Abstract
Introduction
Olfaction is a highly emotionally charged sense and contributes to our quality of life, which olfactory impairment or dysosmia thus strongly impacts. The aim of the present study was to examine how olfactory deficits alter eating behavior, which is a pillar of health and well-being.
Methods
Patients with quantitative smell impairment and control participants were asked to perform a series of chemosensory tasks: odor identification and ratings of odor intensity, pleasantness, familiarity, irritation, and edibility. They also filled out a detailed food questionnaire.
Results
Results showed significant decrease in olfactory function in smell-impaired patients. Although no significant consequences of dysosmia were found for most aspects of food preferences and culinary habits, the patients were less attracted than controls by novel foods and tended to experience less pleasure when eating. They also used significantly more condiments such as sugar, mayonnaise, or sour cream to make their dishes tasty.
Conclusions
Olfactory impairment has a clear effect on certain aspects of eating behavior.
Implications
These findings highlight the compensatory mechanisms that go along with dysosmia. This also reflects the patients’ attempts to restore part of the lost flavor and its hedonic component through non-olfactory cues.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Olfactory disorder, or dysosmia, mainly consists in anosmia (absence of olfactory function) or hyposmia (decreased sensitivity to odorants or decreased odor identification). Dysosmia originates from a variety of causes (e.g., acute or chronic infection, tumor, head trauma, allergy, pollutants, medication) (Hummel et al. 2017). The prevalence of dysosmia in the general population is high. Several studies performed in various western countries revealed that 10 to 15% of young adults and 20 to 30% of elderly people exhibit smell deficits (Murphy 2002; Bramerson et al. 2004; Landis et al. 2004; Hummel et al. 2007; Joussain et al. 2016).
Olfactory deficits are not without effects on the quality of life, especially with regard to behavior and mental health. In particular, patients with impaired sense of smell are more likely to (i) sustain household accidents (Santos et al. 2004); (ii) display depressive symptoms (Smeets and Veldhuizen 2009; Croy and Hummel 2017); (iii) show impairment in safety-related areas such as detection of fire, smoke, gas, or spoiled food; in personal hygiene (e.g., worries about body odor or bad breath); and in their sex life and social relationships (Croy et al. 2013); (iv) experience occupational problems in some specific cases (cooks or perfumers; (Keller and Malaspina 2013)); and (v) take repeated medical appointments if not counseled adequately (Landis et al. 2010).
However, food-related problems are by far the most frequent issues in smell impairment (Landis et al. 2010; Croy et al. 2014). Patients with smell deficits experience reduced richness of food perception, which may lead to reduced pleasure of eating, with consequent decrease in appetite. An important but understudied issue in patients with dysosmia concerns compensation mechanisms. Croy and colleagues (Croy et al. 2014) noticed that patients tend to compensate for olfactory loss by seeking trigeminal and textural sensations in eating. Mattes et al. (Mattes et al. 1990) observed that 42% of patients with olfactory loss increased their use of spices. Likewise, the use of salt increases in about one third of hyposmic patients (Henkin 2014). Finally, the most important food attributes for patients with dysosmia are texture (80%) followed by vision (20%) (Merkonidis et al. 2015).
The main aim of the present study was to better understand the compensation mechanisms that may accompany dysosmia, by examining which ingredients patients like to add to their dishes to make them tastier. A large panel of common condiments and other additional food items were considered. In addition, positive attitudes toward new foods (food neophilia) and pleasure experienced when eating were evaluated. Participants were also asked whether olfactory impairment had induced changes in their food preferences and culinary habits.
The secondary aim of this study was to specify dysosmia-related olfactory changes. The usual diagnostic signs of dysosmia are increased odor detection threshold and/or impaired odor identification ("namely the ability to name odor sources") (Hummel et al. 2007; Joussain et al. 2016); changes in other aspects of olfactory categorization, such as familiarity, pleasantness, or edibility, however, are less clear.
