Abstract
Background
Significant improvement of objective response rate and overall survival period has been achieved in several types of solid tumors by treatment with PD-1/PD-L1 inhibitors, which shed some light on hepatocellular carcinoma (HCC). Currently, a number of clinical trials concerning the application of checkpoint inhibitors in HCC are ongoing, some of which have shown favorable expectations. Hereby, we conducted a meta-analysis of existing studies to reveal the efficacy and safety of checkpoint inhibitors in advanced HCC.
Methods
Medline, Embase, Cochrane Library, and Web of Science were searched from inception to January 31, 2020. The clinical trials reporting the efficacy of PD-1/PD-L1 inhibitors in advanced HCC patients were eligible. Overall results of complete response (CR), partial response (PR), stable disease (SD), progression of disease (PD), objective response rate (ORR), disease control rate (DCR), overall survival (OS), progression-free survival (PFS) and rate of adverse events (AE) with their 95% confidence intervals (95%CI) were calculated as the primary focus of the meta-analysis. Subgroup analyses were conducted primarily according to the categories of PD-1 inhibitor or PD-L1 inhibitor and combination therapy or monotherapy. In addition, pooled results of PD-1/PD-L1 monoclonal antibodies (mAb) combining with anti-VEGF agents were calculated separately.
Results
A total of 20 studies with 1232 patients were included. The overall CR, PR and SD rate were 0.01 (95% CI 0.01–0.03), 0.17 (95% CI 0.14–0.22) and 0.39 (95% CI 0.34–0.43), respectively. The overall ORR and DCR were 0.20 (95% CI 0.16–0.24) and 0.60 (95% CI 0.54–0.67), respectively. The overall PFS and OS were 3.58 months (95% CI 2.65–4.50) and 12.24 months (95% CI 10.48–14.00), respectively. For patients treated with PD-1/PD-L1 mAb combing with anti-VEGF agent, ORR was 29% (95% CI 0.15–0.43) and DCR was 77% (95% CI 0.70–0.84). For all included studies, the overall rate of AE was 0.63 (95% CI 0.45–0.78) and serious adverse events (SAE) was 0.11 (95% CI 0.06–0.22).
Conclusions
PD-1/PD-L1 inhibitors showed favorable outcomes concerning response rates and survival periods in advanced HCC. Updated results from high-quality clinical trials are expected to validate these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is currently the third leading cause of cancer-related death worldwide and its incidence has been increasing rapidly in recent years [1]. Surgical resection remains the major treatment option for early-stage HCC, meanwhile a lot of therapeutic strategies like trans-arterial chemoembolization (TACE), radiofrequency ablation (RFE), and stereotactic body radiation therapy (SBRT) which constituted system therapy were mature and extensively used in clinics [2]. However, the clinical benefit for patients with advanced HCC is still far from satisfactory [3]. Sorafenib is the currently best performing first-line molecular targeted drug for HCC, yet its efficacy is still not satisfactory [4, 5]. Thus, improving the outcome of therapies for HCC is still a major healthcare challenge for the world.
Since 2010, when Hodi et.al [6] first reported the application of CTLA4 monoclonal antibody (mAb) in patients with metastatic melanoma, the immune checkpoint inhibitors have shown significant improvement regarding objective response and overall survival in a variety of advanced solid malignant tumors (e.g., lung cancer, melanoma, urothelial and renal carcinomas, ovarian cancer, bladder cancer, Hodgkin’s lymphoma and tumors originated from digestive system) [7, 8]. PD-L1, also called B7-H1 or CD274, is a molecule expressed on the surface of several types of cells (including cancer cell) and can lead to the exhaustion of T cells [9]. In addition, overexpression of PD-L1 on cancer cells was related to poor prognosis [10]. A proposed mechanism for this phenomenon was that immune activation to cancer cells was impaired and immune tolerance was induced by interaction between PD-1 and PD-L1 receptor, which induced cancer cells to evade the immune surveillance [11]. PD-1/PD-L1 monoclonal antibodies can specifically block the PD-1/PD-L1 signaling pathway, restore the sensitivity of immune response and lead to an increase in anticancer activity. The success of PD-1/PD-L1 inhibitors in solid tumors has shed some light on the treatment of advanced HCC [12].
