Abstract
Objective
To investigate the effect of Auditory, Tactile, Visual and Vestibular stimulus (ATVV) on neuromotor development in preterm infants.
Methods
Fifty preterm infants born at 28–36 wk with a birth weight ranging from 1,000–2,000 g were recruited for the study. They were block randomized into a control group (n = 25) and study group (n = 25). New Ballard score was used for the baseline measurement of neuromaturity in both groups. In neonatal intensive care unit (NICU), the study group received multisensory stimulation for 12 min per session, 5 sessions per wk along with routine NICU care either from 33 wk corrected gestational age for infants born at 28–32 wk or from 48 h of birth for infants born at 33–36 wk until discharge from the hospital. The control group received the routine NICU care. At term age the preterm infants were assessed using Infant Neurological International Battery (INFANIB) and the groups were compared using independent t test.
Results
The multisensory stimulated infants showed higher neuromotor score (p = 0.001) compared to the control group. The french angle components of INFANIB including heel to ear (p = 0.016) and popliteal angle (p = 0.001) were statistically significant between the groups.
Conclusions
Multisensory stimulation appears to have a beneficial effect on the tonal maturation in preterm infants. However, further studies are warranted to investigate the long-term effects of multisensory stimulation on neurodevelopmental outcome in preterm infants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preterm infants are nurtured in the neonatal intensive care unit (NICU) for the first few days or weeks of their life. The NICU environment is much different from that of intrauterine environment and hence may pose a risk to these fragile neonates [1]. The preterm infants have to adapt to extrauterine environment with immature body systems which include musculoskeletal, neuromuscular, cardiovascular, pulmonary, and integumentary systems [2]. Furthermore, they are deprived of various sensory inputs perceived in utero that are regulated both in intensity and nature [3]. Preterm infants are reported to have delayed development of gross motor abilities and often referred for developmental intervention, which aims to facilitate the neurobehavioral function and physiological stability [4]. Environmental modifications such as controlling the negative stimuli (excessive light, loud noise) and providing positive sensory experiences are generally being used as developmental intervention. Early sensory information and motor experiences can enhance brain development by affecting the structure of brain [5].
Interventions mimicking the intrauterine environment may have a beneficial effect on the development of preterm infants and assist them cope up better with the unfavorable environment [6]. Multisensory stimulation (ATVV) has been shown to be safe in stable preterm infants [7]. It has resulted in improving alertness in preterm babies, hastening the feeding progression and reducing the length of hospital stay [8, 9]. Currently, conflicting evidence exists on the effect of multisensory stimulation on neuromotor and neurobehavioral aspects of development in preterm infants. Initially, Leib reported higher developmental status in multisensory enriched group of high risk preterm infants on Bayley scales of infant development at 6 mo corrected age [10]. However, Brown et al. did not observe any short term (at discharge) or long term (at 1 y follow up) effect with multisensory stimulation [11]. A recent Cochrane systematic review included only three randomized controlled trials which demonstrated the effect of multisensory (ATVV) stimulation on neurodevelopment. All those three studies reported better behavioral states in preterm infants; however, there was no study specifically investigating the neuromotor aspect of development [6]. Currently, studies investigating the short term effects of multisensory ATVV stimulation on neuromotor development in stable preterm infants are rarely reported. Hence the purpose of the present study was to investigate the immediate (short-term) effect of multisensory stimulation on neuromotor development in preterm infants.
Material and Methods
The inclusion criteria were infants born between 28 and 36 wk of gestation and birth weight ranging from 1,000–2,000 g. The exclusion criteria were medically unstable preterm infants, and infants with congenital anomalies, congenital infections and central nervous system injury. Sample size was calculated using the formula for comparing means with the level of significance as 0.05, with 80 % power and 2 units in the neuromotor score as clinically meaningful difference. Assuming a 20 % drop out rate, a total sample of n = 50 was estimated for the study. The study protocol was approved by the University Ethical Committee (Manipal University, No: UEC/12/2010). Preterms in the NICU of Kasturba Hospital, Manipal (India) were recruited for the study. Initially, 57 preterm infants were screened out of which 7 were excluded (5 congenital anomalies, 1 congenital pneumonia and 1 congenital rubella). Fifty preterm infants were equally block randomized into study and control group (5 blocks of 10 infants each using lottery method). Figure 1 demonstrates the recruitment process. Informed consent to participate in the study was sought from the parents of the preterm infants.
