Abstract
Purpose
Biomarkers, such as mutant RAS, predict resistance to anti-EGFR therapy in only a proportion of patients, and hence, other predictive biomarkers are needed. The aims were to identify candidate genes upregulated in colorectal cancer cell lines resistant to anti-EGFR monoclonal antibody treatment, to knockdown (KD) these genes in the resistant cell lines to determine if sensitivity to anti-EGFR antibody was restored, and finally to perform a pilot correlative study of EGR1 expression and outcomes in a cohort of metastatic colorectal cancer (mCRC) patients given cetuximab therapy.
Methods
Comparative expression array analysis of resistant cell lines (SW48, COLO-320DM, and SNU-C1) vs sensitive cell lines (LIM1215, CaCo2, and SW948) was performed. The highest up-regulated gene in each resistant cell line was knocked down (KD) using RNA interference, and effect on proliferation was assessed with and without anti-EGFR treatment. Expression of the candidate genes in patients’ tumours treated with cetuximab was assessed by immunohistochemistry; survival analyses were performed comparing high vs low expression.
Results
Genes significantly upregulated in resistant cell lines were EGR1 (early growth response protein 1), HBEGF (heparin-binding epidermal growth factor-like growth factor), and AKT3 (AKT serine/threonine kinase 3). KD of each gene resulted in the respective cells being more sensitive to anti-EGFR treatment, suggesting that the resistant phenotype was reversed. In the pilot study of mCRC patients treated with cetuximab, both median PFS (1.38 months vs 6.79 months; HR 2.77 95% CI 1.2–19.4) and median OS (2.59 months vs 9.82 months; HR 3.0 95% CI 1.3–23.2) were significantly worse for those patients with high EGR1 expression.
Conclusion
High EGR1 expression may be a candidate biomarker of resistance to anti-EGFR therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most common cancer worldwide and the second leading cause of cancer-related death in the Western world [1]. The treatment of mCRC has improved over recent years, with targeted therapies providing additional benefit to standard chemotherapy. One such treatment is monoclonal antibodies targeting EGFR, but not all tumours respond. It is well known that mutation in KRAS exon 2 occurs in up to 40% of mCRC and patients with this mutation do not respond to cetuximab [2]. Recent studies have revealed that while much less prevalent, mutations in KRAS exon 3 (4%) or 4 (3–6%), or exons 2 or 3 of NRAS (3–5%) are also associated with resistance to anti-EGFR therapy, making the mutation status of these clinically relevant [3,4,5] and is the new standard of care. The role of PIK3CA mutation and PTEN loss in conferring resistance to EGFR-directed therapy in colorectal cancer remains controversial [6]. BRAF mutation is confirmed as a poor prognostic factor; however, its role as a negative predictive marker of response to anti-EGFR therapy is still under investigation with one meta-analysis in first-line treatment with anti-EGFR monoclonal antibodies inconclusive [7], while other studies supported BRAF mutation assessment as a predictive marker [8], particularly in second and subsequent lines of treatment [9, 10]. Despite the new findings that extended RAS testing to identify KRAS exon 3/4 and NRAS exon 2/3 increases the proportion of potential responders, there remain a significant number of patients who will derive little or no benefit from cetuximab therapy [11, 12]. In the era of ‘precision medicine’, the determination of biomarkers that will predict those patients who will derive the greatest benefit from EGFR-targeted therapy is important to better select patients for this therapy. This would reduce unnecessary exposure to adverse effects of an ineffective therapy and permit an alternate therapeutic pathway to be offered in a timely fashion.
Materials and methods
Cell lines and reagents
The cell lines SW48, CaCo2, SNU-C1, SW948, and COLO-320DM were purchased from the American type culture collection (ATCC, Manassas, VA, USA). Cell line LIM1215 was a kind gift from the Ludwig Institute, Melbourne, Australia. The cell lines did not harbour any mutations known to be associated with resistance to anti-EGFR antibody treatment (https://cansar.icr.ac.uk/cansar/cell-lines). Cells were cultured in RPMI 1640 medium (Life Technologies, Carlsbad, CA, USA) supplemented with 10% fetal bovine serum, 100 U/mL penicillin, 100 µg/mL streptomycin, and 200 µg/mL glutamine (life technologies), at 37 °C in 5% CO2 incubator.
