Abstract
Caspase 14 is one of the latter discovered members of the caspase enzyme family and, although sharing sequence homologies with the other caspases, it is not involved in apoptosis. Together with its co-factor filaggrin, it plays an important role in skin barrier formation. It is already known that caspase 14 proteins are reduced during neoplastic dedifferentiation in cervical intraepithelial neoplasms and in invasive cervical carcinomas. Oral squamous carcinoma tissues have not been systematically evaluated for caspase 14 expression yet. Formalin-fixed and paraffin-embedded samples from oral squamous carcinomas (n = 36 tumours from 34 patients), metastases (n = 15) and controls (leukoplakia, n = 10) were analysed by immunohistochemistry. In carcinomas, human papilloma virus (HPV) infection was tested by PCR. Here we demonstrate that, in oral epithelia, caspase 14 is expressed mainly by cells of the intermediate and superficial cell layers while filaggrin is expressed only in keratinising foci in leukoplakia. Caspase 14 and filaggrin are co-localised. In invasive oral carcinomas, reduced expression of caspase 14 was detectable in 47 % of tumours but was not associated with keratinisation, tumour differentiation or HPV infection. Filaggrin was detectable in a subfraction of tumours (56 %) and was restricted to keratinising areas of the carcinomas. In summary, in contrast to cervical carcinomas, partial loss of caspase 14 is not associated with dedifferentiation in neoplastic lesions of the oral mucosa or HPV infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Caspases are a protein family which are major mediators of apoptosis. After exogenous or endogenous induction of apoptosis, inactive cytoplasmic pro-caspases are cleaved and activated in a cascade which transmits the signal for initiation of cell death to the nucleolus. This leads finally to degradation of DNA and disintegration of the cell. One exemption is 19p13.1-encoded caspase 14 which shares homologies with other caspases but is not involved in apoptosis, e.g. activation of other caspases during apoptosis does not include activation of caspase 14 in the cell death signal cascade [1]. It was found to be expressed in epithelial cells and is associated with differentiation. The tissue which mainly expresses caspase 14 is the skin (epidermal cells and hair follicles) and the protein can also be detected in the choroid plexus, the retinal pigment epithelium and thymic Hassall’s bodies but also in placenta trophoblast cells where caspase 14 is involved in trophoblast differentiation [2–5]. In the skin, in addition to caspase 14, apoptosis-associated caspases 1–4 and 6–10 are expressed [6]. In proliferating cells, caspase 14 expression is decreased while induction of terminal differentiation of epidermal keratinocytes leads to up-regulation [7, 8]. The expression of pro-caspase/caspase 14 is increased after cell stimulation by vitamin D3 and decreased by vitamin A [9]. Caspase 14-associated transcription factors are GATA binding protein 3 (GATA3), jun proto-oncogene (JUN) as well as nuclear factor of kappa light polypeptide gene enhancer in B-cells 1 (NFKB1) [10, 11]. The production of inactive pro-caspase 14 increases from supra-basal cells of the stratum spinosum to more apical cells of the stratum granulosum and stratum corneum. The basal cell layer shows weak or absent pro-caspase 14 expression. In the granular layer, caspase 14 was found to be associated with the nucleus and in the cytoplasm with the keratohyalin granules and the desmosomes [12]. Caspase 14 is activated in the apical layers where the cells also express the co-factor of caspase 14 filaggrin and cleavage of pro-filaggrin to filaggrin is associated with activated caspase 14 [12, 13]. The functions of caspase 14 and filaggrin are the protection against UVB light and these proteins are also involved in the hydration status of the skin [12, 14–18]. Caspase 14 is involved in degenerative and neoplastic diseases. In line with its regulatory function of filaggrin activation, in patients with atopic dermatitis, active caspase 14 is markedly down-regulated [19]. Loss of glucocorticoid receptor function correlates with the lack of processing of caspase 14 [20].
