Abstract
Objectives
To examine the feasibility, efficacy, and safety of sustained low-efficiency dialysis (SLED) in hemodynamically unstable, critically ill children.
Methods
Critically ill patients, 1–18 y old with hemodynamic instability (≥ 1 vasoactive drugs) and severe acute kidney injury (AKI) requiring kidney replacement therapy (KRT) in a tertiary care pediatric intensive care unit were prospectively enrolled. Patients weighing ≤ 8 kg or with mean arterial pressure < 5th percentile despite > 3 vasoactive drugs, were excluded. Patients underwent SLED until hemodynamically stable and off vasoactive drugs, or lack of need for dialysis. The primary outcome was the proportion of patients in whom the first session of SLED was initiated within 12 h of its indication and completed without premature (< 6 h) termination. Efficacy was estimated by ultrafiltration, urea reduction ratio (URR), and equilibrated Kt/V. Other outcomes included: changes in hemodynamic scores, circuit clotting, adverse events, and changes in indices on point-of-care ultrasonography and echocardiography.
Results
Between November 2018 and March 2020, 18 patients with median age 8.6 y and vasopressor dependency index of 83.2, underwent 41 sessions of SLED. In 16 patients, SLED was feasible within 12 h of indication. No session was terminated prematurely. Ultrafiltration achieved was 4.0 ± 2.2 mL/kg/h, while URR was 57.7 ± 16.2% and eKt/V 1.17 ± 0.56. Hemodynamic scores did not change significantly. Asymptomatic hypokalemia was the chief adverse effect. Sessions were associated with a significant improvement in indices on ultrasound and left ventricular function. Fourteen patients died.
Conclusions
SLED is feasible, safe, and effective in enabling KRT in hemodynamically unstable children with severe AKI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) affects 30%–40% of patients admitted to the pediatric intensive care units (ICU) and is associated with extended hospital stay and high mortality [1, 2]. Despite consensus on the indications, the optimal modality for kidney replacement therapy (KRT) in critically ill patients remains unclear. Sustained low-efficiency dialysis (SLED) is a form of prolonged intermittent renal replacement therapy (PIRRT) that combines the advantages of intermittent hemodialysis and continuous KRT [3]. Retrospective pediatric studies and clinical trials in adults suggest that SLED is useful and feasible in critically ill patients [4,5,6,7,8,9]. The experience on SLED in children is limited to three retrospective reports on 152 patients from India and Taiwan [4,5,6]. The feasibility and efficacy of SLED in providing KRT to critically ill pediatric patients with severe AKI was prospectively evaluated using objective parameters [10].
Material and Methods
This prospective interventional pilot study was conducted at a single pediatric ICU between November 2018 and March 2020. All critically ill patients in whom dialysis was indicated, were consecutively enrolled. The study protocol was approved by the Institute Ethics Committee. The study report complies with the STROBE (strengthening the reporting of observational studies in epidemiology) statement. Parents or legally authorized representatives provided written informed consent. All patients continued to receive standard care, including antibiotics and nutrition, as per unit protocols.
Consecutive patients, 1–18 y old, admitted to the pediatric ICU and with hemodynamic instability, were eligible if they developed severe AKI (Kidney Disease Improving Global Outcomes, KDIGO stages 2–3) that required dialysis [10]. Hemodynamic instability was defined by the requirement of ≥ 1 vasoactive drugs (dopamine or dobutamine ≥ 10 μg/kg/min, adrenaline or noradrenaline ≥ 0.1 μg/kg/min, or milrinone ≥ 0.25 μg/kg/min) to maintain mean arterial pressure at ≥ 5th percentile and adequate tissue perfusion (capillary refill time ≤ 2 s) [11, 12]. Indications for dialysis included oliguria with fluid overload > 10% or anticipated worsening by ≥ 5%, persistent or worsening metabolic acidosis (standard base deficit > 5 mmol/L), or refractory or significant hyperkalemia (serum potassium > 5.5 mEq/L) [13, 14]. Reasons for ineligibility were body weight ≤ 8 kg, hemodynamic instability despite use of > 3 vasoactive drugs in maximum doses, prior enrollment in the study, anticipated delay of > 12 h in initiating KRT, or physician’s decision to not escalate therapy.
