Abstract
Objective
To define the therapeutic role of vitamin D in children with moderate to severe bronchial asthma as an adjunct to standard treatment.
Methods
Hundred asthmatic children of either sex, attending the respiratory and asthma clinic were enroled in the study. Diagnosis was made on the basis of history and clinical examination. Randomization was done using sealed opaque envelop method. In addition to the treatment as per GINA guidelines, one group received oral vitamin D3 (Cholecalciferol) 60,000 IU per month for 6 mo and the other group received placebo powder in the form of glucose sachet with a double blinded design. Monthly follow up of every patient was done and during every visit change in severity, level of control, Peak expiratory flow rate (PEFR), steroid dosage, number of exacerbations and number of emergency visits were assessed.
Results
Monthly doses of 60,000 IU vitamin D significantly reduced the number of exacerbations as compared to placebo (p = 0.011). PEFR significantly increased in the treatment group (p = 0.000). Monthly doses of vitamin D significantly reduced the requirement of steroids (p = 0.013) and emergency visits (p = 0.015). Control of asthma was achieved earlier in patients who received monthly vitamin D. Vitamin D significantly reduced the level of severity of asthma patients over 6 mo of treatment (p = 0.016).
Conclusions
Vitamin D has a definite role in the management of moderate to severe persistent bronchial asthma as an adjunct to standard treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma is a chronic inflammatory disorder of the airways in which many cells and cellular elements play a significant role. A worldwide increase in the prevalence of asthma has been reported in recent years, particularly in developing countries such as India [1, 2]. With an increase in prevalence comes an increased burden of disease in terms of morbidity, mortality and compromised quality of life.
Vitamin D is a potent immune system regulator having a potential role in various allergic diseases. A potential role of vitamin D in metabolic syndrome, colorectal cancer, breast cancer, multiple sclerosis, tuberculosis, pneumonia, influenza, respiratory distress [3], depression has been proposed. Supplementation with oral vitamin D has led to significant improvement in patients with pneumonia [4, 5] and atopic dermatitis [6].
The role of vitamin D in asthma is not yet clear. Few studies have proposed a possible link between asthma and polymorphisms in other genes involved in vitamin D synthesis, bioavailability and metabolism [7, 8]. Lower serum 25(OH)D have been correlated with a higher prevalence, hospitalization and emergency visits along with decreased lung function and increased airway hyperresponsiveness with exercise in various studies conducted in asthmatic children [9–12]. A protective effect of higher maternal vitamin D intake on asthma in children and adults has been demonstrated [13–15]. A few studies conducted in the recent past to evaluate the efficacy of vitamin D supplementation in patients of asthma have also shown promising results [16, 17].
Material and Methods
The present study was carried out in the department of pediatrics, Pt. BD Sharma University of Health Sciences, Rohtak, on 100 consecutive asthmatic children of either sex fulfilling the inclusion criteria, attending the respiratory and asthma clinic from May 2012 through December 2013. Institutional ethical committee approval was obtained.
Children with moderate to severe asthma as per GINA guidelines [18], aged between 3 and 14 y of age diagnosed by the physician were included in the study. Patients on immunotherapy or anti IgE or with history of premature birth (<36 wk) or home use of oxygen were excluded. Children with non wheezy asthma and clinical features of vitamin D deficiency (bony deformities and hypocalcemic symptoms) were also excluded.
Diagnosis was made on the basis of history and clinical examination. An informed consent was obtained from the parents of the asthmatic patients who were enroled in the study. Eligible patients underwent detailed history and clinical examination for the age, onset of disease, progression, duration of illness, symptoms, aggravating factors, treatment history, level of control etc. and findings were recorded in a predesigned patient proforma.
Randomization was done using sealed opaque envelop method. Patients fulfilling inclusion criteria were enroled in group A and B. Blinding was done by putting the names as group A and group B and patient as well as investigator did not know about the component of A and B. Thus, double blinding was ensured.
Children were given treatment as per their group. One group received oral vitamin D3 (Cholecalciferol) 60,000 IU per month for 6 mo. Vitamin D sachet was procured from Cadila and opaque sachet was made in the hospital pharmacy and other group received placebo powder in the form of glucose sachet.