Patient tissue
To explore the predictive value of biomarkers in the outcome of mCRC patients treated with cetuximab, a pilot study was performed using primary tumour tissue sections from archived formalin-fixed paraffin-embedded tissue blocks from the CO.20 clinical trial [13]. The expression levels for HBEGF, EGR1, and AKT3 were determined in 15 tumours. Informed consent for biomarker studies was obtained from all patients at the time of recruitment.
Proliferation assay
Cells were seeded into 96-well plates and treated with 2 µg of anti-EGFR antibody (528:Sc-120; Santa Cruz Biotechnology, Santa Cruz, CA, USA). Untreated cells were included as a reference. After 72 h incubation at 37 °C in 5% CO2 incubator, cells were treated with 20 µL of the MTS/PMS solution (CellTiter 96® AQueous Assay kit, Promega, Madison, WI, USA) and absorbance read at 490 nm on the Fluostar Optima (BMG Labtech, Jena, Germany).
Gene expression array analysis
RNA was extracted from colon cancer cell lines using the PureLink RNA Mini Kit and quantified by NanoDrop 2000 spectrophotometer (both from Life Technologies, Carlsbad, CA, USA). RNA integrity (RIN score) was assessed using the Agilent 2100 Bioanalyzer (Agilent Technologies, Santa Clara, CA, USA). RNA (500 ng) was reverse-transcribed using the RT2 First Strand Kit (Qiagen, Valencia, CA, USA) as per the manufacturer’s protocol. The resulting cDNA was PCR amplified using the RT2 Profiler™ PCR Array Human EGF/PDGF-signalling pathway kit (PAHS-040Z, Qiagen) and run using the CFX96™ Real-Time PCR Detection System (Bio-Rad, Carlsbad, CA, USA). Each array plate contained a panel of 84 pathway-focused genes. The results were analysed using the RT2 Profiler™ PCR Array Data Analysis version 3.5 software provided online. The three candidate genes that showed the greatest upregulation in resistance cell lines relative to sensitive cells lines were selected for knockdown and anti-EGFR sensitivity studies.
Confirmation of over-expressed genes
Taqman probe assays (Life Technologies) for the candidate genes were used to confirm expression data from the arrays. Each cDNA sample of the cell lines was run in triplicate PCR and the results normalised against reference gene HPRT1 (2−ΔΔCt).
Knockdown of candidate genes using RNA interference
Briefly, cells were transfected with siRNA (Dharmacon ONTarget Plus, Life Technologies) targeting HBEGF, EGR1, and AKT3 using DharmaFECT transfection reagent (Life Technologies) according to the manufacturer’s instructions. Cells were plated in triplicate and the experiment repeated three times. RNA was extracted as before at 72 h post transfection for RT-PCR confirmation of knockdown. Protein was isolated at 96 h after transfection for western blot analysis: cells were lysed in RIPA buffer (Life Technologies) and the protein concentration determined using EZQ Assay (Life Technologies). Proteins (30 µg in Laemmli loading buffer) were separated by 12% SDS-PAGE (Mini-PROTEAN TGX stain-free gel, Bio-Rad) and transferred to polyvinylidene difluoride membranes (Bio-Rad). Target proteins were detected by chemiluminescence western blot detection system using mouse monoclonal antibodies (all at 1:1000 dilution): anti-HBEGF (ab66792), anti-EGR1 (ab55160), anti-AKT3 antibody (ab13919), anti-actin (ab8229) (all from Abcam, Cambridge, MA, USA), and goat anti-mouse horseradish peroxidase secondary antibody (Bio-Rad) at 1:2000 dilution. Blots were imaged using the LAS4000 and quantified using the image analysis software (Qiagen). Proliferation was measured as before to determine the resistance/sensitivity of these siRNA-treated cells to anti-EGFR antibody (Santa Cruz Biotechnology).
Immunohistochemistry
Antigen retrieval was performed by microwave-heating the sections (5 µm) in Target Retrieval Solution Tris–EDTA buffer pH 9 (DAKO, Denmark) for 20 min. Slides were incubated with either mouse anti-HBEGF (Abcam) at a dilution of 1:50, mouse anti-EGR1 (Abcam) at a dilution of 1:100, or mouse anti-AKT3 (Abcam) at a dilution of 1:100 at room temperature for 30 min and counterstained with haematoxylin. Staining was scored independently by two pathologists, using the staining intensity score 3+ (strong), 2+ (moderate) 1+ (weak), or 0 (negative), multiplied by the area (%) of positive cells. For the purpose of statistical analyses, the scores were ranked for each marker as either low expression (≤ median score) or high expression (> median score). An overall high rank score was defined as high expression for at least 2 markers.