The baseline data for both groups were collected from the medical records which included birth weight, length, head circumference, Apgar score at 1 min and 5 min. The New Ballard score was used for the baseline measurement of neuromaturity in the preterm infants. Table 1 shows the baseline characteristics of the preterm infants. The study group was subjected to ATVV stimulation along with the routine NICU care which consisted of kangaroo mother care and exclusive breast feeding. The infants assigned to control group received the routine care in the NICU.
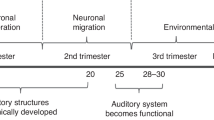
The study group infants received intervention when they achieved a gestational age of 33 wk, because at this age the tactile, vestibular, visual and auditory sensory pathways are well developed [8]. For infants born at 33–36 wk, stimulation was started after 48 h of birth. The stimulations were provided during quiet alert state of preterm infant, 30 min before feeding. Stimulations were given for duration of 12 min daily, 5 d per wk until discharge from the hospital. The following multisensory stimuli were provided.
Auditory Stimulation
—Soft lullaby between (30–40 dB) for 3 min using a miniature speaker (PHILIPS, MI 1500, INDIA) and an mp3 player (MOSERBAER, MP565-2C, INDIA); Tactile Stimulation—Gentle stroking massage for 3 min in a sequence of chest, upper limbs and lower limbs in supine position; Visual Stimulation—Black and white visual stimulation card hung at a distance of 8–10 in. from the neonate for 3 min; Vestibular Stimulation—Gentle horizontal and vertical rocking for 3 min.
During the ATVV intervention programme, physiological stress signs were observed using multiparameter monitor (PHILIPS IntelliVue MP 20, India). The physiological stress was defined as any change in physiological parameters, heart rate (HR) >200 or <100 bpm, respiratory rate (RR) > 20 over baseline and oxygen saturation (SpO2) below 86 % for more than 15 s [7]. The behavioral stress signs observed for were as proposed by Als in the Synactive theory on the behavioral organization of development [12]. These included startle, tremors, yawning, finger splay, tone changes, state changes, gaze aversion, cry, hiccups and tongue protrusion. The intervention was modified (particular stimulation paused for 15 s and resumed if parameters recovered) based on the infant’s physiological and behavioral stress responses in order to prevent overloading of the sensory inputs.
Infant Neurological International Battery (INFANIB) was used as the primary outcome measure to assess the neuromotor development of the preterm infants at term age (between 38 and 40 wk of corrected gestational age). INFANIB is a valid and reliable outcome measure which consists of 20 items that assesses the infant’s motor development in supine, prone, standing, and suspended positions for reflexes and French angles as well as muscle tone and body posture [13]. The mean total INFANIB scores between the groups were compared using independent t test. Mann Whitney U test was used to compare the individual components of the INFANIB Scale. Data were analyzed using SPSS version 15 software.
Results
Fifty healthy preterm infants with head circumference ranging from 24.7–31.8 cm and length ranging from 34–46.7 cm were investigated. The average number of intervention session was 12. For two infants, four ATVV sessions were missed; one child was intubated during the study period due to hypoglycemia and respiratory distress and one child had intense cry due to hypoglycemia and so the intervention was difficult to administer. Both the study and control groups were comparable at baseline in terms of gestational age, weight, length, head circumference, length of hospital stay and New Ballard score with a p value greater than 0.05 as demonstrated in Table 1. The mean INFANIB total score of control group (x = 59.16, SD = 3.23) and study group (x = 62.24, SD = 3.07) showed statistically significant difference (p = 0.001) with a 95 % confidence interval of (−4.87, −1.28). Mann Whitney U test revealed significant differences among individual INFANIB components between the groups in the heel to ear (p = 0.016), popliteal angle (p = 0.001) and weight bearing in standing component (p = 0.044) as shown in (Table 2).
Discussion
The primary purpose of the present study was to investigate the immediate effects of multisensory ATVV stimulation on neuromaturity in stable preterm infants. The present results showed improved neuromotor development in the study group as demonstrated by the differences in total INFANIB scores and also individual INFANIB components such as heel to ear, popliteal angle scores (French angles) and weight bearing in standing component between the groups.
