Abstract
Objective
Stereotactic ablative radiotherapy (SABR), also known as stereotactic body radiotherapy (SBRT), is now a standard treatment option for patients with stage I non-small cell lung cancer or oligometastatic lung tumor who are medically inoperable or medically operable but refuse surgery. When mass-like consolidation is observed on follow-up CT after SABR, it is sometimes difficult to differentiate tumor recurrence from SABR-induced pulmonary fibrosis. In this study, we evaluated the role of 18F-fluorodeoxyglucose positron emission tomography combined with computed tomography (FDG-PET/CT) in differentiating tumor recurrence from radiation fibrosis after SABR.
Methods
Between June 2006 and June 2009, 130 patients received SABR for stage I non-small cell lung cancer or metastatic lung cancer at our institution. Fifty-nine patients of them were imaged with FDG-PET/CT after SABR. There were a total of 137 FDG-PET/CT scans for retrospective analysis. The FDG uptake in the pulmonary region was assessed qualitatively using a 3-point scale (0, none or faint; 1, mild; or 2, moderate to intense), and the shape (mass-like or non mass-like) was evaluated. For semi-quantitative analysis, the maximum standardized uptake value (SUVmax) was calculated.
Results
Sixteen of 59 patients had local failure. In recurrent tumor, the combination of intensity grade 2 and mass-like shape was most common (21/23; 91 %). By contrast, in cases of radiation fibrosis, the combination of intensity grade 0 or 1 and non mass-like shape was most common (48/59; 81 %). The SUVmax of tumor recurrence after 12 months was significantly higher than that of radiation fibrosis (8.0 ± 3.2 vs. 2.1 ± 0.9, p < 0.001), and all tumor recurrence showed the SUVmax > 4.5 at diagnosis of local failure. At ≥12 months after SABR, these two variables, the combination of intensity 2 and mass-like FDG uptake or SUVmax > 4.5 acquired a significant high predictive value of local recurrence, finding sensitivity 100 % and specificity 100 % for both of them.
Conclusions
The combination of FDG uptake patterns and SUVmax was useful for distinguishing tumor recurrence from radiation fibrosis after SABR.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hypofractionated high-dose stereotactic ablative radiotherapy (SABR), also known as stereotactic body radiotherapy (SBRT), is effective for local control of stage I non-small cell lung cancer (NSCLC) [1–3].
The radiographic appearance of radiation-induced pulmonary changes caused by SABR is distinct from the changes induced by conventional radiotherapy, because of its complex beam arrangements and steep dose gradients around the target volume to deliver high-dose localizing to the tumor [4–7]. Therefore, CT changes after SABR can develop as mass-like patterns and it is sometimes difficult to determine whether a mass-like lesion on follow-up CT is radiation fibrosis or tumor recurrence [7].
In these cases, 18F-fluorodeoxyglucose (FDG) positron emission tomography (PET) can play an important role [8]. Fused images of FDG-PET and CT may allow the differentiation of metabolically active recurrent tumor from inactive radiation-induced fibrosis. However, reports of the clinical significance of FDG-PET/CT after SABR are extremely limited [9, 10]. In this study, we evaluated patterns of FDG uptake and the maximum standardized uptake value (SUVmax) for differentiating tumor recurrence from radiation fibrosis after SABR.
Materials and methods
Patients
Between June 2006 and June 2009, 130 patients with stage I NSCLC or metastatic lung cancer received SABR at our institution. For these patients, the maximum cumulative tumor diameter was smaller than 5 cm and the number of tumors in the lung was one to three [11]. For this study, we retrospectively collected the patients’ data. All of the patients provided written informed consent for SABR and our institutional review board approved this study on July 29, 2010 and waved the need for informed consent based on the retrospective design. Inclusion criteria were as follows: (1) availability of at least one FDG-PET/CT scan performed 1 or more months after SABR, (2) no other conventional radiation therapy for the lung tumor was performed, (3) follow-up for at least 6 months after completion of SABR.
