Abstract
Purpose
Hypoxia is an indispensable factor in the progression of metastasis. Hypoxia inducible factor-1α (HIF-1α), the core element in generating the hypoxia response, induces invasion and metastasis by promoting epithelial–mesenchymal transition (EMT). This study explored the underlying mechanism of hypoxia associated with the invasion and metastasis of gastric cancer (GC).
Methods
Six methods were employed to assess the function of the long noncoding RNA (lncRNA) prostate cancer gene expression marker 1 (PCGEM1) including gene silencing, RT-PCR, the separation of nuclear and cytoplasmic fractions, scrape motility assay, transwell migration assay, and Western-blot.
Results
LncRNA PCGEM1 was overexpressed in GC cells and tissues, and was induced by hypoxia in GC cells. Additional experiments confirmed that the knockdown of PCGEM1 significantly repressed the invasion and metastasis of GC cells. SNAI1, a key transcription factor of EMT, was regulated by PCGEM1. Overexpression of SNAI1 rescued the inhibition of PCGEM1-knockdown during the invasion and metastasis of GC cells. In addition, PCGEM1 and SNAI1 jointly affected the biomarkers of EMT.
Conclusion
Our findings indicated that PCGEM1 is a hypoxia-responsive lncRNA, and contributes to the invasion and metastasis of GC. The potential mechanism is attributed to the regulation of EMT by PCGEM1 and its influence on the expression of SNAI1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the declining incidence of gastric cancer (GC) in recent years, it remains the fourth most common cancer type and the second leading cause of cancer-related death [1]. Distant metastases or a high risk of complications are present in a large number of GC patients at the time of diagnosis. Despite progress in the treatment of GC, clinical prognosis remains dismal. Evidence has shown that the tumor hypoxic microenvironment is closely associated with cancer progression and metastasis [2]. The stabilization of hypoxia inducible factors (HIFs) have been demonstrated to induce tumor cells to adapt to this microenvironment stress [3]. Specifically, hypoxia inducible factor-1 (HIF-1), a significant heterodimeric transcription factor composed of a labile HIF-1α subunit and a stable HIF-1β subunit, has been shown to up-regulate epithelial–mesenchymal transition (EMT)-related transcription factors (EMT-TFs) [4]. HIF-1α is the core element in generating the hypoxia response and has a close relationship with human cancers [5]. In previous research, we demonstrated that HIF-1α is an independent prognostic factor in GC [6]. However, the molecular mechanism by which hypoxia impacts GC metastasis has not yet been fully characterized.
With completion of the Human Genome Project (HGP) and the parallel development of Next Generation Sequencing, human transcriptome analysis revealed that more than 98% of the transcriptional output encodes non-coding RNAs (ncRNAs) [7]. Evidence has confirmed that the dysregulation of ncRNAs plays a crucial role in the regulation of oncogenes or tumor suppressor genes [8]. Long noncoding RNAs (lncRNAs), a class of ncRNAs longer than 200 nucleotides, showed little evidence of protein-coding capacity [9], have move to the center of ncRNA arena. Researchers have demonstrated that lncRNAs affect and regulate gene expression at multiple levels, including the epigenetic, transcriptional, post-transcriptional and translational levels. Two types of lncRNA-HIFs interactions have been identified: tumor local hypoxia, which affects the expression of lncRNAs, and HIF signaling, which is positively or negatively regulated by lncRNA [10]. These two types of lncRNAs are defined as hypoxia-responsive lncRNAs (HRLs) [11]. Although some HRLs have been reported to play important roles in diverse processes, only a few HRLs which mediate transcriptional regulation in GC have been described. The lncRNAs GAPLINC [12] and HIF1A-AS2 [13] are overexpressed in GC and are associated with poor prognosis. The lncRNAs BC005927 [14], AK058003 [15] and AK123072 [16] promote GC invasion and metastasis under hypoxic conditions.
