [26], is not likely to account for the findings in this study. If it were true that older persons are more resilient because of their coping strategies and resources, or their psychological attitudes, then we would have found age-related differences in response to urinary dysfunction, which we did not. Urinary dysfunction was positively associated with depressive symptoms in both age groups. In addition, there were no major age-related differences in overall level of depressive symptoms.
The present findings may have implications for clinical care and interventions for men treated for localized prostate cancer. Clinicians can help prepare patients for what to realistically expect in terms of rate and amount of improvements in genitourinary functioning. Providing information on the general age-related trends of changes in genitourinary functioning over time may help to reduce uncertainty in some patients and in turn, improve quality of life [47]. These findings can also assist clinicians to better identify patients who may be at higher risk of dysfunction and then provide information on interventions designed to improve functioning. Interventions that address sexual functioning may be most helpful to younger men, especially since younger men treated for prostate cancer are likely to have more unmet sexuality-related needs than older men [48–50]. With time, urinary functioning improves dramatically in most men. A variety of effective rehabilitation techniques are available to potentially accelerate patients' urinary control, including Kegel exercises, biofeedback, and electrical stimulation [51, 52]. Approaches to sexual rehabilitation have been more varied and intensively studied.
A recent review by Latini and colleagues [53] showed that educational and psychosocial interventions provided to patients or couples coping with prostate cancer can significantly improve sexual functioning and sexual satisfaction, as well as reduce bother associated with sexual dysfunction. They also note that some men may benefit more or less from sexual rehabilitation interventions than others. For example, younger men or those who have high desire combined with low sexual functioning may be especially receptive to and likely to benefit from sexual rehabilitation interventions. Targeting these high-risk groups may increase the effectiveness of interventions and reduce costs. In contrast, men who are on androgen ablation therapy may not benefit from education and counseling alone because of the adverse effects of the therapy on sexual desire and functioning [54]. Such men might need additional pharmacological or medical interventions, such as using a vacuum device, phosphodiesterase type 5 inhibitors (sildenafil, tadalafil, vardenafil), or penile prostheses. The efficacy of any of these treatments appears to be affected by a wide range of patient, sexual partner, and treatment factors, indicating that a patient-centered approach and shared decision making will be most effective for managing sexual dysfunction and promoting sexual health and satisfaction in men treated for prostate cancer [55].
Some limitations of the study should be noted including the inadequate representation of men from minority groups and lower socio-economic status. Thus, results may not hold true in a more diverse population of men treated for localized prostate cancer. In addition, this study only included men with localized disease; therefore, results cannot be generalized to men with advanced disease. Finally, the lack of pretreatment measures of genitourinary functioning limited our ability to assess the full impact of treatments on men’s functioning.
Our study suggests that although older men do not recover as much or as steadily in genitourinary functioning as younger men, they do not appear to have higher depressive symptoms than younger men. Low levels of urinary functioning appear to affect men’s level of depressive symptoms regardless of age; however, low levels of sexual functioning appears to be more distressing to younger men. Therefore, when designing or ecommending existing interventions aimed at improving depressive symptoms in men with prostate cancer, particular emphasis should be placed on targeting men with low urinary functioning and younger men with low sexual functioning. Younger prostate cancer patients may be more interested in posttreatment education and counseling about methods of addressing sexual dysfunction associated with prostate cancer treatments. They also may have a greater need than older men for pretreatment counseling about the effects of various prostate cancer treatments on sexual functioning, which they might consider in making an informed decision about treatments.
References
Jemal A, Siegel R, Ward E, et al. Cancer statistics. CA Cancer J Clin. 2008;58:71-96.
Draisma G, Boer R, Otto SJ, et al. Lead times and overdetection due to prostate-specific antigen screening: Estimates from the European randomized study of screening for prostate cancer. J Natl Cancer Inst. 2003;95:868-78.
Michaelson MD, Cotter SE, Gargollo PC, Zietman AL, Dahl DM, Smith MR. Management of complications of prostate cancer treatment. CA Cancer J Clin. 2008;58:196-213.
Blank TO, Bellizzi KM. A gerontologic perspective on cancer and aging. Cancer. 2008;112:2569-76.
Stanford JL, Feng Z, Hamilton AS, et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: The prostate cancer outcomes study. JAMA. 2000;283:354-60.
Bisson JI, Chubb HL, Bennett S, Mason M, Jones D, Kynaston H. The prevalence and predictors of psychological distress in patients with early localized prostate cancer. BJU Int. 2002;90:56-61.