Among the 130 patients, 59 patients were excluded by criterion (1), 7 patients by criterion (2), and 5 patients by criterion (3). As of June 2009, 59 patients with 66 lung tumors were included in this study. Seven patients with two lesions were each treated twice with SABR at different times. Thus, we investigated a total of 66 SABR series. The characteristics of the study patients are shown in Table 1. Thirty-nine patients were male; twenty were female. The median age of the patients was 75 years old (range 45–92). There were 50 primary lung cancers and 16 metastatic lung tumors. Regarding primary lung cancer, there were 19 lesions of pathologically proven adenocarcinoma and 9 lesions of squamous cell carcinoma.
The remaining 22 lesions were considered as lung cancer without pathologically proven evidence. In patients with significant comorbidities and limited lung function, biopsy can be considered unsafe and is, therefore, contraindicated. These patients were diagnosed by measuring successive increases in tumor size on CT, as well as by increased uptake on PET and/or elevated levels of tumor markers. Among the metastatic lung tumors, the primary sites were colon, uterus, and other sites. The post-SABR median follow-up duration was 29 months (range 7–52).
Treatment methods
All patients were irradiated using stereotactic techniques. For SABR, a micro-multileaf collimator system “BrainLAB m3” (BrainLAB, Germany) was used. An immobilization body frame (BodyFIX, Medical Intelligence, Germany) was used for patient fixation during planning CT scanning and during SABR. Three-dimensional RT planning was performed using a treatment planning system (BrainSCAN, BrainLAB, Germany). The software of BrainSCAN uses the pencil beam method as calculation algorithm. The internal target volumes (ITV) were defined as visible lesions on slow CT images (slice thickness 2 mm, 4 s/slice) acquired under shallow breathing using an abdominal compression belt. In determination of the planning target volume (PTV), a margin of 5 mm was added to the contours of the ITV. At our institution, the typical leaf margin of the micro-multileaf collimator was 3 mm. In principle, the dose fractionation schedules for T1 NSCLC lesions were 48 Gy in four fractions at the isocenter, and for T2 NSCLC lesions or metastatic lung tumors, 60 Gy in five fractions were delivered at the isocenter using 4 MV photons.
PET scanning
Patients fasted for 4 h before the intravenous injection of approximately 3.0 MBq/kg body weight of FDG. The serum glucose level immediately before the injection was measured to ensure the value was less than 120 mg/dl. Dual-modality PET-CT imaging was performed using Aquiduo (Toshiba Medical Systems Corporation, Otawara, Japan). The system provides separate CT and PET datasets, which can be accurately fused on an image viewer Vox-Base II (J-MAC System, Inc., Sapporo, Japan). Whole-body CT (Auto-mA(SDN), 120 kV, 2.0 mm × 16, 0.5 s, 512 × 512 matrix size, 30 mm/rotation (HP15), 2- and 4-mm incremental reconstruction) covered a region ranging from the head to the upper thighs. Whole-body PET images with attenuation correction were acquired about 90 min later. The acquisition time of PET was adapted according to the patients’ weight. The time was set to 120 s per field of view, 500 mm, for patients up to 50 kg body weight, to 150 s for those with 50–75 kg body weight, to 180 s for those with 75–100 kg body weight. PET images were scatter corrected and iteratively reconstructed into a 128 × 128 matrix with 1.34 zooming, using interactive algorithms (ordered-subset expectation maximization, 2 iterations, 14 subsets) and the CT-based attenuation map, and noise was reduced by smoothing the images with a 7-mm full width at half maximum (FWHM) Gaussian filter.