Until now, final or interim results of studies focusing on the efficacy of PD-1/PD-L1 mAbs in advanced HCC patients were reported in about 20 clinical trials or case series studies, and several randomized control trials (RCTs) are ongoing [13]. The efficacy of nivolumab, the first-reported PD-1/PD-L1 mAbs for the treatment of HCC, was evaluated in CA209-040 trials in 2015. In this Phase I/II study, nine of 39 advanced HCC patients achieved objective response (CR + PR) [14]. Nivolumab was also assessed in CheckMate-040 trial [15] as well as other clinical trials with larger sample size.
These clinical trials were different on clinical phases, sample size and response evaluation criteria. To estimate the overall benefit and overcome the limitations of individual studies, we conducted this systematic review and meta-analysis to assess the efficacy of PD-1 and PD-L1 inhibitors in advanced HCC patients.
Methods
Data source and literature search strategy
Online databases including Medline, Embase, Cochrane Library, and Web of Science were searched from inception to January 31, 2020, for eligible studies. The search terms used to define the therapy included “programmed death-ligand 1”, PD-L1, “programmed death receptor-1”, PD-1, nivolumab, opdivo, pembrolizumab, keytruda, atezolizumab, tecentriq, sintilimab, IBI-308, imfinzi, durvalumab, SHR-1210, camrelizumab, bavencio, avelumab, toripalimab, tislelizumab, and cemiplimab. The terms used to define the disease included "hepatocellular carcinoma", “HCC”, "liver cancer", “liver cell carcinoma”, “hepatic cellular cancer”, hepatoma, “hepatic malignancy”, and “hepatic malignant tumors”. In addition, we also checked the reference lists of all relevant articles to identify additional studies.
Study selection
Studies were included if they met the following criteria: (1) published in English; (2) study type being clinical trials, retrospective studies, and case series; (3) study including patients with advanced HCC, which can be described as “unresectable”, “metastasis”, “first-line treatment failure”, etc.; (4) study focusing on the efficacy of checkpoint inhibitors of PD-L1 or PD-1 (but not CTLA4) such as nivolumab, pembrolizumab, atezolizumab, sintilimab, durvalumab, camrelizumab, avelumab, toripalimab, tislelizumab, or cemiplimab. PD-1/PD-L1 used in monotherapy or combination therapy was all included. Combination therapy refers to PD-1 or PD-L1 inhibitor combined with non-checkpoint-inhibitor agents, while monotherapy refers to only receive PD-1 or PD-L1 inhibitor therapy; (5) data for complete response (CR), partial response (PR), stable disease (SD), progression of disease (PD), objective response rate (ORR), disease control rate (DCR), overall survival (OS), progression-free survival (PFS), or median time to progression (TTP) were reported or calculable. Studies with sample size less than 10 patients were excluded. For the repetitive studies based on the same study patients, the latest or most comprehensive data were included.
Data extraction
Study selection and data extraction were performed by two investigators (Q. R. and M. L.) independently according to Quality of Reporting of Meta-Analyses (QUORUM) guidelines. Any disagreement on study inclusion or interpretation of data was resolved by consulting a senior investigator (Z. Z.). The following information was extracted for each study: data source, title of article, first author, year of publication, National Clinical Trials (NCT) registry number, country, applied agents (anti-PD-1/PD-L1 mAb), combination therapy, phase of the trial, evaluation criterion, sample size, primary disease of HCC, adverse events, rate of CR, PR, SD, PD, ORR, DCR, OS, PFS and median time to progression.
Quality assessment
Quality of the included studies was assessed as reported in the literature, which consists of 20 items [16]. The checklist examines the main domains including study design, population, intervention, outcome measures, statistical analysis, results/conclusions, competing interest, and sources of financial support.
Statistical analysis
Characteristics of included studies were described. Random-effect models were adopted for all meta-analyses because of the clinical heterogeneity inherent to the data. Heterogeneity among studies was quantified by I2 test, and I2 > 50% was considered substantial heterogeneity. To reveal the high heterogeneity, subgroup analyses were performed on the basis of clinical consideration. Stratification factors included type of therapy (monotherapy vs. combination therapy), target of drug (PD-1 vs. PD-L1), evaluation criteria (RECIST vs. mRECIST), region of study (Global vs. Local), primary disease of HCC (HBV/HCV etiology ≤ 50% vs. > 50%), and CTP class (Mixture of CTP A/B/C vs. CTP A only). In addition, pooled results of studies focusing on two most tested drugs (nivolumab and pembrolizumab), and studies of PD-1/PD-L1 combining with anti-VEGF agent were pooled separately and respectively.