Statistical analysis
Significant differences in gene expression results were determined using Student’s t test. The survival outcomes of patients according to each marker rank were summarized with the use of Kaplan–Meier curves, and the difference between these groups compared using the log-rank test (GraphPad Prism version 6.05 for Windows, GraphPad Software, La Jolla California USA). Progression-free survival (PFS), the primary endpoint was defined as the time from enrolment until documented evidence of disease progression, the occurrence of new disease or death from any cause. The secondary endpoints were overall survival (OS), defined as the time from enrolment date until death from any cause, and objective response rate (ORR), defined according to the response evaluation criteria in solid tumours (RECIST) version 1.0. Fishers exact test (GraphPad Prism) was used to determine association between high and low levels of each marker with any tumour response (partial response or stable disease) vs no response (progressive disease).
Results
Determination of cell lines resistant vs sensitive to anti-EGFR antibody
SW48 and SNU-C1 and COLO-320DM cell lines showed resistance to anti-EGFR treatment, with a mean of 70, 83.8, and 68.3% cell proliferation, respectively, relative to untreated control cells, while LIM1215, CaCo2, and SW948 were significantly more sensitive to the treatment with 18.6, 42, and 29.1% proliferation, respectively (p = 0.006) (Fig. 1). A cut-off point of 50% was used to determine resistance or sensitivity of the CRC cell lines to anti-EGFR treatment [14].
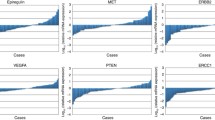
Determination of biomarkers upregulated in resistant cell lines
The RT2 Profiler Array PCR Data Analysis version 3.5 software (Qiagen) was used to determine candidate biomarkers that were upregulated in anti-EGFR resistant CRC cell lines. Each of the anti-EGFR resistant cell lines was compared with the sensitive CRC cell lines, nine combinations in total. Thirty percent (25/84) of genes on the array were upregulated >threefold in resistant relative to sensitive cell lines, with five genes upregulated in common in two or more cell lines (Venn diagram, Online Resource Fig. 1) Candidate genes were selected from those significantly upregulated more than threefold in resistant cell lines in the largest number of comparisons. The top three candidates that fulfilled these criteria were early growth response protein 1 (EGR1), Heparin-binding epidermal growth factor-like growth receptor (HBEGF), and v-akt murine thymoma viral oncogene homolog 3 (AKT3) (Table 1). The differential expression of the three candidate genes was confirmed using qRT-PCR. When compared to all the sensitive cell lines, the highest up-regulated genes in the resistant cell lines were EGR1 in SW48, HBEGF in SNUC1, and AKT3 in COLO320-DM (Table 1).
Knockdown of over-expressed biomarkers in resistant cell lines
At the mRNA level (qRT-PCR), EGR1 expression was reduced by 85.6% in SW48, HBEGF expression by 79.4% in SNUC1, and AKT3 expression by 95.3% in COLO-320DM (Fig. 2a). Quantification of bands on the western blots showed knockdown at the protein level of 48, 52, and 47% for HBEGF, EGR1, and AKT3 in the respective cell lines (Fig. 2b, c).
siRNA knockdown. a Gene expression (qRT-PCR) 72 h post siRNA transfection of HBEGF in SNUC1 cells, EGR1 in SW48 cells, and AKT3 in COLO320 cells. ****p < 0.0001 (ANOVA). b Western blots showing protein knockdown in specific siRNA-treated cells: (a) SNUC1, (b) SW48, and (c) COLO320. c Quantification of protein bands normalised to β actin loading control and mock transfection control showed 48, 52, and 47% knockdown of HBEGF, EGR1, and AKT3 in the respective cell lines
Proliferation assays of siRNA-treated cells to assess sensitivity to anti-EGFR treatment
After 24 h treatment of siRNA-transfected SNUC1, SW48 and COLO320 cells with anti-EGFR, together with untransfected and mock transfected cells, the mean proliferation rate for HBEGF-, EGR1-, and AKT3-knocked down cells was 46.9, 49.1, and 64.1%, respectively. Figure 3 shows that knockdown of the respective genes in the resistant cell lines has resulted in the cell lines being significantly more sensitive to anti-EGFR treatment (p < 0.0001).
