Abstract
Objective
To study the utility of diagnostic flexible bronchoscopy and bronchoalveolar lavage (BAL) in children with non-resolving pneumonia.
Methods
This was a cross-sectional study conducted in a tertiary care hospital from July 2015 through June 2016. Fifty-two consecutive children of both genders from 1 mo to 14 y of age with a diagnosis of non-resolving pneumonia were included. Flexible bronchoscopy was done in all patients with or without bronchoalveolar lavage (BAL). BAL was sent for gram staining, culture, gene expert™ and lipid laden macrophages examination. Main outcome measures were to find any morphological abnormality in the tracheobronchial tree and organism profile of a positive BAL culture.
Results
During the period of 12 mo, 52 consecutive patients of non-resolving pneumonia were enrolled. Median (IQR) age of the study population was 12 (68.8) mo. Mean ± SD duration of illness was 22.7 ± 5.6 d. Flexible bronchoscopy was found to be very safe and effective tool that directly led to definitive diagnosis in 30.7% of cases. It was positive for different organisms in 22 (52.3%) children. Neglected foreign body was seen in five patients.
Conclusions
Non-resolving pneumonia is often an area of clinical dilemma. Bacterial infections are the commonest etiology. Non-infectious causes like tracheobronchomalacia and foreign body aspiration are other important etiologies to be looked for. Early bronchoscopy and bronchoalveolar lavage analysis can play a crucial role in the evaluation of these patients and may provide an important clue or strongly support the specific diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood pneumonia continues to be the single largest killer worldwide. Although the implementation of safe, effective and affordable interventions has reduced pneumonia mortality from 4 million in 1981 [1] to just over one million in 2013 [2, 3], it still accounts for nearly one-fifth of childhood deaths worldwide.
Non-resolving pneumonia/slowly resolving pneumonia is a common entity in hospital practice and can pose a significant challenge to the treating doctor. Although there is no standard definition for this entity, it may be defined as failure of radiographic resolution by 50% in 2 wk or failure of complete resolution by one month despite adequate antibiotic therapy [4]. This can be due to defects in local or systemic immune defense mechanisms, the presence of unusual organism, resistant bacteria or diseases that mimic pneumonia, like neglected foreign body. As there is no universally accepted definition, the true incidence of non-resolving pneumonia in children is not known. The disease carries high mortality and more aggressive evaluation is required to find its etiology. Diagnostic flexible bronchoscopy with broncho alveolar lavage (BAL) has been found to be very effective in the evaluation of adult patients with this condition. The present study was conducted to find the utility of flexible bronchoscopy in establishing the etiological diagnosis of Non-resolving pneumonia.
Material and Methods
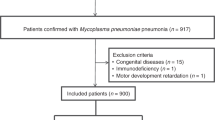
This cross-sectional study was conducted in the pediatric department of a tertiary care hospital in northern India from July 2015 through June 2016. Fifty two children of both genders from 1 mo to 14 y of age with the diagnosis of non-resolving pneumonia were enrolled in the study after obtaining written informed consent from the parents. Non-resolution was defined by the persistence of clinical symptoms and signs and failure of resolution of the radiographic features by 50% in 2 wk in spite of appropriate antibiotic therapy for a minimum duration of 10 d.
Flexible bronchoscopy was done in all patients with or without BAL. BAL was sent for gram staining, culture, gene expert™ and lipid laden macrophages examination.
A standardized data extraction form was used to obtain the demographic and clinical data including age, sex, weight and duration of symptoms. Laboratory data, including complete blood count, blood culture, chest radiograph, chest computerized tomography, if available and Mantoux test were also recorded from the study population. Flexible bronchoscopy (Olympus video bronchoscope) was done in all the patients. The authors used a BF-XP160F™ scope with channel size 1.2 mm in children less than four years of age and BF-MP-160F™ scope with a channel diameter of 2 mm in children above four years of age. Written informed consent was taken from all patients before undertaking the procedure. The procedure was done under sedation using IV midazolam either alone or in combination with ketamine/fentanyl boluses. Continuous oxygen was provided to all patients through nasal prongs during the procedure. ECG and oxygen saturation were also monitored during the procedure. Complications of the procedure were recorded in a standard format. Macroscopic appearance/abnormality of the bronchial tree during flexible bronchoscopy (Tracheomalacia, bronchomalacia, any foreign body, presence of secretions/pus, the appearance of the bronchial mucosa, etc.) was noted. BAL was collected from the affected lobe or from the right middle lobe bronchus in case of a diffuse disease. BAL was performed with the use of normal saline warmed to body temperature with a volume of 3 ml/kg administered in three divided doses. It was sent for gram staining, lipid laden macrophages examination, bacterial culture, fungal culture, Acid fast bacillus (AFB), and gene expert™ for Mycobacterium tuberculosis. Two patients also underwent Functional endoscopic evaluation of swallowing (FEES) in addition to routine bronchoscopy and lavage to diagnose aspiration pneumonia. Finally, efficacy of flexible bronchoscopy as a diagnostic tool to determine etiology of the pneumonia was assessed.