Egger’s test was performed to evaluate publication bias [17]. Stata Software, version 15.0 (StataCorp, College Station, TX) was used for meta-analysis. p value < 0.05 was considered statistically significant.
Results
Study selection and characteristics of eligible studies
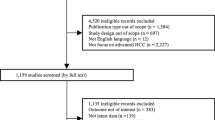
The initial search identified 420 articles in Medline, 63 articles in Embase, 126 articles in Cochrane Library and 708 articles in Web of Science. After title and abstract review, 157 studies were selected for full-text review. Then 135 articles were further excluded for inconsistency with eligibility criteria. Additionally, one article was identified during reference review of included studies. Finally, a total of 23 studies were included in this meta-analysis. The selection process is shown in Fig. 1.
Among the 23 included studies, 3 were phase III RCTs and 20 were single-arm trials (Tables S1, S2). The 20 single-arm studies were all published in the last 5 years: 8 were published in 2019, 7 in 2018, 4 in 2017, and 1 in 2015, indicating rapid development of immune checkpoint inhibitor in HCC treatment. There were 15 and 5 studies focusing on PD-1 mAb and PD-L1 mAb, respectively. Thirteen studies adopted monotherapy with PD-1/PD-L1 inhibitor and 7 adopted combination therapy. A total of 8 different PD-1/PD-L1 inhibitors were involved, with 5 PD-1 mAbs (camrelizumab, nivolumab, pembrolizumab, tislelizumab, cemiplimab) and 3 PD-L1 mAbs (durvalumab, atezolizumab, avelumab).
A total of 1232 patients were included in the meta-analysis, in which 502 patients received nivolumab. Majority of included patients were male (81%). Mean age was approximately 64 years, with a range from 49 to 68 years.
Response rate of CR, PR, SD, and PD
All the 20 single-arm studies reported response rate (CR, PR, SD, and PD). For patients who received anti-PD-1/PD-L1 mAb therapy, CR was achieved in 28/1232 patients (0.01, 95% CI 0.01–0.03), PR was achieved in 219/1232 patients (0.17, 95% CI 0.14–0.22), SD was obtained in 478/1232 patients (0.39, 95% CI 0.34–0.43), and PD was observed in 445/1232 patients (0.33, 95% CI 0.26–0.40). For patients who received monotherapy and combination therapy, CR was achieved in 23/975 patients (0.02, 95% CI 0.01–0.04) vs 5/257 patients (0.01, 95% CI 0.00–0.08), PR was achieved in 147 /975 patients (0.15, 95% CI 0.13–0.18) vs 72/257 patients (0.24, 95% CI 0.15–0.36), SD was obtained in 362/975 patients (0.35, 95% CI 0.30–0.41) vs 116/257 patients (0.45, 95% CI 0.39–0.51), and PD was observed in 395/975 patients (0.39, 95% CI 0.33–0.46) vs 50/257 patients (0.20, 95% CI 0.13–0.30), respectively. In patients receiving PD-1 inhibitor and PD-L1 inhibitor therapy, CR was achieved in 27/1054 patients (0.02, 95% CI 0.01–0.04) vs 1/178 patients (0.01, 95% CI 0.00–0.04), PR was achieved in 186/1054 patients (0.18, 95% CI 0.14–0.23) vs 33/178 patients (0.14, 95% CI 0.07–0.26), SD was obtained in 403/1054 patients (0.38, 95% CI 0.33–0.42) vs 75/178 patients (0.43, 95% CI 0.33–0.54), and PD was observed in 382/1054 patients (0.32, 95% CI 0.25–0.40) vs 63/178 patients (0.36, 95% CI 0.22–0.54), respectively. However, substantial heterogeneity was observed (Table 1).
Rate of ORR and DCR
20 studies reported ORR and DCR. As shown in Table 1, the overall ORR was 0.20 (95% CI 0.16–0.24) and DCR was 0.60 (95% CI 0.54–0.67). Between monotherapy and combination therapy, ORR were 0.17 (95% CI 0.14–0.20) and 0.25 (95% CI 0.13–0.37), and DCR were 0.54 (95% CI 0.47–0.61) and 0.75 (95% CI 0.68–0.82), respectively. For PD-1 and PD-L1 inhibitors, ORR were 0.21 (95% CI 0.16–0.26) and 0.15 (95% CI 0.04–0.25), and DCR were 0.61 (95% CI 0.53–0.68) and 0.59 (95% CI 0.41–0.77) in both groups. There was significant heterogeneity in ORR (I2 = 67.0%, p < 0.01) and DCR (I2 = 81.0%, p < 0.01) (Fig. 2).