EMT involves the key steps in initiating tumor cell metastasis by which polar epithelial cells are transformed into mesenchymal phenotypic cells and is accompanied by the down-regulation of epithelial markers and the up-regulation of mesenchymal markers [17]. SNAI1, a key transcription factor of EMT, binds to the promoters of E-cadherin and inhibits the EMT biological process, which reduces cell adhesion and improves migration.
In the present study, we focused on the lncRNA prostate cancer gene expression marker 1 (PCGEM1), a prostate-related gene regulated by androgen [18], which is located at 2q32.3 and includes four exons. We aimed to investigate the role of PCGEM1 in GC invasion and metastasis, and hypothesized that PCGEM1 acts as an oncogene partly by targeting SNAI1 to regulate EMT.
Materials and methods
Cell lines and cell culture
The normal human gastric epithelial cell line GSE-1 and human gastric cancer cell lines SGC-7901 and BGC-823 were cultured in RPMI 1640 medium supplemented with 10% fetal bovine serum (FBS, Invitrogen, Carlsbad, CA, USA), 100 U/mL penicillin, and 100 μg/mL streptomycin (Invitrogen) at 37 °C under 5% CO2 and 1% O2 (or 20% O2). Cells were obtained from China Medical University (Shenyang, China). All experiments were performed in triplicate with independent cell cultures.
Tissues and ethical statement
Forty GC tissues and matched non-tumor adjacent tissues were obtained from patients who underwent surgical resection at the Liaoning Province Cancer Hospital and Institute between 2015 and 2017. Informed consent was obtained from patients before surgery at the Liaoning Province Cancer Hospital and Institute.
Separation of nuclear and cytoplasmic fractions
The PARIS kit (AM1921; Thermo Fisher Scientific, Yokohama, Japan) was used to divide the total cellular fractions into nuclear and cytoplasmic fractions according to the manufacturer’s protocol. The kit was able to isolate RNA from the same experimental sample, and guaranteed to separate the nuclear and cytoplasmic components before RNA was separated.
Real-time reverse transcription polymerase chain reaction (RT-PCR)
TRIzol (Invitrogen) cell separation reagent and the PURELINK miRNA Isolation Kit (Invitrogen) were used to extract total RNA according to the manufacturer’s instructions. Complementary DNA (cDNA) was generated from 500 ng of total RNA using the Promega miRNA first-strand cDNA core kit (Promega, Madison, WI, USA). Real-time PCR (LightCycler 480; Roche AG, Basel, Switzerland) was performed using the SYBR Master Mixture (Takara Bio, Inc., Kusatsu, Japan). Each sample was analyzed in triplicate. U6 DNA was used as the loading control. Fold changes in RNA expression among different cells were determined by 2− △△CT normalization.
Western blot analysis
Samples of equal amounts of cell protein (20 μg) were separated on a 10–15% SDS polyacrylamide gel and transferred to PVDF membranes. After blotting, the membranes were blocked in TBS-Tween buffer containing 20 mM Tris–HCl, 5% nonfat milk, 150 mM NaCl, and 0.05% Tween-20 (pH 7.5) for 1 h at 21 °C, and then incubated with primary antibodies against SNAI1(1:400, Abcam, Cambridge, UK), N-cadherin, Vimentin, E-cadherin and β-catenin (1:200, Boster Biological Technology, Pleasanton, CA, USA) and β-actin (1:4000, Santa Cruz Biotechnology, Santa Cruz, CA, USA) overnight at 4 °C, and finally incubated with secondary antibody (1:5000, Santa Cruz Biotechnology). β-actin served as a control for protein quantity. The gray value of the expression of all proteins was measured using ImageJ software (NIH, Bethesda, MD, USA). Data are presented as averages of the results of three independent experiments.
