Abstract
Purpose
To evaluate the usefulness of maximum standard uptake value (max SUV) calculated from F-18 fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) examination and findings from ultrasonographic (US) examination on incidentally detected thyroid FDG uptake on FDG PET/CT.
Materials and methods
We collected and reviewed FDG PET/CT images performed at our institution from March 2005 to March 2008. This study included 190 subjects with increased FDG uptake of thyroid gland who later underwent thyroid US and histological examinations. Of these subjects, the uptake pattern on FDG PET/CT was classified as either diffuse or focal. The FDG uptake pattern, max SUV, and US findings were evaluated and correlated with the histological results.
Results
In the focal FDG uptake pattern cases (n = 148), the mean max SUV of malignant cases was higher than that of benign cases (5.93 ± 5.35 vs. 3.47 ± 2.89). Of the diffuse FDG uptake cases (n = 42), nodules were detected in 25 subjects (59.5%) by US examination. Thyroid nodules were well characterized on US studies, and combined findings of suspicious US features or high max SUV of focal FDG uptake lesion increased sensitivity, PPV, NPV, and accuracy.
Conclusions
Focal uptake pattern and high max SUV may be helpful in differentiating benign and malignant nodules on FDG PET/CT. However, US examination provides further information, and for lesions with increased FDG uptake of thyroid, US examination should be recommended.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As a tool for screening the whole body or for examining metastasis in patients already diagnosed with malignancy or under cancer treatment, the demand for F-18 fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) has increased. While performing FDG PET/CT studies, unexpected thyroid incidentalomas are occasionally detected, and the incidence has been reported ranging from 1.2 to 4.3%, in previous studies [1–5]. In studies reported by Kim et al. [6], who described the incidentaloma as diffuse uptake or focal uptake, the incidences of diffuse FDG uptake and focal FDG uptake were comparable. From several studies, it has been established that in cases in which the incidentaloma appears to be focal on PET images, malignant nodules are frequent [1–6]. Some authors believed that the diffuse FDG uptake of thyroid gland might be a normal variant, or a finding highly indicative of chronic thyroiditis [6–10]. In addition, the fact that high-resolution ultrasonography makes detection of nonpalpable thyroid nodules possible and has a potential role in the differentiation of benign from malignant lesions is known [11–14].
Therefore, establishing diagnostic guidelines for unexpected thyroid uptake lesions discovered on FDG PET/CT would be of use in clinical practice. We evaluated the ability of the FDG uptake pattern and, max SUV to differentiate benign from malignant lesions. Also, we assessed the usefulness of ultrasonographic (US) examinations for evaluation of incidental FDG uptake noted on FDG PET/CT.
Materials and methods
Materials
This study was performed in accordance with all regulations of our hospital’s Institutional Review Board. All subjects (n = 12840) who underwent FDG PET/CT examination for preventive health screening or for the examination of tumors in areas other than thyroid gland from March 2005 to March 2008 were reviewed retrospectively. 1151 of 12840 subjects showed increased FDG uptake of thyroid gland on FDG PET/CT images. Of these subjects, only the 190 subjects who had histological results were included in this study. They consisted of 46 males and 144 females, with a mean age of 56 years.
FDG PET/CT evaluation
For the FDG PET/CT examination, Biograph LSO (Siemens Medical Solutions; Knoxville, TN, USA) integrated with a dual-section helical CT scanner (Somatom Emotion; Siemens) was used. All subjects fasted for at least 6 h (blood glucose level <130 mg/dL) before their FDG PET/CT examinations. Image acquisition for the whole body scan started about 60 min after the intravenous administration of 550 MBq of F-18 FDG. Whole body emission scans consisted of 7–8 bed positions for 2 min at each position.