PFS and OS
Ten studies reported the duration of PFS and 5 studies reported duration of OS. The overall PFS was 3.58 months (95% CI 2.65–4.50), and the overall OS was 12.24 months (95% CI 10.48–14.00). For patients receiving anti-PD-1/PD-L1 mAb monotherapy, the PFS and OS were 3.32 months (95% CI 2.34–4.29) and 12.36 months (95% CI 10.54–14.18), respectively (Table 2). Subgroup of combination therapy was not analyzed due to limited number of studies. For patients receiving PD-1 and PD-L1 mAb, PFS was 3.42 vs 3.58 months, and OS was 12.31 vs 11.82 months (Table 2). Significant heterogeneity was observed in overall result of PFS (I2 = 71.5%, p < 0.01). However, there was no evidence of heterogeneity between studies for OS (I2 = 0.0%, p = 0.69) (Fig. 3).
The pooled PFS rates at 6 months, 9 months and 12 months were 0.44 (95% CI 0.28–0.60), 0.29 (95% CI 0.23–0.34) and 0.21 (95% CI 0.08–0.34), respectively. And the pooled OS rates at 6 months, 9 months, and 12 months were 0.76 (95% CI 0.70–0.82), 0.70 (95% CI 0.63–0.77), and 0.51 (95% CI 0.42–0.59), respectively (Figs. S1, S2).
Subgroup analysis
In studies regarding PD-1/PD-Ll inhibitor combination therapy, seven different combination drugs were reported: apatinib, bevacizumab, ramucirumab, axitinib, lenvatinib, codrituzumab, and FOLFOX/GEMOX, of which five were anti-VEGF agents, thus constituting PD-1/PD-L1 inhibitors plus anti-VEGF agent subgroup. In this subgroup, CR was achieved in 5/203 patients (0.02, 95% CI 0.00–0.09), PR was achieved in 62/203 patients (0.27, 95% CI 0.17–0.41), SD was obtained in 88/203 patients (0.43, 95% CI 0.37–0.50), PD was observed in 36/203 patients (0.18, 95% CI 0.10–0.31), ORR was 0.29 (95% CI: 0.15–0.43), and DCR was 0.77 (95% CI 0.70–0.84). PD-1 and PD-L1 inhibitors were also analyzed separately (Table 3). Pooled analysis of OS and PFS was not conducted in this subgroup due to insufficiency of studies reporting the two indicators.
In studies reporting PD-1 inhibitors, 7 studies including 8 datasets were about nivolumab, and 3 studies were about pembrolizumab. For nivolumab, CR was achieved in 21/502 patients (0.03, 95% CI 0.01–0.06), PR was achieved in 77/502 patients (0.15, 95% CI 0.11–0.21), SD was obtained in 199/502 patients (0.39, 95% CI 0.32–0.47), PD was observed in 172/502 patients (0.33, 95% CI 0.29–0.37), ORR was 0.17 (95% CI 0.10–0.24) and DCR was 0.56 (95% CI 0.47–0.66) (Table S3). The heterogeneity between studies was decreased as reflected by I2 value. The pooled PFS and OS were 3.34 months (95% CI 1.44–5.24) and 12.34 months (95% CI 8.64–16.04), respectively (Table S4). Analysis results regarding pembrolizumab are demonstrated in Tables S3 and S4.
Further, subgroup analyses stratified by primary disease of HCC, CTP class, evaluation criteria, and region of study are shown in Tables S5 and S6.