Lentivirus vector system, plasmids and cell transfection
Lentiviruses (LV) carrying shRNA sequences targeting human HIF-1α and siRNA sequences targeting human PCGEM1 were obtained from GeneChem (Shanghai, China). The viruses and Polybrene reagent (Abbott Laboratories, Chicago, IL, USA) were used to infect the cells. GC cells were cultured for 72 h in medium containing puromycin for cell screening. Western blotting and RT-PCR were performed to identify and verify clones with stable HIF-1α knockdown. Full-length human SNAI1 cDNA was generated by PCR and subcloned into the pcDNA 3.1 vector. SGC-7901 and BGC-823 cells used in the in vitro experiments were transfected with si-PCGEM1, and si-PCGEM1 + pcDNA3.1- SNAI1 plasmid in combination or alone using Lipofectamine 2000 (Invitrogen) for 24 h.
Scrape motility and transwell invasion assays
Cell migration was evaluated by the scrape motility assay using culture inserts (Ibidi, Regensburg, Germany). Untreated and infected SGC-7901 and GBC-823 cells were plated into culture inserts. After 24 h incubation, a wound gap was created by removing the inserts. Images of wound monolayers were acquired using an inverted microscope (XDS-100, Shanghai Caikon Optical Instrument Co., Ltd., Shanghai, China) at 0 and 24 h post-wounding.
Cell invasiveness was determined by the transwell invasion assay. Untreated and infected SGC-7901 and GBC-823 cells were plated into transwell upper chambers and coated with gelatin. Then, 600 μL of 30% FBS (Fetal Bovine Serum) was added as a chemoattractant into the lower chambers (Costar, Lowell, MA, USA). The cells were then fixed with methanol and stained with hematoxylin and eosin (Sigma-Aldrich, St. Louis, MO, USA) following incubation for 24 h. Cells were removed from the upper filter surface and cells migrating to the lower filter surface were counted as migrated cells under a microscope at 200 × magnification. Migrated cells were counted in five fields on each filter, with the average representing the number of migrating cells per field.
Statistical analysis
The Statistical Package for Social Sciences (SPSS; IBM, Armonk, NY, USA) version 19.0 was used for statistical analysis. All data are presented as mean ± SD (standard deviation). The Student’s t test was used when the variance between groups was similar; otherwise, the Wilcoxon-signed rank test was used. One-way analysis of variance (ANOVA) was used to compare multiple groups. Differences at P < 0.05 were considered statistically significant.
Results
PCGEM1 is overexpressed in human GC
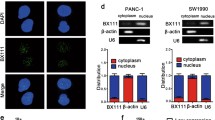
The RT-PCR results showed that PCGEM1 was overexpressed in BGC-823 and SGC-7901 cells relative to their levels in control GES-1 cells (Fig. 1a, P < 0.05) under 20% O2.We also examined PCGEM1 expression by RT-PCR to investigate its role in GC tissue. Expression levels in 40 GC tissue samples were examined and compared with adjacent non-cancerous tissues. PCGEM1 expression was observed in all GC tissue samples and was up-regulated in GC samples compared to the levels in adjacent non-cancerous tissues (Fig. 1b). In addition, the results of nuclear/cytoplasmic RNA fractionation in the subcellular distribution assay confirmed that PCGEM1 was mainly located in the cytoplasm (Fig. 1c, d). Taken together, these results showed that PCGEM1 was overexpressed in GC.
The expression and distribution of PCGEM1 in human GC. a PCGEM1 expression in GC cell lines (SGC-7901 and BGC-823) and the human normal gastric epithelial cell line (GSE-1) by RT-PCR. b PCGEM1 expression in GC tissue compare to paired adjacent tissue in 40 patients. c, d The expression level of PCGEM1 in the subcellular fractions of SGC-7901 and BGC-823 cells was detected by RT-PCR. U6 and β-actin were used as nuclear and cytoplasmic markers, respectively. U6 was used as a loading control in RT-PCR; n = 3, *P < 0.05
PCGEM1 is a hypoxia-responsive lncRNA in GC cells
To investigate whether PCGEM1 overexpression was induced by hypoxia, PCGEM1 expression levels were detected at 1% O2 and 20% O2. Under hypoxic conditions, PCGEM1 was strongly up-regulated (Fig. 2a). The expression levels were detected at 0, 12, 24, 48 and 72 h, and dysregulation initially appeared at 0 and reached a peak at 24 h, after which the levels gradually decreased, but were still much higher than under normoxia conditions (Fig. 2b).
