Abstract
Purpose
The prognostic value of 18F-FDG PET/CT for primary intestinal diffuse large B-cell lymphoma (PI-DLBCL) patients has not been determined. This prompted us to explore the value of 18F-FDG PET/CT for prognostic stratification in patients with PI-DLBCL treated with an R-CHOP-like regimen.
Materials and methods
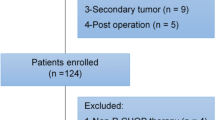
Seventy-three PI-DLBCL patients who underwent baseline PET/CT between January 2010 and May 2019 were included in this retrospective study. Total metabolic tumor volume (TMTV) and total lesion glycolysis (TLG) were computed using the 41% SUVmax thresholding method. Progression-free survival (PFS) and overall survival (OS) were used as endpoints to evaluate prognosis.
Results
During the follow-up period of 3–117 months (29.0 ± 25.5 months), high TLG, non-germinal center B-cell-like (non-GCB) and high National Comprehensive Cancer Network International Prognostic Index (NCCN-IPI) were significantly associated with inferior PFS and OS. TLG, cell-of-origin and NCCN-IPI were independent predictors of PFS, and both TLG and NCCN-IPI were independent predictors of OS. The grading system was based on the number of risk factors (high TLG, non-GCB, high NCCN-IPI) and patients were divided into 4 risk groups (PFS: χ2 = 33.858, P < 0.001; OS: χ2 = 29.435, P < 0.001): low-risk group (none of the 3 risk factors, 18 patients); low-intermediate risk group (1 risk factor, 24 patients); high-intermediate risk group (2 risk factors, 16 patients); and high-risk group (all 3 risk factors, 15 patients).
Conclusions
High TLG, non-GCB and high NCCN-IPI can identify a subset of PI-DLBCL patients with inferior survival outcomes. Furthermore, the grading system can identify PI-DLBCL patient groups with markedly different prognoses, which might contribute to the adjustment of the therapeutic regime.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The gastrointestinal tract is the most commonly involved extranodal site of non-Hodgkin’s lymphoma (NHL). Intestinal NHL (I-NHL) is far less frequent than gastric lymphoma and accounts for 30–40% of primary gastrointestinal lymphomas [1, 2]. A multicenter, retrospective analysis of 581 patients showed that patients with non-Hodgkin’s lymphoma of the small and large intestines primarily displayed diffuse large B-cell lymphoma (DLBCL) subtype (66.4%) [3]. Combination treatment of surgery and CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) or R-CHOP (rituximab plus) chemotherapy was reported to provide better survival outcomes for primary intestinal DLBCL (PI-DLBCL) patients than chemotherapy alone [4]. However, surgical resection of the primary mass remains a topic of debate because DLBCL itself is a disease that can be cured by chemotherapy, and some PI-DLBCL patients were observed to respond well to chemotherapy in the absence of surgical tumor resection [5, 6]. To date, the appropriateness(the chemotherapy or surgical tumor resection) in the therapeutic strategy of PI-DLBCL has not been defined. Therefore, an accurate risk stratification method is urgently needed to tailor therapies for individual patients.
A growing body of literature shows that quantitative FDG PET/CT indices, such as metabolic tumor volume (MTV) or total lesion glycolysis (TLG), prior to treatment can be used to risk-stratify patients with nodal DLBCL and may be valuable in guiding clinical and therapeutic decisions [7,8,9]. However, evidence that the quantitative metrics are able to predict survival in patients with primary gastrointestinal DLBCL remains limited due to the scarcity of research on this subject [10, 11]. Moreover, gastric and intestinal NHL are often discussed together in most studies but differ significantly from each other in clinical features, pathology, treatment and prognosis [2, 12, 13]. The published data and recommendations concerning the role of 18F-FDG PET in PI-DLBCL are still lacking. Therefore, in the current study we explored the value of 18F-FDG PET/CT for prognostic stratification in patients with newly diagnosed PI-DLBCL treated with an R-CHOP-like regimen.
