Abstract
Background
Individuals with a sibling who has had colorectal cancer diagnosed before age 61 are at increased risk for colorectal cancer and may derive particular benefit from screening. Tailored interventions may increase participation in appropriate colorectal cancer screening.
Purpose
This study evaluated the efficacy of two tailored interventions and a generic print intervention.
Methods
Participant siblings (N = 412) who were not up-to-date with colorectal cancer screening were randomly assigned to receive either a generic print pamphlet, a tailored print pamphlet, or a tailored print pamphlet and tailored counseling call. Colorectal cancer screening 6 months after the baseline interview was the outcome measure.
Results
Results indicated that colorectal cancer screening adherence increased among intermediate risk siblings enrolled in all three intervention groups. Participants in both tailored intervention groups reported having colorectal cancer screening at significantly higher rates than participants in the generic print group. The increase in colorectal cancer screening in the tailored print and counseling call group was not significantly higher than that achieved by the tailored print alone. Decisional balance partially mediated treatment effects. Tailored behavioral interventions are effective methods for increasing screening adherence but telephone counseling did not add significantly to treatment effects.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the fourth most commonly diagnosed cancer and the second leading cause of cancer deaths in the United States [1]. Lifetime risk for CRC is approximately 5% after age 50. Individuals with a first-degree relative (FDR; sibling, parent, child) diagnosed with CRC have an estimated lifetime CRC risk of 10% [2–4]. The risk increases as the age of the proband at diagnosis decreases [5, 6] with estimates ranging between two and four times the average risk [3, 5].
Screening results in earlier detection of CRC and reduces disease-specific mortality [7, 8]. Various agencies have published screening guidelines for relatives of CRC patients. A number of professional organizations recommend that FDRs should follow population screening guidelines but begin CRC screening (CRCS) at a younger age than general guidelines with recommended screening starting at age 40 [9]. Others specifically recommend colonoscopy starting at an age that depends on the family history [1]. Estimates of CRCS among family members at increased risk for CRC have varied widely with reported rates of 22% [10], 39% [11], 55% [12], 64% [13], and 79% [14], depending upon the screening procedure examined and the targeted at-risk population.
Given the increased risk for CRC among FDRs of individuals diagnosed with CRC and the relatively low participation in this at-risk population, effective methods of increasing CRCS participation are needed. Unfortunately, the few behavioral interventions targeting this at-risk population have shown limited impact on screening adherence. Glanz and colleagues [15] evaluated the impact of an individual face-to-face health counseling intervention that was accompanied by tailored print material and two follow-up phone calls compared with a general health counseling intervention among FDRs of CRC patients. Results indicated that the counseling intervention increased screening significantly among non-adherent participants compared with the general health counseling. Rawl and colleagues [16] compared the efficacy of a tailored print intervention versus a non-tailored print intervention on CRCS among FDRs of CRC patients. While both interventions resulted in increased CRCS, CRCS rates did not differ between the study groups nor were there differences in forward progression in stage of adoption of CRCS.
The primary aim of this study was to evaluate the effect of three increasingly intense behavioral interventions on CRCS adherence among FDRs of individuals diagnosed with CRC before the age of 61 years who were not on-schedule with regard to CRCS. We compared a generic print intervention (GP), a tailored print intervention (TP), and a tailored print and telephone counseling intervention (TP + TC). We hypothesized that the greatest CRCS would be among individuals participating in the TP + TC intervention followed by individuals enrolled in the TP intervention. The lowest CRCS adherence was predicted in the GP intervention because it would lead to messages that were not perceived as directly relevant to the individual. In contrast, by tailoring materials superfluous information would be eliminated. The remaining tailored information would be considered more personally relevant and receive greater attention and, thus, would be more likely to have an effect [17]. A recent meta-analysis of tailored interventions indicated that tailored messages are more effective in triggering behavioral change than generic messages [18] and recent work has suggested that tailored messages result in significant effects on CRCS among average risk individuals [19].
Because tailoring is not in itself a theoretical or conceptual framework, we drew on established health behavior theories as well as the constructs shown to be associated with screening adherence for guidance concerning which variables to use as the basis for developing tailored messages. In our prior work [12], we integrated constructs from three conceptual models: the Health Belief Model (HBM) [20–22], the Transtheoretical Model (TTM; [23, 24]), and the Dual Process Theory [25, 26]. The models are largely complementary and there is considerable overlap among them. For the present study, tailoring for both the print and telephone counseling was based upon the following constructs from these models that we found to be associated with CRCS adherence and intention in the targeted population in our previous work [12]: pros of CRCS, cons of CRCS, processes of change (i.e., commitment to CRCS), stage of adoption, perceived CRC preventability, perceived CRC risk, physician and family support for CRCS, the closeness of the relationship with the affected sibling, medical insurance status, and knowledge of CRC and CRCS.
The secondary aim was to evaluate possible moderators and mediators for intervention effects. Behavioral interventions may not be beneficial for all participants and thus it is important to identify subgroups of persons who are particularly amenable or resistant to the effect of each intervention. Ultimately, this will provide more effective and possibly cost-effective interventions for those who will benefit most. Intervention moderators were selected based upon factors predictive of response to other cancer screening interventions such as mammography [27–28]. Moderators evaluated included previous CRCS history, the number of family members with CRC, whether the participant had received a physician recommendation for CRCS at the baseline interview, baseline screening intention, and the closeness of the participant’s relationship to the affected sibling.