Adverse events
The overall rate of adverse events (AE) was 0.63 (95% CI: 0.45–0.78) and AE with grade ≥ 3 was 0.18 (95% CI 0.11–0.29). The rate of serious adverse events (SAE) was 0.11 (95% CI 0.06–0.22) and SAE with grade ≥ 3 was 0.05 (95% CI 0.04–0.08). The rate of any immune-related adverse events (irAE) was 0.09 (95% CI 0.03–0.22). For irAE grade ≥ 3, the rate was 0.05 (95% CI 0.02–0.09). The overall rate of fatigue, rash, pruritus, increased AST and increased ALT (common adverse event) were 0.17 (95% CI 0.10–0.27), 0.15 (95% CI 0.11–0.20), 0.14 (95% CI 0.10–0.19), 0.16 (95% CI 0.12–0.22) and 0.13 (95% CI 0.09–0.20), respectively. There was significant heterogeneity in AE (AE: I2 = 95.0%, p < 0.01; AE with grade ≥ 3: I2 = 91.0%, p < 0.01), SAE (I2 = 89.0%, p < 0.01) and irAE (I2 = 84.0%, p < 0.01), but no heterogeneity was observed in SAE with grade ≥ 3 (I2 = 0%, p = 0.63) and irAE with grade ≥ 3 (I2 = 0%, p = 0.41) (Table S7).
Assessment of study quality and publication bias
Quality assessment of 20 single-arm studies is summarized in Table S8. No evidence of publication bias was observed via Egger’s tests in the pooled analysis of ORR, DCR, PR, SD, OS, PFS, and MTP, whereas significant publication bias was observed in the meta-analysis of CR and PD (Table S9).
Discussion
For advanced HCC patients, options on effective treatment strategies were still limited. Since FDA’s (United States Food and Drug Administration) approval of sorafenib, a multi-targeted kinase inhibitor, for the systemic treatment therapy with advance HCC in 2007, the average duration of overall survival was improved by 2.3–2.8 months [2, 4]. Nowadays the options of candidate drugs have expanded to include lenvatinib, regorafenib, and so on [18, 19]. However, the expectant survival still remains no more than 1 year [20]. In recent years, immunotherapy has attracted increasing attention due to its sensitivity, specificity, and self-renewing capacity of the immune system. However, different from other organs, liver sustained an immunosuppressive milieu because of a series of regulatory mechanisms including inherent tolerogenicity, chronic HBV- or HCV-mediated immunosuppression, and HCC immune escape [21]. Therefore, conventional immunotherapy had limited effect in HCC. On the other hand, immunotherapies mediated by checkpoint inhibitors (CTLA4, PD-1, and PD-L1 mAb) have demonstrated preliminary therapeutic benefit in solid tumors. For HCC, a series of clinical trials on PD-1/PD-L1 inhibitors showed favorable results which may start a new chapter on the treatment of advanced HCC [13].
Our meta-analysis calculated the overall CR, PR, SD, PD, ORR, DCR, PFS, and OS of existing evidence, involving more than 1200 advanced HCC patients with PD-1/PD-L1 inhibitor therapy. The analysis of the 20 included studies estimated an ORR of 20% and a DCR of 60%. The overall PFS was 3.58 months and overall OS was 12.08 months. Currently, partial results of 3 phase III RCTs have been published (Table S2). Finn et al. [22] reported a consistently favorable risk-to-benefit ratio for pembrolizumab in advanced HCC. However, the OS and PFS failed to reach statistical significance. Yau T’s et al. reported that nivolumab achieved clinically meaningful improvements in OS, ORR, and CR for advanced HCC, compared to sorafenib. However, the OS also failed to reach statistical significance as compared to sorafenib [23]. In the third study, the combination therapy of atezolizumab plus bevacizumab demonstrated statistically significant and clinically meaningful improvement in both OS and PFS in the first-line treatment of unresectable HCC, as compared to sorafenib [24]. Still, more data from updated clinical trials are needed to further understand the potential benefit of checkpoint inhibitors.