Monthly follow up of every patient was done and during every visit, change in severity was assessed and was recorded in a predesigned patient proforma on the basis of GINA guidelines. PEFR was assessed using Breathe-o meter (Cipla).
Primary outcome measure was change in the level of severity of asthma according to GINA guidelines.
Secondary outcome measures were
-
Number of exacerbations during treatment period
-
Change in the PEFR
-
Change in the Steroid dosage
-
Level of control
-
Emergency visits
Data was analyzed by SPSS Version 17 statistical software. At the end of the study, the data was analyzed using appropriate statistical tests and as some of the subjects were lost to follow up, the data was analyzed by intention to treat analysis. p value of <0.05 was taken as significant.
Results
Age of children in the study population ranged from 5 y to 13 y. The study included 51 females and 49 male children with a male to female ratio of 1:1.04 (Table 1). There was no statistically significant difference between baseline characteristics of the two groups except for the mean age of onset of asthma which was significantly higher in the placebo group (Table 1). Maximum number of patients in the study population belonged to lower middle class as assessed by modified Kuppuswamy’s socioeconomic status (SES) scale. The education level of father of the study patients was higher than the mother. There was no statistically significant difference in the disease characteristics between the two treatment groups.
A total of 51 patients, 25 from placebo group and 26 from vitamin D group had received some form of treatment for asthma. There was no statistically significant difference between severity, level of control and treatment technique in the two groups. Shortness of breath was the most common symptom complained by the patients followed by tightness of chest and night cough. Smoking by the parents was the most common aggravating factor for asthma in the study patients. There was no statistically significant difference in symptoms and aggravating factors between the two treatment groups. A history of early injury to the airways in the form of parental smoking was present in 55 patients followed by exposure to smoke at home (21 patients) and pneumonia (19 patients).
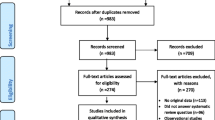
Out of the enroled patients, ten from placebo group and eight from vitamin D were lost to follow up (Fig. 1). Intention to treat analysis was applied to measure the treatment outcomes.
There was a slight increase in the asthma severity from moderate to severe in the placebo group till 5 mo follow up mainly due to increase in the requirement of steroids, while there was no increase in asthma severity in vitamin D group, however this difference was not statistically significant (Table 2). At 6 mo follow up, the improvement in asthma severity was statistically significant in favor of vitamin D group (p = 0.016) (Table 2). Episodes of acute exacerbations during the treatment period were significantly less in the vitamin D group as compared to placebo group (Table 3).
There was a significant improvement in the PEFR in both the groups at the follow up visits up to 6 mo (p = 0.000). However, the improvement in PEFR of the vitamin D group was significantly higher than the placebo group (p = 0.000) (Fig. 2).
There was an increase in the mean dose of steroid required in both the groups initially due to inadequate control; however the requirement was lower in vitamin D group as compared to placebo group. There was a statistically significant decrease in steroid dosage in both the groups at the follow up at 6 mo (p = 0.000). The decrease in the steroid dose was significantly higher in vitamin D group as compared to placebo group (p = 0.013) (Fig. 3).
Asthma control was achieved in all the patients of both the groups after 4 mo of treatment. At 1 mo, 21 patients in placebo group had their asthma well controlled as compared to 35 patients in vitamin D group (p = 0.005). Thus, control was achieved earlier in vitamin D group as compared to placebo group (Table 4).
None of the patient in the study required emergency visits after 3 mo of treatment. Mean number of emergency visits showed a statistically significant difference in favor of vitamin D group (p = 0.015) (Table 5).
Discussion
Based on the available information regarding causal role and therapeutic benefits of vitamin D in asthma, the present double blind randomized study was planned to define the therapeutic role of vitamin D as an adjunct to standard treatment in asthmatic children.
The level of severity was statistically similar for both the groups till 5 mo of follow up but at 6 mo, the level of severity was less in vitamin D group as compared to placebo group. A delayed beneficial effect on asthma severity was seen. Thus, monthly doses of vitamin D can reduce the level of severity of asthma patients.