Although accumulating evidence indicates that CRCS interventions show efficacy in improving CRCS adherence, little is known about why these interventions work; that is, we have not identified the mediators of intervention effects. An understanding of why these interventions work will guide the development of more effective screening interventions as well as provide support for theories guiding these interventions. We selected potential mechanisms of change based upon HBM, TPB, and Dual Process Theory constructs that were targeted in the tailored interventions. Mediators evaluated included CRC knowledge, CRCS knowledge, physician support for CRCS, family support for CRCS, perceived CRC risk, perceived CRC severity, perceived CRC preventability, four processes of change, decisional balance, and personalization of the print materials.
In the present study, we targeted siblings of individuals diagnosed with CRC prior to the age of 61 years for intervention rather than patients’ children or parents. The age range of children would likely be too young to meet screening guidelines and the parents of these individuals may no longer be alive.
Method
Sample Recruitment and Randomization
Participants were siblings of patients recruited from the oncology, gastroenterology, and surgical practices at 26 participating medical centers located across the USA (sites contributed 1–93 participants). Prospective patients were identified from tumor registries or medical records. IRB approval was received for each site. Physicians of record for each patient name identified gave permission for their patients to be contacted. Sample recruitment began in December 2003 and ended in July 2007. Follow-up assessments were completed in January 2008.
Eligibility criteria for patients whose siblings were the focus of this study included: (1) patient was diagnosed with colon or rectal cancer since 1997, (2) patient currently living, (3) patient age was less than 61 years at diagnosis, (4) patient had no history of hereditary cancer syndrome (e.g., Familial Adenomatous Polyposis Syndrome, Hereditary Nonpolyposis Colorectal Cancer), (5) patient had no history of Inflammatory Bowel Disease (ulcerative colitis or Crohn’s disease), and (6) patient was able to comprehend English. Patients who met these criteria were mailed a letter describing the study and subsequently contacted by telephone to determine eligibility. At this time, patients gave permission to contact all biological siblings and permission for medical information to be obtained from their medical chart. Next, identified siblings were mailed a letter describing the study. They were contacted by telephone and eligibility was determined. After written informed consent and HIPAA acknowledgement (which was required after April, 2003), a telephone interview was conducted. During the telephone interview, data for the present study were obtained. Eligibility criteria for siblings were: (1) sibling age was greater than or equal to 35 years or less than 10 years younger than the age at which the patient was diagnosed (if the proband’s diagnosis was made at an age less than 50 years); (2) sibling was a full biological sibling (no half-siblings); (3) sibling was not on-schedule with regard to CRCS defined as: had not had a colonoscopy in the past 5 years or had not had a flexible sigmoidoscopy (FS) in the past 5 years and had not had annual fecal occult blood testing (FOBT); screening is recommended for a person of this age (e.g., if the proband was diagnosed at age 40, the sibling had CRCS if s/he was 30 years or more at the time of the proband’s diagnosis); (4) sibling had no history of cancer with the exception of non-melanoma skin cancer or childhood cancer diagnosed under the age of 2 years; (5) sibling had no family history of hereditary cancer syndromes; (6) sibling had no history of inflammatory bowel disease; (7) sibling was able to give meaningful informed consent; and (8) sibling was English-speaking.
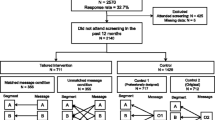
The flow diagram of progress through the study is shown in Fig. 1. The main reasons for patient ineligibility were that the patient was no longer alive (34.5% of ineligible), the patient had no siblings (34.5%), and the patient did not meet medical history criteria (IBD, hereditary cancer syndrome) (11.4%). The main reasons for sibling ineligibility were that the sibling was compliant with CRCS guidelines (93% of ineligible siblings) and the sibling did not meet medical history criteria (did not meet age at diagnosis criteria or diagnosis criteria, personal cancer history, IBD, hereditary cancer syndrome) (3%).
A comparison between the 769 siblings who refused the study with the 412 sibling participants on available demographic information indicated that refusers were more likely to be male than participants (χ 2(1, 1,187) = 30.7, p < .001; percent maleparticipant sample = 42.2%; percent malerefuser sample = 57.8%). Participants were also significantly younger than refusers (t (1,186) = 3.4, p < .01; M participants = 47.9, SD = 9.0, M refusers = 51.0, SD = 9.1).
Participants completed the baseline survey by telephone. After that time, participants were randomized to study condition. Randomization was done by family. All participants received intervention materials (see below). Six months after the baseline survey, participants were contacted by telephone to complete the 6-month follow-up survey. Participants were given $15 gift certificates for each assessment completed.
Interventions
Generic Print Intervention
Participants were mailed a cover letter and the generic pamphlet. The letter contained a reference to the pamphlet, asked the participant to read the pamphlet, and reminded the participant that the best way to prevent CRC is by having screening. The Centers for Disease Control and Prevention pamphlet, “Colorectal Cancer Screening Saves Lives” [29], was the generic educational print material. The pamphlet reviewed the basic screening tests, presented the screening guidelines for average and increased risk individuals, and presented basic information about CRC. The information was not developed specifically for at-risk populations. The pamphlet was mailed within 1 week of the baseline survey completion.