Since heterogeneity between different studies is inevitable, random-effect models were adopted and subgroup analysis was performed. Compared to monotherapy, combination therapy showed an improvement in ORR (17% vs 25%) and DCR (54% vs 75%). In addition, PFS for monotherapy and combination therapy were 3.32 months (95% CI 2.34–4.29) and 4.80 months (95% CI 3.17–6.43), respectively, which showed an improvement. However, PFS was only reported in two studies for combination therapy, and more data were needed. ORR of PD-1 and PD-L1 subgroup were 21% vs 15%, respectively, whereas DCR of the two subgroups were similar. For clinical consideration, therapies with nivolumab, pembrolizumab, and PD-1/PD-L1 mAb + anti-VEGF agent were also analyzed separately as different subgroups. For combination therapy, it was shown in Shigeta et al.'s study [25] that a combination of anti-PD-1 and VEGFR-2 agents has a consistent vessel fortification effect in HCC and can overcome treatment resistance, as compared to monotherapies with either of the two agents. In addition, the combination of anti-PD-1 and VEGFR-2 agents increases overall survival in both anti-PD-1 therapy-resistant and anti-PD-1 therapy-responsive HCC models. In our study, combination therapy of PD-1/PD-L1 mAb + anti-VEGF agent also showed a favorable outcome in HCC. In addition, in the study of Lee et al., combination therapy of atezolizumab plus bevacizumab was compared with atezolizumab monotherapy, where combination therapy showed a statistically significant improvement in PFS (5.6 vs 3.4 months, HR 0.55, p < 0.05) [26]. Moreover, the IMbrave150 trial, a phase III RCT, showed significantly better OS and PFS outcomes with atezolizumab plus bevacizumab than with sorafenib in patients with unresectable HCC. This combination therapy also demonstrated statistically significant and clinically meaningful improvement in both ORR and DCR, showing promising clinical efficacy of PD-1/PD-L1 mAb + anti-VEGF therapy in the treatment of advance HCC [24]. CTLA4 was another common target of checkpoint inhibitor. Currently, several studies on the combination of multiple immune checkpoints are ongoing. The efficacy and safety of combination therapy consisting of nivolumab (anti-PD-1 mAb) plus ipilimumab (anti-CTLA4 mAb) was studied in advanced HCC [27]. In this study, 148 patients refractory to sorafenib were randomized. The minimum follow-up for OS (from last patient randomization date to data cutoff) was 24 months. Overall, ORR of the combination therapy was twice that of nivolumab monotherapy (31% and 14%, respectively). Moreover, the DCR was 49% and OS rate at 24 months was 40%, which showed an encouraging outcome. Subgroup analyses according to different RECIST criteria (RECIST vs. mRECIST) and different regions of the study (global vs. local) were also performed, which showed similar results of DCR, but some difference in ORR, PFS, and OS.
Time to progression (TTP) was an alternative endpoint when the follow-up was not long enough, so TTP is widely used for early-phase trials to evaluate the treatment efficacy [28]. In this meta-analysis, TTP in four studies with five sets of data was analyzed. The overall TTP was 3.94 months (95% CI 2.79–5.10), which was a favorable result (Fig. S3).
Regarding adverse effects, Feng et al.’s study demonstrated comparable incidence rates for treatment-related adverse events (TrAEs) between PD-1/PD-L1 mAb cohort and sorafenib cohort, and an increased incidence of ≥ grade 3 TrAEs was observed in the combination cohort [29]. In this meta-analysis, the pooled rate of fatigue, rash, pruritus, increased AST and increased ALT were 0.17 (95% CI 0.10–0.27), 0.15 (95% CI 0.11–0.20), 0.14 (95% CI 0.10–0.19), 0.16 (95% CI 0.12–0.22) and 0.13 (95% CI 0.09–0.20), respectively. Rate of immune-related adverse events (irAE) was 0.09 (95% CI 0.03–0.22), and rate of irAE grade ≥ 3 was 0.05 (95% CI 0.02–0.09).There was significant heterogeneity in AE and SAE, but no heterogeneity was observed in SAE with grade ≥ 3. Subgroup analysis was conducted according to type of therapy (monotherapy/combination) and type of agents (PD-1/PD-L1 mAb). As indicated by the results of subgroup analysis, PD-L1 mAb and combination therapy both had an increased rate of AE, compared to their respective counterparts (Table S7). However, due to the small number of studies for combination therapy and PD-L1, further study is still needed to clarify these concerns.
