Abstract
Objective
The relationship between chronic hepatitis B virus (HBV) infection and fatty liver in patients remains unclear. Although high-fat diets-induced hepatic steatosis was proved to reduce HBV replication in transgenic mice, the interplay between HBV and fatty liver in immunocompetent mouse model is yet to be elucidated. Here, we aimed to develop an effective animal model for intracellular HBV persistence combined with hepatic steatosis and to explore their interactions.
Methods
FVB/N mice with HBV genotype B replicon DNA were established by hydrodynamic injection. Mice injected with HBV or control plasmid vectors were then randomized into NAFLD + HBV, HBV, NAFLD, and control groups and treated with a high-fat or standard diet for up to 14 weeks. The characteristics of NAFLD were evaluated by physical indices, liver function tests, glycolipid metabolism, and liver histopathological changes. Viral dynamics were also analyzed by HBV DNA and HBV-related antigens.
Results
HBV clone persistently replicated in the livers of FVB/N mice, and hepatic steatosis was induced by a high-fat diet. The NAFLD and NAFLD + HBV groups shared similar physical features, glycolipid metabolism, liver function, and hepatic steatosis. Serum hepatitis B e antigen (HBeAg), hepatic hepatitis B s antigen (HBsAg),hepatitis B c antigen (HBcAg), and HBV DNA were decreased in the NAFLD + HBV group compared with those in the HBV group at the end of 14 weeks.
Conclusion
In an HBV-immunocompetent mouse model, non-alcoholic hepatic steatosis inhibited HBV replication, as indicated by the reduction of HBV DNA and HBV-related antigens. HBV replication did not alter lipid metabolism in mice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic hepatitis B virus (HBV) infection remains a global health issue associated with substantial morbidity and mortality owing to induction of acute and chronic necro-inflammatory liver diseases, hepatic cirrhosis, and hepatocellular carcinoma (HCC) [1]. Despite the development of a highly effective preventive vaccine and antiviral agent, in 2010, about 248 million individuals worldwide were estimated to be hepatitis B s antigen (HBsAg) positive and at risk of developing end-stage liver disease, including cirrhosis and HCC, owing to viral factors, such as HBV DNA, hepatitis B e antigen (HBeAg), genotype, and other metabolic factors [2]. As the global prevalence of obesity and other components of metabolic syndrome have increased in the last decade, non-alcoholic fatty liver disease (NAFLD) has also become increasingly common in the general population [3].The disease spectrum of NAFLD ranges from simple hepatic steatosis to non-alcoholic steatohepatitis (NASH) and eventually to liver cirrhosis or HCC [4]. This disease could eventually become the major cause of end-stage liver disease and thus represents a major health concern.
Although many Asian patients suffer from both NAFLD and chronic HBV infection, the bilateral effects and underlying mechanisms have not yet been adequately clarified. Hepatic steatosis, a hallmark histological feature of NAFLD that is associated with chronic hepatitis C (CHC) infection [5], occurs in at least one-quarter of cases of chronic HBV infection and may be responsible for more rapid disease progression and increased risk of liver cirrhosis and HCC in patients with HBV and NAFLD [6,7,8]. In addition, hepatic steatosis can decrease the response to PEGylated interferon (PEG-IFN) and entecavir antiviral treatment in patients with chronic HBV infection [9, 10]. However, the relationship between HBV chronicity and hepatic steatosis remains controversial. Several studies have shown that hepatic steatosis may contribute to HBsAg clearance, HBeAg seroconversion, and suppression of hepatitis B viral replication in patients with CHB and hepatic steatosis [11,12,13,14]. These findings were further confirmed by a recent large-scale cohort study indicating a negative association of hepatic steatosis with viral load, suggesting that hepatic steatosis may enhance viral clearance and inhibit HBV DNA replication [6]. In contrast, some studies have reported that there is no difference in HBV replication between patients with and without NAFLD [15, 16], and another large-scale cohort study showed that HBV infection decreased the risk of NAFLD, implying that HBV may play an independent and protective role in the development of NAFLD [17]. Accordingly, it is essential to develop an animal model for the systematic investigation of hepatic steatosis and HBV persistence. As HBV only infects humans and primates, HBV studies are restricted by the available animal models. Transgenic mouse models have been applied to investigate HBV-associated diseases as effective tools, which are inherently tolerant to transgene products. However, these animals are not manipulated under normal physiological conditions. Therefore, establishment of an immunocompetent mouse model of HBV persistence and NAFLD would enable scientists to study the mechanisms of HBV chronicity and hepatic steatosis.