PCGEM1 is up-regulated in human GC cell lines, and hypoxia (1% O2) regulates the expression of PCGEM1 in GC cells. a PCGEM1 is up-regulated under hypoxic culture conditions in GC cells. b Following hypoxia exposure, the expression levels of PCGEM1 was detected by RT-PCR at 0, 12, 24, 48 and 72 h after hypoxia exposure. c–e RT-PCR and GFP fluorescence showing the efficiency of HIF-1α knockdown compared with that of the scrambled control in GC cells. f GC cells were transfected with HIF-1α shRNA; PCGEM1 levels was determined by RT-PCR. U6 was used as a loading control; n = 3, *P < 0.05
To confirm delivery of lentivirus (LV)-HIF-1α or LV-control into GC cells (NC), transfected cells were visualized by GFP fluorescence. Figure 2e shows that numerous cell bodies were highly fluorescent, indicating that the lentivirus was successfully transfected into GC cells. To ensure the efficiency of interference and avoid off-target effects, RT-PCR assays were performed. The results revealed that HIF-1α mRNA expression was significantly reduced after infection with either (LV)-HIF-1α or LV-control (Fig. 2e, P < 0.05). The RT-PCR results showed that, compared with the scrambled control, HIF-1α knockdown at the mRNA level was effective. The maximum knockdown efficiency observed was for shRNA-HIF-1α-II (Fig. 2c, d).
As HIF-1α expression is inhibited by LV infection, down-regulated PCGEM1 levels in GC cells were measured by RT-PCR (Fig. 2f). The results indicated that PCGEM1 is a HRL, and its expression is associated with HIF-1α.
Suppression of PCGEM1 expression affects the invasion and metastasis of GC cells
To study the biology of PCGEM1 in GC, the GC cell lines SGC7901 and BGC-823 were transfected with PCGEM1-specific siRNAs or a control siRNA (1% O2). Two siRNAs targeting PCGEM1 were tested (si-PCGEM1#1 and si-PCGEM1#2), and si-PCGEM1#1 was more effective in suppressing PCGEM1 expression and was selected for subsequent research. To assess the effect of PCGEM1 on cell invasion and metastasis, transwell experiments and scrape motility assays were performed in vitro. These experiments showed that reduced PCGEM1 expression significantly inhibited the invasion and metastasis of GC cells in the transwell (Fig. 3b, c, P < 0.05) and scrape motility assays (Fig. 3e–f, P < 0.05). These observations indicated that PCGEM1 is a positive metastatic regulator of GC.
PCGEM1 is involved in cell invasion of gastric cancer. a GC cells transfected with si-PCGEM1 or NC were confirmed by RT-PCR. U6 was used as a loading control in RT-PCR. b, c Transwell assays were used to evaluate the role of PCGEM1 in invasion in PCGEM1-knockdown. d–f Scrape motility assays were monitored for 24 h in PCGEM1-knockdown GC cells. In all figures, 200 × magnification was used. n = 3, *P < 0.05
PCGEM1 regulates the expression of SNAI1 in GC cells
As EMT is one of the key factors in invasion and metastasis, we determined whether PCGEM1 affected invasion and metastasis of GC through EMT. We assessed the expression of SNAI1 with PCGEM1-knockdown under hypoxic conditions (1% O2). The RT-PCR and Western-blot results showed that SNAI1 was down-regulated by PCGEM1 (Fig. 4a, b, P < 0.05). To confirm the effect of PCGEM1 on the biological function of GC and to further verify that it is closely related to SNAI1, we stably suppressed PCGEM1 expression and overexpressed SNAI1. Transwell experiments and scrape motility assays were performed to investigate the effect of PCGEM1 and SNAI1 on cell invasion and metastasis. The results showed that reduced PCGEM1 expression significantly inhibited the invasion and metastasis of GC cells, and this decrease was partially abolished by overexpression of SNAI1 (Fig. 4c–f, P < 0.05).