Tailored Print Intervention
Participants were mailed a personalized cover letter and the tailored booklet. The letter contained a statement that the pamphlet was prepared specifically for the participant, asked the participant to read the pamphlet, and reminded the participant that the best way to prevent CRC is by having screening. The tailored booklet had four pages and four pictures. The first page was a cover page which was entitled, “The Good News: Colorectal Cancer is Preventable!” The introductory section outlined the contents of the booklet and informed the participant that the pamphlet was tailored specifically to their survey. A picture of a gender- and ethnicity-matched individual had a caption discussing the participant’s highest ranking barrier. The remaining three pages were tailored to participants’ marital status, gender, ethnicity, incorrect CRC knowledge, incorrect colonoscopy knowledge, CRC risk, low-rated benefits (with alternative views of benefits), highly rated barriers (with alternative views of barriers), the level of family support for CRCS, stage of adoption, closeness with the affected sibling, and commitment to screening.
One month after the participants received the tailored print they received a one page tailored follow-up newsletter. The newsletter reviewed the participants’ stage of adoption, reinforced facts and alternative views of barriers, and contained a picture of a colorectal cancer survivor who discussed the importance of screening.
Tailored Print and Telephone Counseling
Participants were mailed a personalized letter and TP using the same procedures as described above. The telephone counseling session was scheduled at least 1 week after the TP was mailed. The counselor utilized a motivational interviewing style [30]. Motivation and readiness to have CRCS was assessed by asking the participant to rate the perceived importance of having CRCS and perceived confidence of having CRCS and to provide a rationale for each rating. Benefits of having CRCS and not having CRCS, ways of obtaining greater support for CRCS from family and friends, correcting factual information about CRC and colonoscopy, and recommended screening guidelines were reviewed. Perceptions of how the family history affected personal risk on the decision to have CRCS were discussed. The interventionist used open questions to facilitate discussion. The session was guided by a script (available from the first author).
One month after the participants received the tailored print they were mailed a one page tailored follow-up newsletter. The newsletter reviewed the participants’ stage of adoption, reinforced facts about CRC, and presented alternative views of barriers. A picture of the health educator who conducted the session was included with a quote summarizing the call and recommending screening.
TC Training, Supervision, and Fidelity
Three health educators conducted the counseling sessions. All were trained in the intervention by a review of the manual and practice TC sessions that were reviewed by an expert in MI. Ongoing supervision was also provided by the MI expert which consisted of reviewing audiotapes, discussion of alternative strategies, and providing feedback. Treatment fidelity was scored by three treatment fidelity coders using a rating system designed specifically for this study. The rating system contained 27 fidelity criteria (e.g., “How motivated is the participant to have screening?”) rated by whether or not the topic was covered. Fidelity coder training consisted of a review of the health education script and fidelity criteria followed by practice ratings with the project manager and first author. Once raters achieved an 80% inter-rater reliability with the criterion coder, they were permitted to code tapes. A fidelity score consisted of the percentage of topics completed divided by the total number of fidelity criteria. Fifty-two of the 98 sessions were audible and able to be coded. Treatment fidelity was 80%.
Outcome Measure: Screening Status at Follow-up
Participants were asked whether they had a CRCS test since the baseline survey, what the screening test was, and the date of the screening test. Because some follow-up assessments were conducted after the 6-month time frame, a cut off of 8 months post-baseline was selected to calculate screening status. The variable was defined as either had appropriate screening (had a colonoscopy or had a FS and an FOBT) or did not have appropriate screening. Because no participants had both a FS and an FOBT, screening compliance reflected colonoscopy status at 8 months and therefore will be labeled colonoscopy screening.
Participants who reported a screening test at the follow-up were asked for the name and contact information of the physician who performed the test. Of the 88 colonoscopy procedures reported at follow-up, 77 were confirmed by the participant’s physician, nine could not be confirmed as physician information provided by the participant was not correct, and two were not confirmed thus comprising an 87.5% confirmation rate. Of the two FS reported at follow-up both were confirmed. Of the 34 FOBTs reported, 16 were confirmed, six were denied by the physician, and 12 could not be confirmed as the physician information was not correct or the physician’s office did not respond to requests for confirmation comprising a 47% confirmation rate. All analyses were conducted on self-report screening data.
If screening status was not collected at follow-up, the participant was considered non-compliant for the intent to treat (ITT) analyses.
Covariates
Participant gender, marital status (married or not), ethnicity (Caucasian or not), current employment (full time, part time, unemployed, retired), age, income, education, medical insurance status (yes/no), and the number of siblings in the family were evaluated as possible covariates. In addition, the gender of the affected sibling, the cancer stage at diagnosis, the affected sibling’s age at the time of diagnosis, and time elapsed since diagnosis were evaluated.
Mediators (Baseline and Follow-up)
Participants completed measures of CRC knowledge (seven items), procedural knowledge (35 items), physician support for CRCS (three items), family support for CRCS (two items), perceived CRC risk (four items), perceived CRC severity (five items), perceived CRC preventability (two items), decisional balance (28 items; calculated as the mean of the ten pros of screening items minus the mean of the 18 cons of screening items), processes of change (commitment to CRCS, nine items; information sharing, seven items; thinking beyond oneself, eight items; and avoidance of the health care system, four items), and personalization of the print materials (two items). Further details about the scales are available from the authors.