All FDG PET/CT images were analyzed by two experienced nuclear medicine physicians. Given the physiological distribution of FDG, uptake areas were identified as abnormal if the accumulation of FDG was higher than that of the contralateral thyroid gland or surrounding soft tissue. However, faint FDG uptake in bilateral thyroid glands, which was often higher than uptake in the surrounding muscles or soft tissues, may be physiological. Nakamoto et al. [10] reported normal FDG uptake in head and neck and found that SUV mean in normal thyroid uptake was 1.31 ± 0.30 in 78 subjects. So, faint, uniform, and SUV less than 1.3 in bilateral thyroid glands should be considered as physiological uptake, and was excluded from consideration in this study. The abnormal FDG uptake on FDG PET/CT images was classified to have either a diffuse or focal uptake pattern. Cases showing homogenous uptake in both thyroid lobes were defined as diffuse, and cases only showing uptake in a part of one thyroid lobe were defined as focal. Focal uptake with underlying diffuse uptake was considered as focal uptake. The maximum standard uptake values (max SUVs) were measured in the FDG uptake areas. In addition, nodules detected on noncontrast CT portion from FDG PET/CT were evaluated for size, attenuation, presence of calcification within the thyroid lesion, and presence of concomitant abnormal cervical lymph nodes on PET/CT images. Even rim calcification surrounding a nodule was separately noted.
Ultrasonographic evaluation
Two experienced radiologists performed US examinations. Thyroid US examination was performed with an 8 MHz linear transducer (Siemens; SEQUOIA 512; Acuson Corporation; Mountain View, CA, USA).
Thyroid nodules satisfying any one of the following conditions were classified as malignant: (1) marked hypoechogenicity (cases with noticeably lower echogenicity than the strap muscle), (2) tall or irregular shape, (3) spiculated or ill-defined margin, and (4) micro- or macro-calcification within the nodule. Cases that did not satisfy any of those four criteria were considered as benign nodules on US examinations [11–16].
Histological evaluation
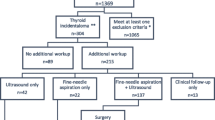
At our institution, we usually perform fine needle aspiration biopsy of a solitary nodule with FDG uptake on FDG PET/CT. In cases of multiple nodules, the nodules with the highest FDG uptake and suspiciously malignant appearance on US examination are confirmed. In cases of diffuse FDG uptake, the nodules with suspiciously malignant appearance on US examination are confirmed. As no suspiciously malignant appearance was observed on US examination in any of the diffuse FDG uptake cases, in practice biopsy was done only of the largest nodule of the subject (Fig. 1).
Histological results were obtained by ultrasonography-guided fine needle aspiration for all cases showing focal uptake on FDG PET/CT and nodules detected by US examination. In one case, a nodule showing focal uptake on FDG PET/CT was not detected by US examination and a lobectomy was later performed.
Fine needle aspiration on the nodule was performed, and histological results were obtained for cases showing diffuse uptake on FDG PET/CT and nodules present on US examination. For 17 cases without definite nodular lesions, fine needle aspiration was performed from focal hypoechoic areas in 12 cases, total thyroidectomy was performed due to the increased size of the thyroid in 2 cases, lobectomy was done in 2 cases, and excisional biopsy was performed in 1 case.
Statistical analysis
Receiver operating characteristic (ROC) analysis was performed to determine the optimal SUV threshold. The FDG PET/CT results (positive vs. negative), based on each SUV threshold, were compared with the pathological findings to identify the true-positive, true-negative, false-positive, and false-negative rates. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy were calculated for each SUV threshold. The US results (positive vs. negative) were compared with the pathological findings and FDG PET/CT. We performed a logistic regression analysis to calculate the probability of positivity based on SUV using SAS (ver. 8.0). Also, by comparing the area under the curve (AUC) of the ROC analysis for FDG PET/CT and ultrasonography, we determined the diagnostic accuracy. The mean max SUV of each group and CT findings of FDG PET/CT were compared by T-test. P values less than or equal to 0.05 were considered significant. Numerical data were expressed as mean ± SD.
Results
Among all 12840 subjects who received FDG PET/CT examinations from 1 March 2005 to 1 March 2008, for preventive health screening or to assess tumors, 1151 (9%) subjects showed increased thyroid uptake. Diffuse thyroid uptake was seen in 539 (4.2%) subjects, and focal FDG uptake in 612 (4.8%) subjects. Of them, 12 subjects with faint FDG uptake and 53 subjects with known thyroid cancer were excluded. 714 subjects without further US examination and 170 subjects without histopathologic results were also excluded. Twelve subjects with mismatched location of the nodules on FDG PET/CT and US were similarly excluded from this study. The details of the patient selection process are shown in a flow chart (Fig. 1). So, the final study population consisted of 190 nodules of 190 subjects with thyroid uptake on FDG PET/CT who were further evaluated by both US and histological examinations.