Following written informed consent, eligible children underwent SLED, as described previously and in Supplementary Table S1 [3, 15]. Briefly, SLED was performed using a low-flux hemodialyzer for at least 6 h, at a blood flow rate of 3–5 mL/kg/min, and dialysate flow rate up to twice the blood flow rate, or the minimum possible with the available dialysis machine, Fresenius 4008S ARrt Plus [3, 15]. The circuit was primed whenever extracorporeal volume exceeded 10% of blood volume and/or for anticipated hemodynamic worsening. Packed red blood cells were used for priming when hematocrit was < 21% [3]. Unfractionated heparin or saline flushes were used to maintain circuit patency. SLED was performed daily or on alternate days at physician’s discretion, with ultrafiltration rate ≤ 0.2 mL/kg/min [16]. SLED was discontinued once any of the following endpoints was achieved: (i) clinical improvement enabling hemodynamic stability off vasoactive drugs, such that intermittent hemodialysis was considered safe and feasible; (ii) recovery from AKI such that dialysis was no longer indicated; (iii) clinical deterioration meriting switch to continuous KRT or therapy discontinuation; or (iv) death. While on SLED, doses of medications were modified assuming an estimated glomerular filtration rate (eGFR) of 10–50 mL/min per 1.73 m2 [17, 18].
The primary outcome was the proportion of patients who underwent the first SLED session within 12 h of its indication without premature termination (session length < 6 h). Secondary outcomes, assessed during each session, were: (i) efficacy, as estimated by net ultrafiltration, urea reduction ratio, and equilibrated Kt/V (eKt/V) (Supplementary Table S2); (ii) hemodynamic instability, including changes in vasopressor dependency index, vasoactive–inotropic score and inotrope score (Supplementary Table S2), and occurrence of hypotension requiring discontinuation of ultrafiltration, saline bolus or increase in inotrope/vasopressor dose; (iii) metabolic impact, including serum potassium < 3.5 mEq/L or > 5.5 mEq/L, metabolic acidosis or need for phosphate supplementation; (iv) occurrence of circuit clotting; and (v) changes in inferior vena cava (IVC) diameter and distensibility, B-lines in lung fields, and left ventricle ejection fraction on point-of-care ultrasonography [19,20,21,22,23]. Dialysis adequacy was defined by single pool Kt/V (spKt/V) of ≥ 1.2 per session, weekly eKt/V > 3.9, and/or weekly spKt/V of ≥ 2 [3, 24, 25]. Clinical outcomes, assessed until follow-up at discharge or death, included switch to alternative KRT modality; renal recovery; duration of dialysis; vasopressor use and mechanical ventilation; length of ICU and hospital stay; and mortality at days 7 and 14.
Retrospective series suggest that 10% of sessions of SLED might require premature termination [5, 6]. For an absolute deviation of 10% and 95% confidence level, 35 patients were required to assess the feasibility of performing SLED without premature termination. This pilot study intended to enroll at least 15 patients, thus providing 80% confidence in the estimate.
Information was analyzed using Stata version 14.0 (StataCorp, College Station, TX) and standard statistical tests. Standard deviation scores for anthropometric measures were calculated using WHO AnthroPlus [26]. Data were summarized as proportions (95% confidence interval, CI) and mean ± standard deviation or median (interquartile range, IQR). Kaplan–Meier survival curves estimated time on KRT and patient survival. Univariate analysis was conducted to determine predictors of dialysis adequacy (eKt/V and net ultrafiltration) and mortality.
Results
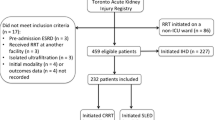
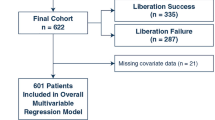
During November 2018 to March 2020, KRT was indicated for 47 episodes of severe AKI in 42 critically ill patients. Twenty-nine episodes were excluded, chiefly for hemodynamic instability despite maximal vasoactive support (n = 14; 48%) (Fig. 1). Eighteen patients were enrolled and underwent 41 sessions of SLED over median (IQR) 2 (2, 4) d. Table 1 shows that the enrolled patients had severe illness, with uniform need for vasoactive drugs (median vasopressor dependency index of 83.2) and predicted mortality of 24.8%. Except 1, all patients were mechanically ventilated; 16 patients had coagulopathy. Except for 1 patient with hemolytic uremic syndrome, AKI was presumably due to acute tubular necrosis, usually associated with sepsis. Fluid overload exceeded 10% in 7 patients and was anticipated to worsen in 6 others. Eight patients were switched to SLED from an alternative modality, following (i) hemodynamic worsening on intermittent hemodialysis (n = 4); (ii) hemodynamic improvement while on continuous KRT (n = 1), and (iii) persistent fluid overload or azotemia despite peritoneal dialysis (n = 3). Seven patients underwent one session of SLED, while 11 patients underwent two or more sessions.