Patients and methods
Patients
We conducted a retrospective study of patients with newly diagnosed PI-DLBCL between January 2010 and May 2019, who underwent baseline whole-body FDG PET/CT. Main inclusion criteria were histological confirmation of PI-DLBCL and treatment with an R-CHOP-like regimen with curative intent. Patients were excluded if they were treated surgically. Patients who had a previous malignancy, chemotherapy, radiotherapy, pregnancy or lactation, or diabetes mellitus with a fasting blood glucose level greater than 150 mg/dL were also excluded from this study. Clinical parameters [sex, age, B symptoms, Eastern Cooperative Oncology Group Performance Status (ECOG PS), International Prognostic Index (IPI), and LDH level] were collected from the medical records. Ann Arbor stage modified by Musshoff was defined [14, 15]. The NCCN-IPI estimating a maximum of 8 scoring points was evaluated, and patients with a score of 0/1 are categorized as low risk, 2/3 as low-intermediate, 4/5 as high-intermediate and 6/7/8 as high risk [16]. For the purpose of this study, the four NCCN-IPI risk groups were dichotomized into low-risk NCCN-IPI (comprising low- and low-intermediate-risk patients) and high-risk (comprising high-intermediate- and high-risk patients) groups. Approval was obtained from the Ethics Committee of Nanjing Drum Tower Hospital, the Affiliated Hospital of Nanjing University Medical School.
PET/CT scan protocol
All patients underwent whole-body 18F-FDG PET/CT on a combined Gemini GXL PET/CT scanner with a 16-slice CT component (Philips Corp, the Netherlands). After six hours of fasting (no oral or intravenous fluids containing dextrose or other sugars), 185–370 MBq of 18F-FDG (5.18 MBq/kg) was administered intravenously. The patient’s blood glucose level was checked immediately before 18F-FDG administration. Each patient was weighed for standardized uptake value (SUV) determination prior to each scan. Whole-body PET/CT scans (from the top of the head to the upper thigh) were started sixty minutes after radiopharmaceutical injection. CT scan was performed with parameters set to 80 milliamperage-seconds (mAs) and 150 kilovolt peak (kVp). Slice thickness was 3.75–5 mm. For the FDG-PET scan, 2-min emission acquisitions per field of view were obtained in three-dimensional mode. PET scans were reconstructed in a 128 × 128 matrix with an ordered subset maximum expectation iterative reconstruction algorithm and attenuation correction based on CT data. The acquired images from the PET and CT scans were sent for image registration and fusion using Syntegra software.
Imaging analysis
PET/CT images were read by 2 physicians specializing in nuclear medicine. They were blinded to all patient information including the patient’s clinical condition. The results were determined by a consensus reached by the two physicians. Images were reviewed using the volume viewer software on a dedicated workstation (CompassView 5.0, Philips Corp, the Netherlands) to calculate SUV, MTV and TLG. Two-dimensional regions of interest (ROIs) were placed manually to cover the lesion and then a volumetric ROI was produced automatically by the software. Finally, the determined ROI was adjusted manually to fully encase all involved lesions in axial, coronal and sagittal PET/CT images. When a polylobular or extremely extensive lesion with multiple hypermetabolic tumor foci was present, the ROI of each hypermetabolic tumor focus was drawn separately. The PET parameters such as SUVmean, SUVmax as well as MTV of the lesion were produced automatically by the software. The boundaries of voxels were produced automatically with the 41% SUVmax threshold method recommended by the European Association of Nuclear Medicine, because of the high interobserver reproducibility previously described in lymphoma [17]. The circle was modified to include pathological lesions and to exclude sites of normal organs and false-positive lesions (e.g., inflammation, infection or other benign FDG-avid lesions). When the localization of lesions or intestine level of 18F-FDG uptake were unidentifiable on PET/CT, the endoscopy and abdomen enhanced CT results were used for reference. The TMTV was obtained by summing the MTV of all lesions. TLG was calculated as the sum of all MTV × SUV (mean of lesions) in each patient. SUVmax values were obtained and corrected for bodyweight using the following standard formula: mean ROI activity (MBq/mL)/[injected dose (MBq)/body weight (kg)].