Patients treated with vitamin D had significantly less exacerbations during the treatment period. Similarly, in a randomized, double-blind, placebo-controlled trial, Urashima et al. compared the effect of 1,200 IU/d of vitamin D3 vs. placebo in schoolchildren suffering from influenza during the winter months. In the sub-analyses, vitamin D3 supplementation was associated with a decreased risk of exacerbations compared with placebo, with a relative risk of 0.17 [16]. In a more recent randomized, double-blind parallel arm 6-mo clinical trial conducted by Majak et al., children receiving supplemental 500 IU/d vitamin D had a reduced risk of asthma exacerbations triggered by acute respiratory viral infections [17].
Improvement in mean PEFR was observed in both the treatment groups during follow up visits. But, the improvement in the PEFR in the vitamin D group was significantly higher as compared to placebo group showing the effect of vitamin D on airway narrowing. Low vitamin D levels have been associated with decreased lung function [9, 10]. Recently, Alyasin et al. in a cross-sectional study concluded that 25(OH)D levels had direct and significant correlations with both predicted FEV1 and FEV1/FVC [11]. Thus, serum 25-hydroxy vitamin D levels were inversely associated with asthma, and there was a direct and significant relationship between vitamin D levels and pulmonary function test outcomes in asthmatic children.
The requirement of steroid increased in both the groups due to poor control till 5 mo and thereafter decreased. There was a significant reduction in steroid dose required in both the groups but the reduction in vitamin D group was significantly higher than placebo group. Thus, monthly doses of vitamin D have a potential to reduce the steroid dose required to control asthma. Searing et al. in a cross-sectional study of 100 children (mean age-7 y) of moderate to severe persistent asthma have noted increased corticosteroid requirements in children as a function of decreased 25(OH)D concentrations [10].
Significantly higher number of patients were well controlled in vitamin D group as compared to placebo group after 1 mo of treatment. At 2 and 3 mo in the follow up period, statistically similar number of patients were well controlled in both the groups. At 4 mo, asthma was well controlled in all the patients. So, asthma control was achieved earlier in the vitamin D group, however due to the additional treatment given according to severity of asthma, gradually asthma control was achieved in placebo group as well. Better asthma control has been correlated with high vitamin D levels previously by Chinellato et al. [19].
The mean number of emergency visits decreased till 3 mo of treatment in both the groups. None of the patients in any of the groups required visit to emergency after 3 mo of treatment. The treatment given according to severity of asthma was able to reduce visits to emergency as there was a significant fall in number of emergency visits at follow up in both the groups. However, the fall in the number of emergency visits in vitamin D group was statistically higher than placebo group. So, monthly doses of vitamin D were effective in reducing the number of emergency visits in moderate to severe asthma patients. Brehm et al. have also shown that the risk of hospitalization and emergency visit was more common among vitamin D-deficient children [20]. However, the present study has certain limitations.
Measurement of vitamin D levels prior to the administration of vitamin D and follow up would have supported the outcome of the study.
Conclusions
The patients in the index study who received monthly doses of vitamin D had less number of exacerbations and achieved better and earlier control of asthma. PEFR significantly increased and the requirement of steroids was significantly reduced. Moreover, the emergency visits were also reduced. Thus, vitamin D has a definite role in the management of moderate to severe persistent bronchial asthma as an adjunct to standard treatment. However, larger trials involving more number of patients are required to define the role of vitamin D in asthma.
References
International study of Bronchial Asthma and allergies in childhood (ISAAC). Worldwide variations in the prevalence of Bronchial Asthma symptoms. Euro Respir J. 1998;12:315–35.
Morbidity and Health Care International Institute for Population Sciences (IIPS) and Macro International; National Family Health Survey (NFHS-3), 2005–06: India: Vol. 1. Mumbai: IIPS; 2007. pp. 423.
Tiwari S, Kumar R, Singla S, Dudeja A, Nangia S, Saili A. Congenital rickets presenting as refractory respiratory distress at birth. Indian J Pediatr. 2013. doi:10.1007/s12098-013-1099-3.