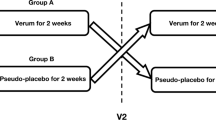
Two experiments were therefore conducted. In order to characterize a set of odors with representative categories to be used in the main study, we performed a first pilot study (experiment 1). Here, a set of eight odors covering important aspects of the olfactory perceptual space, including food and non-food odors (vegetal, body, and threatening odors), was characterized in normosmic individuals along various perceptual dimensions: not only identification and intensity, but also pleasantness, familiarity, edibility, and irritation. These eight odors were then used in the main study (experiment 2), in which a different sample of participants, including dysosmic patients and control participants, perceived these olfactory stimuli and rated them along the same perceptual dimensions (identification, intensity, pleasantness, familiarity, edibility, and irritation). In experiment 2, participants were also asked to fill in a detailed food questionnaire.
Methods
Experiment 1
Participants
One hundred and eleven volunteers participated in experiment 1 (mean age ± SEM 35.60 ± 1.64 years; 61 women and 50 men). The experimental procedure, conducted according to the ethical principles of the declaration of Helsinki, was explained in detail to each participant, who gave informed consent. The test was performed at home or during social, scientific, or cultural meetings or events in the city of Lyon, France.
Olfactory Stimuli
A total of eight odorants were used (within parentheses: “quality,” CID, volume/volume concentration): l-carvone (“mint”; 439,570; 22.5%), cis-3-hexen-1-ol (“grass”; 5,281,167; 28%), trans-anethole (“anise”; 637,563; 22.5%), valeric acid (“sweat”; 7991; 2.25%), alpha-pinene (“pine”; 6654; 22.5%), beta-ionone (“flower”; 638,014; 28%), isoamyl acetate (“banana”; 31,276; 5.6%), and tetrahydrothiophene (“gas”; 1127; 22.5%). Odorant molecules were trapped in tight aminoplast microcapsules (diameter, 4–8 μm). The microcapsule-based ink was printed on a cardstock (silk 250 g; dimensions, 11 cm × 21 cm). Each odorant was printed on a delimited area (2 cm2 disc). The odor was released by rubbing the printed microcapsule reserve (scratch-and-sniff device).
Note that the development of this paper olfactory test initially included a series of tests in order to verify that both the intensity and the quality of the smells were not distorted by the printing process. This phase was performed on a set of 12 odorant molecules. Among these 12 odorants, 4 odorants did not show a good reliability in that perception was not strong enough or odor quality was significantly distorted. For the remaining 8 odorants, we then performed another pilot study in 11 participants (mean age ± SD 39.36 ± 14.43; 3 males) who were asked to rate the intensity and the pleasantness of the stimuli. Results revealed that odorants were well perceived in a range of intensity of 1.6 (for flower) to 3.1 (for gas) (on a scale from 0 for “very weak,” to 4 for “very strong”). Pleasantness also varied across odorants from − 1.9 (for gas) to + 1.6 (for mint) (on a scale from − 2 for “very unpleasant” to + 2 for “very pleasant”). In terms of use, the test was developed so that it could be used only in a single experimental session.
Protocol
For each odorant, participants were required to perform six tasks.
(i) Odor identification was assessed by a multiple-choice procedure, consisting in selecting one out of four descriptors (within parentheses: target followed by 3 distractors): l-carvone (mint, nut, olive, onion), cis-3-hexen-1-ol (grass, leather, rubber, chocolate), trans-anethole (anise, cinnamon, fish, tea), valeric acid (sweat, apricot, caramel, paint), alpha-pinene (pine, tar, orange, cucumber), beta-ionone (flower, butter, pear, bread), isoamyl acetate (banana, almond, lemon, carrot), and tetrahydrothiophene (gas, vinegar, coffee, plastic). Participants were also asked to estimate ii) odor pleasantness (very unpleasant, unpleasant, neutral, pleasant, or very pleasant), iii) intensity (very weak, weak, medium, strong, or very strong), iv) familiarity (unknown, not well-known, fairly well-known, well-known, or very well-known), v) irritating character (not irritating, hardly irritating, possibly irritating, irritating, very irritating), and vi) edibility of the odor source (not edible, hardly edible, possibly edible, edible, very edible).