FDG PET/CT results
In the 42 diffuse FDG uptake cases, the histology was benign in 40 cases and malignant in 2 cases. In the 148 focal FDG uptake cases, the histology was benign in 93 and malignant in 55. The range and mean of max SUV are shown in Table 1 for the diffuse and focal uptake areas. Mean max SUV of malignant nodules showing the focal uptake pattern was statistically significantly higher than that of benign nodules (P < 0.05) (Figs. 2, 3).
A 44-year-old woman with papillary cancer. a In ultrasonography, the thyroid is not enlarged, and its internal echotexture is normal. There is a 1.5 cm sized oval-shaped marked hypoechoic nodule containing macrocalcifications in the right thyroid lobe. b In FDG PET/CT, focally increased uptake is seen. The max SUV is 16.5. On the CT image, a low attenuating mass containing calcification is seen in the right lobe
The sensitivity, specificity, PPV, NPV and accuracy of the FDG PET/CT depend on the cutoff value of max SUV. When all the diffuse and focal uptake lesions were included and the histological result was considered the gold standard, the max SUV cutoff value of 3.8 yielded sensitivity, specificity, PPV, NPV and accuracy of 59.7, 73.7, 42.3, 81, and 69.5%, respectively. When 4.2 was the cutoff value, sensitivity, specificity, PPV, NPV and accuracy were 50.9, 77.4, 49.2, 78.6, and 69.5% (Table 2). If focal FDG uptake criteria were combined with the max SUV, specificity, PPV, NPV, accuracy were increased, while sensitivity was decreased (Table 2).
A total of 115 nodules, including 69 confirmed benign and 46 confirmed malignant nodules, were also seen in the CT portion of the PET/CT. The size, mean max SUV, attenuation, calcification of nodules and associated cervical lymphadenopathy are shown in Table 3. There was a significant difference in the presence of calcification between benign and malignant nodules (P < 0.05).
Ultrasonographic results
FDG PET/CT results were compared with US results and analyzed.
In cases showing diffuse FDG uptake, 17 cases had no evident nodule on US examination. Among the diffuse uptake cases, nodules that were not detected by FDG PET/CT were detected by US examination in 25 cases (59.5%). There was a solitary nodule in 4 subjects and multiple nodules (2–7) in 21 subjects. Among the multiple nodules, only nodules with suspiciously malignant features or the largest ones were confirmed through fine needle aspiration in each subject. Benign features were seen in 20 cases and malignancies were suspected in the other 5 cases on US examination. In 2 of the 5 cases, the histological results were malignancies (Fig. 4).
A 44-year-old woman with diffuse uptake on FDG PET/CT and malignant nodule on ultrasonography; papillary cancer was confirmed. a In ultrasonography, the thyroid is not enlarged, and its internal echotexture is normal. There is a 0.6 cm sized irregular shaped markedly hypoechoic nodule containing microcalcifications in the left thyroid lobe, suggesting malignancy. b In FDG PET/CT, diffusely increased uptake is seen. The max SUV is 6.5
In cases showing a focal uptake pattern, one case did not show evidence of a nodule on ultrasonography, and the absence of malignancy was confirmed following lobectomy. Of the 96 cases with benign US findings in the area coinciding with the focal FDG uptake, the histological examination results were benign in 87 subjects and malignant in 9 subjects. Of the 52 cases with US results suggesting malignancy of the focal FDG uptake, the histology was malignancy in 47 and benign in 5 subjects.
The sensitivity, specificity, PPV, NPV and accuracy of ultrasonography were 84.2, 94, 85.7, 93.3 and 91.1%, respectively.
Combination of FDG PET/CT and ultrasonographic results
Combining the findings of FDG PET/CT and US examination, and considering the positive case when either one of the two examinations was suspicious for malignancy, the sensitivity, specificity, PPV, NPV and accuracy were 96.5, 68.4, 56.7, 97.9 and 76.8%, respectively when applying 3.8 as the cutoff value of max SUV in FDG PET/CT, and 94.7, 71.4, 58.7, 96.9 and 78.4%, when using 4.2 as the cutoff value (Table 2). Also in the case of US suspicious findings combined with high max SUV of only focal uptake lesions, the specificity, PPV, NPV and accuracy were increased (Table 2).