Manaseki-Holland S, Qader G, Isaq Masher M, Bruce J, Zulf Mughal M, Chandramohan D, et al. Effects of vitamin D supplementation to children diagnosed with pneumonia in Kabul: A randomised controlled trial. Trop Med Int Health. 2010;15:1148–55.
Khadilkar VV, Khadilkar AV. Use of vitamin D in various disorders. Indian J Pediatr. 2013;80:215–8.
Amestejani M, Salehi BS, Vasigh M, Sobhkhiz A, Karami M, Alinia H, et al. Vitamin D supplementation in the treatment of atopic dermatitis: A clinical trial study. J Drugs Dermatol. 2012;11:327–30.
Wjst M, Altmüller J, Faus-Kessler T, Braig C, Bahnweg M, André E. Asthma families show transmission disequilibrium of gene variants in the vitamin D metabolism and signalling pathway. Respir Res. 2006;7:60.
Pillai DK, Iqbal SF, Benton AS, Lerner J, Wiles A, Foerster M, et al. Associations between genetic variants in vitamin D metabolism and asthma characteristics in young African Americans: A pilot study. J Investig Med. 2011;59:938–46.
Chinellato I, Piazza M, Sandri M, Peroni DG, Cardinale F, Piacentini GL, et al. Serum vitamin D levels and exercise-induced bronchoconstriction in children with asthma. Eur Respir J. 2011;37:1366–70.
Searing DA, Zhang Y, Murphy JR, Hauk PJ, Goleva E, Leung DY. Decreased serum vitamin D levels in children with asthma are associated with increased corticosteroid use. J Allergy Clin Immunol. 2010;125:995–1000.
Alyasin S, Momen T, Kashef S, Alipour A, Amin R. The relationship between serum 25 hydroxy vitamin D levels and asthma in children. Allergy Asthma Immunol Res. 2011;3:251–5.
Ozaydın E, Bütün MF, Cakır BC, Köse G. The association between vitamin D status and recurrent wheezing. Indian J Pediatr. 2013. doi:10.1007/s12098-013-1005-z.
Camargo JCA, Rifas-Shiman SL, Litonjua AA, Rich-Edwards JW, Weiss ST, Gold DR, et al. Maternal intake of vitamin D during pregnancy and risk of recurrent wheeze in children at age 3 years. Am J Cli Nutr. 2007;85:788–95.
Devereux G, Litonjua AA, Turner S, Craig LC, McNeill G, Martindale S, et al. Maternal vitamin D intake during pregnancy and early childhood wheezing. Am J Clin Nutr. 2007;85:853–9.
Morales E, Romieu I, Guerra S, Ballester F, Rebagliato M, Vioque J, et al; INMA Project. Maternal vitamin D status in pregnancy and risk of lower respiratory tract infections, wheezing, and asthma in offspring. Epidemiology. 2012;23:64–71.
Urashima M, Segawa T, Okazaki M, Kurihara M, Wada Y, Ida H. Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren. Am J Clin Nutr. 2010;91:1255–60.
Majak P, Olszowiec-Chlebna M, Smejda K, Stelmach I. Vitamin D supplementation in children may prevent asthma exacerbation triggered by acute respiratory infection. J Allergy Clin Immunol. 2011;127:1294–6.
Global Initiative for Asthma (GINA), National Heart, Lung and Blood Institute (NHLBI). Global strategy for asthma management and prevention: Bethesda (MD); 2011. pp. 2. Available from: www.ginasthma.com.
Chinellato I, Piazza M, Sandri M, Peroni D, Piacentini G, Boner AL. Vitamin D serum levels and markers of asthma control in Italian children. J Pediatr. 2011;158:437–41.
Brehm JM, Schuemann B, Fuhlbridgge AL. The role of Vitamin D in asthmatic disease. Breathe. 2010;7:194.
Conflict of Interest
None.
Role of Funding Source
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yadav, M., Mittal, K. Effect of Vitamin D Supplementation on Moderate to Severe Bronchial Asthma. Indian J Pediatr 81, 650–654 (2014). https://doi.org/10.1007/s12098-013-1268-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-013-1268-4