PCGEM1 promotes GC invasion and metastasis via SNAI1. a, b Inhibition of PCGEM1 expression by LV infection downregulated SNAI1 levels in GC cells as measured by RT-PCR and western-blot. U6 and β-actin were used as a loading control in RT-PCR and western-blot. c, d Transwell assays were used to evaluate the association of PCGEM1 and SNAI1 in invasion in PCGEM1-knockdown and PCGEM1-knockdown + SNAI1-overexpression GC cells. e, f Scrape motility assays were monitored for 24 h in PCGEM1-knockdown and PCGEM1-knockdown + SNAI1-overexpression GC cells. In all figures, 200 × magnification was used. n = 3, *P < 0.05
PCGEM1 and SNAI1 regulate epithelial-mesenchymal transition in GC
To clarify the association between PCGEM1 and EMT, we next examined EMT markers in PCGEM1-knockdown and PCGEM1-knockdown + SNAI1-overexpressing GC cells (1% O2). Mesenchymal markers N-cadherin and Vimentin were suppressed due to lack of PCGEM1, and were partly rescued by overexpression of SNAI1 (Fig. 5a–c, P < 0.05). However, epithelial markers E-cadherin and β-catenin up-regulated PCGEM1-knockdown, and the overexpression of SNAI1 reversed this phenomenon (Fig. 5a, e, f, P < 0.05).
PCGEM1 regulated EMT via SNAI1. a PCGEM1-knockdown inhibits SGC-7901 and BGC-823 EMT. b, c Mesenchymal markers N-cadherin and Vimentin were suppressed when lack of PCGEM1, and partly rescued by overexpressed SNAI1. d, e Epithelial markers E-cadherin and β-catenin are up-regulated when lack of PCGEM1, and partly rescued by overexpressed SNAI1. β-Actin was used as a loading control; n = 3, *P < 0.05
Discussion
Gastric cancer metastasis is a major challenge in clinical treatment. Hypoxia and the HIF-signaling pathway are triggers in the metastatic cascade. Individual and collective tumor cells take advantage of multiple mechanisms to migrate and invade, and EMT is one of the most important mechanisms. The overexpression of HIFs is sufficient to induce EMT and promote metastasis in various cancer cell types [5]. It has been shown that HIFs target the hypoxia-response elements (HREs) of key EMT transcription factors to regulate EMT, such as ZEB1, Snail, and Twist [19]. However, with the in-depth understanding of the mechanism of lncRNA, accumulating evidence supports the involvement of HRLs in this biological process, which functions as a “guide” or “scaffold” [20]. The imprinted oncofetal lncRNA H19 was the first reported HRL [21]. The overexpression of H19 is related to the malignant phenotype: angiogenesis, cell survival, and proliferation [22]. In addition, the most well-known HRL, HOX transcript antisense intergenic RNA (HOTAIR), is the first lncRNA involved in tumorigenesis and metastasis, and predicts a negative prognosis in a range of cancer types [11]. Furthermore, other HRLs, such as urothelial carcinoma associated 1 (UCA1) and metastasis-associated lung adenocarcinoma transcript 1 (MALAT1), have been confirmed. The classic HIF-HRLs interactive mechanism involves HIF-1 binding to the HREs under hypoxia. Unfortunately, there is little information available on the mechanism of HRLs involved in the development of GC under hypoxia. In this study, we found that the lncRNA PCGEM1 is overexpressed in GC cells and tissues compared with normal gastric epithelial cells and adjacent non-tumor tissues. Further examination showed that the expression of PCGEM1 was strongly up-regulated under hypoxic conditions, and was associated with the expression of HIF-1α. These findings are similar to the overexpression of PCGEM1 under hypoxia in colorectal cancer [23]. These results indicate that PCGEM1 may be a potential HRL.