Proliferation rate for knockdown (KD) cells. After treatment with 2 µg anti-EGFR antibody for 24 h, normalised to isotype control antibody treated cells (100%) KD of each gene resulted in significantly increased sensitivity of the respective cells to anti-EGFR treatment compared to the siRNA negative (scrambled) controls: ****p < 0.0001 (ANOVA) (n = 3). Grey bars, SNUC1 cells (HBEGF KD); black bars SW48 cells (EGR1 KD); white bars COLO320-DM (AKT3 KD)
Expression levels of biomarkers in tumour sections
IHC staining was scored independently by two pathologists without knowledge of clinical details. For the purpose of dichotomisation, scores were ranked as high (≥ the median score for each marker), or low (< median score) (Table 2). Representative images of high- and low-scored staining of each marker in patient’s tumour tissue are shown in Fig. 4. HBEGF was found to be highly expressed (> median) in 7/15 (47%) patients; EGR1 was highly expressed in 5/15 (33%) and AKT3 was highly expressed in 7/15 (47%).
Tumour response and survival analyses
Fisher’s exact test showed a trend for correlation between high levels of EGR1 marker and lack of tumour response (progressive disease), p = 0.08, while no significant association was found for HBEGF or AKT3. Kaplan–Meier analysis based on individual markers showed that only high EGR1 expression was associated with significantly worse PFS: 1.38 months (mo) (high rank) vs 6.79 months (low rank); HR 2.77 95% CI 1.2–19.4, p = 0.04 and OS (2.59 months vs 9.82 months; HR 3.0 95% CI 1.3–23.2, p = 0.03) (Fig. 5a, b). There was no significant difference in PFS or OS between patients with high rank vs low rank for the other markers AKT3, HBEGF, or for combined overall rank (> two out of three markers with high rank) compared to patients with an overall low rank. The median PFS for overall high rank was 4.0 vs 6.5 months for low rank; HR 1.96, 95% CI 0.83–6.78. p = 0.1 log-rank test (NS), while the median OS was 5.9 (high rank) vs 8.5 months (low rank); HR 1.3, 95% CI 0.5–3.6 (NS) (Fig. 5c forest plot and Online Resource Fig. 2). Correlation between RECIST scores and EGR1 expression levels is shown in a waterfall plot (Fig. 5d).
Survival analyses. a, b Kaplan–Meier (KM) curves showing PFS (a) or OS (b) according to high vs low expressions of EGR1; c forest plot showing only EGR1 high expression to be significantly associated with poorer PFS; d waterfall plot showing correlation between RECIST scores and EGR1 expression levels
Discussion
Cetuximab, a monoclonal antibody targeting EGFR, is now an important part of mCRC therapy for patients with RAS WT, yet there remains a proportion of patients who do not respond to this therapy. Importantly, these patients may suffer adverse effects without benefit, and this, coupled with the high costs of treating patients, has prompted the investigation of other biomarkers to better define patient selection.
In this pilot study, we used a gene expression array related to the EGF/PDGF-signalling pathways and identified the highest differentially up-regulated gene in each of the resistant CRC cell lines: HBEGF in SNUC1, EGR1 in SW48, and AKT3 in COLO320. We found that knockdown of each of these genes by RNA interference in vitro reversed the resistant phenotype of the respective cells, suggesting a role in cetuximab resistance mechanisms. All three have a relevant role in tumour growth and progression. HBEGF is a member of the EGF-like growth factor family, and its expression is altered in a number of cancers, including CRC: it is a potent inducer of tumour growth and angiogenesis (reviewed in [15]; EGR1 is a transcription factor implicated in regulating mitotic cell fate [16], while AKT3, a serine/threonine kinase, is part of the AKT-PI3K signalling pathway that is activated in many malignancies [17]. Constitutive upregulation of these factors would, therefore, bypass EGFR-initiated signalling; hence, the cells would show resistance to anti-EGFR treatment.
Our pilot study of survival analyses of mCRC patients treated with cetuximab in the chemo-refractory setting showed that those with low tumour EGR1 expression had significantly longer PFS and OS than those with high EGR1. EGR1 level also showed a trend toward association with tumour response. Taken together, these data suggest that EGR1 level may be a useful marker of resistance to cetuximab therapy. While other studies have shown that EGR1 is constitutively expressed at a relatively high level in colon carcinoma cell lines [18] and upregulated in early onset colorectal cancers [19], and in the majority of advanced colon cancer tumours [20], this is the first study to report the association between EGR1 levels and tumour response or survival outcomes with cetuximab therapy.