In epithelial neoplasms, aberrant caspase 14 expression has been shown in cervical carcinoma, breast cancer, lung squamous carcinomas as well as lung adenocarcinomas and colon carcinomas but gene mutations are mainly absent [21–24]. Cancer cell line A431 (epidermoid cancer), OSC2 (oral squamous cancer), HSG (salivary gland cancer) do not express caspase 14 but exogenous expression of caspase 14 led to growth inhibition and reduced the tumorigenicity [25]. In non-keratinising cervical epithelial cells, it has been demonstrated that the apically pronounced expression pattern of caspase 14 is similar to skin epithelial cells and that caspase 14 proteins are reduced during neoplastic basaloid dedifferentiation in cervical intraepithelial neoplasm type I–III (CIN I–III) and in invasive carcinoma [22]. Approximately 80 % of cervical carcinomas mainly lost caspase 14 expression [22]. In a later study, it could be demonstrated that human papilloma virus (HPV)-derived protein E6, a virus known to be associated with development of cervical and oral carcinoma, disrupts terminal skin differentiation and prevents pro-caspase 14 cleavage [26].
Oral squamous carcinoma tissues from patients have not been systematically evaluated for caspase 14 expression. We hypothesised that caspase 14 expression may, similar to CIN, be decreased in squamous intraepithelial neoplasms (SIN) and, similar to cervical carcinoma and oral carcinoma cell line OSC2, lost in invasive oral carcinomas. Furthermore, we analysed the co-expression of filaggrin and tested whether aberrant caspase 14 expression may be associated with HPV infection in oral squamous carcinoma.
Materials and Methods
Study Group
Tumour samples and corresponding resection margins (n total = 36) from a total of 34 patients were included in this study, including three local relapse samples from one patient. In this latter case, after initial diagnosis and resection of a squamous carcinoma of the tongue, the tumour relapsed after seven, nine, 16 and 17 years after initial presentation. Samples from the nine, 16 and 17-year relapses were available for analysis. Carcinomas of all other patients were primary manifestations before radio-/chemotherapy. In 15 patients, metastases from lung (n = 1), skin (n = 1) and lymph nodes (n = 13) were evaluated. For control purposes, non-neoplastic hyperplasias/leukoplakias (n total = 10) from a total of nine patients without simultaneous carcinoma and from one of the carcinoma cases (leukoplakia 2 years after tumour resection) were analysed. Further details are provided in Table 1.
Ethical Background
All samples had been taken as part of standard clinical care. Samples were formalin-fixed and paraffin-embedded (FFPE) and were retrieved from the tissue archive of the Institute of Pathology, Hannover Medical School. The retrospective analysis of these clinical samples, after the diagnosis had been established, was approved by the local Ethics Committee, Hannover Medical School.
Detection of Caspase 14 and Filaggrin
For protein expression analysis, we used ~1 μm FFPE sections. Xylol-deparaffinised sections were pre-treated in an autoclave prior to incubation with antisera: anti-caspase 14 antibody (1:200, monoclonal mouse, clone D-10, Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA), anti-filaggrin antibody (1:100, monoclonal mouse, clone SPM181, GeneTEx, Inc., Irvine, CA, USA), anti-GATA3 antibody (1:200, monoclonal mouse, clone L50-823, Biocare Medical, Concord, CA, USA) and anti-p16 antibody (cyclin-dependent kinase inhibitor 2A, CDKN2A/p16; ready-to-use, monoclonal mouse, Merck KGaA, Darmstadt, Germany). Both antibodies detect the inactive precursor proteins of caspase 14 and filaggrin as well as the active proteins. Both antibodies have been validated in FFPE sections from skin tissue. A ZytoChem-Plus HRP Polymer kit (Zytomed Systems, Berlin, Germany) and DAB (Dako, Glostrup, Denmark) were used for visualisation of immunostaining. Sections were counterstained with haematoxylin.
Immunohistochemistry for caspase 14 and filaggrin was scored semi-quantitatively as described before [27]: 0 (no apparent reaction), 1+ (positivity in <30 % tumour cells), 2+ (positivity in ≥30 % but <60 %), 3+ (positivity in ≥60 %). Intensity of immunostaining was scored as 0 (absent), 1+ (weak), 2+ (intermediate) or 3+ (strong). CDKN2A/p16 was scored as positive if staining pattern was diffuse/confluent and intensity of immunostaining was 2+ or 3+ (Control: HPV16-positive cervix carcinoma).