Diefenbach M, Mohamed NE, Horwitz E, Pollack A. Longitudinal associations among quality of life and its predictors in patients treated for prostate cancer: The moderating role of age. Psychol Health Med. 2008;13:146-61.
Eton DT, Lepore SJ. Prostate cancer and health-related quality of life: A review of the literature. Psychooncology. 2002;11:307-26.
Penson DF, Litwin MS, Aaronson NK. Health related quality of life in men with prostate cancer. J Urol. 2003;169:1653-61.
Lubeck DP, Litwin MS, Henning JM, Stoddard ML, Flanders SC, Carroll PR. Changes in health-related quality of life in the first year after treatment for prostate cancer: results from CaPSURE. Urology. 1999;53:180-6.
Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118:622-9.
Fowler FJ Jr, Barry MJ, Lu-Yao G, Wasson J, Roman A, Wennberg J. Effect of radical prostatectomy for prostate cancer on patient quality of life: Results from a medicare survey. Urology. 1995;45:1007-13.
Perczek RE, Burke MA, Carver CS, Krongrad A, Terris MK. Facing a prostate cancer diagnosis: Who is at risk for increased distress? Cancer. 2002;94:2923-9.
Lepore SJ, Eton DT. Response shifts in prostate cancer patients: An evaluation of suppressor and buffer models. In: Schwartz CE, Sprangers M, eds. Adaptation to changing health: Response shift in quality-of-life research. Washington: American Psychological Association; 2001:37-51.
Helgeson VS, Lepore SJ. Quality of life following prostate cancer: The role of agency and unmitigated agency. J Appl Soc Psychol. 2004;34:2559-2585.
Bacon CG, Giovannucci E, Testa M, Glass TA, Kawachi I. The association of treatment-related symptoms with quality-of-life outcomes for localized prostate carcinoma patients. Cancer. 2002;94:862-71.
Fan A. Psychological and psychosocial effects of prostate cancer. Nurs Stand. 2002;17:33-7.
Moore KN, Estey A. The early post-operative concerns of men after radical prostatectomy. J Adv Nurs. 1999;29:1121-9.
Greimel ER, Padilla GV, Grant MM. Physical and psychosocial outcomes in cancer patients: A comparison of different age groups. Br J Cancer. 1997;76:251-5.
Hewitt M, Rowland JH, Yancik R. Cancer survivors in the United States: Age, health, and disability. J Gerontol A Biol Sci Med Sci. 2003;58:82-91.
Garman KS, Pieper CF, Seo P, Cohen HJ. Function in elderly cancer survivors depends on comorbidities. J Gerontol A Biol Sci Med Sci. 2003;58:M1119-24.
Mor V, Allen S, Malin M. The psychosocial impact of cancer on older versus younger patients and their families. Cancer. 1994;74:2118-27.
Kornblith AB, Powell M, Regan MM, et al. Long-term psychosocial adjustment of older vs younger survivors of breast and endometrial cancer. Psychooncology. 2007;16:895-903.
Schroevers MJ, Ranchor AV, Sanderman R. The role of age at the onset of cancer in relation to survivors’ long-term adjustment: A controlled comparison over an eight-year period. Psychooncology. 2004;13:740-52.
Williamson GM, Shaffer DR. Age and physical functioning. In: Psychology, health and medicine. 2nd ed. Cambridge: Cambridge University; 2007. p. 10–4
Williamson GM, Dooley WK. Aging well: Outlook for the 21st century. In: Snyder CR, Lopez SJ, eds. Coping with stress: Effective people and processes. New York: Oxford University; 2001:240-58.
Prohaska TR, Keller ML, Leventhal EA, Leventhal H. Impact of symptoms and aging attribution on emotions and coping. Health Psychol. 1987;6:495-514.
Lepore SJ, Helgeson VS, Eton DT, Schulz R. Improving quality of life in men with prostate cancer: A randomized controlled trial of group education interventions. Health Psychol. 2003;22:443-52.
Litwin MS, Hays RD, Fink A, et al. Quality-of-life outcomes in men treated for localized prostate cancer. JAMA. 1995;273:129-35.
Litwin MS, Hays RD, Fink A, Ganz PA, Leake B, Brook RH. The UCLA prostate cancer index: Development, reliability, and validity of a health-related quality of life measure. Med Care. 1998;36:1002-12.
Lubeck DP, Litwin MS, Henning JM, Carroll PR. Measurement of health-related quality of life in men with prostate cancer: The CaPSURE database. Qual Life Res. 1997;6:385-92.
Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385-401.
Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: Evaluation of the center for epidemiological studies depression scale (CES-D). J Psychosom Res. 1999;46:437-43.
Stommel M, Given BA, Given CW, Kalaian HA, Schulz R, McCorkle R. Gender bias in the measurement properties of the center for epidemiologic studies depression scale (CES-D). Psychiatry Res. 1993;49:239-50.
Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D (center for epidemiologic studies depression scale). Am J Prev Med. 1994;10:77-84.
Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121-30.
Bennett G, Badger TA. Depression in men with prostate cancer. Oncol Nurs Forum. 2005;32:545-56.
Korfage IJ, Essink-Bot ML, Janssens AC, Schroder FH, de Koning HJ. Anxiety and depression after prostate cancer diagnosis and treatment: 5-year follow-up. Br J Cancer. 2006;94:1093-8.
Potosky AL, Davis WW, Hoffman RM, et al. Five-year outcomes after prostatectomy or radiotherapy for prostate cancer: The prostate cancer outcomes study. J Natl Cancer Inst. 2004;96:1358-67.
Litwin MS. Health related quality of life in older men without prostate cancer. J Urol. 1999;161:1180-4.
Kamath C, Dueck A. Incorporating clinical significance into a study. Curr Probl Cancer. 2005;29:306-16.
Bacon CG, Mittleman MA, Kawachi I, Giovannucci E, Glasser DB, Rimm EB. Sexual function in men older than 50 years of age: Results from the health professionals follow-up study. Ann Intern Med. 2003;139:161-8.
Martin CE. Sexual activity in the aging male. In: Money J, Musaph N, eds. Handbook of sexology. New York: Elsevier-North Holland; 1977:813-824.
Mitchell HS. Testosterone, sexuality, and erectile function in aging men. J Androl. 2003;24:S42-5.
Dahn JR, Penedo FJ, Gonzalez JS, et al. Sexual functioning and quality of life after prostate cancer treatment: Considering sexual desire. Urology. 2004;63:273-7.
Sommers BD, Beard CJ, D'Amico AV, Kaplan I, Richie JP, Zeckhauser RJ. Predictors of patient preferences and treatment choices for localized prostate cancer. Cancer. 2008;113:2058-67.
Shaha M, Cox CL, Talman K, Kelly D. Uncertainty in breast, prostate, and colorectal cancer: Implications for supportive care. J Nurs Scholarsh. 2008;40:60-7.
Ream E, Quennell A, Fincham L, et al. Supportive care needs of men living with prostate cancer in England: A survey. Br J Cancer. 2008;98:1903-9.
Smith DP, Supramaniam R, King MT, Ward J, Berry M, Armstrong BK. Age, health, and education determine supportive care needs of men younger than 70 years with prostate cancer. J Clin Oncol. 2007;25:2560-6.
Steginga SK, Occhipinti S, Dunn J, Gardiner RA, Heathcote P, Yaxley J. The supportive care needs of men with prostate cancer (2000). Psychooncology. 2001;10:66-75.
MacDonald R, Fink HA, Huckabay C, Monga M, Wilt TJ. Pelvic floor muscle training to improve urinary incontinence after radical prostatectomy: A systematic review of effectiveness. BJU Int. 2007;100:76-81.
Matthewson-Chapman M. Pelvic muscle exercise/biofeedback for urinary incontinence after prostatectomy: An education program. J Cancer Educ. 1997;12:218-223.
Latini DM, Hart SL, Coon DW, Knight SJ. Sexual rehabilitation after localized prostate cancer: Current interventions and future directions. Cancer J. 2009;15:34-40.
Schover LR. Sexual rehabilitation after treatment for prostate cancer. Cancer. 1993;71:1024-30.
Hatzimouratidis K, Hatzichristou DG. A comparative review of the options for treatment of erectile dysfunction: Which treatment for which patient? Drugs. 2005;65:1621-50.
Acknowledgement
This work was supported by the National Institutes of Health Grant CA68354. We are grateful to the clinicians and patients who participated in this study, the research staff and consultants, and Thomas Blank for his comments on an earlier draft.
Conflict of Interest
None
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Roberts, K.J., Lepore, S.J., Hanlon, A.L. et al. Genitourinary Functioning and Depressive Symptoms Over Time In Younger Versus Older Men Treated for Prostate Cancer. ann. behav. med. 40, 275–283 (2010). https://doi.org/10.1007/s12160-010-9214-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-010-9214-4