Accordingly, in this study, we adopted a nontransgenic, immunocompetent mouse model with persistent HBV genotype B replication in the liver by taking advantage of the liver-targeting feature of hydrodynamic injection. NAFLD was then induced by long-term consumption of a high-fat diet (HFD) for up to 14 weeks, and the effects of NAFLD on HBV persistent replication and viral dynamics were assessed. This animal model will facilitate our understanding of the relationships and mechanisms of HBV tolerance and hepatic steatosis.
Materials and methods
Mice and experimental procedures
FVB mice (male, 6–8 weeks of age) purchased from the Beijing Vital River Laboratory Animal Technology (Beijing, China) were bred in the specific pathogen-free animal experiment center of Huazhong University of Science and Technology. For the experiment, 10 μg pHBV1.3-B6 replicon DNA or the control vector in a volume of phosphate-buffered saline equivalent to 8% of the mouse’s body weight was introduced by tail vein injection within 6–8 s. Angular vein blood was collected from the eyes on the third day after the injection and assayed for HBeAg. HBeAg-positive and control mice were randomly assigned to be fed HFD containing 60% of the total kilocalories from fat or a normal diet containing 10% of the total kilocalories from fat as the NAFLD + HBV, NAFLD, HBV, and control groups, respectively, for 14 weeks. All mice were provided food and water ad libitum, and their body weights were recorded weekly. The mice were killed at the end of 14 weeks. Blood samples collected from the angular vein were maintained at − 80 °C. The livers were quickly removed and weighed. Part of the liver was immediately fixed in 4% paraformaldehyde solution for histological analysis. The left liver tissue was frozen at − 80 °C for further analysis.
Measurement of blood biochemical indexes
Serum levels of HBeAg were detected using chemiluminescent immunoassays (Abbott I4000 IM0109). Serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), fasting blood glucose (FBG), total cholesterol (TC), triglycerides (TGs), high-density lipoprotein (HDL), and low-density lipoprotein (LDL) were measured using a Roche automatic biochemical analyzer. Serum insulin was detected using an enzyme-linked immunosorbent assay (ELISA) kit (Mercodia, Sweden).The insulin resistance score was determined using homeostasis model assessment (HOMA-IR = fasting insulin [mU/L] × fasting glucose [mg/dL] × 0.05551/22.5).
Hepatic histology analysis
Liver tissues from mice were fixed in 4% paraformaldehyde solution and embedded in paraffin for hematoxylin and eosin (H&E) and oil red O staining according to standard methods. Total TG levels in livers were measured by enzymatic assays using a TG assay kit (Nanjing Jianchen Bioengineering Institute, China), according to the manufacturer’s instructions. Liver sections were stained with rabbit anti-HBcAg antibodies (1:100 dilution; Novus Biologicals, USA) and were then detected using the streptavidin–peroxidase complex method with a Histostain-plus kit, DAB (Boster Biotechnology, Wuhan, China) following the manufacturer’s instructions. HBsAg in the liver was measured using chemiluminescent immunoassays (Abbott I4000 IM0109). Liver HBV DNA was detected by quantitative polymerase chain reaction (PCR) kit (KHB, Shanghai, China). Liver total RNA was extracted from liver tissues for analysis. 1 μg of total RNA was reverse-transcribed to cDNA using a PrimeScript RT reagent kit (TaKaRa Biotechnology, Dalian, China). cDNA equivalent to 50 ng of total RNA was used for PCR assay. The mRNA expression of tumor necrosis factor-α (TNF-α), interleukin (IL)-6, IL-1β, and HBV pgRNA was measured by real-time reverse transcription PCR (RT-PCR) using a SYBR Premix Ex Taq kit (TaKaRa Biotechnology, Dalian, China) in accordance with the manufacturer’s instructions. The specific primer pairs were: IL-1β-forward: 5- TGTAATGAAAGACGGCACACC-3, IL-1β-reverse: 5-TCTTCTTT GGGTATTGCTTGG-3; TNF-α-forward: 5-GGCAGGTCTACTTTGGAGTCATTG-3, TNF-α -reverse: 5-ACATTCGAGGCTCCAGTGAATTCGG-3; IL-6-forward: 5-CCACGGCCTTCC CTACTTC-3, IL-6-reverse: 5-CTCATTTCCACGATTTCCCAG-3; HBV pgRNA-forward: 5- AGTGTGGATTCGCACTCCT-3, HBV pgRNA-reverse: 5-GAGTTCTTCTTCTAGGG GACCTG-3; β-actin-forward: 5-GGTCAGAAGGACTCCTATGTGG-3, β-actin-reverse: 5-TGTCGTCCCAGTTGGTAACA-3; ELISA kits (Neobioscience, Shenzhen, China) were used to determine the concentrations of TNF-α, IL-6, IL-1β, IFN-β, and IFN-γ in hepatic homogenates. Western blotting analyses of TNF-α (1:4000, Abcam, Cambridge, UK), IL-6 (1:4000, Guge Biotechnology, Wuhan, China), and IL-1β (1:4000, Abcam, Cambridge, UK) in hepatic homogenates were conducted as previously reported. β-actin (1:4000, Abbkine, CA, USA) quantification was used as an internal standard to correct for variations in total protein loading. Densitometric analysis of the blots was performed by using the software AlphaEase FC (Alpha Innotech, Silicon Valley, CA, USA).