The overexpression of PCGEM1 was initially confirmed in aggressive prostate cancer [24]. Subsequent studies found that the promoter of PCGEM1 can be combined by myocyte enhancer factor 2 (MEF2). Activated PCGEM1 was also found to decrease the expression of miR-148a and affect cell apoptosis [25]. Similarly, P54/nrb can also combine the promoter of PCGEM1. Overexpressed PCGEM1 can contribute to castration resistance in prostate cancer [26]. Moreover, PCGEM1 also exacerbates the malignancy of ovarian cancer. It competitively combines with miR-129-5p and promotes the invasion and metastasis of ovarian cancer by targeting RhoA and regulating RhoA pathways [27] or STAT3 and regulating EMT [28]. The overexpression of PCGEM1 is also a biomarker of the malignancy of endometrial carcinoma [28] and glioma [29]. Our results show that suppressing the expression of PCGEM1 inhibits the invasion and metastasis of GC, and this phenomenon can be rescued by the up-regulation of SNAI1 which is a core transcription factor of EMT. We suspected that PCGEM1 might regulate the invasion and metastasis of GC by regulating EMT. When the expression of PCGEM1 was knocked down, the mesenchymal markers N-cadherin and Vimentin were suppressed, but the overexpression of SNAI1 reversed this phenomenon. In contrast to the mesenchymal markers, the epithelial markers E-cadherin and β-catenin were up-regulated when PCGEM1 was silenced. This phenotype was also reversed by overexpression of SNAI1. These findings show that PCGEM1, a HRL, promotes GC invasion and metastasis by regulating the expression of SNAI1. These results indicate that the oncogenic function of PCGEM1 in GC may be associated with EMT.
It is well known that lncRNAs mediate transcriptional or post-transcriptional gene regulation in tumors by four molecular functions: signal, guidance, scaffold and decoy. And lncRNA can recruit various molecules to form a scaffold, and uses specific signal components to perform related specific and biological functions. Previous studies have demonstrated that HIF-1α can bind to the SNAI1 promoter and play a biological role [19]. We suggest that PCGEM1, as a scaffold, combines with HIF-1α and SNAI1 to form a triple complex. However, the underlying mechanism needs to be confirmed in future studies.
Although we identified and verified the importance of PCGEM1 in the invasion and metastasis of GC using molecular biological approaches, the present study has some limitations. Firstly, the direct mechanism involved was not identified. Secondly, the expression of PCGEM1 and its functions in GC should be validated in in vivo experiments.
Conclusion
In conclusion, we identified PCGEM1 as a HRL, which was located in the cytoplasm, and the expression of PCGEM1 was associated with HIF-1α. Furthermore, we found that PCGEM1 may be involved in the invasion and metastasis of GC by participating in EMT. To the best of our knowledge, this is the first study to identify PCGEM1 as a potential biomarker of GC. In addition, SNAI1 is a potential downstream target gene of PCGEM1, and its expression is regulated by PCGEM1. Further research is warranted to address the limitations of this study, and future efforts will focus on the clinical application of PCGEM1 and hypoxia in GC treatment.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. A Cancer J Clin. 2017;7(1):7–30. https://doi.org/10.3322/caac.21387.
Wilson WR, Hay MP. Targeting hypoxia in cancer therapy. Nat Rev Cancer. 2011;11(6):393–410. https://doi.org/10.1038/nrc3064.
Koyasu S, Kobayashi M, Goto Y, Hiraoka M, Harada H. Regulatory mechanisms of hypoxia-inducible factor 1 activity: two decades of knowledge. Cancer Sci. 2018;109(3):560–71. https://doi.org/10.1111/cas.13483.