Evaluation and analysis
There were a total of 137 FDG-PET/CT scans acquired from the 59 study patients. FDG-PET/CT was performed pre-SABR to confirm stage I status for 41 patients (43 scans total). The median tumor SUVmax on pre-treatment FDG-PET/CT was 3.7 (range 0.4–15.9). The indication of post-SABR FDG-PET/CT was decided by physician in charge or combined conference, which was not performed routinely, but undergone mainly when tumor recurrence was suspected on clinical evaluation. A total of 94 PET/CT examinations were performed post-SABR because of clinical or imaging concerns for disease progression. Forty-four patients had one PET/CT scan, 18 patients had two PET/CT scans, and 2 patients had three or four scans after SABR, respectively. In most cases, we evaluated which mass-like consolidation was local recurrence or radiation fibrosis, based on clinical courses of the patients, including follow-up CT images, FDG-PET/CT findings, and laboratory data. When we observed a suspicious mass which showed continuous enlargement on two or more follow-up CT after FDG-PET/CT, with or without the elevation of tumor marker or appearance of new lesions, we diagnosed it as local recurrence. Biopsy to confirm local recurrence could not be performed except in 1 patient for their poor lung function. In 7 cases, tumor recurrence was pathologically confirmed by salvage surgery.
For analysis, the PET/CT scans of patients with local failure and no recurrence were divided into four groups according to the length of time between the completion of SABR and the PET/CT scan (Table 2). The intensity and shape of FDG uptake in the lung was evaluated qualitatively and semi-quantitatively.
For the qualitative evaluation, the intensity of FDG uptake was visually assessed using a 3-point scale [12]: 0, none or faint uptake; 1, mild uptake, comparable to that in the blood pool; and 2, moderate to intense uptake, greater than that in the blood pool. The shape of the tracer uptake was categorized as non mass-like or mass-like. The qualitative evaluations were determined by a board-certified radiologist, a nuclear medicine physician, and a board-certified radiation oncologist with consensus on information about elapsed time between SABR and FDG-PET/CT. For the semi-quantitative analysis, we calculated the SUVmax after setting a region of interest (ROI).
Statistical analysis
The relationship between the SUVmax and time after SABR was represented by Pearson’s correlation coefficient. Between the group of tumor recurrence and of radiation fibrosis, the comparisons of post-SABR tumor SUVmax were performed using the Mann–Whitney U test. Logistic regression analysis was performed to assess the significance of qualitative scoring of FDG uptake or SUVmax for local recurrence. The overall predictive ability of these variables was evaluated by use of the area under the receiver operating characteristic (ROC) curve. The sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of each variable in predicting local recurrence were calculated. Statistical analysis was performed with Dr. SPSS II for Windows (Statistical Package for social Sciences, SPSS, Tokyo, Japan) software. All statistical tests were two-sided. The level of statistical significance was set at p < 0.05.
Results
Sixteen of 59 patients had local failure and 34 patients had no recurrence; the outcomes of 9 patients were uncertain. For seven of 9 patients, the diagnosis was difficult because their follow-up duration was less than 12 months, and in 2 cases, since mass-like consolidation was appeared near the primary tumor treated with SABR, distinguishing tumor recurrence from second primary lung cancer was difficult.
In 16 patients diagnosed as having local failure, salvage lung resection for recurrence after SABR was successfully performed in 7 patients, and the mass-like lesion on FDG-PET/CT found to be proven as tumor recurrence. The remaining 9 patients were diagnosed as tumor recurrence without pathological confirmation. Among them, 4 patients experienced apparent continuous tumor enlargement on two or more follow-up CT after suspicion of local recurrence, thus they were clinically determined as local failure. They were treated with re-SABR or conventional radiotherapy after recurrence, but three of them died of continuous tumor progression. Tumor control was obtained in one patient who treated with re-SABR. In 3 patients, in addition to subsequent tumor increase on follow-up CT, tumor markers were elevated at the same duration. Two of them were dead related to lung cancer, whereas one patient who treated with re-SABR was alive without disease. One patient was diagnosed as local failure because of both increase of primary lesion and the mediastinum and the hilar lymph nodes swelling were observed at the same CT scan. In one patient, multiple lung nodules were appeared with enlargement of primary lesion. The latter two patients died of tumor progression.
We evaluated the combination of FDG uptake intensity and shape.
Qualitative evaluation
Table 2 shows the combination of grade of FDG uptake intensity and shape versus time after SABR.