Statistical analyses were performed using SPSS 20. The normality of the data was checked by using the Shapiro-Wilk test. Parametric data are expressed as mean ± SD and non-parametric test as median (IQR). Categorical variables are presented as percentages.
Results
During the period of 12 mo 52 patients of both genders having clinical and/or radiological diagnosis of Non-resolving pneumonia were enrolled in this study; of these 32 were boys and 20 girls. Median (IQR) age of the study population was 12 (68.8) mo. The age ranged from 25 d to 14 y. Mean ± SD duration of illness was 22.7 ± 5.6 d. Median weight (IQR) of the study population was 9(13) kg. Four (2.08%) patients had pre-existing cystic fibrosis. Baseline investigations in the studied population did not point towards any primary or secondary immune deficiency; however, one patient was a known case of nephrotic syndrome and was on low dose long term steroids. Mantoux was positive in four patients. Flexible bronchoscopy was done in all 52 patients and BAL in 42 patients. Functional abnormalities of the tracheobronchial tree like bronchomalacia were seen in seven patients. All these children were less than one y of age. Neglected foreign body was seen in five patients. It was found in the right intermediate bronchus in four patients and left lower lobe bronchus in one patient (Fig. 1). Two patients from this group were already put on empiric anti-tubercular drugs with no improvement in symptoms. In two patients hydatid cysts were directly visualized on bronchoscopy, which was later confirmed by the presence of scolices in BAL fluid. FEES were done in two patients using methylene blue dye. Both the patients were known cases of cerebral palsy. FEES was positive for both the patients, which indicated oromotor incoordination as a cause of their persistent symptoms. Bronchoscopic findings are shown in Table 1. BAL was positive for microorganisms in 22 (52.3%) patients. Table 2 shows organism profile of BAL fluid. Gene expert™ was positive for Mycobacterium tuberculosis in two patients. Both patients had a history of contact with TB patients. One patient with underlying diabetes was infected with Zygomycetes. Foamy macrophages in BAL fluid were seen in five patients, which indicated gastro esophageal reflux as a cause of their persistent symptoms.
Discussion
There is a lack of uniformity regarding definitions for non-resolving pneumonia, but in many studies, the entity of “slow resolution” has been defined as failure of radiographic resolution by 50% in 2 wk or failure of complete resolution by one month despite adequate antibiotic therapy [4]. It is a diagnostic challenge for a pediatrician. These patients are often subjected to costly and inappropriate investigations with no much benefit and in the majority of patients the condition still remains undiagnosed. Eigen et al. found definite etiology in only 20 of 81 children evaluated for recurrent/persistent pneumonia [5]. The use of flexible bronchoscopy has become a safe and effective tool to evaluate Non-resolving pneumonia in pediatric patients [6]. The diagnostic yield is increased by the information obtained from BAL. There are many published studies on the etiology of Non-resolving pneumonia; however flexible bronchoscopy was rarely involved as a diagnostic tool in these studies [7, 8]. The current study is the first study from the region, evaluating the role of flexible bronchoscopy in children with Non- resolving pneumonia. The authors found flexible bronchoscopy to be very safe and effective tool, that directly led to definitive diagnosis in 30.7% of cases on mere visualization of the tracheobroncheal tree. Gokdemir et al. in a large study on 434 patients found that flexible bronchoscopy diagnosed 33% of patients with non-resolving pneumonia [9]. Tracheobronchomalacia is an important cause of chronic respiratory symptoms, especially in young infants; flexible bronchoscopy is the main diagnostic modality to diagnose the above condition. The authors found a 13% incidence of tracheobronchomalacia in their studied patients. Baets, et al. [10] found a 47% incidence of tracheobronchomalacia in their study population. However, they only included children less than 2 y of age, which could explain the apparent high prevalence of above disorder in his study group.