Tissue microarrays and immunohistochemistry
Three representative cores (0.6 mm) of formalin-fixed, paraffin-embedded tissue (FFPE) from each case were used to build tissue microarrays (TMAs). Immunohistochemical staining was performed on 4-μm sections using standard procedures. GCB and non-GCB phenotypes were defined using the decision tree established by Hans and colleagues with indicated cut-offs [18].
Treatment and follow-up period
All patients had been treated with four to eight cycles of a standard-dose R-CHOP-like regimen. Follow-up evaluation consisted of history, physical examinations, endoscopy, abdominal ultrasound, whole-body FDG PET/CT (not in all patients), MRI scans of the head and CT scans of the neck, thorax, abdomen, and pelvis (if necessary). Patients were examined every 3 months for at least 2 years and twice a year afterwards.
Statistical methods
Progression-free survival (PFS) and overall survival (OS) were chosen as the end points to evaluate the prognosis of PI-DLBCL patients. PFS was defined as the interval between the date of diagnosis and the date of first relapse, progression, death from any cause, or last follow-up examination. OS was defined as the interval from the date of diagnosis until the time of death from any cause or last follow-up. Survival functions were estimated using the Kaplan–Meier method and were compared using log-rank tests. All PET and clinical variables, as well as prognostic scores, including the IPI and NCCN-IPI, deemed significant in the univariate analysis were entered into a multivariate analysis using the Cox proportional hazards model. Receiver operating characteristic (ROC) curves were constructed to estimate accuracy in predicting ideal cut-off values for SUVmax, TMTV and TLG. All statistical analyses were performed using SPSS 22.0, and P values less than 0.05 were considered to be significant.
Results
Patient characteristics and treatment results
The clinical characteristics of the 73 patients (27 women and 46 men) included in the study are summarized in Table 1. After a median follow-up of 20 months (range 3–117 months), 33 patients had disease relapse or progression, and 26 patients died.
Clinical characteristics of patients in relation to TMTV and TLG
The differences in clinical characteristics between the dichotomized TLG groups are shown in Table 2.
ROC curve analysis of SUVmax, TMTV and TLG
In the present study, ROC curve analysis was used to calculate the accuracy of ideal cut-off values to distinguish a low SUVmax group from a high SUVmax group, a low TMTV group from a high TMTV group and a low TLG group from a high TLG group. The estimated area under the ROC curve (AUROC) for SUVmax was 0.656, that for TMTV was 0.784 and that for TLG was 0.794. The ideal cut-off values for SUVmax, TMTV and TLG were 25.3, 211.1 cm3 and 1559.8, respectively (Fig. 1).
Univariate and multivariate analysis
The mean PFS was 60.5 months (95% CI 46.7–74.2, range 3–117 months), and the mean OS was 71.4 months (95% CI 57.9–85.0, range 3–117 months). The PFS and OS estimates for all patients were 54.8% and 64.4%, respectively. The univariate analyses are shown in Table 3 and Fig. 2. High NCCN-IPI, non-GCB as well as high TLG were significantly correlated with both inferior PFS and OS. NCCN-IPI (P = 0.001), non-GCB (P = 0.037) and TLG (P = 0.025) remained statistically independent predictors of PFS, and both TLG (P < 0.001) and NCCN-IPI (P = 0.016) were statistically independent predictors of OS after multivariate analysis (Table 4).
Kaplan–Meier plots for PFS and OS in all patients in relation to TLG (< 1559.8 vs. ≥ 1559.8), cell-of-origin (GCB and non-GCB) and NCCN-IPI score (low-risk score 0–3 vs. high-risk score 4–8). PFS (a) and OS (b) in relation to TLG; PFS (c) and OS (d) in relation to the cell-of-origin; PFS (e) and OS (f) in relation to the NCCN-IPI score
Grading system to predict PFS and OS in PI-DLBCL
The grading system was based on the number of risk factors following the results of univariate and multivariate analysis (high TLG, non-GCB, high NCCN-IPI), and patients were divided into 4 risk groups (PFS: χ2 = 33.858, P < 0.001; OS: χ2 = 29.435, P < 0.001); low-risk group (none of the 3 risk factors, 18 patients); low-intermediate risk group (1 risk factor, 24 patients); high-intermediate risk group (2 risk factors, 16 patients); and high-risk group (all 3 risk factors, 15 patients) (Fig. 3a). Survival curves generated by Kaplan–Meier analysis are used to display the differences among these 4 risk groups by the grading system, which showed a stronger ability to reveal further discrimination among subgroups compared with NCCN-IPI alone (Fig. 3b, c and Table 5).