Discussion
FDG PET/CT has been used to determine the presence or absence of metastasis in cancer patients as well as for the purpose of cancer screening examination in healthy patients, and the frequency of its use is increasing. The incidence of thyroid incidentalomas detected by FDG PET/CT is increasing in parallel, and several studies on increased FDG uptake of thyroid gland have been reported [1–5]. In our study, the frequency of thyroid uptake was 9%, which is higher than in other reports (1.2–4.3%) [1–5]. The higher frequency of our study is attributed to the fact that we included a relatively large number of diffuse uptake lesions, unlike other studies.
In the present study, the overlapping range of benign and malignant lesions was wide as shown in Table 1. But the mean max SUV of malignant lesions was statistically higher than that of benign lesions in the focal uptake cases. The sensitivity, specificity, PPV, NPV, and accuracy of FDG PET/CT were dependent on the cutoff value of max SUV: when a lower cutoff value was selected, higher sensitivity was present. So, to improve the sensitivity, we selected a cutoff value of 3.8 for the diagnostic process (Figs. 5, 6). In the CT portion of PET/CT, some nodules were not detected. According to a report of Choi et al. [5], very low attenuation is useful in differentiation. In contrast, only calcification was useful in differentiating benign from malignant lesions in our study. Further evaluation is needed about the significance of CT portion of PET/CT.
The sensitivity, specificity, PPV, NPV and accuracy of ultrasonography were higher than those of FDG PET/CT. However, in our study, US examinations were only evaluated in cases with diffuse or focal FDG uptakes on the FDG PET/CT images. The US results might have been different if the US examination had been performed independently of the PET/CT findings. It is worth noting that in one of our cases, a matching nodule to focal uptake lesion on FDG PET/CT could not be identified by ultrasonography. US examinations have known limitations such as operator dependency and subjectivity, but the max SUV of FDG PET/CT can be an objective, numerical value for evaluating thyroid lesions. Some authors believe that several factors should be considered in the decision process for subjects with thyroid incidentalomas that are identified with PET examinations [1].
Since the SUV of the benign diffuse uptake lesions (3.8) was slightly higher than that of the benign nodules with focal uptake (3.47), in diffuse FDG uptake cases, the high uptake levels may mask an internal focal uptake, justifying a simultaneous US examination. In the present study, of those cases showing a diffuse uptake pattern, there were 25 cases (59.5%) in which a nodule was not seen on FDG PET/CT but was detected by US examination. Two of the 25 cases were diagnosed as thyroid carcinoma. In some reports, increased FDG uptake mimicked thyroid cancer in subjects with chronic thyroiditis, so differentiation between chronic thyroiditis and malignancy was difficult [7, 17]. US examination is needed for subjects with diffuse uptake in FDG PET/CT.
The first limitation of this study was that the number of diffuse uptake cases in particular was small, because the high probability of diffuse FDG uptake being benign has been recognized by numerous studies and such cases were less likely to be confirmed by histology. The second limitation was that only histologically confirmed lesions were included in this study. In cases of multiple nodules, only nodules with suspiciously malignant features or the largest nodules were confirmed histologically. In addition many nodules showing benign findings on ultrasonography and thus without histological confirmation were excluded from this study. So, the malignancy rate may be higher. An additional limitation was that thyroid lesions that did not show increased uptake on FDG PET/CT were excluded regardless of the CT portion findings. Therefore, to see whether FDG PET/CT is useful as a screening test for thyroid cancer, a detailed investigation is required.
The first conclusion of our study is that histological examination is not required for cases with both diffuse uptake on FDG PET/CT and no evident nodule by US examination. Second, cases showing focal uptake on FDG PET/CT always require US examination or ultrasonography-guided fine needle aspiration biopsy. Finally, US examination and max SUV of FDG PET/CT have complementary roles: if the max SUV is elevated in focal uptake lesions on FDG PET/CT images or features of malignancies are seen on ultrasonography, then malignancy is possible and ultrasonography-guided fine needle aspiration biopsy should be considered. From these conclusions (Fig. 5), we recommend a diagnostic process for evaluation of the incidental thyroid uptake lesions noted on FDG PET/CT (Fig. 6).