What were the reasons that affect the response of PD-1/PD-L1 inhibitor for HCC patients? The answer may be the key for the development of HCC immunotherapy. By subgroup analyses of primary disease of HCC and Child–Turcotte–Pugh grading (CTP) of included patients, we found that mostly patients were complicated with assorted primary diseases or conditions, e.g., HBV, HCV, NAFLD, alcohol liver disease, etc. Thus, we stratified studies by the proportion of patients with HBV/HCV infection (cut-off value 50%). Subgroup analysis indicated that studies with proportion of HBV/HCV-infected patients > 50% had a relatively higher rate of CR, PR, SD, ORR and DCR. In addition, these studies reported relatively longer OS, but shorter PFS. These findings indicated that the primary disease of HCC might influence the benefit of PD-1/PD-L1 inhibitors. However, there was no study that was specialized in the etiology of liver cancer and the treatment of inhibitors. In addition, studies only included patients with CTP A reported relatively higher rates of CR, PR, SD, ORR, and DCR, and a lower rate of PD. Similarly, pooled duration of OS and PFS of studies with CTP A patients only were slightly longer, indicating that disease severity may have an impact on the clinical effect of PD-1/PD-L1 inhibitor therapy. Less serious patients might achieve more benefit from the PD-1/PD-L1 inhibitor therapy. Nevertheless, regarding the factors that may have potential influences on the efficacy of PD-1/PD-L1 inhibitors: the complex immune microenvironment of the liver cancer, expression of PD-L1 on the surface of hepatocellular carcinoma cells, the selection of checkpoint inhibitors, the selection of combination therapy drugs (chemotherapy drugs, anti-VEGF agents or another checkpoint inhibitor), starting point of treatment, previous treatment, and management of adverse effects should also be considered and explored [30].
Our study may have some limitations. First, the included studies exhibited a high level of heterogeneity and a certain level of publication bias. Second, studies of the PD-1/PD-L1 in HCC were still in its early phase and more RCTs were needed as higher level evidences. Third, most of the studies showed interim results and published with abstract or poster; relevant information is not sufficient and thorough. Lastly, the number of studies for PD-1 is much larger than that of PD-L1, and all anti-PD-L1 drugs were published as abstracts, which may be a possible source of bias.
Conclusion
In conclusion, our meta-analysis suggested that PD-1/PD-L1 inhibitors improved the outcomes of response rates and survival time in advanced HCC. PD-1/PD-L1 inhibitors have generally changed the situation of HCC systemic therapy, and further the greater changes in this field of research may still be on the way.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424.
Tella SH, Mahipal A, Kommalapati A, Jin Z. Evaluating the safety and efficacy of nivolumab in patients with advanced hepatocellular carcinoma: evidence to date. Onco Targets Ther 2019;12:10335–10342.
Lin S, Hoffmann K, Schemmer P. Treatment of hepatocellular carcinoma: a systematic review. Liver Cancer 2012;1:144–158.
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008;359:378–390.
Siegel AB, Olsen SK, Magun A, Brown RS Jr. Sorafenib: where do we go from here? Hepatology 2010;52:360–369.
Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 2010;363:711–723.
Nishijima TF, Shachar SS, Nyrop KA, Muss HB. Safety and tolerability of PD-1/PD-L1 inhibitors compared with chemotherapy in patients with advanced cancer: a meta-analysis. Oncologist 2017;22:470–479.
Carretero-Gonzalez A, Lora D, Ghanem I, Zugazagoitia J, Castellano D, Sepulveda JM, Lopez-Martin JA, et al. Analysis of response rate with ANTI PD-1/PD-L1 monoclonal antibodies in advanced solid tumors: a meta-analysis of randomized clinical trials. Oncotarget 2018;9:8706–8715.
Boussiotis VA. Molecular and biochemical aspects of the PD-1 checkpoint pathway. N Engl J Med 2016;375:1767–1778.
Ceeraz S, Nowak EC, Noelle RJ. B7 family checkpoint regulators in immune regulation and disease. Trends Immunol 2013;34:556–563.
Li JH, Ma WJ, Wang GG, Jiang X, Chen X, Wu L, Liu ZS, et al. Clinicopathologic significance and prognostic value of programmed cell death ligand 1 (PD-L1) in patients with hepatocellular carcinoma: a meta-analysis. Front Immunol 2018;9:2077.
Zongyi Y, Xiaowu L. Immunotherapy for hepatocellular carcinoma. Cancer Lett 2020;470:8–17.
Kudo M. Immune checkpoint inhibition in hepatocellular carcinoma: basics and ongoing clinical trials. Oncology 2017;92(Suppl 1):50–62.
El-Khoueiry AB, Melero I, Crocenzi TS, Welling TH, Yau TC, Yeo WN, Chopra A, et al. Phase I/II safety and antitumor activity of nivolumab in patients with advanced hepatocellular carcinoma (HCC): CA209-040. J Clin Oncol 2015;33(18_suppl):LBA101.
El-Khoueiry AB, Sangro B, Yau T, Crocenzi TS, Kudo M, Hsu C, Kim TY, et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet 2017;389:2492–2502.