Discussion
The combined treatment of rituximab with CHOP (R-CHOP) was readily adopted as a standard treatment for DLBCL and shown to achieve a significant improvement in the prognosis of patients with nodal DLBCL [19, 20]. However, the published data based on PI-DLBCL are still limited. PI-DLBCL, as a subtype of DLBCL with the extranodal presentation, has significantly different molecular and clinical characteristics from nodal DLBCL, suggesting that they should be regarded as separate entities [21,22,23]. Therefore, we aimed to explore the value of 18F-FDG PET/CT for prognostic stratification in patients with PI-DLBCL treated with an R-CHOP-like regimen in the current study.
The quantization parameters (MTV and TLG) of 18F-FDG PET/CT have been shown to be useful in the prognosis evaluation in patients with nodal DLBCL [9]. TLG on baseline PET appeared to be a powerful predictor of patients with extranodal DLBCL originating from primary mediastinal [24], central nervous system [25] and testicular [26] areas. In the present study, we addressed the issue of the prognostic value of TLG on 18F-FDG PET/CT prior to pretreatment in PI-DLBCL patients. The results indicated that patients with TLG greater than 1559.8 had lower survival, with TLG being an independent predictor of survival outcomes after multivariate analysis. This finding is inconsistent with Alagöz et al.’s research, which demonstrated that TLG was not a predictive marker for primary gastrointestinal lymphoma [11]. The reasons for these discrepancies may be partially explained by the fact that patients included in Alagöz et al.’s study are gastric and intestinal DLBCL patients combined, which significantly differ from each other in prognosis [12]. Interestingly, the TMTV was also evaluated but was found to not be an independent predictor in our study. The reason for this finding could be partially explained by the fact that TLG obtained by multiplying SUV mean by MTV can contribute to patient management by assessing both tumor volume and metabolism together [27].
In recent years, with the progress of molecular genetic research, it was determined that molecular tumor heterogeneity is directly correlated with the treatment response and prognosis and will be crucial to the development of individualized risk-adapted therapy [28]. The cell-of-origin phenotype has been demonstrated to be a strong prognostic biomarker that the presence of the non-GCB type would be associated with a dismal prognosis in DLBCL [18, 29, 30]. In our study, non-GCB type was shown to be significantly associated with PFS (HR 3.400, P = 0.004) and OS (HR 2.830, P = 0.026), and an independent predictor of PFS. These results confirmed that cell-of-origin phenotype is a powerful tool to predict survival outcomes in PI-DLBCL patients.
Following the introduction of rituximab in the treatment of patients with DLBCL, the impact of IPI on the prognostic prediction was deduced and questioned [31,32,33]. With the pressing needs for newer strategies to better subcategorize DLBCL patients in the rituximab era, NCCN-IPI was proposed by Zhou et al. in 2014 and can better discriminate low and high-risk subgroups than the IPI [16]. In the current study, the Kaplan–Meier curves for PFS and OS were plotted with 2 subgroup stratification based on IPI and NCCN-IPI, respectively, and patients in the 2 NCCN-IPI groups showed a distinctive clinical outcome (PFS: HR 3.219, P = 0.001; OS: HR 3.515 P = 0.002), whereas patients subcategorized by the IPI exhibited a less discriminatory survival pattern (PFS: HR 2.891, P = 0.002; OS: HR 2.723, P = 0.011). Moreover, NCCN-IPI was shown to be an independent predictor of survival outcomes in multivariate analysis. Our result confirms that the NCCN-IPI is a more robust and useful prognostic tool to stratify PI-DLBCL patients.