SLED was conducted using temporary vascular access into the internal jugular (n = 11) or femoral (n = 7) vein. Twenty-three (56%) sessions were performed using pediatric blood lines (Fresenius AV set, FMCPaed/Baby R; volume 56 mL). Thirty-nine (95%) sessions were primed with albumin (69.2%) or packed red cells (28.2%). Blood and dialysate flow rates were 3.7 ± 0.6 mL/kg/min and 241 ± 49.9 mL (12.6 ± 6.1 mL/kg) per minute, respectively. Three sessions performed without anticoagulation experienced circuit clots. Two of these sessions required circuit change; no session was terminated prematurely for clotting.
Sixteen of the 18 eligible patients were initiated on SLED within 12 h of its indication. Two patients underwent SLED later than 12 h. The median (IQR) time to initiate SLED from its indication was 4.7 (4, 5.5) h. The mean session length was 6.45 ± 0.68 h; none of the sessions were terminated before 6 h. Thus, SLED was feasible in 16 (89%; 95% CI 67%–97%) cases without premature termination.
Table 2 details the predefined objective measurements of efficacy and safety. The mean ultrafiltration achieved was 26 ± 15 mL/kg. While hemodynamic parameters did not change significantly, 5 (12.2%; 95% CI 5.3%–25.5%) sessions were associated with reversible hypotension. The mean eKt/V was 1.17 ± 0.56, which met adequacy estimates of spKt/V of ≥ 1.2 per session in 18 (43.9%; 29.9%–59%) sessions; weekly spKt/V of ≥ 2 in all (100%; 82.4%–100%) patients; and weekly eKt/V of > 3.9 in 7 (38.9%; 20.3%–61.3%) patients.
Metabolic parameters: One (2.4%) and 7 (17%) sessions were associated with new-onset metabolic acidosis and hypokalemia, respectively (Table 2). These abnormalities persisted in 12 (29.3%; 17.6%–44.5%) sessions each. Levels of blood lactate and standard base deficit did not change significantly.
Point-of-care ultrasonography: IVC parameters were not assessed in seven (17%) sessions in 3 patients due to IVC stent block, and high-frequency oscillatory ventilation and prone ventilation in 1 patient each. Left ventricle ejection fraction and B lines were not assessed in the patient on prone ventilation. Following SLED sessions, there were significant improvements in IVC diameter [median change 0.4 (IQR −2.3, 0.4) mm], IVC distensibility [6.1 (−6.6, 19)%] and left ventricle ejection fraction [7 (0, 16)%]; B lines did not alter significantly. Changes in IVC parameters and left ventricular function correlated with net ultrafiltration (Table 3).
Fourteen patients died, including 5 deaths within 48 h of enrollment and 6 while continued on SLED (Table 4). Ten patients were transitioned to intermittent hemodialysis. Two patients were electively transitioned to continuous KRT after one session each of SLED, at physician’s discretion, one for intermittent hypotension, and another for hyperammonemia associated with an inborn error of metabolism; both patients died subsequently. Seven patients discontinued KRT at median 11 (IQR 5, 30) d (Fig. 1, Fig. S1).
All 22 critically ill patients who were excluded (Fig. 1) were on mechanical ventilation and had sepsis with multiorgan dysfunction. Seven patients died before dialysis initiation, 10 underwent continuous KRT, 2 each received hemodialysis and peritoneal dialysis, and 1 patient weighing < 8 kg underwent SLED. Twenty-one of these patients died.