Statistical analysis
Data are presented as means ± standard errors of the means (SEMs). The Kruskal–Wallis H test was used to assess significant intergroup variability and the Mann–Whitney U two-tailed test was used for between-group comparison. Differences with a p values of less than 0.05 were considered statistically significant.
Results
Viral characterization in FVB/N mice by hydrodynamic injection of HBV
FVB/N mice were hydrodynamically injected with a pGEM4Z/HBV1.3 replication plasmid containing a 1.3-fold overlength of a genotype B HBV genome or control vector. After HBV DNA injection, serum HBeAg was used as a marker to monitor HBV persistence in mice. HBV clone was persistently replicated in the livers of approximately 90% of FVB/N mice on the third day and 70% of mice at 14 weeks after injection (data not shown). Three days after injection and before HFD, the serum levels of HBeAg did not differ between the HBV and NAFLD + HBV groups (Fig. 1a). Compared with the HBV group, the serum levels of HBeAg and the levels of hepatic HBsAg, HBcAg, HBV DNA, and HBV pgRNA in the NAFLD + HBV group were decreased after 14 weeks of HFD, with the latter reaching significance at the end of the 14-week experiment (Fig. 1b). Immunohistochemistry further showed that the number of HBcAg-positive cells and the HBcAg-positive ratio were decreased in the NAFLD + HBV group as compared to that in the HBV group (Fig. 1c).
Viral characterization in FVB/N mice by hydrodynamic injection. The plasma HBeAg level did not show any difference on the third day (a), but the hepatic HBsAg, HBV DNA and HBV pgRNA levels were decreased in the NAFLD/HBV group compared with the NAFLD group (b). Immunohistochemistry staining of hepatitis B c antigen (HBcAg) and HBcAg-positive ratio were decreased in the NAFLD/HBV group compared with the NAFLD group (c)
Effects of HBV combined with NAFLD on physical and plasma biochemical parameters
After administration of the HFD, mice in the NAFLD + HBV and NAFLD groups suffered from obesity (Fig. 2a) and showed a significant increase in the liver to body weight ratio when compared with the other groups of mice (data not shown). There were no significant differences in plasma ALT, AST, FBG, insulin, TG, TC, HDL, or LDL levels between the control and HBV groups. Similarly, these plasma biochemical indices displayed no differences between the NAFLD and NAFLD + HBV groups during the experiment. However, the plasma levels of ALT, AST, TG, TC, LDL, FBG, and insulin as well as insulin resistance increased significantly both in the NAFLD and NAFLD + HBV groups compared to the control or HBV groups at 14 weeks, respectively (Fig. 2b–e).
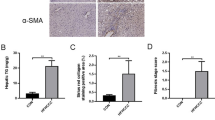
Effects of HBV combined with hepatic steatosis on histopathological changes
No obvious histopathological changes were observed in the HBV group by H&E and oil red O staining compared with controls. However, we observed progressive hepatic micro- and macrovesicular steatosis in the NAFLD + HBV and NAFLD groups during the experiment (Fig. 3a). Following exposure to HFD for 14 weeks, there was no obvious infiltration of inflammatory cells in the NAFLD + HBV and NAFLD groups. Analysis of the expression levels of TNF-α, IL-1β, and IL-6 by RT-PCR, ELISA, and western blot showed no difference between two groups and further confirmed these observations (Fig. 3b–d).