Prior studies have demonstrated that integration of molecular indices or PET quantization parameters with IPI or NCCN-IPI could yield a better stratification for DLBCL patients [34, 35]. Other studies also reported the combination of molecular and PET imaging metrics at diagnosis could lead to a more accurate selection of patients [36, 37]. To establish a risk stratification model for PI-DLBCL patients, we encompass the factors that showed the significant prognostic value in multivariate analysis. The grading system, including clinical and laboratory information (NCCN-IPI), volume and metabolism (TLG), as well as molecular profile (cell-of-origin), showed a more favorable capability to stratify patients in different groups separated by the number of risk factors compared with NCCN-IPI alone.
This study has several limitations. First, our analysis is based on a single-center retrospective analysis with a limited number of patients. Multicenter prospective studies with many more patients are needed to avoid potential bias in analysis results. Additionally, the differences in threshold used for delineating the tumor when calculating TMTV and TLG might result in inconsistencies among studies. While SUV ≥ 2.5 as a marginal threshold method was reported to be easier to utilize in practice [38], it is more prone to variability by different reconstruction protocols or PET/CT systems than the method using threshold of 41% SUVmax recommended for tumor imaging by the European Association of Nuclear Medicine [17]. To date, the proper method to calculate and identify volumetric parameters is still under debate and warrants further research. Besides, the sum of volumes obtained from the manual positioning of ROI would be affected by a systematic error due to the operators.
In summary, our study focused on the prognostic value of PET/CT quantitative parameters in PI-DLBCL. The results of our study suggest that NCCN-IPI, non-GCB as well as TLG could be prognostic factors of PI-DLBCL. The grading system based on NCCN-IPI, non-GCB and TLG could more accurately predict the prognosis of patients and guide treatments.
References
d’Amore F, Brincker H, Grønbaek K, Thorling K, Pedersen M, Jensen MK, et al. Non-Hodgkin’s lymphoma of the gastrointestinal tract: a population-based analysis of incidence, geographic distribution, clinicopathologic presentation features, and prognosis. Danish Lymphoma Study Group. J Clin Oncol. 1994;12:1673–84.
Nakamura S, Matsumoto T, Iida M, Yao T, Tsuneyoshi M. Primary gastrointestinal lymphoma in Japan: a clinicopathologic analysis of 455 patients with special reference to its time trends. Cancer. 2003;97:2462–73.
Kim SJ, Choi CW, Mun YC, Oh SY, Kang HJ, Lee SI, et al. Multicenter retrospective analysis of 581 patients with primary intestinal non-hodgkin lymphoma from the Consortium for Improving Survival of Lymphoma (CISL). BMC Cancer. 2011;11:321.
Kim SJ, Kang HJ, Kim JS, Oh SY, Choi CW, Lee SI, et al. Comparison of treatment strategies for patients with intestinal diffuse large B-cell lymphoma: surgical resection followed by chemotherapy versus chemotherapy alone. Blood. 2011;117:1958–65.
Kobayashi H, Nagai T, Omine K, Sato K, Ozaki K, Suzuki T, et al. Clinical outcome of non-surgical treatment for primary small intestinal lymphoma diagnosed with double-balloon endoscopy. Leuk Lymphoma. 2013;54:731–6.
Daum S, Ullrich R, Heise W, Dederke B, Foss HD, Stein H, et al. Intestinal non-Hodgkin's lymphoma: a multicenter prospective clinical study from the German Study Group on Intestinal non-Hodgkin’s Lymphoma. J Clin Oncol. 2003;21:2740–6.
Sasanelli M, Meignan M, Haioun C, Berriolo-Riedinger A, Casasnovas RO, Biggi A, et al. Pretherapy metabolic tumour volume is an independent predictor of outcome in patients with diffuse large B-cell lymphoma. Eur J Nucl Med Mol Imaging. 2014;41:2017–22.
Xie M, Zhai W, Cheng S, Zhang H, Xie Y, He W. Predictive value of F-18 FDG PET/CT quantization parameters for progression-free survival in patients with diffuse large B-cell lymphoma. Hematology. 2016;21:99–105.