Moderators
At baseline, participants completed a cancer family history form, indicated whether their physician had recommended CRCS (yes/no), and answered questions about their prior CRCS history, closeness with the affected sibling [31] (five items, α = 0.93), and CRCS intentions (four items, α = 0.89).
Evaluation of Intervention Materials
Participants completed a ten-item evaluation of the telephone counseling session. The recall variable assessed whether participants remembered receiving the telephone call from the counselor. The ten evaluation questions were modeled after those used in prior research [32, 33]. Items assessed the extent to which the session provided information that was interesting, new, comprehensible, valid, prepared with them in mind, made it easier to think about getting screening, and addressed reasons they may have had for not getting screening. Internal consistency was good (α = 0.86). Ten items evaluated the print materials. Participants reported whether they remembered receiving the print materials (yes/no), whether they were comprehensible, valid, made it easier for them to think about getting screening, addressed reasons they may have had for not getting screening, and whether they saved the material (yes/no), showed it to others (yes/no), or discussed it with their physician (yes/no).
Results
Sample Characteristics
Participant characteristics are shown in Table 1. Three hundred twelve patients (and therefore 312 families) provided siblings for this study. Among the 312 patients, 58% were diagnosed with colon cancer and 42% were diagnosed with rectal cancer. Approximately half (53%) were diagnosed with advanced disease. The average time since the initial cancer diagnosis was 2.1 years (SD = 1.6 years, range = within the past year–8 years ago).
Process Evaluation
The majority of participants remembered receiving a pamphlet in the mail (92%). Similarly, the majority of participants reported reading (85%) and saving the pamphlet (85%). Approximately half of the sample showed the pamphlet to others (57%) but only a subset (15%) reported discussing it with their physician. There were no differences across study groups in any of these outcomes. On average, the print materials were evaluated positively (M = 5.6, SD = 0.95) and there were no significant differences in the print evaluation (other than personalization which is reported in the next section) across study groups.
Among the 98 participants who received the TC session, the mean call length was 19 min (range 4–75 min, median = 18 min). Seventy-two participants completed the follow-up counseling evaluation survey (73.4%). Sixty-three of these individuals (88%) reported that they remembered receiving the call. On average, the sessions were evaluated positively (M = 5.6, SD = 0.8). The highest rating regarded the helpfulness of the session (M = 5.8, SD = 1.1). Participants felt the length of the call was acceptable (M = 4.4; SD = .99, 4 = “just right”, 7 = “much too long”). A relatively low average rating was noted for the item, “I feel the telephone health educator addressed reasons that I may have had for not getting screened” (M = 5.0, SD = 1.9).
Intervention Effects
Overview of Statistical Approach to Analysis
Colonoscopy at follow-up was the primary outcome measure. An intent to treat analysis was conducted on these data. Because the sample included some individuals from the same family (a nested data structure), the assumption of statistical independence of the observations was not necessarily tenable. To accommodate this possibility, a generalized estimating equations (GEE) analysis was undertaken using the Generalized Linear Model approach implemented in the SAS procedure GENMOD. Since the outcome was binary, a logit link function was employed using the binomial distribution and an exchangeable error structure. Moderator analyses were conducted using the procedures just described and each moderator was crossed with the treatment condition in an ITT analysis. Mediation analyses were undertaken following Baron and Kenny’s [34] approach as modified by Kenny et al. [35]. Since decisional balance was a continuous variable, prior to undertaking the mediation analyses described below, a mixed linear model was used to determine if it was necessary to account for the nested data structure noted above. An unconditional means model implemented in the SAS procedure MIXED was used for this purpose. Again, the mediation analyses were conducted as ITT.
In addition to following the recommendation of Kenny et al. [35], the significance of the indirect effect was assessed using bootstrap sampling with a 95% confidence interval (CI) around the indirect effect. If the interval did not contain zero, it was assumed that the indirect path was statistically significant and would represent evidence for mediation. For this purpose, 1,000 bootstrap samples were generated using random sampling with replacement.
Intervention Effects on CRCS Adherence
At the follow-up, 88 of the 412 participants reported having been appropriately screened while 264 did not report appropriate screening. There were 60 people for whom data on screening at follow-up were missing. For the ITT analysis, the latter group was coded as not having been screened. Across study conditions, CRCS adherence at follow-up was: 15.4% in GP (19/123), 28.4% in TP (40/141), and 33.0% in TP + TC (29/88). In ITT analyses, CRCS adherence at follow-up was 13.7% in GP, 24.8% in TP, and 25.9% in TP + TC.
In the initial ITT analyses, potential covariates of screening adherence were assessed and none were significant. The GEE analysis of screening adherence as a function of the intervention indicated that there was a significant (Wald Chi-square = 6.84; p = 0.033) intervention effect. Contrasts indicated that those in the TP + TC condition were significantly (Wald Chi-square = 4.40; p = 0.036) more likely to be screened than those in the GP condition, as were those in the TP condition (Wald Chi-square = 6.15; p = 0.013). However, there was no difference in screening adherence for those in the two tailored conditions.