The effects of HBV combined with hepatic steatosis on histopathological changes. Histological features of liver disease in FVB/N mice in different groups. HE staining and oil red O staining for the control, non-alcoholic fatty liver disease (NAFLD), HBV and NAFLD/HBV groups at the end of 14 weeks (× 400) (a). The TNF-a, IL-6, and IL-1β levels were measured by RT-PCR (b), ELISA (c), and western blot (d)
Inverse association between cumulative plasma or hepatic TGs and HBV replication
The levels of hepatic TGs were significantly higher in the NAFLD + HBV and NAFLD groups than in the control and HBV groups at 14 weeks (Fig. 4a). There were no significant differences between the HBV and control groups or between the NAFLD + HBV and NAFLD groups (Fig. 4a). Inverse associations between cumulative plasma or hepatic TGs and hepatic HBsAg, HBcAg-positive ratio, and HBV DNA were observed by correlation analysis (Fig. 4b, c).
Inverse association between cumulative plasma or hepatic TGs and HBV replication. a Hepatic TGs were increased in the NAFLD + HBV group and NAFLD group as compared to the HBV and control group. b The correlations between plasma TG and hepatic HBV DNA and hepatic HBsAg level and the correlations between hepatic TG and hepatic HBV DNA and hepatic HBsAg level were shown
Discussion
Although the coexistence of HBV replication and NAFLD is frequently observed in clinical practice, their association is still controversial. Therefore, the establishment of an effective animal model of HBV combined with hepatic steatosis is required to understand their relationship. The most widely used model for chronic HBV infection is the HBV transgenic mouse, with the advantage of inherent immuno-tolerance to HBV and thereby serologically and immunologically resembling chronic HBV infection after neonatal transmission [18,19,20]. Previous work by Chen et al. established a successful FVB/N mouse model of HBV persistent replication by introducing HBV replicon DNA into the livers of FVB/N mice via hydrodynamic injection, in which these immunocompetent mouse strains provided a great convenience to explore the host and viral factors associated with HBV persistence in vivo [21]. Based on this information, FVB/N mice were injected with HBV clone and exposed to HFD (NAFLD + HBV and NAFLD groups) for up to 14 weeks. We observed that mice fed HFD presented with widely macrovesicular and microvesicular hepatic steatosis. Hepatic steatosis was further verified by the finding of disrupted lipid metabolism, such as significantly elevated levels of glycolipids and insulin resistance compared with that in mice fed a standard diet. These data demonstrated FVB/N mice could be adopted as a useful model for NAFLD. Intriguingly, only low levels of inflammatory responses were induced in NAFLD + HBV and NAFLD groups, as demonstrated by the lack of infiltrating inflammatory cells into livers. Thus, these typical manifestations of HFD-induced NAFLD were consistent with the first stage of NAFLD, namely non-alcoholic fatty liver (NAFL), and not NASH. Therefore, this model provides a basis for further studies of the relationship between persistent HBV replication and hepatic steatosis.
Viral replication in chronic HBV infection combined with NAFLD has not been extensively studied. Notably, an inverse relationship between HBV replication and hepatic steatosis has been observed in most studies. According to an early study by Chu et al., moderate to severe hepatic steatosis may contribute to HBsAg seroclearance in HBsAg carriers [11]. Moreover, a cohort study by Chu et al. showed that in HBsAg carriers with increased body mass index, hepatic steatosis can accelerate HBsAg seroclearance by approximately 5 years, although the beneficial effects of HBsAg seroclearance should be balanced against the harmful effects of hepatic steatosis [12]. A recent clinical study by Ceylan et al. reported that viral replication is decreased in patients with chronic HBV infection with NAFLD [14]. Additionally, some studies have demonstrated that there is no relationship between HBV replication and metabolic index in patients [15, 16]. This discrepancy may reflect the complexity of HBV infection combined with NAFLD in clinical practice. In our animal models, we found that serum HBeAg, hepatic HBcAg and HBsAg, HBV DNA, and pgRNA were obviously reduced in the NAFLD + HBV group compared with those in the HBV group. FVB/N mice exhibit additional defects in the secretion of C5 complement by macrophages, leading to lower levels of inflammatory responses; this factor may contribute to the high HBV persistence rates [21]. Consistent with this, we did not observe obvious inflammatory cells or cytokines in both the HBV and NAFLD groups. Thus, the decreased HBV DNA may be due to the metabolism of hepatic cells instead of activation of the liver immune response. Our findings implied that hepatic steatosis may directly affect HBV-related antigen expression and viral replication. Further studies are needed to confirm these results and elucidate the mechanisms through which hepatic steatosis affects viral dynamics.