Kim TM, Paeng JC, Chun IK, Keam B, Jeon YK, Lee SH, et al. Total lesion glycolysis in positron emission tomography is a better predictor of outcome than the International Prognostic Index for patients with diffuse large B cell lymphoma. Cancer. 2013;119:1195–202.
Song MK, Chung JS, Shin HJ, Moon JH, Lee JO, Lee HS, et al. Prognostic value of metabolic tumor volume on PET/CT in primary gastrointestinal diffuse large B cell lymphoma. Cancer Sci. 2012;103:477–82.
Alagöz E, Okuyucu K, İnce S, Kantarcıoğlu M, Özaydın Ş, Heper C, et al. Uptake patterns of untreated primary gastrointestinal extranodal lymphomas on initial staging (18)F-FDG PET/CT and metabolic tumor parameters. Mol Imaging Radionucl Ther. 2017;26:83–92.
Koch P, del Valle F, Berdel WE, Willich NA, Reers B, Hiddemann W, et al. Primary gastrointestinal non-Hodgkin’s lymphoma: I. Anatomic and histologic distribution, clinical features, and survival data of 371 patients registered in the German Multicenter Study GIT NHL 01/92. J Clin Oncol. 2001;19:3861–73.
Fischbach W, Dragosics B, Kolve-Goebeler ME, Ohmann C, Greiner A, Yang Q, et al. Primary gastric B-cell lymphoma: results of a prospective multicenter study. The German-Austrian Gastrointestinal Lymphoma Study Group. Gastroenterology. 2000;119:1191–202.
International Non-Hodgkin's Lymphoma Prognostic Factors Project. A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl J Med. 1993;329:987–94.
Radaszkiewicz T, Dragosics B, Bauer P. Gastrointestinal malignant lymphomas of the mucosa-associated lymphoid tissue: factors relevant to prognosis. Gastroenterology. 1992;102:1628–38.
Zhou Z, Sehn LH, Rademaker AW, Gordon LI, Lacasce AS, Crosby-Thompson A, et al. An enhanced International Prognostic Index (NCCN-IPI) for patients with diffuse large B-cell lymphoma treated in the rituximab era. Blood. 2014;123:837–42.
Meignan M, Sasanelli M, Casasnovas RO, Luminari S, Fioroni F, Coriani C, et al. Metabolic tumour volumes measured at staging in lymphoma: methodological evaluation on phantom experiments and patients. Eur J Nucl Med Mol Imaging. 2014;41:1113–22.
Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103:275–82.
Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R, et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med. 2002;346:235–42.
Sehn LH, Donaldson J, Chhanabhai M, Fitzgerald C, Gill K, Klasa R, et al. Introduction of combined CHOP plus rituximab therapy dramatically improved outcome of diffuse large B-cell lymphoma in British Columbia. J Clin Oncol. 2005;23:5027–33.
López-Guillermo A, Colomo L, Jiménez M, Bosch F, Villamor N, Arenillas L, et al. Diffuse large B-cell lymphoma: clinical and biological characterization and outcome according to the nodal or extranodal primary origin. J Clin Oncol. 2005;23:2797–804.
Al-Humood SA, Al-Qallaf AS, Alshemmari SH, Francis IM, Junaid TA, Marouf RA, et al. Genotypic and phenotypic differences between nodal and extranodal diffuse large B-cell lymphomas. J Histochem Cytochem. 2011;59:918–31.
Shi Y, Han Y, Yang J, Liu P, He X, Zhang C, et al. Clinical features and outcomes of diffuse large B-cell lymphoma based on nodal or extranodal primary sites of origin: analysis of 1085 WHO classified cases in a single institution in China. Chin J Cancer Res. 2019;31:152–61.
Ceriani L, Martelli M, Zinzani PL, Ferreri AJM, Botto B, Stelitano C, et al. Utility of baseline 18FDG-PET/CT functional parameters in defining prognosis of primary mediastinal (thymic) large B-cell lymphoma. Blood. 2015;126:950–6.