Since there were no differences between the two tailored conditions, the data for these arms were combined and compared to GP. In what follows, the reconfigured group will be referred to as the combined tailored condition. The GEE analysis continued to indicate a significant (Wald Chi-square = 6.97, p = 0.008) combined treatment effect. In this analysis, those in the combined tailored condition were 2.12 times more likely to be adherent than those in the GP condition.
Moderator Effects
Moderator effects included previous CRCS history (yes/no), number of family members with CRC, whether the participant had received a physician recommendation for CRCS at the baseline interview, baseline CRCS intention, and the closeness of the participant’s relationship to the affected sibling. None of these variables moderated the treatment effects on screening adherence.
Mediator Effects
The results for screening adherence reported above address Kenny and colleagues’ [35] first criterion for mediation which was satisfied. In the second step of the mediation procedure, it is necessary to demonstrate that the treatment predicts the hypothesized mediating variable. For decisional balance and personalization of the print materials, a preliminary analysis using an unconditional means approach within a linear mixed model framework was conducted to determine whether it was necessary to take into account the possibility that responses of individuals within the same family might be correlated with one another thus requiring control in any subsequent analyses. Two models were run for decisional balance and personalization. The first model assumed that the responses were uncorrelated with one another and the second that they were correlated. The difference in the deviance measures for these two models are distributed as a Chi-square with degrees of freedom equal to the difference in the number of parameters to be estimated in the two models [36]. These tests indicated no statistical support for the hypothesis that an analysis controlling for clustering within families was necessary. As a result, the second step of mediation employed a traditional ANCOVA with the baseline assessment of decisional balance as the covariate. Since personalization was measured only once (at follow-up), the combined tailored condition was the only explanatory variable in the model.
If decisional balance and personalization met the criterion of being predicted by the combined tailored condition, each was then included in the GEE model predicting screening adherence as a function of the combined tailored condition. This analysis allowed an assessment of the possible mediating effect of decisional balance and personalization.
The combined tailored condition was a significant predictor of decisional balance at follow-up (F (1,393) = 5.92; p = 0.015). The mean decisional balance score for those in the combined tailored condition was significantly higher than for those in the GP condition (5.89 vs. 3.71). As noted above, those in the combined tailored condition were significantly more likely to be compliant with CRCS compared to those in the GP condition. When decisional balance was added to this model, those with higher decisional balance scores (more pros of CRCS than cons) were significantly more likely to be adherent (z = 4.01; p < 0.0001). The addition of the follow-up decisional balance score (controlling for baseline decisional balance) indicated that while the magnitude of the parameter estimate for treatment condition decreased compared to the model without decisional balance (0.73 vs 0.75), it was still statistically significant (z = 2.53; p = .012).
To assess the significance of the indirect path from the combined tailored conditions compared to the GP arm on decisional balance and from decisional balance to screening adherence, 1,000 bootstrap samples were used to generate the 95% CI for the indirect effect. Since this interval did not contain zero (0.014, 0.297), decisional balance did mediate the effect of the combined tailored condition on screening adherence. However, since the combined tailored condition continued to be a significant predictor of screening adherence after decisional balance was included in the model, this result suggests that, in addition to decisional balance, there are other potential mediators of the combined tailored condition.
The combined tailored condition was also a significant (F (1,268) = 15.87, p < 0.0001) predictor of personalization of the print materials. The mean personalization score for those in the combined tailored condition was significantly higher than for those in the GP condition (5.68 vs. 5.02). When personalization was added to the model predicting screening adherence, it was a significant predictor of screening adherence (z = 2.63, p = 0.009). However, rather than decreasing in magnitude as one would expect if personalization was a mediator, the parameter estimate for treatment condition increased (1.05 vs 0.75). Thus, personalization was not a mediator of the effect of the combined tailored condition on screening adherence.
Discussion
Results of our analyses indicate that CRCS adherence increased among intermediate risk siblings enrolled in all three intervention groups. Participants in both tailored intervention groups obtained CRCS at a significantly higher rate than participants in the generic print group. These findings are impressive because this population was relatively resistant to CRC screening. Indeed, the average time since the affected sibling’s diagnosis was more than 2 years and these participants had not yet obtained appropriate CRC screening. The fact that the tailored interventions were able to assist participants in overcoming barriers to having screening is encouraging.
CRCS adherence in the two tailored groups (ITT results = 24.8% in TP, 25.9% in TP + TC) was greater than that noted in previous studies of intermediate risk FDRs of individuals with CRC. Rawl and colleagues [16] reported risk-appropriate screening rates of 14.3% in their tailored print group and Glanz and colleagues [15] reported an increase in CRCS screening of 20% after 4 months in their CRC risk counseling intervention group. However, our rates were lower than Glanz’s 1 year follow-up, in which the risk counseling resulted in a 33% increase in CRCS over baseline rates. The significant increase in screening rates in the two tailored intervention groups of 11–12.8% relative to GP is consistent with Glanz and colleagues [15] who reported a 13% to 14% difference between their more intensive risk counseling and general health counseling groups.