Analysis of HPV Infection
DNA was extracted from 3–5 10–20-μm-thick FFPE tissue sections from tumour blocks (>80 % carcinoma cells) with the DNeasy kit (Qiagen, Hilden, Germany). The DNA concentration was determined with a Nanodrop 2000 (Thermo Scientific, Wilmington, DE, USA). Per case, 50 ng DNA was analysed with PCR for 32 high- and low-risk HPV (types 6, 11, 16, 18, 31, 33, 35, 39, 42, 44, 45, 51–54, 56, 58, 59, 61, 62, 66–68, 70, 72, 73, 81–84, 90, 91) as previously described [28]. A chip-based LCD Array HPV Kit was used according to the manufacturer’s instructions (Chipron, Berlin, Germany). Samples without HPV-DNA PCR products were classified as negative; the sensitivity of the PCR for all the above-mentioned HPV types is reported by the manufacturer to be 20 virus copies/μg extracted DNA. Cases with PCR products were further analysed on a chip for determination of the particular HPV species. Controls: FFPE tissue-derived DNA from HPV16-positive cervix sample and DNA-free water.
Statistical Analyses
Intensity and percentage of caspase 14 and filaggrin expressing tumour cells were compared according to the following groups: non-/minimal-keratinising versus keratinising carcinomas, histological grade of differentiation, HPV+ versus HPV− cases and primary tumour versus metastasis. Data were statistically analysed with Prism 5.0 (GraphPad Software, San Diego, CA, USA) by applying two-tailed t test (Mann-Whitney test). Median and ranges were calculated with Prism 5.0.
Results
Co-localisation of Caspase 14 and Filaggrin in Oral Hyperkeratotic Lesions
In oral epithelia of resection margins, caspase 14 was expressed mainly by cells of the intermediate cell layer and superficial cells, while positivity of the basal cell layer was variable (Fig. 1). The protein was mainly localised in the cytoplasm and nuclear expression was variably present. Filaggrin was not expressed in oral epithelia but in skin (stratum granulosom and stratum corneum) and hair follicles (in one tumour sample, the adjacent normal skin was evaluable). Immunohistochemistry of the caspase 14-associated transcription factor GATA3 was tested but, in our case, the staining was negative.
Protein expression of caspase 14 and its co-factor filaggrin in oral squamous lesions. a In leukoplakia, caspase 14 is mainly expressed in the suprabasal cell layers and the intensity of protein expression increases from basal to apical. b Site of transition between normal, non-keratinising squamous epithelia without filaggrin expression and leukoplakia with expression of the caspase 14 co-factor filaggrin. Caspase 14 and filaggrin are co-localised in areas of keratinisation (see supplementary Figure 1). c In high-grade dysplasia, caspase 14 expression is not reduced and the baso-apical increase of protein expression is preserved. d In caspase 14-positive carcinoma, the expression pattern mimicked leukoplakia: in caspase 14, expression is increased in keratinising foci, while peripheral carcinoma cells show a weaker expression. e Filaggrin expression was less intense and fewer tumour cells in keratinising foci were positive. f Almost absent caspase 14 expression in a keratinising oral carcinoma. g Keratinising carcinoma without filaggrin expression. Original magnification in all images ×100
In leukoplakia, caspase 14 expression was more intense in the keratinising areas and co-localisation of filaggrin was detected only in these keratinising lesions (supplementary Figure 1).
Expression of Caspase 14 in Oral SIN and Invasive Squamous Carcinomas
In SIN, irrespective of the grade of dysplasia, a general reduction or loss of caspase 14 was not observed (Fig. 1). Similar to leukoplakias, filaggrin was expressed only in superficial keratinising areas but not in other cells.
In invasive carcinomas, caspase 14 was expressed in most cases in a pattern similar to that in oral epithelia with reactive changes (Fig. 1): the pseudo-basaloid cells were mainly negative while the intensity increased in the pseudo-superficial keratinised cells and caspase 14 accumulated mainly in areas of keratinisation. The proteins were localised mainly in the cytoplasm and partially in the nucleus. Prominent translocation in the nucleus and loss of cytoplasmic accumulation was observed in two G3 and one G2 tumours (supplementary Figure 2). Three local relapses of squamous carcinoma were evaluated in one case and caspase 14 expression and filaggrin was not detectable at all times.