Okuyucu K, Alagoz E, Ince S, Ozaydin S, Arslan N, et al. Can metabolic tumor parameters on primary staging (18)F-FDG PET/CT aid in risk stratification of primary central nervous system lymphomas for patient management as a prognostic model? Rev Esp Med Nucl Imagen Mol. 2018;37:9–14.
Yang J, Zhu S, Pang F, Xu M, Dong Y, Hao J, et al. Functional parameters of (18)F-FDG PET/CT in patients with primary testicular diffuse large B-Cell lymphoma. Contrast Media Mol Imaging. 2018;2018:8659826.
Sarikaya I, Sarikaya A. Assessing PET parameters in oncologic (18)F-FDG studies. J Nucl Med Technol. 2019. https://doi.org/10.2967/jnmt.119.236109.
Sehn LH, Gascoyne RD. Diffuse large B-cell lymphoma: optimizing outcome in the context of clinical and biologic heterogeneity. Blood. 2015;125:22–32.
Alizadeh AA, Eisen MB, Davis RE, Ma C, Lossos IS, Rosenwald A, et al. Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature. 2000;403:503–11.
Rosenwald A, Wright G, Chan WC, Connors JM, Campo E, Fisher RI, et al. The use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. N Engl J Med. 2002;346:1937–47.
Ziepert M, Hasenclever D, Kuhnt E, Glass B, Schmitz N, Pfreundschuh M, et al. Standard International prognostic index remains a valid predictor of outcome for patients with aggressive CD20+ B-cell lymphoma in the rituximab era. J Clin Oncol. 2010;28:2373–80.
Sehn LH, Berry B, Chhanabhai M, Fitzgerald C, Gill K, Hoskins P, et al. The revised International Prognostic Index (R-IPI) is a better predictor of outcome than the standard IPI for patients with diffuse large B-cell lymphoma treated with R-CHOP. Blood. 2007;109:1857–61.
Yang Y, Wang L, Ma Y, Han T, Huang M. The enhanced international prognostic index for diffuse large B-cell lymphoma. Am J Med Sci. 2017;353:459–65.
Alizadeh AA, Gentles AJ, Alencar AJ, Liu CL, Kohrt HE, Houot R, et al. Prediction of survival in diffuse large B-cell lymphoma based on the expression of 2 genes reflecting tumor and microenvironment. Blood. 2011;118:1350–8.
Shagera QA, Cheon GJ, Koh Y, Yoo MY, Kang KW, Lee DS, et al. Prognostic value of metabolic tumour volume on baseline (18)F-FDG PET/CT in addition to NCCN-IPI in patients with diffuse large B-cell lymphoma: further stratification of the group with a high-risk NCCN-IPI. Eur J Nucl Med Mol Imaging. 2019;46:1417–27.
Cottereau AS, Lanic H, Mareschal S, Meignan M, Vera P, Tilly H, et al. Molecular profile and FDG-PET/CT total metabolic tumor volume improve risk classification at diagnosis for patients with diffuse large B-Cell lymphoma. Clin Cancer Res. 2016;22:3801–9.
Toledano MN, Desbordes P, Banjar A, Gardin I, Vera P, Ruminy P, et al. Combination of baseline FDG PET/CT total metabolic tumour volume and gene expression profile have a robust predictive value in patients with diffuse large B-cell lymphoma. Eur J Nucl Med Mol Imaging. 2018;45:680–8.
El-Galaly TC, Villa D, Gormsen LC, Baech J, Lo A, Cheah CY. FDG-PET/CT in the management of lymphomas: current status and future directions. J Intern Med. 2018;284:358–76.
Acknowledgements
The authors wish to thank all the radiographers in the Department of Nuclear Medicine, Nanjing Drum Tower Hospital, the Affiliated Hospital of Nanjing University Medical School, for their help in this study.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jiang, C., Teng, Y., Chen, J. et al. Value of 18F-FDG PET/CT for prognostic stratification in patients with primary intestinal diffuse large B cell lymphoma treated with an R-CHOP-like regimen. Ann Nucl Med 34, 911–919 (2020). https://doi.org/10.1007/s12149-020-01536-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-020-01536-w