Our finding that the addition of a telephone counseling session did not increase CRCS significantly is consistent with a study of average risk individuals in which a phone contact did not produce significant gains in CRCS when it was added to a tailored print intervention [19]. We do not know why telephone counseling was not effective. It is possible that the telephone counseling, while highly regarded by participants, did not address barriers to screening that had not already been covered by the tailored print and/or the relatively structured approach may not have allowed the participant and counselor to process thoroughly the practical and emotional barriers to screening in a great deal of depth. It is also possible that a single telephone session was not a sufficient dose to motivate screening adherence beyond that achieved by TP. Perhaps adding more telephone sessions, as has been done in behavioral interventions for other health behaviors (e.g., [37]) would have increased the call’s effectiveness particularly considering the lack of screening adherence evident in this sample. Resistance to the counseling contact may have been a factor. Although we were able to complete 87% of these sessions, in most cases, the effort required to complete the session was significant. Fifty percent of participants assigned to this condition canceled or missed their session at least once before completing it. Overall, the additional time and expense to deliver the single telephone counseling offered in this study did not result in improved CRCS rates beyond that achieved by the tailored print and it is doubtful that additional telephone contacts or a more comprehensive discussion of screening barriers would be either feasible or effective.
Mediators of change have received little attention in intervention studies seeking to improve cancer screening practices. In our study, we examined a number of social-cognitive variables that were targeted in the interventions. Among these factors, we identified only one mediator, decisional balance. Decisional balance partially mediated the relationship between intervention group and CRCS adherence among participants in the combined tailored condition. Knowledge of CRC and CRCS, perceived CRC risk, CRC preventability, CRC severity, physician and family support for screening, four processes of change, and personalization of the print materials did not meet criteria for mediation. Surprisingly, although personalization of the print materials was significantly impacted by the combined tailored interventions and not the generic intervention, it did not mediate treatment effects. These findings are the first published attempt to evaluate possible mechanisms for CRCS interventions. There have been two other published studies examining possible mechanisms for behavioral interventions to improve cancer screening. Our results are partially consistent with one of these studies. Aiken and colleagues [27] reported that their psychological intervention targeting mammography adherence resulted in increased perceptions of risk, which in turn led to increased perceptions of the benefits of mammography, which then lead to increases in screening intentions and ultimately to increased progression in steps to mammography (e.g., making an appointment). Although we did not evaluate these complex intermediate associations (risk and/or severity leading to intentions), our results are somewhat consistent with Aiken in that we found that decisional balance was impacted by the combined tailored interventions and served as a partial mediator of CRCS. Our results are also similar to research identifying mediators of physical activity interventions suggesting that benefits and barriers mediate activity changes [38].
The identification of mediators was challenging for this study. A review of the limited relevant literature suggests that mediator identification has been relatively challenging for other cancer screening interventions as well. For example, Hay and colleagues [39] also evaluated several social-cognitive theory constructs as possible mediators of a nurse intervention to increase skin self-examination and reported that only self-efficacy mediated treatment effects. One factor that may have influenced our results is the fact that mediators were assessed at the same time as screening status, at the 6-month follow-up time point. Future studies should include an immediate post-intervention assessment to assess changes in putative mediators which may not have lasted for 6 months.
It is surprising that decisional balance was the only mediator for the tailored interventions and that it only partially mediated the treatment effect. Along with our results suggesting that TC did not add to the effects of TP on CRCS, these results suggest that unknown characteristics of the counseling session did not add to the efficacy of TC. A more in-depth process or content analysis of the elements of the TC sessions may elucidate the reasons why TC did not add to the experimental effects.
Several limitations of this study should be noted. First, the population was primarily white, married, and possessed health insurance. There were more women in the sample than men. The gender inequity is not representative of this population which is likely comprised of an equal representation of men and women. This could limit the ability to generalize the study’s findings. Second, the acceptance rate among index patients and siblings was modest. It should be noted that our participation rate among eligible index patients (32%) was slightly higher than rates reported in other studies [16] (19%). The acceptance rate among eligible siblings (34.9%) was lower than the rates of 50% and 75% reported in two prior studies [15, 16]. Participant siblings in the present study were more likely to be female and younger than refusers which may have biased our study results in an unknown manner. A third limitation regards the timing of the assessment of mediating variables which were assessed at the time of the follow-up assessment. One criterion for proving mediation is that change in the mediator should occur before meaningful change in the outcome significantly more frequently than would be expected on the basis of chance in the intervention condition [34]. Because we did not collect data after the intervention but before the 6-month follow-up, it is possible that a change in the outcome (screening) preceded a change in the mediators which is incompatible with the concept of mediation. For example, it is possible that once the participant had screening, he/she realized that it was not as aversive as he/she initially believed (e.g., screening led to a reduction in perceived barriers). It has been noted that it is vital to document that change in the mediator precedes change in the outcome to establish mediation in randomized trials [40]. Several of the mediation measures consisted of one or two items (preventability, curability, family support) and it is possible these measures were not sufficiently sensitive to detect experimental effects. Fourth, the follow-up period was only 6 months and it is possible that there would have been greater reported CRCS rates with a longer follow-up. A final limitation is the external validity and potential for dissemination of the tailored print intervention evaluated in this study. Green and Glasgow [41] have developed a set of criteria for evaluating the external validity and potential for implementation of research which include reach and representativeness, implementation and consistency of effects, and maintenance and institutionalization. Although the present study meets a number of these criteria such as the reporting of the sample characteristics, an evaluation of possible mechanisms of change, and an assessment of moderators, it may be a challenge to access siblings of early onset CRC patients in the community and it may be difficult and costly to implement a tailored print intervention in a clinic setting. Future effectiveness research on tailored print interventions in clinic settings may best be able to address the external validity of this study.