Experiment 2
Participants
Seventy-nine individuals were tested in three metropolitan areas (Lyon-Villefranche, Geneva, and Dresden) and divided into two groups according to known olfactory deficit: (i) dysosmic (n = 39; mean age ± SEM 55.72 ± 2.08 years; 22 women and 18 men) and (ii) normosmic control participants (n = 40; mean age ± SEM 56.82 ± 1.84 years; 22 women and 18 men) free of olfactory impairment. Diagnosis of dysosmia followed a three-step procedure by ENT physicians: interview, clinical examination (including nasal endoscopy), and olfactory screening (Sniffin’ Sticks test (Hummel et al. 2007)). For patients, disease duration ranged from 1 to 12 years; origins of the disease were varied: idiopathic (n = 9), allergy (n = 2), polyposis (n = 4), post-upper respiratory tract infection (n = 19), post-traumatic (n = 4), and post-surgery (n = 2); and functional status ranged from hyposmia to anosmia. The experimental procedure, conducted according to the ethical principles of the declaration of Helsinki, was explained in detail to each participant, who gave informed consent.
Olfactory Tasks
Participants completed the same olfactory tasks using the same set of odors as in experiment 1.
Food Questionnaire
The food questionnaire comprised five items and was administered as follows: (1) Do you ever taste new foreign dishes or drinks? (never, rarely, sometimes, often, always; only one choice possible); (2) Do you enjoy eating? (never, rarely, sometimes, often, always; only one choice possible); (3) In general, what do you like to add to your dishes to make them tastier? (sugar, ketchup, mayonnaise, spices, salt, vinegar, butter, herbs, pepper, mustard, soya sauce, olive oil, lemon, sour cream, syrups; several choices possible); (4) Do you have any preferences for vegetables, fruits, meat, fish, starchy foods, dairy products? (for each: a little, medium, a lot); (5) Including lunch and dinner, on average, how many times a week do you: (i) cook for yourself and/or for others (0 to 14), (ii) eat prepared meals at home or outside (0 to 14), (iii) eat in a restaurant (0 to 14). Participants also filled in questionnaires on demographic items (date, time of test, age, gender, weight, handedness, height, time of last meal or snack, socio-occupational category), smoking habits, perfume and cosmetics use, native language, pregnancy and menstruation (for women), general sensitivity, and medication. Note that experimental rooms differed across countries but both olfactory testing and food questionnaires were all the same and were all administered in the same way.
Data Analysis
Distribution normality was first checked in all datasets of both experiments; all Shapiro-Wilk tests showed that the hypothesis of normality was not confirmed (p < 0.0001 in all cases). Thus, non-parametric tests were used (Friedman test for within-subject comparison of multiple conditions; Wilcoxon signed rank test for paired comparisons; Mann-Whitney test for between-subject comparisons). In experiment 2, discrimination between normosmic and dysosmic subjects was further examined on linear discrimination analysis (LDA), attempting to predict a categorically dependent variable (olfactory deficit level: normosmia/dysosmia) as a linear combination of different independent variables (odor identification and intensity, familiarity, pleasantness, edibility, and/or irritation ratings). All statistical tests were performed using R software (http://www.r-project.org/).
Results
Experiment 1
To examine whether the eight odors were correctly identified by the participants, a binomial test was used to check whether odor identification was better than chance for each olfactory stimulus (n = 111, p = 0.25, confidence level = 0.95). Results, depicted in Fig. 1a, showed that all odors were identified better than chance and were indeed much better except for grass.
Characterization of odors in experiment 1. a Odors were identified more often than chance (chance level in dashed line, average identification score in black). b–f Intensity, familiarity, pleasantness, irritation, and edibility ratings of all eight odors (means and confidence intervals). g Hierarchical clustering performed on the factor map of the eight odors (Color figure online)
To further ensure that the eight odors were perceptually different, they were compared along each of the five perceptual dimensions: intensity, pleasantness, familiarity, edibility, and irritation. A Friedmann test was performed for each rating, with odor as within-subject factor. Results revealed that odors significantly differed in terms of intensity (χ 2 = 264.66, p < 0.0001), pleasantness (χ 2 = 344.54, p < 0.0001), familiarity (χ 2 = 346.47, p < 0.0001), edibility (χ 2 = 492.16, p < 0.0001), and irritation (χ 2 = 264.26, p < 0.0001) (Fig. 1b–f).
Note also that Hartigans’ dip test for unimodality/multimodality revealed that whatever the smell (mint, grass, anise, sweat, pine, flower, banana, gas) and the rating (intensity, pleasantness, familiarity, edibility, irritation), the distribution was never unimodal (D value from 0.0811 to 0.1937, p < 0.0001). Only the edibility rating distribution for the smell of gas was unimodal (D = 0.0180, p = 0.9960). Supplementary Fig. 1 depicts as an example of the distribution for intensity ratings for the smell of grass and edibility ratings for the smell of gas.