Tsai YP, Chen HF, Chen SY, Cheng WC, Wang HW, Shen ZJ, et al. TET1 regulates hypoxia-induced epithelial-mesenchymal transition by acting as a co-activator. Genome Biol. 2014;15(12):513. https://doi.org/10.1186/s13059-014-0513-0.
Rankin EB, Giaccia AJ. Hypoxic control of metastasis. Science (New York, NY). 2016;352(6282):175–80. https://doi.org/10.1126/science.aaf4405.
Zhang J, Wu Y, Lin YH, Guo S, Ning PF, Zheng ZC, et al. Prognostic value of hypoxia-inducible factor-1 alpha and prolyl 4-hydroxylase beta polypeptide overexpression in gastric cancer. World J Gastroenterol. 2018;24(22):2381–91. https://doi.org/10.3748/wjg.v24.i22.2381.
Djebali S, Davis CA, Merkel A, Dobin A, Lassmann T, Mortazavi A, et al. Landscape of transcription in human cells. Nature. 2012;489(7414):101–8. https://doi.org/10.1038/nature11233.
Schmitt AM, Chang HY. Long noncoding RNAs in cancer pathways. Cancer Cell. 2016;29(4):452–63. https://doi.org/10.1016/j.ccell.2016.03.010.
Lau E. Non-coding RNA: zooming in on lncRNA functions. Nat Rev Genet. 2014;15(9):574–5. https://doi.org/10.1038/nrg3795.
Brady LK, Wang H, Radens CM, Bi Y, Radovich M, Maity A, et al. Transcriptome analysis of hypoxic cancer cells uncovers intron retention in EIF2B5 as a mechanism to inhibit translation. PLoS Biol. 2017;15(9):e2002623. https://doi.org/10.1371/journal.pbio.2002623.
Wu X, Tudoran OM, Calin GA, Ivan M. The many faces of long noncoding RNAs in cancer. Antioxid Redox Signal. 2018;29(9):922–35. https://doi.org/10.1089/ars.2017.7293.
Liu L, Zhao X, Zou H, Bai R, Yang K, Tian Z. Hypoxia promotes gastric cancer malignancy partly through the HIF-1alpha dependent transcriptional activation of the long non-coding RNA GAPLINC. Front Physiol. 2016;7:420. https://doi.org/10.3389/fphys.2016.00420.
Chen WM, Huang MD, Kong R, Xu TP, Zhang EB, Xia R, et al. Antisense long noncoding RNA HIF1A-AS2 Is upregulated in gastric cancer and associated with poor prognosis. Dig Dis Sci. 2015;60(6):1655–62. https://doi.org/10.1007/s10620-015-3524-0.
Liu X, Wang Y, Sun L, Min J, Liu J, Chen D, et al. Long noncoding RNA BC005927 upregulates EPHB4 and promotes gastric cancer metastasis under hypoxia. Cancer Sci. 2018;109(4):988–1000. https://doi.org/10.1111/cas.13519.
Wang Y, Liu X, Zhang H, Sun L, Zhou Y, Jin H, et al. Hypoxia-inducible lncRNA-AK058003 promotes gastric cancer metastasis by targeting gamma-synuclein. Neoplasia (New York, NY). 2014;16(12):1094–106. https://doi.org/10.1016/j.neo.2014.10.008.
Yang Z, Wang R, Zhang T, Dong X. Hypoxia/lncRNA-AK123072/EGFR pathway induced metastasis and invasion in gastric cancer. Int J Clin Exp Med. 2015;8(11):19954–68.
Lamouille S, Xu J, Derynck R. Molecular mechanisms of epithelial-mesenchymal transition. Nat Rev Mol Cell Biol. 2014;15(3):178–96. https://doi.org/10.1038/nrm3758.
Srikantan V, Zou Z, Petrovics G, Xu L, Augustus M, Davis L, et al. PCGEM1, a prostate-specific gene, is overexpressed in prostate cancer. Proc Natl Acad Sci USA. 2000;97(22):12216–21. https://doi.org/10.1073/pnas.97.22.12216.