In terms of ATVV stimulation used in the present study, the sound level of lullabies administered was calibrated to 45–55 dB because it is recommended to support stable vital signs of infants in NICU [14]. Black and white pattern cards were used for visual stimulus for the reason that the preterm infants are attentive to these colors [3]. Tactile stimulation was followed by vestibular stimulation owing to its moderating effect on the rapid heart rate response found with tactile stimulation [15]. Moreover, tactile stimulations have been reported to be too arousing and hence suggested to be followed by vestibular stimulation [16]. However, the ATVV stimulation used in the index study is less comparable to other studies owing to differences in duration, type and order of stimulus. Future studies could possibly investigate the effects of various type, duration and order of ATVV stimulation on neurodevelopment in preterm infants.
The development of the normal tone in the study group could be attributed to the effect of vestibulo–proprioceptive input received by the infant during the ATVV stimulation. Vestibular stimulation in the form of hammock positioning has shown to develop flexor tone in preterm infants [17]. Weight bearing and proprioceptive stimulations have also shown to develop normal tone in preterm infants [18]. The development of flexor tone could possibly reduce the incidence of secondary complications such as hip abductor contracture and thereby prevent delay in motor milestones. Furthermore, since the development of normal tone is in caudo-cephalic direction the authors opine that a neuromotor evaluation at a later age would have revealed tonal development in the upper limbs as well. Individual INFANIB components such as foot grasp, tonic labyrinthine supine, asymmetric tonic neck reflex, pull to sit, all fours and tonic labyrinthine prone showed no difference between the groups which indicates a lack of reflex maturation in the study group. Although the authors investigated the neurodevelopment of preterm infants in term age, some of the studies report a high sensitivity but low specificity in predicting the abnormal functional outcome when assessments are made at neonatal period [19], henceforth a long-term follow up of the infants in the study is needed to determine their future neuromotor outcome.
Each component of multisensory ATVV stimulation was given in a successive manner. Thus there was a better control over the intervention and the stimulation could be stopped immediately in case of any stress signs noted. In the present study, the response of the infants to stimulation was within the physiological limits, hence ATVV stimulations are safe to administer in stable preterm infants. The present observations are consistent with Nelson, who also showed no clinically significant difference in the HR, RR and SpO2 between the control group and the ATVV stimulated group in preterm infants of 33–35 wk post conceptional age [20].
The literature search revealed two previous studies which investigated the short term effects of ATVV stimulation on neurodevelopmental aspect of preterm infants. Out of these, one study investigated healthy preterm infants [11] and the other investigated infants with periventricular leukomalacia [8]. Both the studies used Neonatal Behavioral Assessment Scale (NBAS) as outcome measure and did not report any significant effect of multisensory stimulation. However, the index study is different from those studies in terms of duration, type, order of stimulation and the outcome measure (neuromotor scale) used, hence the present study results could not be compared with those studies.
A few limitations of the present study include, firstly, blinding of the assessor was not possible owing to feasibility issues such as availability of personnel and time constraints associated with the research. Secondly, the lower limit of 95 % confidence interval for the mean difference in total INFANIB scores between the groups was 1.28, which necessitates caution in interpreting the results. Finally, although INFANIB is used for assessing preterm infants at 0–18 mo, it has been primarily validated in infants of age group 3–22 mo.
Conclusions
Multisensory stimulation appears to have an immediate beneficial effect on the neuromotor development in preterm infants at their term age. ATVV procedure could be an integral part of the routine neonatal physiotherapy for the healthy preterm infants. However, future studies are warranted to investigate whether the early development of flexor tone in the preterm infants has a long-term effect on the neurodevelopmental outcome. Furthermore, the safety and efficacy of this multisensory stimulation should be investigated in preterm infants with associated co-morbidities such as periventricular leukomalacia or similar central nervous system injury.
References
Holditch-Davis D, Blackburn S, VandenBerg K. Newborn and infant neurobehavioral development. Comprehensive Neonatal Nursing: A Physiologic Perspective. 3rd ed. St Louis: Saunders; 2003. pp. 272–73.
Sweeney JK, Heriza CB, Blanchard Y. Neonatal physical therapy. Part I: clinical competencies and neonatal intensive care unit clinical training models. Pediatr Phys Ther. 2009;21:296.
Tecklin JS. Pediatric Physical Therapy. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2008.