To describe and illustrate these perceptual distances between odors, hierarchical clustering and principal component analysis were used, considering all ratings (intensity, pleasantness, familiarity, edibility, irritation). Figure 1g shows clear groups of odors, with edible odors (mint, banana, anise) on the right side of the perceptual space, unpleasant odors (gas, sweat) on the left, and the other non-edible odors (grass, flower, pine) in the center.
The main aim of this pilot study was to characterize a set of odors with representative categories to be used in the main study. Our data suggest that the eight odors were correctly identified (although less well for grass that the other seven) and were perceptually different. Importantly, we also showed that the eight odors spanned the olfactory space well, with representative categories (food, non-food, unpleasant), allowing us to examine—in Experiment 2—the question of how quantitative smell impairments affect different levels of odor processing using a representative set of odors.
Experiment 2
Effects of Olfactory Status on Olfactory Perception
We first examined whether patients and controls differed in overall olfactory perception, using the Mann-Whitney test for between-subject comparisons. Comparison between groups revealed that dysosmics showed poorer identification ability (U = 168.5, p < 0.0001, Fig. 2a). Interestingly, a complementary analysis revealed no difference as a function of group and/or country in terms of identification for any of the eight odors (max χ 2 = 0.79172, max p = 0.3736). Differences between groups were also observed for other perceptual dimensions: dysosmics rated odors lower in terms of intensity (U = 152.5, p < 0.0001, Fig. 2b), familiarity (U = 405.5, p = 0.0002, Fig. 2c), and irritation (U = 552.5, p = 0.0248, Fig. 2f). No difference between groups was observed for pleasantness (U = 748.5, p = 0.7556, Fig. 2d) or edibility (U = 764.0, p = 0.8748, Fig. 2e). Linear discriminant analysis of the perceptual data revealed that the two groups could be discriminated, with correct differential percentage classification according to the variables entered in the model: 82.27% when all variables were considered (identification, intensity, familiarity, pleasantness, irritation, edibility), 82.27% when the three most significant variables were considered (identification, intensity, and familiarity), and 86.07% when only two variables were considered (identification and intensity).
Results for individual odorants, comparing patients vs. controls, showed the following: (i) poorer odor identification for mint (U = 419.5, p = 0.0004), sweat (U = 571.0, p = 0.0404), pine (U = 496.0, p = 0.0054), banana (U = 475.0, p = 0.0028), and gas (U = 298.5, p < 0.0001), but not for grass (U = 746.5, p = 0.7425), anise (U = 613.0, p = 0.1015), or flower (U = 692, p = 3882); (ii) lower odor intensity rating for all eight odorants (U values from 83 to 472, p values from 0.0025 to < 0.0001); (iii) lower familiarity rating for mint (U = 397.5, p = 0.0002), anise (U = 496.0, p = 0.0054), sweat (U = 526.5, p = 0.0129), banana (U = 534.5, p = 0.0161), and gas (U = 272.5, p < 0.0001), but not for grass (U = 658.0, p = 0.2316), pine (U = 633.0, p = 0.1495), or flower (U = 675.5, p = 0.3055); (iv) less marked rating of unpleasantness for sweat (U = 473, p = 0.0026) and gas (U = 259, p < 0.0001) and lower pleasantness rating for mint (U = 489.0, p = 0.0043) and anise (U = 562.0, p = 0.0325); (v) no difference in edibility rating (p > 0.05 in all 8 cases); and (vi) lower irritation rating for sweat (U = 419, p = 0.0004) and gas (U = 464, p = 0.0019) (Fig. 3a–f).