References
Cohen MS, Arslan N, Dehdashti F, Doherty GM, Lairmore TC, Brunt LM, et al. Risk of malignancy in thyroid incidentalomas identified by fluorodeoxyglucose-positron emission tomography. Surgery. 2001;130:941–6.
Kang KW, Kim SK, Kang HS, Lee ES, Sim JS, Lee IG, et al. Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for metastasis evaluation and cancer screening in healthy subjects. J Clin Endocrinol Metab. 2003;88:4100–4.
Chen YK, Ding HJ, Chen KT, Chen YL, Shen YY, et al. Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for cancer screening in healthy subjects. Anticancer Res. 2005;25:1421–6.
Yi JG, Marom EM, Munden RF, Truong MT, Macapinlac HA, Gladish GW, et al. Focal uptake of fluorodeoxyglucose by the thyroid in patients undergoing initial disease staging with combined PET/CT for non-small cell lung cancer. Radiology. 2005;236:271–5.
Choi JY, Lee KS, Kim HJ, Shim YM, Kwon OJ, Park KC, et al. Focal thyroid lesions incidentally identified by integrated 18F-FDG PET/CT: clinical significance and improved characterization. J Nucl Med. 2006;47:609–15.
Kim TY, Kim WB, Ryu JS, Gong GY, Hong SJ, Shong YK. 18F-fluorodeoxyglucose uptake in thyroid from positron emission tomography (PET) for evaluation in cancer patients: high prevalence of malignancy in thyroid PET incidentaloma. Laryngoscope. 2005;115:1074–8.
Yasuda S, Shohtsu A, Ide M, Takagi S, Takahashi W, Suzuki Y, et al. Chronic thyroiditis: diffuse uptake of FDG at PET. Radiology. 1998;207:775–8.
Shreve PD, Anzai Y, Wahl RL. Pitfalls in oncologic diagnosis with FDG PET imaging: physiologic and benign variants. Radiographics. 1999;19:61–77.
Gordon BA, Flanagan FL, Dehdashti F. Whole-body positron emission tomography: normal variations, pitfalls, and technical considerations. AJR Am J Roentgenol. 1997;207:775–8.
Nakamoto Y, Tatsumi M, Hammound D, Cohade C, Osman MM, Wahl RL. Normal FDG distribution patterns in the head and neck: PET/CT evaluation. Radiology. 2005;234:879–85.
Kim EK, Park CS, Chung WY, Oh KK, Kim DI, Lee JT, et al. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol. 2002;178:687–91.
Jeh SK, Jung SL, Kim BS, Lee YS. Evaluating the degree of conformity of papillary carcinoma and follicular carcinoma to the reported ultrasonographic findings of malignant thyroid tumor. Korean J Radiol. 2007;8:192–7.
Frates MC, Benson CB, Charboneau JW, Cibas ES, Clark OH, Coleman BG, et al. Society of Radiologists in Ultrasound. Management of thyroid nodules detected at US. Radiology. 2005;237:794–800.
Koike E, Noguchi S, Yamashita H, Murakami T, Ohshima A, Kawamoto H, et al. Ultrasonographic characteristics of thyroid nodules. Arch Surg. 2001;136:334–7.
Kang HW, Chung JH, Min YK, Lee MS, Lee MK, Yang JU, et al. Prevalence, clinical and ultrasonographic characteristics of thyroid incidentalomas. Thyroid. 2004;14:29–33.
Khoo ML, Asa SL, Witterick IJ, Freeman JL. Thyroid calcification and its association with thyroid carcinoma. Head Neck. 2002;24:651–5.
Schmid DT, Kneifel S, Stoeckli SJ, Padberg BC, Merrill G, Goerres GW. Increased 18F-FDG uptake mimicking thyroid cancer in a patient with Hashimoto’s thyroiditis. Eur Radiol. 2003;13:2119–21.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kang, B.J., O, J.H., Baik, J.H. et al. Incidental thyroid uptake on F-18 FDG PET/CT: correlation with ultrasonography and pathology. Ann Nucl Med 23, 729–737 (2009). https://doi.org/10.1007/s12149-009-0299-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-009-0299-4