The intensity and the quantity of positive tumour cells varied. None of the carcinomas was completely negative and at least focal caspase 14 expression in the minority of cells was detectable, in particular in four cases with <10 % caspase 14-positive tumour cells. In general, in 16/34 tumours (47 %), >70 % carcinoma cells were negative and these cases were classified as having an incomplete loss of caspase 14 expression. Histopathological characteristics (non-/minimal-keratinising versus keratinising carcinomas, histological grade of differentiation) were not associated with intensity of caspase 14 expression or percentage of positive tumour cell fraction (Table 2; supplementary Figure 3). A link of caspase 14 expression to disease-free survival could not be found (supplementary Figure 3).
Filaggrin was detectable in a subfraction of tumours (n = 15/34, 44 %) but protein expression was restricted to small foci of keratinisation. Filaggrin was detectable in most tumours in <10 % of tumour cells (n = 16/34, 47 %) and only in few cases in 10–50 % of tumour cells (n = 3/34, 9 %). Keratinisation per se was not strictly associated with filaggrin expression and from 19/34 carcinomas with overt keratin deposition 7/19 (37 %) were negative (Fig. 1; Table 2). Caspase 14 positivity/negativity correlated only in a subfraction of carcinomas with filaggrin positivity/negativity, e.g. in five carcinomas with strong caspase 14 expression (immunostaining grade 3+), three showed focal filaggrin expression (1+ and 2+) while the other two were filaggrin-negative.
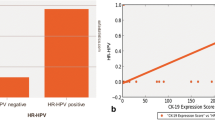
HPV is not Associated with Reduced Caspase 14 Expression in Oral Squamous Carcinomas
HPV was tested by PCR and two carcinoma samples showed HPV-PCR products (n = 2/34; 3 %), a result which corresponds to other findings [29]. Sub-typing of HPV by chip assay showed HPV 16 in both cases and CDKN2A/p16 was strongly expressed in tumour cells (diffuse and confluent staining pattern; supplementary Figure 4). In one of these two cases, 40 % of carcinoma cells were strongly immuno-positive for caspase 14 while the other case showed weak staining in 10 % carcinoma cells.
Similar Expression of Caspase 14 Expression in Primary Oral Tumour and Metastasis
Comparison of primary carcinomas with metastasis revealed a similar caspase 14 expression pattern in most cases (supplementary Table 1, supplementary Figure 2). Expression of caspase 14 in primary carcinoma but loss of caspase 14 in metastasis was observed in 4/15 (26 %) cases; in all four cases filaggrin was co-expressed in the primary tumour but was expressed in only 2/4 metastasis.
In cases with keratinisation-associated caspase 14 accumulation, metastatic cells also accumulated caspase 14 in keratinising areas and, in the case with nuclear expression/cytoplasmatic loss in the primary tumour, the metastasis showed the same type of caspase 14 expression. Of note, in lymph node metastasis but also in lymphocytes in the connective tissue of primary carcinomas, the normal lymphocytes were negative for caspase 14 (supplementary Figure 2).
Discussion
Caspase 14 is one of the latter discovered caspase family members and it is remarkable that, although sharing sequence homologies with other caspases, this factor is not involved in apoptosis [1, 6, 12]. For example, in highly proliferating haematopoietic cells which constantly undergo apoptosis and apoptosis-like processes, caspase 3 and caspase 9 but not caspase 14 is expressed [30]. Accordingly, we found no caspase 14 expression in lymphocytes in oral mucosa-associated lymphatic tissue or lymph nodes. Skin pathologies and several cancer types have been investigated earlier [21–24] but neither oral squamous epithelia nor oral squamous cancer has been analysed for the expression of differentiation-associated caspase 14. Similar to skin and normal cervix epithelia [7, 8, 21, 22] we found accumulation of caspase 14 in the apical layers of the oral mucosa while its co-factor filaggrin is not expressed in non-keratinizing oral epithelia. Histopathological changes in terms of leukoplakia are paralleled by increased caspase 14 accumulation and, similar to previous finding [31], we found that filaggrin is now also expressed in the aberrantly keratinizing areas.