In cases of radiation pneumonitis/fibrosis: the combination of intensity 1 and non mass-like shape uptake was observed in 29 scans (49 %), the range of SUVmax was 1.0–3.2. Intensity 0 and non mass-like shape uptake was in 19 scans (32 %), the range of SUVmax was 1.0–1.8; intensity 2 and non mass-like shape uptake was in 7 scans (12 %), the range of SUVmax was 2.9–3.6; intensity 1 and mass-like shape uptake was in 2 scans (3 %), the range of SUVmax was 1.3–2.5; intensity 2 and mass-like shape uptake was in 2 scans (3 %), the range of SUVmax was 4.2–5.5.
In cases of tumor recurrence: the combination of intensity 2 and mass-like shape uptake was observed in 21 scans (91 %), the range of SUVmax was 2.2–11.2; intensity 0 and non mass-like shape uptake in 1 scan (4 %), with SUVmax of 1.0; intensity 1 and mass-like shape uptake in 1 scan (4 %), with SUVmax of 1.3.
Semi-quantitative evaluation
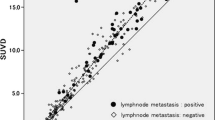
A scatter plot of SUVmax versus time after SABR in cases of radiation pneumonitis/fibrosis was shown in Fig. 1a. A negative correlation was observed between the SUVmax and time after SABR (Pearson’s correlation coefficient = −0.309; p = 0.017).
SUVmax and the time duration between SABR and FDG-PET/CT in cases of radiation pneumonitis/fibrosis. a Scatter plot of SUVmax versus time after SABR showed a negative correlation coefficient of −0.309 (p = 0.017, Pearson’s correlation). b Mean (diamond) and standard deviation (vertical bar) of SUVmax at each time point between SABR and FDG-PET/CT imaging post-SABR. The SUVmax was highest at <6 months, and gradually decreased with time after SABR
In cases of radiation pneumonitis/fibrosis: the SUVmax (mean ± SD) was 2.8 ± 1.4 at <6 months, 2.4 ± 1.0 at 6–12 months, 2.0 ± 0.8 at 12–24 months, and 1.8 ± 0.5 at >24 months. (Fig. 1b).
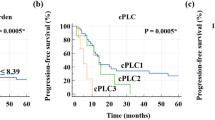
Figure 2 shows changes of the tumor SUVmax in cases of tumor recurrence. The SUVmax of recurrent tumor tended to gradually increase, and at 6–12 months or at 12–24 months, it was significantly higher than the SUVmax of radiation fibrosis (8.0 ± 3.2 vs. 2.1 ± 0.9, p < 0.001, respectively, Mann–Whitney U test).
Correlation between pre-SABR tumor SUVmax and post-SABR tumor SUVmax in cases of local recurrence
Among 16 patients who had local recurrence, 13 patients were studied with FDG-PET/CT before SABR for initial staging. The SUVmax (mean ± SD) was 5.8 ± 4.9 before SABR, and was 8.1 ± 3.4 at diagnosis of recurrence. In patients with pre-SABR tumor SUVmax < 5 (n = 8), all recurrent tumor SUVmax was ≧5 and all higher than each pre-SABR SUVmax.
In 3 cases (marked with asterisks in Table 2), tumor recurrence was diagnosed later, although FDG-PET/CT was performed at early times (2.5, 3.5, and 6.3 months, respectively) after SABR.
In the subgroup of 7 patients with pathologically confirmed local recurrence by salvage surgery, all tumors showed intensity 2 and mass-like FDG uptake and the range of SUVmax was 6.2–12.8 (median 7.5) (Table 3).