As in experiment 1, hierarchical cluster and principal component analysis (based on intensity, pleasantness, familiarity, edibility, and irritation ratings) were used to describe and illustrate perceptual distances between odors. Figure 4a, b shows that as in experiment 1 (see Fig. 1g), odors were clustered as follows: Edible odors formed a group on the right side of the space whereas the remaining odors formed three independent clusters on the left. Clusters were nearly the same in both groups, except that sweat was in the same cluster as pine in controls whereas in patients, it was in the same cluster as flower and grass. Thus, it seems that compared to the controls, patients were able to categorize smells in a similar manner despite their lower olfactory ability. However, distances between odorants seemed to be shorter in patients than in controls (Fig. 4a, b), which may reflect poorer discrimination ability. To check this, we measured the Euclidian distances in a perceptual space comprising intensity, pleasantness, familiarity, edibility, and irritation for all eight odorants in controls and patients separately. Results confirmed that the patients showed significantly shorter perceptual distances between odorants than the controls (z = − 4.6, p < 0.0001, Wilcoxon signed rank test, Fig. 4c).
Multidimensional representation of odors in a controls and b patients using hierarchical clustering performed on the factor map of the eight odors. c Euclidian distances between odors in the perceptual space (intensity, familiarity, pleasantness, irritation, and edibility) in controls (black bars) and patients (white bars) (means and confidence intervals). *p < 0.05
Effects of Olfactory Status on Food Behavior
Firstly, results revealed a significant overall effect (U = 529.0, p = 0.0138, Fig. 5a) whereby patients used more condiments and additional foods than controls. Taking each condiment/additional food individually, results showed significant effect in three cases: patients used more sugar (U = 555.0, p = 0.0274), mayonnaise (U = 540.0, p = 0.0186), and sour cream (U = 536, p = 0.0167); there was also a trend toward significantly greater use of ketchup by patients (U = 596.0, p = 0.0712). No significant differences were observed for the remaining items (butter, olive oil, spices, pepper, herbs, soya sauce, salt, lemon, vinegar, mustard, or syrup) (all p values > 0.1036; Fig. 5b).
Secondly, statistical analyses regarding neophilia and the pleasure of eating showed that patients were less neophilic (U = 423.5, p = 0.0012; Fig. 5c) and tended to experience less pleasure in eating (U = 568.5, p = 0.0788; Fig. 5d, Table 1) (see Supplementary Fig. 2 for an illustration of the distributions of the variables “food neophilia,” “eating pleasure,” and “added condiments” as a function of groups). However, there were no significant differences in preference for vegetables, fruits, meat, fish, starchy foods, or dairy products (all p values > 0.5718) (Table 1). Finally, there were also no differences in culinary habits: cooking for oneself, eating prepared meals, or eating out in a restaurant (all p values > 0.1193) (Table 1).
Thirdly, to further examine whether among patients, anosmics differed from hyposmics in terms of food behavior, patients were split into a group of 23 anosmics and a group of 15 hyposmics (categorization of one patient was uncertain since the ENT examination revealed the presence of an olfactory disorder, but the Sniffin’ Sticks test was not completed). Statistical analyses comparing anosmics and hyposmics did not reveal any difference for any items: food neophilia (U = 188, p = 0.3751), pleasure to eat (U = 181, p = 0.5137), and added condiments (U = 180, p = 0.8337). Moreover, there were no significant differences in preference for vegetables, fruits, meat, fish, starchy foods, or dairy products (all p values > 0.1314) and in culinary habits (all p values > 0.2748).
Finally, a complementary analysis further asked whether weight (W) or body mass index (BMI) can explain individual differences in terms of food behavior within each group. For patients, correlational analyses between food behavior parameters on the one hand and BMI and W on the other hand did not show any significant relationships: food neophilia (BMI: r = − 0.0045; W: r = 0.1661), pleasure to eat (BMI: r = 0.0962; W: r = − 0.0743), added condiments (BMI: r = 0.0232; W: r = − 0.0508), cooking at home (BMI: r = 0.1512; W: r = − 0.0974), eating food ready to eat (BMI: r = − 0.0717; W: r = − 0.0838), and eating at the restaurant (BMI: r = − 0.2613; W: r = − 0.0693). Results for controls did not show any significant correlation either: food neophilia (BMI: r = 0.0141; W: r = 0.1729), pleasure to eat (BMI: r = 0.0063; W: r = 0.0684), added condiments (BMI: r = 0.2303; W: r = 0.2700), cooking at home (BMI: r = − 0.2512; W: r = − 0.2856), eating food ready to eat (BMI: r = − 0.0652; W: r = 0.0199), and eating at the restaurant (BMI: r = 0.0141; W: r = 0.0946).