In the presence of EGFR inhibition, tumour growth may be driven by constitutive activation of the RAS-MAPK and PI3K pathways via mutations in oncogenes, such as RAS, BRAF, and PI3KCA or loss of the tumour suppressor gene PTEN [21]. In addition, tumour proliferation may be driven by activation of parallel-signalling pathways, such as HER2 [22], HER3 [23], or HGF-MET [24]. The oncogenic activation of these various pathways results in persistence of ERK signalling and upregulation of the transcription factor EGR1, essential for mitosis [25]. EGR1 has also been found to act as an inhibitor of the death receptor 5-induced apoptotic pathway [18] resulting in increased cell survival contributing to tumour growth and progression. Together, these factors result in circumvention of EGFR inhibition and impairment of the clinical efficacy of anti-EGFR monoclonal antibodies.
The management of mCRC is continuing to evolve as additional predictive biomarkers are identified and the expanded tumour profiling should improve prognostication and prediction of treatment efficacy. Patients eligible for anti-EGFR-targeted therapy stand to benefit from better selection criteria based on such markers, ensuring maximum efficacy of a given treatment, and at the same time avoiding potential toxicities and delays due to ineffective therapies. The results of this pilot study suggest that EGR1 expression may be a further candidate predictive marker, which must be confirmed in additional clinical trial cohorts using anti-EGFR therapies, including the anti-EGFR monoclonal antibody panitumumab.
References
Roda D, Cervantes A. Biomarkers in colorectal cancer: the future is getting closer. Clin Transl Oncol. 2010;12(4):241–2. doi:10.1007/s12094-010-0498-4.
Karapetis CS, Khambata-Ford S, Jonker DJ, O’Callaghan CJ, Tu D, Tebbutt NC, et al. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008;359(17):1757–65.
Douillard J-Y, Oliner KS, Siena S, Tabernero J, Burkes R, Barugel M, et al. Panitumumab–FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med. 2013;369(11):1023–34. doi:10.1056/NEJMoa1305275.
Clarke SJ, Karapetis CS, Gibbs P, Pavlakis N, Desai J, Michael M, et al. Overview of biomarkers in metastatic colorectal cancer: tumour, blood and patient-related factors. Crit Rev Oncol/Hematol. 2013;85(2):121–35.
Peeters M, Oliner KS, Parker A, Siena S, Van Cutsem E, Huang J, et al. Massively parallel tumor multigene sequencing to evaluate response to panitumumab in a randomized phase III study of metastatic colorectal cancer. Clin Cancer Res. 2013;19(7):1902–12. doi:10.1158/1078-0432.ccr-12-1913.
Misale S, Di Nicolantonio F, Sartore-Bianchi A, Siena S, Bardelli A. Resistance to anti-EGFR therapy in colorectal cancer: from heterogeneity to convergent evolution. Cancer Discov. 2014;4(11):1269–80. doi:10.1158/2159-8290.CD-14-04622159-8290.CD-14-0462.
Zhou M, Yu P, Hou K, Fu L, Chen Y, Qu J, et al. Effect of RAS status on anti-EGFR monoclonal antibodies +5-FU infusion-based chemotherapy in first-line treatment of metastatic colorectal cancer: a meta-analysis. Meta Gene. 2016;9:110–9. doi:10.1016/j.mgene.2016.05.001.
Pietrantonio F, Petrelli F, Coinu A, Di Bartolomeo M, Borgonovo K, Maggi C, et al. Predictive role of BRAF mutations in patients with advanced colorectal cancer receiving cetuximab and panitumumab: a meta-analysis. Eur J Cancer. 2015;51(5):587–94.
Bronte G, Silvestris N, Castiglia M, Galvano A, Passiglia F, Sortino G, et al. New findings on primary and acquired resistance to anti-EGFR therapy in metastatic colorectal cancer: do all roads lead to RAS? Oncotarget. 2015;6(28):24780–96.
Van Cutsem E, Cervantes A, Adam R, Sobrero A, Van Krieken JH, Aderka D, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;. doi:10.1093/annonc/mdw235.
Karapetis CS, Jonker D, Daneshmand M, Hanson JE, O’Callaghan CJ, Marginean C, et al. PIK3CA, BRAF, and PTEN status and benefit from cetuximab in the treatment of advanced colorectal cancer—results from NCIC CTG/AGITG CO.17. Clin Cancer Res. 2014;20(3):744–53. doi:10.1158/1078-0432.ccr-13-0606.
Sree Kumar S, Price TJ, Townsend A, Hocking C, Hardingham JE. Predictive biomarkers of response to anti-EGF receptor monoclonal antibody therapies. Colorectal Cancer. 2014;3:223–32.