For the entire group, both of the combination of intensity 2 and mass-like FDG uptake and SUVmax was significantly associated with local recurrence (OR: 299.4, 95 % CI 50.9–3244.4, p < 0.0001, and OR: 3.22, 95 % CI 2.1–6.1, p < 0.0001, logistic regression). ROC analysis was performed to evaluate the predictive ability of these variables. The area under the curve was 0.94 and 0.90, respectively, which suggests that the value was important to the prediction of local recurrence. The sensitivity and specificity of the combination of intensity 2 and mass-like FDG uptake was 91.3 and 96.6 %, respectively and negative predictive value (NPV) was 96.6 %, positive predictive value (PPV) was 91.3 %. We determined the cutoff value of SUVmax to obtain a reasonable balance of sensitivity and specificity based on the ROC curve; 4.5 of SUVmax acquired a sensitivity of 87 % and specificity of 98.3 %, NPV of 95.1 % and PPV of 95.2 %. In the current study, all recurrent tumors showed the SUVmax > 4.5 at the diagnosis of local recurrence. At 6–12 months after SABR, as for local recurrence, the combination of intensity 2 and mass-like FDG uptake obtained a sensitivity of 100 %, specificity 95 %, NPV of 100 %, and PPV of 88.9 %, respectively. At the same duration, cutoff value of SUVmax = 4.5 had a sensitivity 88.9 %, specificity 94.5 %, and NPV was 95.0 %, PPV was 88.9 %, respectively. As well, at ≧12 months after SABR, these two variables acquired a significant high predictive value of local recurrence, finding sensitivity 100 % and specificity 100 % for both of them.
Figure 3 showed one representative case of tumor recurrence. FDG-PET/CT images at 13 months post-SABR showed intense and mass-like FDG uptake in a consolidation. As local recurrence was strongly suggested, salvage surgery was performed.
A 74-year-old man with metastatic lung cancer from sigmoid colon cancer who underwent SABR with a prescription dose of 60 Gy in five fractions at the isocenter. a SABR treatment planning images with isodose lines show a highly conformal dose distribution to the tumor in the right middle lobe. b CT image at 9 months post-SABR shows a consolidation with volume loss and bronchiectasis. c CT image at 13 months post-SABR shows a mass-like consolidation suggesting tumor recurrence. d FDG-PET/CT image shows a consolidation with intensity 2 and mass-like FDG uptake (the SUVmax = 6.2), strongly suggestive of tumor recurrence. e Salvage surgery was performed for local recurrence after SABR. At cut sections of the right middle lobe, the tumor is outlined in red. f Hematoxylin–eosin (H–E) stains (×20) demonstrated active metastatic adenocarcinoma. g H–E stains (×20) showed obstructed vessels and damaged alveolar cells induced by SABR. h Azan stains (×10) demonstrated that smooth muscles of damaged vessel wall (staining blue) were replaced by fibrosis
CT and FDG-PET/CT images in a case of radiation fibrosis were shown in Fig. 4.
Mass-like consolidation after SABR in a 74-year-old woman with highly suspected of non-small cell lung cancer. a Pretreatment CT image shows a solid mass in the left lower lobe. b Pretreatment FDG-PET/CT image shows intense FDG uptake (SUVmax = 3.2) in the tumor. c CT image at 19 months after SABR shows a mass-like consolidation which is difficult to be differentiated from tumor recurrence. d FDG-PET/CT image shows intensity 0 and non mass-like FDG uptake in the mass-like consolidation suggesting fibrosis rather than tumor recurrence. e Follow-up CT image at 36 months after SABR shows decrease in size of the mass-like consolidation, thus this case is clinically considered as radiation-induced fibrosis
Discussion
Because of comorbidity or higher operative risk, as many as 20 % of stage I NSCLC patients are not candidates for surgery [13]. SABR has become an alternative treatment option in such medically inoperable patients. Today, the indications for SABR have expanded to patients who are functionally operable but refuse surgery [2, 3], or who have pulmonary oligometastatic tumors [11].
Although CT findings suggesting tumor recurrence after SABR have been reported in some studies [9, 14], CT is sometimes limited because radiation fibrosis may develop for at least the first 12 months post-treatment. CT findings may not be reliable in some cases because first consolidations representing radiation-induced inflammation or fibrosis can overlap the tumor and prevent evaluation of local tumor status, and second, the direction of the radiation portal is more complicated and high dose is delivered to the target with minimal dose to the adjacent normal tissues, so the shape of the SABR-induced fibrosis could present as a mass-like lesion. Such a mass-like consolidation can occur at a median post-SABR time of 5 months in 68 % of treated cases [14].