Conclusions
The main result of the present study was that olfactory impairment impacts feeding. We showed that patients with smell impairments were less neophilic than controls, tended to experience less pleasure when eating, and also used significantly more condiments/additional foods such as sugar, mayonnaise, and sour cream to make their dishes tastier.
Ratings of intensity for most odors were significantly lower in patients, as were identification scores (30% correct for dysosmics versus 70% for controls). Both results confirm our careful patient selection in terms of partial impairment of olfactory sensitivity. Another prominent aspect of our findings is that we did not see any significant difference between patients and controls in terms of odor identification abilities for some odors, including beta-ionone (flower), trans-anethole (anise), and cis-3-hexenol (grass). One assumption that may be raised here is that our normosmic sample contains some individuals with specific anosmia to these molecules. Interestingly, previous studies in the field have shown the existence of specific anosmia (explained by genetic polymorphism) to the odorant molecules of beta-ionone and cis-3-hexenol (McRae et al. 2012; Jaeger et al. 2013; see also Razafindrazaka et al. 2015). Finally, in line with previous investigations (Gudziol et al. 2001), we also showed that the sensation of irritation, which is mediated by the trigeminal system, was significantly reduced in dysosmia.
Interestingly, the study also explored other perceptual dimensions that are not frequently documented: familiarity, pleasantness, and edibility. Results showed that while perception of familiarity was reduced in dysosmia, edibility was not. One explanation for this may be that despite certain obvious impairments, patients with smell impairment are still able to categorize odors correctly: they may not be able to identify mint odor, but they were still able to categorize it as edible. However, this interpretation runs up against a limitation in the study protocol: participants performed the edibility judgment after the identification task. They received no feedback regarding the correctness of their identification response, but they had been asked to choose between four food-related descriptors (e.g., for the smell of mint, the alternatives were mint, nut, olive, and onion). This was not the case for non-food odors. In other words, patients could be sure from the proposed descriptors that the odor was from an edible source, biasing the above results.
For control subjects, the most pleasant odor was mint and gas was the most unpleasant, and dysosmic patients showed the same pattern. However, the perceptual distance was shorter in patients, who rated mint as less pleasant than controls and rated the two most unpleasant odors (sweat and gas) as less unpleasant. Looking further at the organization of the overall olfactory space, patients were found to categorize odors nearly like controls: their impairment was reflected in shorter distances between odorant representations. It all looks as if odors were less salient (because weaker), more difficult to differentiate semantically, and easier to confuse in some but not all aspects for dysosmic subjects: as if their olfactory world was reduced, but still there.
The second issue that we wanted to explore was the extent to which olfactory impairment impacted eating behavior. Here, some competences remained despite dysosmia: impairment showed no impact on culinary habits or food preferences per se, which remains present in memory. On the other hand, patients tended to experience less pleasure in eating; this phenomenon was described by others (see (Croy et al. 2014)) and appears in patient interviews as a major complaint: food seems tasteless.
A previous investigation of eating pleasure (Arganini and Sinesio 2015) tested smell abilities in 239 65-year-old subjects with good cognitive capacity. Participants were also asked to fill out a questionnaire on their self-assessed smell and taste abilities, appetite, and pleasure in eating. Results showed that participants overestimated their olfactory ability: subjective ratings were higher than psychophysical performance measurements. No correlation was observed between olfactory performance, appetite, and pleasure in eating, whereas other factors (social isolation, perceived health, age, gender, and particular diets) did correlate with olfaction. Several lines of evidence suggest decreased pleasure in eating in patients with olfactory disorders, as in the present study. For example, Blomqvist et al. (Blomqvist et al. 2004) measured dysosmia level and quality of life parameters in 72 patients. Results showed that patients reported more difficulty in detecting dangerous odors, difficulty in cooking, and reduced appetite and food appreciation. Mattes et al. (Mattes et al. 1990) showed that patients with olfactory loss experienced loss of appetite, decreased pleasure in eating, and disturbed diet; interestingly, 42% of the patients showed increased use of spices.