Chronic infection with HCV, particularly genotype 3, has been shown to cause lipid metabolism disorders and induce hepatic steatosis [5]. Nevertheless, it is still unclear whether HBV can affect metabolic factors and cause fatty liver. In some studies, HBx has been shown to increase hepatocellular TGs and lead to hepatic steatosis by stimulating transcription factors or corresponding receptors in lipid metabolic pathways [22,23,24]. According to a study by Li et al., HBV infection in HepG2 cells could stimulate the expression of cholesterol metabolism-related genes and increase hepatic cholesterol via Toll-like receptor 2 [25]. However, hepatic steatosis does not appear to occur any more frequently in HBV-infected patients than in the general population [26]. In addition, host metabolic factors (obesity, hypertension, and dyslipidemia), rather than viral infection, appear to be the dominant determinants of the origination and progression of steatosis or steatohepatitis [27, 28]. In line with these clinical findings, the accumulation of plasma and hepatic lipid or cholesterol did not increase in HBV persistent replication with NAFLD compared with NAFLD alone. Similarly, plasma glucose and insulin levels were not altered in HBV + NAFLD compared with NAFLD groups, but significantly higher as compared with the HBV and control groups. These results were similar to a previous study by Wang et al., who showed that chronic HBV infection was not related to insulin resistance and did not induce hepatic steatosis [29]. Therefore, HFD, rather than viral factors, appeared to be responsible for the establishment of NAFLD in our rodent model.
In summary, through HBV DNA hydrodynamic injection and exposure to HFD in FVB/N mice, we established an animal model of persistent hepatic HBV replication combined with NAFLD. In this HBV-immunocompetent mouse model, non-alcoholic hepatic steatosis inhibited HBV replication, while virus replication did not alter lipid metabolism. Notably, hepatic steatosis may affect antiviral therapy in patients with HBV. Further studies are needed to assess this possibility.
References
Mortality GBD, Causes of Death C. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117–171
Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ. Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet 2015;386:1546–1555
Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology 2011;140:124–131
Wong VW, Wong GL, Choi PC, Chan AW, Li MK, Chan HY, et al. Disease progression of non-alcoholic fatty liver disease: a prospective study with paired liver biopsies at 3 years. Gut 2010;59:969–974
Asselah T, Rubbia-Brandt L, Marcellin P, Negro F. Steatosis in chronic hepatitis C: why does it really matter? Gut 2006;55:123–130
Cheng YL, Wang YJ, Kao WY, Chen PH, Huo TI, Huang YH, et al. Inverse association between hepatitis B virus infection and fatty liver disease: a large-scale study in populations seeking for check-up. PLoS One 2013;8:e72049
Wong GL, Wong VW, Choi PC, Chan AW, Chim AM, Yiu KK, et al. Metabolic syndrome increases the risk of liver cirrhosis in chronic hepatitis B. Gut 2009;58:111–117
Chan AW, Wong GL, Chan HY, Tong JH, Yu YH, Choi PC, et al. Concurrent fatty liver increases risk of hepatocellular carcinoma among patients with chronic hepatitis B. J Gastroenterol Hepatol 2017;32:667–676
Jin X, Chen YP, Yang YD, Li YM, Zheng L, Xu CQ. Association between hepatic steatosis and entecavir treatment failure in Chinese patients with chronic hepatitis B. PLoS One 2012;7:e34198
Ates F, Yalniz M, Alan S. Impact of liver steatosis on response to pegylated interferon therapy in patients with chronic hepatitis B. World J Gastroenterol 2011;17:4517–4522
Chu CM, Lin DY, Liaw YF. Does increased body mass index with hepatic steatosis contribute to seroclearance of hepatitis B virus (HBV) surface antigen in chronic HBV infection? Int J Obes (Lond) 2007;31:871–875
Chu CM, Lin DY, Liaw YF. Clinical and virological characteristics post HBsAg seroclearance in hepatitis B virus carriers with hepatic steatosis versus those without. Dig Dis Sci 2013;58:275–281
Machado MV, Oliveira AG, Cortez-Pinto H. Hepatic steatosis in hepatitis B virus infected patients: meta-analysis of risk factors and comparison with hepatitis C infected patients. J Gastroenterol Hepatol 2011;26:1361–1367
Ceylan B, Arslan F, Batirel A, Fincanci M, Yardimci C, Fersan E, et al. Impact of fatty liver on hepatitis B virus replication and virologic response to tenofovir and entecavir. Turk J Gastroenterol 2016;27:42–46.