The clinical significance of FDG-PET after conventional radiotherapy for NSCLC has been described [8, 15–17]. In detecting residual or recurrent NSCLC after conventional radiotherapy, FDG-PET demonstrates a sensitivity and specificity of 100 % and 89–92 %, respectively [8]. However, FDG-PET studies after SABR are limited [7, 9, 10, 18].
In a retrospective review of 32 FDG-PET scans from 23 patients who underwent SABR for lung cancer and showed no evidence of local recurrence, Matsuo et al. [12] suggested that the FDG uptake of radiation fibrosis tended to be moderate to intense and well-defined at early times post-SABR, especially within 6 months, and then became faint and ill-defined over the later period. They further suggested that moderate to intense uptake of FDG during the early period does not always mean residual or recurrent tumor, and that usually, the demarcations of FDG uptake to radiation fibrosis were ill-defined [12].
Our present study showed characterization of the FDG uptake pattern both in cases of radiation fibrosis (40 lesions, 59 studies) and tumor recurrence (17 lesions, 23 studies). In cases of radiation fibrosis, the combination of intensity grade 1 and non mass-like shape uptake was most common (49 %) and the range of SUVmax was 1.0–3.2. The combination of intensity grade 0 and non mass-like shape uptake was the second most common (32 %), and the range of SUVmax was 1.0–1.8. The FDG uptake tended to be moderate at early times post-SABR but usually decreased and was non mass-like shape uptake at 12 months and over. Two cases of radiation fibrosis exceptionally showed mass-like FDG uptake over 12 months, but the SUVmax of them was low (SUVmax of 1.3 at 19 months and SUVmax of 2.5 at 37 months, respectively).
By contrast, in cases of tumor recurrence, the combination of intensity grade 2 and mass-like shape uptake was the most common (91 %), and the range of SUVmax was 2.2–11.2. The SUVmax of tumor recurrence after 12 months was significantly higher than that of radiation fibrosis (p < 0.001), and all tumor recurrence in our study showed the SUVmax > 4.5 at the time of diagnosis of local failure.
Matsuo et al. [12] reported that there was no incidence of radiation fibrosis in their study in which the SUVmax was > 5.0 at ≧6 months post-SBRT. Bollineni et al. [10] also concluded that residual FDG uptake (SUVmax ≧ 5.0) 12 weeks after SABR was significantly associated with local failure. However, we encountered one case of radiation fibrosis in which the SUVmax was 5.5 at 9.6 months post-SABR. Similarly, Hoopes et al. [18] reported two patients who had no recurrence but were observed with the SUVmax > 5.0 at 23–26 months. Thus, some false positive FDG uptake could be the result of inflammation. Matsuo et al. suggested that false positive cases demonstrated increased FDG uptake that was linear or wedged shape with an ill-defined margin. In our cases of radiation fibrosis, 3 of 36 FDG-PET/CT studies performed at >12 months showed moderate to intense FDG uptake, but the shape of FDG uptake was not mass-like, which is consistent with the results of them.
In addition, we found that recurrent tumor had moderate to intense and mass-like uptake of FDG at the time of diagnosis of recurrence. Focal intense uptake of FDG on PET image seems to be a useful finding for differentiating tumor recurrence from radiation fibrosis. Fused FDG-PET/CT images may allow the differentiation of metabolically active recurrent tumor from metabolically inactive radiation-induced fibrosis. Absent or faint FDG uptake may have high negative predictive value. FDG-PET/CT allows simultaneous evaluation of morphological and functional changes in the irradiated lesions, and seems to be potentially advantageous over CT or FDG-PET alone.
Huang et al. [7] proposed in their systematic review of radiographic changes after lung SABR, that when SUVmax ≧ 5 recurrence should be highly suspected, and histological exploration should be considered, whereas if the original primary tumor had a low SUV, the recurrent tumor SUVs may be low, therefore in patients with SUVmax < 5 who have suspicious CT findings, biopsy should still be considered. We agree with their proposal approach to patients with equivocal lung changes, but in the current study, 8 cases with a low SUVmax (<5) tumor at pretreatment FDG-PET/CT had a SUVmax ≧ 5 at the recurrence, which is almost all (7 of 8 cases) higher than each pre-SABR SUVmax (Fig. 2). Thus, tumor recurrence was strongly suspected.