Van Haastert I, De Vries L, Helders P, Jongmans M. Early gross motor development of preterm infants according to the Alberta Infant Motor Scale. J Pediatr. 2006;149:617–22.
Sweeney JK, Heriza CB, Blanchard Y, Dusing SC. Neonatal physical therapy. Part II: practice frameworks and evidence-based practice guidelines. Pediatr Phys Ther. 2010;22:2.
Symington A, Pinelli J. Developmental care for promoting development and preventing morbidity in preterm infants. Cochrane Database Syst Rev. 2006;2:CD001814.
Burns K, Cunningham N, White-Traut R, Silvestri J, Nelson MN. Infant stimulation: modification of aniIntervention based on physiologic and behavioral cues. J Obstet Gynecol Neonatal Nurs. 1994;23:581–9.
White-Traut RC, Nelson MN, Silvestri JM, et al. Developmental intervention for preterm infants diagnosed with periventricular leukomalacia. Res Nurs Health. 1999;22:131–43.
White-Traut RC, Nelson MN, Silvestri JM, et al. Effect of auditory, tactile, visual, and vestibular intervention on length of stay, alertness, and feeding progression in preterm infants. Dev Med Child Neurol. 2002;44:91–7.
Leib SA, Benfield DG, Guidubaldi J. Effects of early intervention and stimulation on the preterm infant. Pediatrics. 1980;66:83.
Brown J, LaRossa M, Aylward G, Davis D, Rutherford P, Bakeman R. Nursery-based intervention with prematurely born babies and their mothers: are there effects? J Pediatr. 1980;97:487–91.
Als H. Toward a synactive theory of development: promise for the assessment and support of infant individuality. Infant Ment Health J. 1982;3:229–43.
Ellison PH, Horn JL, Browning CA. Construction of an Infant Neurological International Battery (INFANIB) for the assessment of neurological integrity in infancy. Phys Ther. 1985;65:1326.
Philbin MK, Robertson A, Hall 3rd JW. Recommended permissible noise criteria for occupied, newly constructed or renovated hospital nurseries. Adv Neonatal Care. 2008;8:S11.
Mahoney MC, Cohen MI. Effectiveness of developmental intervention in the neonatal intensive care unit: implications for neonatal physical therapy. Pediatr Phys Ther. 2005;17:194.
White-Traut RC, Nelson MN, Silvestri JM, Cunningham N, Patel M. Responses of preterm infants to unimodal and multimodal sensory intervention. Pediatr Nurs. 1997;23:169–75.
Keller A, Arbel N, Merlob P, Davidson S. Neurobehavioral and autonomic effects of hammock positioning in infants with very low birth weight. Pediatr Phys Ther. 2003;15:3.
Tecklin JS. Pediatric Physical Therapy. 3rd ed. Philadelphia: Williams & Wilkins; 1999.
Pedersen S, Sommerfelt K, Markestad T. Early motor development of premature infants with birthweight less than 2000 grams. Acta Paediatr. 2000;89:1456–61.
White-Traut RC, Nelson MN, Silvestri JM, et al. Developmental patterns of physiological response to a multisensory intervention in extremely premature and high-risk infants. J Obstet Gynecol Neonatal Nurs. 2004;33:266–75.
Contributions
PS: Concept and design, acquisition of data and interpretation, critical review and final approval of the study; BKR: Concept and design, interpretation of data, drafting the article, critical review and final approval of the study; DM: concept and design, critical review and final approval of study; LEL: Critical review and final approval of the study; AK: Interpretation of data, critical review and final approval of the study.
Acknowledgments
This research received the best poster award in the Indian Association of Physiotherapists (IAP) Conference, January 2011. The authors acknowledge Dr. G. Arun Maiya Head, Department of Physiotherapy for guiding with research design, Mrs. Shuba R. Nayak Assistant Lecturer Department of Physiotherapy for the supervision of methodology, Mr Hari Prakash Assistant Professor and Mr Ayas Mohammed Lecturer, Department of Speech and Hearing for helping with assessment of noise level of neonatal intensive care unit.
Conflict of Interest
None.
Role of Funding Source
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kanagasabai, P.S., Mohan, D., Lewis, L.E. et al. Effect of Multisensory Stimulation on Neuromotor Development in Preterm Infants. Indian J Pediatr 80, 460–464 (2013). https://doi.org/10.1007/s12098-012-0945-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-012-0945-z