Likewise, the review by Croy and colleagues (Croy et al. 2014) compiled evidence for the hypothesis that pleasure in eating is impaired by dysosmia; patients tended to compensate for their olfactory sensory (and hedonic) loss by seeking trigeminal and textural sensations in eating. Merkonidis et al. (Merkonidis et al. 2015) tested a group of 269 patients with olfactory problems, who filled out a questionnaire on the impact of smell impairment on everyday life. Patients who had lost smell suddenly bore their disability less easily than those with impairment progressing gradually over a long period (minimum 2 years). Compensation mechanisms differed between young patients, who resorted more to texture, and older ones, who resorted more to visual cues in food. Aschenbrenner et al. (Aschenbrenner et al. 2008), using the Sniffin’ Sticks test, measured dysosmia in 176 patients, who were also asked to answer a nutrition questionnaire. Nutrition was more strongly impaired in patients with gradually progressing smell loss and in patients who were either over- or under-weight. Ferris and Duffy (Ferris and Duffy 1988) tested patients who all filled out a nutrition questionnaire. Results showed that most of the undernourished patients were anosmic. Changes in food habits and reduced pleasure in eating were more marked when smell loss was recent (less than 3 years); no change was observed in appetite, but these patients reported using at least one compensation strategy by enhancing food quality with spices. Thus, it would be relevant for future studies to consider some additional factors relating to age, temporal disease course, and nutritional status.
In conclusion and in accordance with the above, the present study showed clear effects in terms of adding condiments/additional foods: patients used or tended to use more sugar, ketchup, mayonnaise, and sour cream. This may result from compensation mechanisms: adding sugar, ketchup, or mayonnaise may be an attempt to (i) restore some lost flavor and (ii) increase palatability. Note that these compensatory mechanisms were also associated to reduced neophilia in patients, which could mean that they were oriented toward the smell that foods used to have before the onset of their impairment rather than toward novel foods; their confidence in novelty is impaired, which fits well with the concept of insecurity induced by olfactory loss (Croy et al. 2014). Finally, the case of sugar was particularly interesting since it involved compensatory mechanisms using a single sensory modality, namely, gustation. We therefore asked in an exploratory analysis whether people who are used to adding sugar in their food (to make them taste) perceived smell differently than those who do not add sugar (this was done separately in controls and patients). In controls, results revealed that individuals who added sugar perceived the smell of beta-ionone as less intense (p = 0.047) and were also less able to identify it (p = 0.003). When considering the remaining odorants, only two results emerged: controls who added sugar perceived the smell of isoamyl acetate as less intense (p = 0.018) and perceived the smell of gas as less irritant (p = 0.008). In patients, only one significant difference was observed: patients who added sugar perceived pine as more pleasant (p = 0.033). Although exploratory, these results open up interesting perspectives on the study of the influence of food behavior on olfactory perception (and vice versa).
Implications
In summary, as expected, the present study showed significant differences in terms of odor perception between dysosmic patients and controls: patients showed reduced odor identification abilities and rated odors as less intense and less emotional. The main result of the study was that such olfactory changes were accompanied by decreased pleasure in eating and by compensatory mechanisms to increase palatability by increasing pleasantness in other modalities (taste, texture). In the future, deciphering in detail the mechanisms by which patients compensate for their olfactory loss can facilitate strategies to help frail people, such as the elderly. When they lose the sense of smell, they are liable to feel disoriented when eating. The aim would be to set up compensation strategies by improving the visual appearance of the dish, playing on texture or enhancing the taste and trigeminal components of the food.