Differentiating tumor recurrence from radiation fibrosis is important particularly when salvage treatment after SABR is possible. Although the selection of the best therapy for local failure after SABR is controversial, some recent reports indicate that surgical salvage is feasible [19, 20]. Neri et al. [20] reported that a surgical salvage strategy was feasible for operable patients, and in at least seven patients, the surgery was accomplished without major technical difficulties or increased postoperative morbidity. Chen et al. [19] also reported that during surgical extirpation, no significant SABR-related adhesions were found in any of five evaluated patients. In the present study, we successfully treated 7 patients who underwent salvage lung resection after SABR. They had no significant toxicity and all achieved good local control. Thus, salvage surgery after SABR should be a consideration for operable patients although more investigation is necessary to verify these findings.
There were several limitations in our study. In addition to the short follow-up, limited sample size and the retrospective nature of the study, pathological confirmation both at diagnosis and at tumor recurrence was obtained in only a few cases because of the significant comorbidity and limited lung function of the patients. The diagnosis in most cases was clinically confirmed by serial radiographic findings or increased tumor markers. Recently, Taremi et al. [21] reported that they found no difference in local control or overall survival rates between patients with and without cytologic proof of malignancy, suggesting that our approach for selecting patients for SABR, along with multimodality evaluation, is safe and effective.
To the best of our knowledge, there are currently few studies reporting FDG-PET/CT findings of tumor recurrence after SABR [9, 18]. A prospective study of serial FDG-PET/CT imaging is needed to investigate the potential for differentiating local recurrence from radiation-induced post-SABR changes.
Conclusions
In conclusion, FDG-PET/CT would be an important modality in the management of patients after SABR. The evaluation of both the intensity and shape is useful for distinguishing tumor recurrence from radiation fibrosis after SABR for stage I non-small cell lung cancer and metastatic lung tumor especially at ≧12 months after SABR.
References
Hoyer M, Roed H, Hansen A. Prospective study on stereotactic radiotherapy of limited-stage non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2006;66:S128–35.
Louie AV, Rodrigues G, Hannouf M, Zaric GS, Palma DA, Cao JQ, et al. Stereotactic body radiotherapy versus surgery for medically operable Stage I non-small-cell lung cancer: a Markov model-based decision analysis. Int J Radiat Oncol Biol Phys. 2011;81:964–73.
Onishi H, Shirato H, Nagata Y, Hiraoka M, Fujino M, Gomi K, et al. Stereotactic body radiotherapy (SBRT) for operable stage I non-small-cell lung cancer: can SBRT be comparable to surgery? Int J Radiat Oncol Biol Phys. 2011;81:1352–8.
Aoki T, Nagata Y, Negoro Y, Takayama K, Mizowaki T, Kokubo M, et al. Evaluation of lung injury after three-dimensional conformal stereotactic radiation therapy for solitary lung tumors: CT appearance. Radiology. 2004;230:101–8.
Koenig TR, Munden RF, Erasmus JJ, Sabloff BS, Gladish GW, Komaki R, et al. Radiation injury of the lung after three-dimensional conformal radiation therapy. AJR Am J Roentgenol. 2002;178:1383–8.
Linda A, Trovo M, Bradley JD. Radiation injury of the lung after stereotactic body radiation therapy (SBRT) for lung cancer: a timeline and pattern of CT changes. Eur J Radiol. 2011;79:147–54.
Huang K, Dahele M, Senan S, Guckenberger M, Rodrigues GB, Ward A, et al. Radiographic changes after lung stereotactic ablative radiotherapy (SABR)—can we distinguish recurrence from fibrosis? A systematic review of the literature. Radiother Oncol. 2012;102:335–42.
Inoue T, Kim EE, Komaki R, Wong FC, Bassa P, Wong WH, et al. Detecting recurrent or residual lung cancer with FDG-PET. J Nucl Med. 1995;36:788–93.