An epithelia type similar to oral mucosa is cervix mucosa and in association with progressive dedifferentiation of cervix epithelia to carcinomas caspase 14 expression is lost in most cases [22]. Furthermore, under normal conditions oral squamous cell line OSC2 does not express caspase 14 proteins [25]. Filaggrin expression is maintained in CIN I-III and well differentiated cervix carcinomas but is lost mainly in moderately and poorly differentiated cervix carcinomas [32]. In contrast to most cervix carcinomas and to the in vitro-derived data, we found caspase 14 expression in leukoplakia, SIN and in a considerable fraction of oral squamous carcinomas. While in cervix carcinoma ~80 % cases show a decreased or absent caspase 14 expression [22], in oral squamous carcinomas >50 % of tumours show no complete/partial loss of caspase 14. In this first analysis of metastatic carcinomas, we found that the pattern of caspase 14/filaggrin expression is transmitted in most cases from the primary tumour to its metastasis; in general loss of caspase 14 and filaggrin expression is not characteristic for metastases.
Co-localisation of caspase 14 and filaggrin make it likely that both factors interact in a fashion similar to skin epithelia [12]. In the granular layer of the skin, caspase 14 is localised near the nucleus, keratohyalin granules and desmosomes [12]. In oral epithelia and carcinoma we found a similar protein localisation. In one carcinoma with basaloid phenotype, caspase 14 was restricted to the nucleus but the molecular pathology of this finding remains to be resolved. The proteins accumulated mainly in keratinising areas of the carcinomas and were partially co-localised with filaggrin. Since maintenance of barrier functions are irrelevant for invasive carcinoma cells, caspase 14 and filaggrin expression may be classified as molecular changes secondary to aberrant keratinisation. However, some keratinising carcinomas were mainly negative for caspase 14 or completely negative for filaggrin, which indicates that this caspase and its co-factor are not absolutely necessary for keratin accumulation in neoplastic cells. The related molecular changes which induce reduced expression of these two proteins are mainly unknown. In breast cancer, GATA3 was found to be a caspase 14-associated transcription factor [10] while in oral squamous carcinomas GATA3 could not be detected. Therefore, other factors, such as JUN or NFKB1, which are known to be expressed in oral cancer, might be involved in regulation of caspase 14 expression [11, 33, 34]. In oral squamous cell lines, increased expression of the NFKB1-related inhibitor conserved helix-loop-helix ubiquitous kinase (CHUK; synonym inhibitor of NFKB1, kinase alpha) is associated with reduced filaggrin expression and dedifferentiation in vitro [35]. We found no correlation with differentiation in oral squamous carcinomas in situ, neither for caspase 14 nor for its co-factor filaggrin. Furthermore, we have tested whether HPV infection might be the basis of partial loss of caspase 14 in oral cancer since HPV-encoded proteins can interfere with caspase 14 homeostasis in the skin [26] but in oral squamous carcinomas no link was found.
In summary, caspase 14 accumulates in oral mucosa in the superficial layers and filaggrin expression is restricted to keratinizing foci in leukoplakia. In oral carcinomas the pattern of caspase 14 and filaggrin expression mimic the pattern in leukoplakia. In contrast to cervical carcinomas, partial or total loss of caspase 14 is not associated with dedifferentiation in neoplastic lesions of the oral mucosa or HPV infection.
References
Van de Craen M, Van Loo G, Pype S, Van Criekinge W, Van den brande I, Molemans F, Fiers W, Declercq W, Vandenabeele P. Identification of a new caspase homologue: caspase-14. Cell Death Differ. 1998;5:838–46.
Kuechle MK, Predd HM, Fleckman P, Dale BA, Presland RB. Caspase-14, a keratinocyte specific caspase: mRNA splice variants and expression pattern in embryonic and adult mouse. Cell Death Differ. 2001;8:868–70.
Alibardi L, Tschachler E, Eckhart L. Distribution of caspase-14 in epidermis and hair follicles is evolutionarily conserved among mammals. Anat Rec A Discov Mol Cell Evol Biol. 2005;286:962–73.
Kam DW, Charles AK, Dharmarajan AM. Caspase-14 expression in the human placenta. Reprod Biomed Online. 2005;11:236–43.
White LJ, Declercq W, Arfuso F, Charles AK, Dharmarajan AM. Function of caspase-14 in trophoblast differentiation. Reprod Biol Endocrinol. 2009;7:98.
Raymond AA, Méchin MC, Nachat R, Toulza E, Tazi-Ahnini R, Serre G, Simon M. Nine procaspases are expressed in normal human epidermis, but only caspase-14 is fully processed. Br J Dermatol. 2007;156:420–7.