Survivors differed from those that died after initiating SLED in being younger (median 5.5 y, IQR 2.5–7.5 y, versus 9.6 y, IQR 7.2–13.8 y; p = 0.034). Survivors also had higher ultrafiltration volumes (median 36.8 mL/kg, IQR 30.9–42.3 mL/kg, versus 15.5 mL/kg, IQR 10.2–19.3 mL/kg; p = 0.011) and higher eKt/V for the first session (1.71, 1.36–1.99, versus 1.00, 0.81–1.51; p = 0.044). Based on receiver operating characteristic curves, the threshold value determining survival was 8.4 y for age, 25 mL/kg body weight for ultrafiltration, and 1.63 for eKt/V; however, ultrafiltration was the only significant predictor of survival (Supplementary Table S3, Fig S2). Dialysis adequacy (eKt/V) was related to session length (coefficient 0.37; 95% CI 0.14–0.61; p = 0.003). Ultrafiltration was determined by blood and dialysate flow rates and dialyzer size (Supplementary Table S3).
Discussion
This prospective study on 18 hemodynamically unstable, critically ill patients with severe AKI showed that SLED was feasible in 89% patients within a reasonable time frame. Circuit clotting did not lead to premature discontinuation, despite no anticoagulation in almost half the sessions. Objective parameters demonstrated that the procedure was safe and effective. The illness was severe, as indicated by the near-uniform need for mechanical ventilation and vasoactive agents, comorbidities, and high predicted mortality. In contrast, prior retrospective pediatric series reported fewer patients on vasopressors (43%–70%) and mechanical ventilation (36%–84%), and lower predicted mortality (15%–25%) [4,5,6]. Compared to previous pediatric series, the patients enrolled in the present study were younger (8 y versus 9–15 y) with lower mean weight (22 kg versus 31–54 kg) [4,5,6]. This work extends the feasibility of SLED to younger children with more severe illness than reported previously.
Given the lower cost and complexity and intermittent nature of therapy, SLED has emerged as an alternative to continuous KRT in adult ICU [27, 28]. However, the experience on SLED in children is limited to three reports on 152 patients [4,5,6]. Administering low-efficiency dialysis in children smaller than 20 kg is often limited by the minimum settings for dialysate flow rates (200–300 mL/min) on hemodialysis machines conventionally designed for adults. While this was an important limitation of the present study, previous reports lack precise details on rates delivered in small children [5, 6, 29]. Barring the dialysate flow rates, the authors’ prescription conformed to suggestions on pediatric PIRRT in recent clinical practice guidelines [3]. Other challenges in prescription included the need to prime circuits and the inability to use anticoagulants in patients with coagulopathy.
Similar to previous reports, the chief indication for dialysis in the present study was current or anticipated fluid overload [5, 6], known to correlate strongly with mortality [30, 31]. In contrast to chronic hemodialysis, where ultrafiltration often exceeds 10 mL/kg/h, fluid removal in hemodynamically unstable patients with AKI is limited to ~ 4–5 mL/kg/h despite fluid overload, necessitating prolonged frequent sessions [15]. While the optimal target remains unclear, the present findings suggest that ultrafiltration at ≥ 4 mL/kg/h is well tolerated and predicts survival.
Since hemodialysis in AKI may be underdosed, KDIGO recommends frequent assessment of dialysis adequacy [25]. However, interpretation of Kt/V in critically ill patients is limited by the unpredictable volume of distribution of urea and catabolic state. By accounting for urea regeneration and rebound following dialysis, eKt/V might estimate urea clearance more accurately than spKt/V in such patients. Previous series on pediatric SLED have chiefly reported pre- and postdialysis urea, pH and bicarbonate, and do not inform about Kt/V or the timing of postdialysis assessment [4,5,6]. Solute clearances were assessed as recommended by the PIRRT and KDIGO expert groups, and estimated weekly Kt/V assuming five sessions a week, based on considerations of feasibility and requirements of critically ill patients [3, 24, 25]. The targets for solute clearance in critically ill patients are low, reflecting the concerns of hypokalemia, hypophosphatemia, nutrients losses, and underdosing of antimicrobials and vasopressors [25, 32]. All the present patients achieved Kt/V ≥ 2, as recommended for pediatric PIRRT [3]. Results of univariate regression (Supplementary Table S3) suggest that prolonged SLED achieves higher solute clearance. Dialysis adequacy appeared to relate to patient survival; multivariable analysis was not performed due to the small study size.
Studies report hemodynamic instability in 40%–60% sessions of SLED and up to 50% of those on continuous KRT [33]. Similar to other pediatric reports, 12% of SLED sessions were associated with hypotension [5, 6]. Past studies have reported hemodynamic instability using heterogeneous definitions. All except one study on adults lacked objective assessment, limiting the interpretation and comparability of safety among dialytic modalities [21]. The safety of SLED in sick patients was confirmed using arterial blood pressure monitoring and objective scores to document vasoactive drug requirements.