Lesmana LA, Lesmana CR, Pakasi LS, Krisnuhoni E. Prevalence of hepatic steatosis in chronic hepatitis B patients and its association with disease severity. Acta Med Indones 2012;44:35–39
Wong VW, Wong GL, Chu WC, Chim AM, Ong A, Yeung DK, et al. Hepatitis B virus infection and fatty liver in the general population. J Hepatol 2012;56:533–540
Joo EJ, Chang Y, Yeom JS, Ryu S. Hepatitis B virus infection and decreased risk of nonalcoholic fatty liver disease: A cohort study. Hepatology 2017;65:828–835
Dembek C, Protzer U. Mouse models for therapeutic vaccination against hepatitis B virus. Med Microbiol Immunol 2015;204:95–102
Zheng Y, Chen WL, Louie SG, Yen TS, Ou JH. Hepatitis B virus promotes hepatocarcinogenesis in transgenic mice. Hepatology 2007;45:16–21
Cobleigh MA, Wei X, Robek MD. A vesicular stomatitis virus-based therapeutic vaccine generates a functional CD8 T cell response to hepatitis B virus in transgenic mice. J Virol 2013;87:2969–2973
Chen SH, Wu HL, Kao JH, Hwang LH. Persistent hepatitis B viral replication in a FVB/N mouse model: impact of host and viral factors. PLoS One 2012;7:e36984
Kim KH, Shin HJ, Kim K, Choi HM, Rhee SH, Moon HB, et al. Hepatitis B virus X protein induces hepatic steatosis via transcriptional activation of SREBP1 and PPARgamma. Gastroenterology 2007;132:1955–1967.
Kim K, Kim KH, Kim HH, Cheong J. Hepatitis B virus X protein induces lipogenic transcription factor SREBP1 and fatty acid synthase through the activation of nuclear receptor LXRalpha. Biochem J 2008;416:219–230
Wu YL, Peng XE, Zhu YB, Yan XL, Chen WN, Lin X. Hepatitis B virus X protein induces hepatic steatosis by enhancing the expression of liver fatty acid binding protein. J Virol 2015;90:1729–1740
Li YJ, Zhu P, Liang Y, Yin WG, Xiao JH. Hepatitis B virus induces expression of cholesterol metabolism-related genes via TLR2 in HepG2 cells. World J Gastroenterol 2013;19:2262–2269
Shi JP, Fan JG, Wu R, Gao XQ, Zhang L, Wang H, et al. Prevalence and risk factors of hepatic steatosis and its impact on liver injury in Chinese patients with chronic hepatitis B infection. J Gastroenterol Hepatol 2008;23:1419–1425
Peng D, Han Y, Ding H, Wei L. Hepatic steatosis in chronic hepatitis B patients is associated with metabolic factors more than viral factors. J Gastroenterol Hepatol 2008;23:1082–1088
Zheng RD, Chen JN, Zhuang QY, Lu YH, Chen J, Chen BF. Clinical and virological characteristics of chronic hepatitis B patients with hepatic steatosis. Int J Med Sci 2013;10:641–646
Wang CC, Hsu CS, Liu CJ, Kao JH, Chen DS. Association of chronic hepatitis B virus infection with insulin resistance and hepatic steatosis. J Gastroenterol Hepatol 2008;23:779–782.
Acknowledgements
The authors express their gratitude to Prof. Chen PJ (Department of Internal Medicine, National Taiwan University Hospital) for the kind gift of the HBV1.3-B6 plasmid.
Funding
This study was supported by the National Natural Science Foundation of China NSFC Grants (81571989, 81100282, 81500452), Program for Innovative Research Team of Chinese Ministry of Education (IRT-14R20) and National Science and Technology Major Project (2017ZX10202201).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Danqing Hu, Hongwu Wang, Hai Wang, Yaqi Wang, Xiaoyang Wan, Weiming Yan, Xiaoping Luo, and Qin Ning declare that they have no competing interests.
Animal study
All experiments were performed using procedures approved by the Huazhong University Institutional Animal Care and Use Committee.
Rights and permissions
About this article
Cite this article
Hu, D., Wang, H., Wang, H. et al. Non-alcoholic hepatic steatosis attenuates hepatitis B virus replication in an HBV-immunocompetent mouse model. Hepatol Int 12, 438–446 (2018). https://doi.org/10.1007/s12072-018-9877-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-018-9877-7