Wu M, Kodani I, Dickinson D, Huff F, Ogbureke KU, Qin H, Arun S, Dulebohn R, Al-Shabrawey M, Tawfik A, Prater S, Lewis J, Wataha J, Messer R, Hsu S. Exogenous expression of caspase-14 induces tumor suppression in human salivary cancer cells by inhibiting tumor vascularization. Anticancer Res. 2009;29:3811–8.
Hsu S, Yamamoto T, Borke J, Walsh DS, Singh B, Rao S, Takaaki K, Nah-Do N, Lapp C, Lapp D, Foster E, Bollag WB, Lewis J, Wataha J, Osaki T, Schuster G. Green tea polyphenol-induced epidermal keratinocyte differentiation is associated with coordinated expression of p57/KIP2 and caspase 14. J Pharmacol Exp Ther. 2005;312:884–90.
Lippens S, Kockx M, Denecker G, Knaapen M, Verheyen A, Christiaen R, Tschachler E, Vandenabeele P, Declercq W. Vitamin D3 induces caspase-14 expression in psoriatic lesions and enhances caspase-14 processing in organotypic skin cultures. Am J Pathol. 2004;165:833–41.
Asselin-Labat ML, Sutherland KD, Vaillant F, Gyorki DE, Wu D, Holroyd S, Breslin K, Ward T, Shi W, Bath ML, Deb S, Fox SB, Smyth GK, Lindeman GJ, Visvader JE. Gata-3 negatively regulates the tumor-initiating capacity of mammary luminal progenitor cells and targets the putative tumor suppressor caspase-14. Mol Cell Biol. 2011;31:4609–22.
Ballaun C, Karner S, Mrass P, Mildner M, Buchberger M, Bach J, Ban J, Harant H, Tschachler E, Eckhart L. Transcription of the caspase-14 gene in human epidermal keratinocytes requires AP-1 and NFkappaB. Biochem Biophys Res Commun. 2008;371:261–6.
Denecker G, Ovaere P, Vandenabeele P, Declercq W. Caspase-14 reveals its secrets. J Cell Biol. 2008;180:451–8.
Eckhart L, Tschachler E. Cuts by caspase-14 control the proteolysis of filaggrin. J Invest Dermatol. 2011;131:2173–5.
Bergeron L, Gondran C, Oberto G, Garcia N, Botto JM, Cucumel K, Dal Farra C, Domloge N. Skin presenting a higher level of caspase-14 is better protected from UVB irradiation according to in vitro and in vivo studies. J Cosmet Dermatol. 2012;11:111–21.
Denecker G, Hoste E, Gilbert B, Hochepied T, Ovaere P, Lippens S, Van den Broecke C, Van Damme P, D’Herde K, Hachem JP, Borgonie G, Presland RB, Schoonjans L, Libert C, Vandekerckhove J, Gevaert K, Vandenabeele P, Declercq W. Caspase-14 protects against epidermal UVB photodamage and water loss. Nat Cell Biol. 2007;9:666–74.
Hoste E, Kemperman P, Devos M, Denecker G, Kezic S, Yau N, Gilbert B, Lippens S, De Groote P, Roelandt R, Van Damme P, Gevaert K, Presland RB, Takahara H, Puppels G, Caspers P, Vandenabeele P, Declercq W. Caspase-14 is required for filaggrin degradation to natural moisturizing factors in the skin. J Invest Dermatol. 2011;131:2233–41.
Sandilands A, Sutherland C, Irvine AD, McLean WH. Filaggrin in the frontline: role in skin barrier function and disease. J Cell Sci. 2009;122:1285–94.
Aho S, Harding CR, Lee JM, Meldrum H, Bosko CA. Regulatory role for the profilaggrin N-terminal domain in epidermal homeostasis. J Invest Dermatol. 2012. doi:10.1038/jid.2012.174.
Yamamoto M, Kamata Y, Iida T, Fukushima H, Nomura J, Saito M, Tajima M, Okubo Y, Momoi T, Tsuboi R, Hibino T. Quantification of activated and total caspase-14 with newly developed ELISA systems in normal and atopic skin. J Dermatol Sci. 2011;61:110–7.
Bayo P, Sanchis A, Bravo A, Cascallana JL, Buder K, Tuckermann J, Schütz G, Pérez P. Glucocorticoid receptor is required for skin barrier competence. Endocrinology. 2008;149:1377–88.