This prospective study confirms that SLED is feasible and safe in critically ill pediatric patients. The interpretation and impact of the present findings are limited by the small study size, high mortality, single-center design, and lack of comparator group. Continued performance of daily SLED was limited by mortality, often within days of enrolling, which was not unexpected in patients with high predicted mortality at admission. The inability to lower dialysate flow rates appropriately in smaller children highlights the challenges in prescribing SLED in young patients at the centers lacking appropriate hemodialysis equipment. The strengths of this report include a prospective design, inclusion of a homogenous group of critically ill hemodynamically unstable patients, and the use of objective criteria to assess dialysis adequacy, hemodynamic parameters, intravascular fluid compartment, and cardiac function.
Conclusion
This prospective pilot study indicates the feasibility of SLED in critically ill pediatric patients with severe AKI. This procedure offers a safe modality of KRT in patients with multiorgan dysfunction who require mechanical ventilation and/or vasopressor support, and have high predicted mortality.
References
Mehta P, Sinha A, Sami A, et al. Incidence of acute kidney injury in hospitalized children. Indian Pediatr. 2012;49:537–42.
Roy JP, Devarajan P. Acute kidney injury: diagnosis and management. Indian J Pediatr. 2020;87:600–7.
Sethi SK, Mittal A, Nair N, et al. Pediatric Continuous Renal Replacement Therapy (PCRRT) expert committee recommendation on prescribing prolonged intermittent renal replacement therapy (PIRRT) in critically ill children. Hemodial Int. 2020;24:237–51.
Lee CY, Yeh HC, Lin CY. Treatment of critically ill children with kidney injury by sustained low-efficiency daily diafiltration. Pediatr Nephrol. 2012;27:2301–9.
Sethi SK, Bansal SB, Khare A, et al. Heparin free dialysis in critically sick children using sustained low efficiency dialysis (SLEDD-f): A new hybrid therapy for dialysis in developing world. PLOS One. 2018;13:e0195536.
Sethi SK, Sinha R, Jha P, et al. Feasibility of sustained low efficiency dialysis in critically sick pediatric patients: A multicentric retrospective study. Hemodial Int. 2018;22:228–34.
Marshall MR, Ma T, Galler D, Rankin AP, Williams AB. Sustained low-efficiency daily diafiltration (SLEDD-f) for critically ill patients requiring renal replacement therapy: towards an adequate therapy. Nephrol Dial Transplant. 2004;19:877–84.
Abe M, Okada K, Suzuki M, et al. Comparison of sustained hemodiafiltration with continuous venovenous hemodiafiltration for the treatment of critically ill patients with acute kidney injury. Artif Organs. 2010;34:331–8.
Abe M, Maruyama N, Matsumoto S, et al. Comparison of sustained hemodiafiltration with acetate-free dialysate and continuous venovenous hemodiafiltration for the treatment of critically ill patients with acute kidney injury. Int J Nephrol. 2011;2011:432094.
Basu RK, Zappitelli M, Brunner L, et al. Derivation and validation of the renal angina index to improve the prediction of acute kidney injury in critically ill children. Kidney Int. 2014;85:659–67.
Davis AL, Carcillo JA, Aneja RK, et al. American college of critical care medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock. Crit Care Med. 2017;45:1061–93.
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–10.
Bouchard J, Soroko SB, Chertow GM, et al. Program to Improve Care in Acute Renal Disease (PICARD) Study Group. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009;76:422–7.
Gaudry S, Hajage D, Schortgen F, et al. AKIKI Study Group. Initiation strategies for renal-replacement therapy in the intensive care unit. N Engl J Med. 2016;375:122–33.
Lobo V. Sustained Low-Efficiency Dialysis (SLED) and Hybrid Therapies in Children. In: Deep A, Goldstein SL, editors. Critical Care Nephrology and Renal Replacement Therapy in Children. Cham: Springer International Publishing; 2018. p. 291–306.
Kramer H, Yee J, Weiner DE, et al. Ultrafiltration rate thresholds in maintenance hemodialysis: An NKF-KDOQI controversies report. Am J Kidney Dis. 2016;68:522–32.
Mushatt DM, Mihm LB, Dreisbach AW, Simon EE. Antibiotic dosing in slow extended daily dialysis. Clin Infect Dis. 2009;49:433–7.