These limitations notwithstanding, we developed and evaluated an efficacious tailored print intervention for intermediate risk siblings of individuals diagnosed with CRC and we provide initial evidence to suggest that the impact of the tailored print intervention may be partially due to increases in perceived benefits and reductions in perceived barriers. Our data also suggest that tailored telephone counseling did not add to the effects of the tailored print intervention indicating that it may not be worthwhile to pursue telephone counseling interventions of this nature with this population. However, it may be fruitful to more carefully evaluate tailored telephone counseling in terms of identifying reasons why it was not helpful. Future research should evaluate other moderators for treatment effects, additional mediators such as self-efficacy for intervention effects, assess mediators during the immediate post-intervention time interval, and consider methods to bolster screening adherence in addition to tailored print. Furthermore, assessment of the cost-effectiveness of these interventions may assist in policy decisions regarding their subsequent dissemination as a component of standard care.
References
American Cancer Society, Cancer facts and figures. Atlanta, Georgia: 2008.
Lynch HT, Lynch PM, Albana WA. Hereditary cancer: Ascertainment and management. CA. 1979; 29: 216–232.
St. John DJB, McDermott FT, Hopper LJ. Cancer risk in relatives of patients with common colorectal cancer. Ann Intern Med. 1993; 118: 785–790.
Rozen P, Fireman Z, Figer A, Legum C. Family history of colorectal cancer as a marker of potential malignancy within a screening program. Cancer. 1987; 60: 248–524.
Fuchs CS, Giovannucci E, Colditz G, Hunter DJ. A prospective study of family history and risk of colorectal cancer. N Engl J Med. 1994; 331: 1669–1674.
Johns LE, Houlston RS. A systematic review and meta-analysis of familial colorectal cancer risk. Am J Gastroenterol. 2001; 96(10): 2992–3003.
Mandel JS, Bond JH, Church TR, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. N Engl J Med. 1993; 328: 1365–1371.
Selby JV, Friedman GD, Quesenberry CPJ, Weiss NS. A case-control study of screening sigmoidoscopy and mortality from colorectal cancer. N Engl J Med. 1992; 326: 653–702.
Levin B, Lieberman A, McFarland B, et al. Screening and Surveillance for the Early Detection of Colorectal Cancer and Adenomatous Polyps, 2008: A Joint Guideline from the American Cancer Society, the US Multi-Society Task Force on colorectal Cancer and the American College of Radiology. CA A Cancer J Clin. 2008; 58: 130–160.
Thrasher J, Cummings M, Michalek A, Mahoney MK, Pillittere D. Colorectal cancer screening among individuals with and without a family history. J Public Health Manag Prac. 2002; 8: 1–9.
Ruthotto F, Papendorf F, Wegener G, et al. Participation in screening colonoscopy in first-degree relatives from patients with colorectal cancer. Ann Oncol. 2007; 18: 1518–1522.
Manne S, Markowitz A, Winawer S, et al. Correlates of colorectal cancer screening compliance and stage of adoption among siblings of individuals with early onset colorectal cancer. Health Psychol. 2002; 21(1): 3–15.
Madlensky L, Esplen MJ, Goel V. Reasons given by relatives of colorectal cancer patients for not undergoing screening. Prev Med. 2004; 39: 643–648.
Caffarey SM, Broughton CIM, Marks CG. Faecal occult blood screening for colorectal neoplasia in a targeted high-risk population. Br J Surg. 1993; 80: 1399–1400.
Glanz K, Steffen AD, Taglialatela LA. Effects of colon cancer risk counseling for first-degree relatives. Cancer Epidemiol Biomarkers Prev. 2007; 16(7): 1485–1491.
Rawl S, Champion V, Scott L, et al. A randomized trial of two print interventions to increase colon cancer screening among first-degree relatives. Patient Educ Couns. 2008; 71(2) :215–227.
Kreuter M, Wray R. Tailored and targeted health communication: Strategies for enhancing information relevance. Am J Health Promo. 2003; Supp 3: S227–32.
Noar S, Benac C, Harris M. Does tailoring matter? Meta-analytic review of tailored bring health behavior change. Psychol Bull. 2007; 133: 673–693.
Myers R, Sifri R, Hyslop T, et al. A randomized controlled trial of the impact of targeted and tailored interventions on colorectal cancer screening. Cancer. 2007; 110: 2083–2091.
Janz NK, Becker MH. The health belief model: A decade later. Health Educ Q. 1984; 84: 104–106.
Rosenstock IM. The health belief model and preventive health behavior. In: Becker MH, ed. The Health Belief Model and Personal Health Behavior. Thorofare, NJ: Charles B. Slack; 1974: 27–59.
Champion V, Skinner CS. The health belief model. In: Glanz K, Rimer BK, Viswanath K, eds. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: Jossey-Bass; 2008: 45–65.