Takeda A, Kunieda E, Takeda T, Tanaka M, Sanuki N, Fujii H, et al. Possible misinterpretation of demarcated solid patterns of radiation fibrosis on CT scans as tumor recurrence in patients receiving hypofractionated stereotactic radiotherapy for lung cancer. Int J Radiat Oncol Biol Phys. 2008;70:1057–65.
Bollineni VR, Widder J, Pruim J, Langendijk JA, Wiegman EM. Residual (18)F-FDG-PET uptake 12 weeks after stereotactic ablative radiotherapy for stage I non-small-cell lung cancer predicts local control. Int J Radiat Oncol Biol Phys. 2012;83:e551–5.
Rusthoven KE, Kavanagh BD, Burri SH, Chen C, Cardenes H, Chidel MA, et al. Multi-institutional phase I/II trial of stereotactic body radiation therapy for lung metastases. J Clin Oncol. 2009;27:1579–84.
Matsuo Y, Nakamoto Y, Nagata Y, Shibuya K, Takayama K, Norihisa Y, et al. Characterization of FDG-PET images after stereotactic body radiation therapy for lung cancer. Radiother Oncol. 2010;97:200–4.
Raz DJ, Zell JA, Ou SH, Gandara DR, Anton-Culver H, Jablons DM. Natural history of stage I non-small cell lung cancer: implications for early detection. Chest. 2007;132:193–9.
Matsuo Y, Nagata Y, Mizowaki T, Takayama K, Sakamoto T, Sakamoto M, et al. Evaluation of mass-like consolidation after stereotactic body radiation therapy for lung tumors. Int J Clin Oncol. 2007;12:356–62.
Bury T, Corhay JL, Duysinx B, Daenen F, Ghaye B, Barthelemy N, et al. Value of FDG-PET in detecting residual or recurrent nonsmall cell lung cancer. Eur Respir J. 1999;14:1376–80.
Frank A, Lefkowitz D, Jaeger S, Gobar L, Sunderland J, Gupta N, et al. Decision logic for retreatment of asymptomatic lung cancer recurrence based on positron emission tomography findings. Int J Radiat Oncol Biol Phys. 1995;32:1495–512.
van Loon J, Grutters J, Wanders R, Boersma L, Oellers M, Dingemans AM, et al. Follow-up with 18FDG-PET-CT after radical radiotherapy with or without chemotherapy allows the detection of potentially curable progressive disease in non-small cell lung cancer patients: a prospective study. Eur J Cancer. 2009;45:588–95.
Hoopes DJ, Tann M, Fletcher JW, Forquer JA, Lin PF, Lo SS, et al. FDG-PET and stereotactic body radiotherapy (SBRT) for stage I non-small-cell lung cancer. Lung Cancer. 2007;56:229–34.
Chen F, Matsuo Y, Yoshizawa A, Sato T, Sakai H, Bando T, et al. Salvage lung resection for non-small cell lung cancer after stereotactic body radiotherapy in initially operable patients. J Thorac Oncol. 2010;5:1999–2002.
Neri S, Takahashi Y, Terashi T, Hamakawa H, Tomii K, Katakami N, et al. Surgical treatment of local recurrence after stereotactic body radiotherapy for primary and metastatic lung cancers. J Thorac Oncol. 2010;5:2003–7.
Taremi M, Hope A, Dahele M, Pearson S, Fung S, Purdie T, et al. Stereotactic body radiotherapy for medically inoperable lung cancer: prospective, single-center study of 108 consecutive patients. Int J Radiat Oncol Biol Phys. 2012;82:967–73.
Acknowledgments
This research was supported in part by Grants-in-Aid for scientific research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (Program for Enhancing Systematic Education in Graduate School).
Conflict of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakajima, N., Sugawara, Y., Kataoka, M. et al. Differentiation of tumor recurrence from radiation-induced pulmonary fibrosis after stereotactic ablative radiotherapy for lung cancer: characterization of 18F-FDG PET/CT findings. Ann Nucl Med 27, 261–270 (2013). https://doi.org/10.1007/s12149-012-0682-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-012-0682-4