Schwartz GJ, Muñoz A, Schneider MF, et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009;20:629–37.
Tattersall JE, DeTakats D, Chamney P, Greenwood RN, Farrington K. The post-hemodialysis rebound: predicting and quantifying its effect on Kt/V. Kidney Int. 1996;50:2094–102.
Daugirdas JT. Physiologic principles and urea kinetic modeling. In: Daugirdas JT, Blake PG, Ing TS, editors. Handbook of dialysis, Fifth Edition. Philadelphia, PA:Wolters Kluwer Health; 2015;34–65.
Mishra SB, Azim A, Prasad N, et al. A pilot randomized controlled trial of comparison between extended daily hemodialysis and continuous veno-venous hemodialysis in patients of acute kidney injury with septic shock. Indian J Crit Care Med. 2017;21:262–7.
Chacko J, Brar G. Bedside ultrasonography: Applications in critical care: Part I. Indian J Crit Care Med. 2014;18:301–9.
Furtado S, Reis L. Inferior vena cava evaluation in fluid therapy decision making in intensive care: practical implications. Rev Bras Ter Intensiva. 2019;31:240–7.
Ostermann M, Bellomo R, Burdmann EA, et al. Controversies in acute kidney injury: conclusions from a kidney disease: improving global outcomes (KDIGO) conference. Kidney Int. 2020;98:294–309.
Kellum JA, Lameire N. KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care. 2013;17:204.
WHO. Application tools: WHO AnthroPlus software. Available at: http://www.who.int/growthref/tools/en/. Accessed on 11 Nov 2021.
Zhang L, Yang J, Eastwood GM, Zhu G, Tanaka A, Bellomo R. Extended daily dialysis versus continuous renal replacement therapy for acute kidney injury: a meta-analysis. Am J Kidney Dis. 2015;66:322–30.
Nash DM, Przech S, Wald R, O’Reilly D. Systematic review and meta-analysis of renal replacement therapy modalities for acute kidney injury in the intensive care unit. J Crit Care. 2017;41:138–44.
Ali US, Arya MK. Efficacy and safety of prolonged daily hemodialysis in critically ill children weighing less than 10 kg. Hemodial Int. 2020;24:108–13.
Messmer AS, Zingg C, Müller M, Gerber JL, Schefold JC, Pfortmueller CA. Fluid overload and mortality in adult critical care patients-a systematic review and meta-analysis of observational studies. Crit Care Med. 2020;48:1862–70.
Zhang L, Chen Z, Diao Y, Yang Y, Fu P. Associations of fluid overload with mortality and kidney recovery in patients with acute kidney injury: a systematic review and meta-analysis. J Crit Care. 2015;30:860.
VA/NIH Acute Renal Failure Trial Network, Palevsky PM, Zhang JH, O’Connor TZ, et al. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med. 2008;359:7–20.
Douvris A, Malhi G, Hiremath S, et al. Interventions to prevent hemodynamic instability during renal replacement therapy in critically ill patients: a systematic review. Crit Care. 2018;22:41.
Acknowledgements
The authors acknowledge the commitment and support of the nursing staff of pediatric hemodialysis and intensive care units.
Funding
The Indian Council of Medical Research provided funding to the Advanced Center for Research in Pediatric Kidney Diseases, Division of Nephrology, Department of Pediatrics, AIIMS [5/7/1090/2013-RHN].
Author information
Authors and Affiliations
Contributions
MY made substantial contribution to the acquisition, analysis, and interpretation of data and drafted the manuscript; ANT and PK helped in clinical work; ANT supervised dialysis sessions; AS, PH, JS, RL, and AB made substantial contributions to the conception and design of the work; revised the work critically for important intellectual content. AB will act as the guarantor for this paper.
Corresponding author
Ethics declarations
Ethics Approval
Institute Ethics Committee, All India Institute of Medical Sciences, Ansari Nagar, New Delhi; IECPG-465/27.09.2018, RT-12/18.10.2018/RT-5/14.11.2018.
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yadav, M., Tiwari, A.N., Lodha, R. et al. Feasibility and Efficacy of Sustained Low-Efficiency Dialysis in Critically Ill Children with Severe Acute Kidney Injury. Indian J Pediatr 90, 355–361 (2023). https://doi.org/10.1007/s12098-022-04214-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-022-04214-z