Luo D, Wang J, Li J, Post M. Mouse snail is a target gene for HIF. Mol Cancer Res. 2011;9(2):234–45. https://doi.org/10.1158/1541-7786.mcr-10-0214.
Deng SJ, Chen HY, Ye Z, Deng SC, Zhu S, Zeng Z. Hypoxia-induced LncRNA-BX111 promotes metastasis and progression of pancreatic cancer through regulating ZEB1 transcription. Oncogene. 2018. https://doi.org/10.1038/s41388-018-0382-1.
Matouk IJ, DeGroot N, Mezan S, Ayesh S, Abu-lail R, Hochberg A, et al. The H19 non-coding RNA is essential for human tumor growth. PLoS One. 2007;2(9):e845. https://doi.org/10.1371/journal.pone.0000845.
Matouk IJ, Raveh E, Abu-lail R, Mezan S, Gilon M, Gershtain E, et al. Oncofetal H19 RNA promotes tumor metastasis. Biochem Biophys Acta. 2014;1843(7):1414–26. https://doi.org/10.1016/j.bbamcr.2014.03.023.
Nishizawa Y, Konno M, Asai A, Koseki J, Kawamoto K, Miyoshi N, et al. Hypoxia stimulates the cytoplasmic localization of oncogenic long noncoding RNA LINC00152 in colorectal cancer. Int J Oncol. 2018;52(2):453–60. https://doi.org/10.3892/ijo.2017.4218.
Zhang A, Zhang J, Kaipainen A, Lucas JM, Yang H. Long non-coding RNA: a newly deciphered “code” in prostate cancer. Cancer Lett. 2016;375(2):323–30. https://doi.org/10.1016/j.canlet.2016.03.003.
Zhang S, Li Z, Zhang L, Xu Z. MEF2 activated long noncoding RNA PCGEM1 promotes cell proliferation in hormone refractory prostate cancer through downregulation of miR148a. Mol Med Rep. 2018;18(1):202–8. https://doi.org/10.3892/mmr.2018.8977.
Ho TT, Huang J, Zhou N, Zhang Z, Koirala P, Zhou X, et al. Regulation of PCGEM1 by p54/nrb in prostate cancer. Sci Rep. 2016;6:34529. https://doi.org/10.1038/srep34529.
Chen S, Wang LL, Sun KX, Liu Y, Guan X, Zong ZH, et al. LncRNA PCGEM1 induces ovarian carcinoma tumorigenesis and progression through RhoA pathway. Cell Physiol Biochem. 2018;47(4):1578–88. https://doi.org/10.1159/000490931.
Li Q, Shen F, Zhao L. The relationship between lncRNA PCGEM1 and STAT3 during the occurrence and development of endometrial carcinoma. Biomed Pharmacother Biomed Pharmacother. 2018;107:918–28. https://doi.org/10.1016/j.biopha.2018.08.091.
Park JY, Lee JE, Park JB, Yoo H, Lee SH, Kim JH. Roles of long non-coding RNAs on tumorigenesis and glioma development. Brain Tumor Res Treat. 2014;2(1):1–6. https://doi.org/10.14791/btrt.2014.2.1.1.
Funding
Liaoning S&T Project (20180550971). Liaoning provincial special Fund for central guiding local science and technology development plan (2018416017)
Author information
Authors and Affiliations
Contributions
ZJ performed the majority of experiments and analyzed the data and drafted the manuscript; ZZC, ZY designed the research; WY, YD, MXY conducted the molecular biology assays and assisted in writing the manuscript; GS, WY collected and analyzed the data; ZY provided critical revision of the manuscript for important intellectual content. JHY provided critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest related to this study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, J., Jin, H.Y., Wu, Y. et al. Hypoxia-induced LncRNA PCGEM1 promotes invasion and metastasis of gastric cancer through regulating SNAI1. Clin Transl Oncol 21, 1142–1151 (2019). https://doi.org/10.1007/s12094-019-02035-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-019-02035-9