Siu L, Shapiro J, Jonker D, Karapetis C, Zalcberg J, Simes J et al. Phase III randomized trial of cetuximab (CET) plus either brivanib alaninate (BRIV) or placebo in patients (pts) with metastatic (MET) chemotherapy refractory K-RAS wild-type (WT) colorectal carcinoma (CRC): The NCIC Clinical Trials Group and AGITG CO.20 trial. J Clin Oncol. 2012;30(4 (suppl)):386.
Jhawer M, Goel S, Wilson AJ, Montagna C, Ling YH, Byun DS, et al. PIK3CA mutation/PTEN expression status predicts response of colon cancer cells to the epidermal growth factor receptor inhibitor cetuximab. Cancer Res. 2008;68(6):1953–61.
Miyata K, Yotsumoto F, Nam S, Kuroki M, Miyamoto S. Regulatory mechanisms of the HB-EGF autocrine loop in inflammation, homeostasis, development and cancer. Anticancer Res. 2012;32(6):2347–52.
Topham C, Tighe A, Ly P, Bennett A, Sloss O, Nelson L, et al. MYC is a major determinant of mitotic cell fate. Cancer Cell. 2015;28(1):129–40. doi:10.1016/j.ccell.2015.06.001.
Agarwal E, Brattain MG, Chowdhury S. Cell survival and metastasis regulation by Akt signalling in colorectal cancer. Cell Signal. 2013;25(8):1711–9. doi:10.1016/j.cellsig.2013.03.025.
Mahalingam D, Natoni A, Keane M, Samali A, Szegezdi E. Early growth response-1 is a regulator of DR5-induced apoptosis in colon cancer cells. Br J Cancer. 2010;102(4):754–64. doi:http://www.nature.com/bjc/journal/v102/n4/suppinfo/6605545s1.html.
Hong Y, Ho KS, Eu KW, Cheah PY. A susceptibility gene set for early onset colorectal cancer that integrates diverse signaling pathways: implication for tumorigenesis. Clin Cancer Res. 2007;13(4):1107–14. doi:10.1158/1078-0432.CCR-06-1633.
Song LJ, Liu RJ, Zeng Z, Alper SL, Cui HJ, Lu Y et al. Gastrin inhibits a novel, pathological colon cancer signaling pathway involving EGR1, AE2, and P-ERK. J Mol Med (Berlin, Germany). 2012;90(6):707–18. doi:10.1007/s00109-011-0851-2.
Scaltriti M, Baselga J. The epidermal growth factor receptor pathway: a model for targeted therapy. Clin Cancer Res. 2006;12(18):5268–72. doi:10.1158/1078-0432.ccr-05-1554.
Kavuri SM, Jain N, Galimi F, Cottino F, Leto SM, Migliardi G, et al. HER2 activating mutations are targets for colorectal cancer treatment. Cancer Discov. 2015;5(8):832–41. doi:10.1158/2159-8290.cd-14-1211.
Cushman SM, Jiang C, Hatch AJ, Shterev I, Sibley AB, Niedzwiecki D, et al. Gene expression markers of efficacy and resistance to cetuximab treatment in metastatic colorectal cancer: results from CALGB 80203 (alliance). Clin Cancer Res. 2015;21(5):1078–86. doi:10.1158/1078-0432.CCR-14-2313.
Bigatto V, De Bacco F, Casanova E, Reato G, Lanzetti L, Isella C, et al. TNF-α promotes invasive growth through the MET signaling pathway. Mol Oncol. 2015;9(2):377–88. doi:10.1016/j.molonc.2014.09.002.
Zwang Y, Oren M, Yarden Y. Consistency test of the cell cycle: roles for p53 and EGR1. Cancer Res. 2012;72(5):1051–4. doi:10.1158/0008-5472.can-11-3382.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Grant funding
Grant funding was received from the Cancer Council of South Australia (APP1028595).
Conflict of interest
Professor Timothy Price is an advisory board member of Amgen and Merck; no other conflicts of interest to report.
Ethical standards
All studies using human tissue have been approved by the ethics committee of The Queen Elizabeth Hospital under the governance of the Central Adelaide Local Health Network and have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kumar, S.S., Tomita, Y., Wrin, J. et al. High early growth response 1 (EGR1) expression correlates with resistance to anti-EGFR treatment in vitro and with poorer outcome in metastatic colorectal cancer patients treated with cetuximab. Clin Transl Oncol 19, 718–726 (2017). https://doi.org/10.1007/s12094-016-1596-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-016-1596-8