Prochaska JO, DiClemente CC. Transtheoretical therapy: Toward a more integrative model of change. Psychother: Theory, Res Prac. 1982; 20: 161–173.
Prochaska JO, Redding C, Evers K. The transtheoretical model and stages of change. In: Glanz K, Rimer BK, Viswanath K, eds. Health Behavior and Health Education: Theory Research and Practice. San Francisco, CA: Jossey-Bass; 2008: 97–121.
Leventhal H. Findings and theory in the study of fear communications. Adv Exp Social Psychol. 1970; 5: 119–186.
Leventhal H, Brissette I, Leventhal EA. The common-sense model of self-regulation of health and illness. In: Cameron LD, Leventhal H, eds. The self-regulation of health and illness behaviour. London: Routledge; 2003: 42–65.
Aiken LS, West SG, Woodward CK, Reno RR. Health beliefs and compliance with mammography-screening recommendations in asymptomatic women. Health Psychol. 1994; 13: 122–129.
Rauscher G, Earp J, O’Malley M. Relation between intervention exposures, changes in attitudes and mammography use in the North Carolina Breast Cancer Screening Program. Cancer Epidemiol Biomarkers Prev. 2004; 13: 741–747.
Center for Disease Control. Colorectal Cancer Screening Saves Lives. CDC Pamphlet, 2002; available at http://www.cdc.gov/cancer/colorectal/sfl/print_materials. Accessability verified October 22, 2008.
Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. New York: Guildord Press; 2002.
Townsend A, Franks M. Binding ties: Closeness and conflict in adult children’s caregiving relationships. Psychol Aging. 1995; 10: 343–351.
Lipkus I, Rimer B, Halabi S, Strigo T. Can tailored interventions increase mammography us among HMO women. Am J Prev Med. 2000; 18(1): 1–10.
Brug J, Steenhuis I, Van Assema P, de Vries H. The impact of a computer-tailored nutrition intervention. Prev Med. 1996; 25: 236–242.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological and research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986; 51: 1173–1182.
Kenny DA, Kashy DA, Bolger N. Data analysis in social psychology. Vol. 1. In: Gilbert D, Fiske ST, Lindzey G, eds. Handbook of Social Psychology. 4th ed. McGraw-Hill: New York; 2003.
Singer JD, Willett JB. Applied Longitudinal Data A: Modeling Change and Event Occurrence. New York: Oxford; 2003.
Prochaska JO, DiClemente CC, Velicer WF, Rossi JS. Standardized, individualized, interactive, and personalized self-help programs for smoking cessation. Health Psychol. 1993; 12: 399–405.
Pinto BM, Lynn H, Marcus BH, DePue J, Goldstein MG. Physical-based activity counseling: Intervention effects on mediators of motivational readiness for physical activity. Ann Behav Med. 2001; 23(23): 2–10.
Hay J, Oliveria S, Dusza S, et al. Psychosocial mediators of a nurse intervention to increase skin self-examination in patients at high risk for melanoma. Cancer Epidemiol Biomarkers Prev. 2006; 15: 1212–1216.
Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001; 158(6): 848–856.
Green LW, Glasgow RE. Evaluating the relevance, generalization and applicability of research: Issues in external validation and translation methodology. Eval Health Prof. 2006; 29 s:126–153.
Acknowledgements
We would like to thank Jackie Allen, Christine Armetta, Hela Bakal, Pat Barry, Trudy Bennett, Cathy Betz, Angela Calnon, Lauren DeEcheandia, Terry Del Rio, Gail DeMaio, Rebekah Dunn, Tim Estrella, Millie Fleetwood, Diane Foglia, Lugenia Ford, Dot Freeman, Jolene Garney, Linda Gray, Leigh Hamilton, Laura Hammond, Danielle Hawthorne, Dr. Tim Hoops, Kim Kiefer, Betsy Kopp, Nancy Koppelman, Dr. Ben Krevsky, Stefanie Lappe, Denise LaRue, Debra Marra, Michele Marshall, Katie Masters, Tracy Max, Stacy McConnell, Kristine Miranda, Cheryl Mongillo, Eileen Morris, Dr. Peter O’Dwyer, Melanie Pirollo, Nancy Rohowyj, Kevin Schumann, Maggie Sibert, Marianna Silverman, Kristen Sorice, Wendy Stanton, Richard Throm, Amanda Tow, Gail Upshaw, Katherine Waite, and Pat Weiser for assistance with data collection. We would like to thank Wayne Bulger and Micromass Communications, Inc., who produced the tailored print materials. Maryann Krayger provided technical assistance in preparation of this article. Belinda Borrelli, Ph.D. provided supervision in MI. We would like to thank the physicians and nurses at all study sites, as well as the staff of the Cancer Community Oncology Program for their assistance in identifying participants for this study. This work was supported by grant RO1CA75795 from the National Institutes of Health to Sharon L. Manne and P30 CA006927 to Fox Chase Cancer Center.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Manne, S.L., Coups, E.J., Markowitz, A. et al. A Randomized Trial of Generic Versus Tailored Interventions to Increase Colorectal Cancer Screening Among Intermediate Risk Siblings. ann. behav. med. 37, 207–217 (2009). https://doi.org/10.1007/s12160-009-9103-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-009-9103-x