Guo B, Moga C, Harstall C, Schopflocher D. A principal component analysis is conducted for a case series quality appraisal checklist. J Clin Epidemiol 2016;69(199–207):e192.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–634.
Bruix J, Qin S, Merle P, Granito A, Huang YH, Bodoky G, Pracht M, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017;389:56–66.
Kudo M, Finn RS, Qin S, Han KH, Ikeda K, Piscaglia F, Baron A, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet 2018;391:1163–1173.
El-Serag HB, Marrero JA, Rudolph L, Reddy KR. Diagnosis and treatment of hepatocellular carcinoma. Gastroenterology 2008;134:1752–1763.
Pardee AD, Butterfield LH. Immunotherapy of hepatocellular carcinoma: unique challenges and clinical opportunities. Oncoimmunology 2012;1:48–55.
Finn RS, Ryoo BY, Merle P, Kudo M, Bouattour M, Lim HY, Breder V, et al. Pembrolizumab as second-line therapy in patients with advanced hepatocellular carcinoma in KEYNOTE-240: a randomized, double-blind, phase III trial. J Clin Oncol 2020;38:193–202.
Yau T, Park JW, Finn RS, Cheng AL, Mathurin P, Edeline J, Kudo M, et al. CheckMate 459: a randomized, multi-center phase III study of nivolumab (NIVO) vs sorafenib (SOR) as first-line (1L) treatment in patients (pts) with advanced hepatocellular carcinoma (aHCC). Ann Oncol 2019;30:874.
Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, Kudo M, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med 2020;382:1894–1905.
Shigeta K, Datta M, Hato T, Kitahara S, Chen IX, Matsui A, Kikuchi H, et al. Duan programmed death receptor-1 and vascular endothelial growth factor receptor-2 blockade promotes vascular normalization and enhances antitumor immune responses in hepatocellular carcinoma. Hepatology 2019;71:1247–1261.
Lee M, Ryoo BY, Hsu CH, Numata K, Stein S, Verret W, Hack S, et al. Randomised efficacy and safety results for atezolizumab (Atezo) plus bevacizumab (Bev) in patients (pts) with previously untreated, unresectable hepatocellular carcinoma (HCC). Ann Oncol 2019;30:875.
Yau T, Kang YK, Kim TY, El-Khoueiry AB, Santoro A, Sangro B, Melero I, et al. Nivolumab (NIVO) plus ipilimumab (IPI) combination therapy in patients (pts) with advanced hepatocellular carcinoma (aHCC): results from CheckMate 040. J Clin Oncol 2019;37(15_suppl):4012.
Terashima T, Yamashita T, Toyama T, Arai K, Kawaguchi K, Kitamura K, Yamashita T, et al. Surrogacy of time to progression for overall survival in advanced hepatocellular carcinoma treated with systemic therapy: a systematic review and meta-analysis of randomized controlled trials. Liver Cancer 2019;8:130–139.
Feng Z, Rong P, Wang W. Meta-analysis of the efficacy and safety of PD-1/PD-L1 inhibitors administered alone or in combination with anti-VEGF agents in advanced hepatocellular carcinoma. Gut 2019. https://doi.org/10.1136/gutjnl-2019-320116
Cheng AL, Hsu C, Chan SL, Choo SP, Kudo M. Challenges of combination therapy with immune checkpoint inhibitors for hepatocellular carcinoma. J Hepatol 2020;72:307–319.
Acknowledgements
This study was supported by National Key Technologies R&D Program of China (no. 2017YFC0110904), National Key Technologies R&D Program of China (no. 2017YFC0110904), National Natural Science Foundation of China (no. 81800577), and Beijing Natural Science Foundation (no. 7202033).
Author information
Authors and Affiliations
Contributions
ZTZ: study design, and manuscript writing, and statistical analysis. WG: study design, manuscript writing, and finalizing. QR: study design, manuscript writing, literature searching, data abstraction, and statistical analysis. ML: manuscript writing and statistical analysis. WX: literature review, and manuscript writing and reviewing. DW: study design, literature search, and review. KP: literature review, and manuscript writing and reviewing. XBG: manuscript writing and reviewing.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rao, Q., Li, M., Xu, W. et al. Clinical benefits of PD-1/PD-L1 inhibitors in advanced hepatocellular carcinoma: a systematic review and meta-analysis. Hepatol Int 14, 765–775 (2020). https://doi.org/10.1007/s12072-020-10064-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-020-10064-8