Koenig U, Sommergruber W, Lippens S. Aberrant expression of caspase-14 in epithelial tumors. Biochem Biophys Res Commun. 2005;335:309–13.
Krajewska M, Kim H, Shin E, Kennedy S, Duffy MJ, Wong YF, Marr D, Mikolajczyk J, Shabaik A, Meinhold-Heerlein I, Huang X, Banares S, Hedayat H, Reed JC, Krajewski S. Tumor-associated alterations in caspase-14 expression in epithelial malignancies. Clin Cancer Res. 2005;11:5462–71.
Fang HY, Chen CY, Hung MF, Hsiao YT, Chiang TC, Lin TY, Chang HW, Chow KC, Ko WJ. Caspase-14 is an anti-apoptotic protein targeting apoptosis-inducing factor in lung adenocarcinomas. Oncol Rep. 2011;26:359–69.
Yoo NJ, Soung YH, Lee SH, Jeong EG, Lee SH. Mutational analysis of caspase-14 gene in common carcinomas. Pathology. 2007;39:330–3.
Hsu S, Qin H, Dickinson D, Xie D, Bollag WB, Stoppler H, Pearl H, Vu A, Watkins M, Koehler M, Schuster G. Expression of caspase-14 reduces tumorigenicity of skin cancer cells. In Vivo. 2007;21:279–83.
Kazem S, van der Meijden E, Struijk L, de Gruijl FR, Feltkamp MC. Human papillomavirus 8 E6 disrupts terminal skin differentiation and prevents pro-Caspase-14 cleavage. Virus Res. 2012;163:609–16.
Bockmeyer CL, Maegel L, Janciauskiene S, Rische J, Lehmann U, Maus UA, Nickel N, Haverich A, Hoeper MM, Golpon HA, Kreipe H, Laenger F, Jonigk D. Plexiform vasculopathy of severe pulmonary arterial hypertension and microRNA expression. J Heart Lung Transpl. 2012;31:764–72.
Pilatz A, Altinkilic B, Rusz A, Izykowski N, Traenkenschuh W, Rische J, Lehmann U, Herbst C, Maegel L, Becker J, Weidner W, Jonigk D. Role of human papillomaviruses in persistent and glucocorticoid-resistant juvenile phimosis. J Eur Acad Dermatol Venereol. 2012. doi:10.1111/j.1468-3083.2012.04542.x.
Kristoffersen AK, Enersen M, Kverndokk E, Sunde PT, Landin M, Solheim T, Olsen I, Grinde B. Human papillomavirus subtypes in oral lesions compared to healthy oral mucosa. J Clin Virol. 2012;53:364–6.
Theophile K, Hussein K, Kreipe H, Bock O. Expression profiling of apoptosis-related genes in megakaryocytes: BNIP3 is downregulated in primary myelofibrosis. Exp Hematol. 2008;36:1728–38.
Grosso M, Lentini M, Bellizi De Marco E, Petracca R, Leoncini P, Carrozza G. Immunohistochemical localization of filaggrin in benign and malignant lesions of the human oral mucosa. Basic Appl Histochem. 1990;34:51–8.
Lara C, Serra V, Marzo C, Valcuende F, Castells A, Bonilla-Musoles FM. Immunohistochemical localization of filaggrin in benign, premalignant and malignant cervical tissue. Arch Gynecol Obstet. 1994;255:73–9.
Turatti E, da CostaNeves A, de Magalhães MH, de Sousa SO. Assessment of c-Jun, c-Fos and cyclin D1 in premalignant and malignant oral lesions. J Oral Sci. 2005;47:71–6.
Nakayama H, Ikebe T, Beppu M, Shirasuna K. High expression levels of nuclear factor kappaB, IkappaB kinase alpha and Akt kinase in squamous cell carcinoma of the oral cavity. Cancer. 2001;92:3037–44.
Nakayama H, Ikebe T, Shirasuna K. Effects of IkappaB kinase alpha on the differentiation of squamous carcinoma cells. Oral Oncol. 2005;41:729–37.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Scharenberg, C., Eckardt, A., Tiede, C. et al. Expression of Caspase 14 and Filaggrin in Oral Squamous Carcinoma. Head and Neck Pathol 7, 327–333 (2013). https://doi.org/10.1007/s12105-013-0445-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-013-0445-0