The authors collected BAL in 42 of their patients. BAL was positive for different organisms in 52.4% of patients. It resulted in a change in antibiotic regimen in 74% of BAL positive patients based on culture sensitivity reports. Baets et al. reported the diagnostic yield of 56% of BAL in children with persistent respiratory symptoms [10].
A foreign body is an important cause of non-resolving consolidation in young children and an early diagnosis is important. A large numbers of patients get treated for weeks and months due to persistent respiratory symptoms before the suspicion of foreign body aspiration. Late diagnosis results in respiratory complications such as lung abscess, atelectasis, bronchiectasis, and obstruction of the airway, which can be fatal [11]. The authors documented foreign body in 9.6% of patients with non-resolving consolidation. All these patients improved completely after removal of the foreign body.
Flexible bronchoscopy in children is a very safe procedure [12]. The authors also did not find any major complication during the procedure in the present study population. Minor complications in the form of transient de-saturation (5.7%), tachycardia (1.9%), transient apnea (1.9%), and transient epistaxis (1.9%) were seen in 6 patients only, making this procedure safe for routine evaluation of non-resolving pneumonia.
Conclusions
To summarize, non-resolving pneumonia is often an area of clinical dilemna; bacterial infections are the commonest etiology. Non-infectious causes like tracheobronchomalacia and foreign body aspiration are other important etiologies to be looked for. Early bronchoscopy and BAL analysis can play a very crucial role in the evaluation of these patients and may provide an important clue or strongly support a specific diagnosis.
References
Leowski J. Mortality from acute respiratory infections in children under 5 years of age: global estimates. World Health Stat Q. 1986;39:138–44.
United Nations Inter Agency Group for Child Mortality Estimation. Levels and Trends in Child Mortality: Report 2014. New York: UNICEF, WHO, the World Bank, United Nations Population Division; 2014.
Global Health Observatory. Proportions of Child Deaths by Cause. Geneva: WHO. Available at: http://www.who.int/gho/child_ health/en/index.html. Accessed 24 July 2014.
Kirtland SH, Winterbauer RH. Slowly resolving, chronic, and recurrent pneumonia. Clin Chest Med. 1991;12:303–18.
Eigen H, Laughlin JJ, Homrighausen J. Recurrent pneumonia in children and its relationship to bronchial hyperreactivity. Pediatrics. 1982;70:698–704.
Godfrey S, Avital A, Maayan C, Rotschild M, Springer C. Yield from flexible bronchoscopy in children. Pediatr Pulmonol. 1997;23:261–9.
Kumar M, Biswal N, Bhuvaneswari V, Srinivasan S. Persistent pneumonia: underlying cause and outcome. Indian J Pediatr. 2009;76:1223–6.
Owayed AF, Campbell DM, Weng EE. Underlying causes of recurrent pneumonia in children. Arch Pediatr Adolesc Med. 2000;154:190–4.
Gokdemir Y, Cakir E, Kut A, et al. Bronchoscopic evaluation of unexplained recurrent and persistent pneumonia in children. J Paediatr Child Health. 2013;49:E204–7.
De Baets F, De Schutter I, Aarts C, et al. Malacia, inflammation and bronchoalveolar lavage culture in children with persistent respiratory symptoms. Eur Respir J. 2012;39:392–5.
Passàli D, Lauriello M, Bellussi L, Passali G, Passali F, Gregori D. Foreign body inhalation in children: an update. Acta Otorhinolaryngol Ital. 2010;30:27–32.
Eber E, Zach M. Flexible fiberoptic bronchoscopy in pediatrics--an analysis of 420 examinations. [Article in German]. Wien Klin Wochenschr. 1995;107:246–51.
Author information
Authors and Affiliations
Contributions
JIB and WAW: Collected and compiled the data for thestudy, and drafted the manuscript; BAC and SWA: Conceptualized anddesigned the study; QIA: Finalized the manuscript; AAA: Did statistical analysis and intermittentdata check. MA: Involved in revising the manuscript and helped in data collection. Critical review was performed by all. JIB will act as guarantor for the paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Source of Funding
None.
Rights and permissions
About this article
Cite this article
Bhat, J.I., Wani, W.A., Ahmad, Q.I. et al. Flexible Bronchoscopy in Non-resolving Pneumonia. Indian J Pediatr 84, 681–684 (2017). https://doi.org/10.1007/s12098-017-2372-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-017-2372-7