References
Arganini C, Sinesio F (2015) Chemosensory impairment does not diminish eating pleasure and appetite in independently living older adults. Maturitas 82:241–244
Aschenbrenner K, Hummel C, Teszmer K et al (2008) The influence of olfactory loss on dietary behaviors. Laryngoscope 118:135–144. https://doi.org/10.1097/MLG.0b013e318155a4b9
Blomqvist EH, Bramerson A, Stjarne P, Nordin S (2004) Consequences of olfactory loss and adopted coping strategies. Rhinology 42:189–194
Bramerson A, Johansson L, Ek L et al (2004) Prevalence of olfactory dysfunction: the Skövde population-based study. Laryngoscope 114:733–737
Croy I, Hummel T (2017) Olfaction as a marker for depression. J Neurol 264:631–638. https://doi.org/10.1007/s00415-016-8227-8
Croy I, Bojanowski V, Hummel T (2013) Men without a sense of smell exhibit a strongly reduced number of sexual relationships, women exhibit reduced partnership security—a reanalysis of previously published data. Biol Psychol 92:292–294. https://doi.org/10.1016/j.biopsycho.2012.11.008
Croy I, Nordin S, Hummel T (2014) Olfactory disorders and quality of life—an updated review. Chem Senses 39:185–194. https://doi.org/10.1093/chemse/bjt072
Ferris AM, Duffy VB (1988) Effect of olfactory deficits on nutritional status does age predict persons at risk? Ann N Y Acad Sci 561:113–123
Gudziol H, Schubert M, Hummel T (2001) Decreased trigeminal sensitivity in anosmia. ORL 63:72–75
Henkin RI (2014) Effects of smell loss (hyposmia) on salt usage. Nutrition 30:690–695
Hummel T, Kobal G, Gudziol H, Mackay-Sim A (2007) Normative data for the “Sniffin’ Sticks” including tests of odor identification, odor discrimination, and olfactory thresholds: an upgrade based on a group of more than 3,000 subjects. Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol - Head Neck Surg 264:237–243. https://doi.org/10.1007/s00405-006-0173-0
Hummel T, Whitcroft KL, Andrews P et al (2017) Position paper on olfactory dysfunction. Rhinology. https://doi.org/10.4193/Rhin16.248
Jaeger SR, McRae JF, Bava CM et al (2013) A Mendelian trait for olfactory sensitivity affects odor experience and food selection. Curr Biol 23:1601–1605
Joussain P, Bessy M, Faure F et al (2016) Application of the European Test of Olfactory Capabilities in patients with olfactory impairment. Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol - Head Neck Surg 273:381–390. https://doi.org/10.1007/s00405-015-3536-6
Keller A, Malaspina D (2013) Hidden consequences of olfactory dysfunction: a patient report series. BMC Ear Nose Throat Disord 13:8. https://doi.org/10.1186/1472-6815-13-8
Landis BN, Konnerth CG, Hummel T (2004) A study on the frequency of olfactory dysfunction. Laryngoscope 114:1764–1769
Landis BN, Scheibe M, Weber C et al (2010) Chemosensory interaction: acquired olfactory impairment is associated with decreased taste function. J Neurol 257:1303–1308
Mattes RD, Cowart B, Schiavo MA, Lowry LD (1990) Dietary evaluation of patients with smell and/or taste disorders. Am J Clin Nutr 51:233–240
McRae JF, Mainland JD, Jaeger SR et al (2012) Genetic variation in the odorant receptor OR2J3 is associated with the ability to detect the “grassy” smelling odor, cis-3-hexen-1-ol. Chem Senses 37:585–593
Merkonidis C, Grosse F, Ninh T et al (2015) Characteristics of chemosensory disorders—results from a survey. Eur Arch Otorhinolaryngol 272:1403–1416. https://doi.org/10.1007/s00405-014-3210-4
Murphy C (2002) Prevalence of olfactory impairment in older adults. JAMA 288:2307. https://doi.org/10.1001/jama.288.18.2307
Razafindrazaka H, Monnereau A, Razafindrazaka D et al (2015) Genetic admixture and flavor preferences: androstenone sensitivity in Malagasy populations. Hum Biol 87:59–70
Santos DV, Reiter ER, DiNardo LJ, Costanzo RM (2004) Hazardous events associated with impaired olfactory function. Arch Otolaryngol Neck Surg 130:317–319
Smeets MAM, Veldhuizen MG (2009) Sense of smell disorder and health-related quality of life. Rehabil Psychol 54:404–412
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by a grant from the Interdisciplinary Mission of the CNRS (DEFISENS call, PREVALOF and O2C2 projects; DEGIGENRE call, Sensotogenre project) to MB and a grant from Region Rhone-Alpes ARC2 Qualité de vie et Vieillissement ADR to CM. The study was also supported by a grant from the Deutsche Forschungsgemeinschaft to TH (DFG HU411/18-1).
Conflict of Interest
The authors have declared no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Electronic Supplementary Material
ESM 1
(DOCX 196 kb)
Rights and permissions
About this article
Cite this article
Manesse, C., Ferdenzi, C., Sabri, M. et al. Dysosmia-Associated Changes in Eating Behavior. Chem. Percept. 10, 104–113 (2017). https://doi.org/10.1007/s12078-017-9237-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12078-017-9237-3